OBJECTIVE: To investigate the clinimetric properties of the de Morton Mobility Index (DEMMI) in a Geriatric Evaluation and Management (GEM) population.
DESIGN: A longitudinal validation study (n = 100) and inter-rater reliability study (n = 29) in a GEM population.
Patients: Consecutive patients admitted to a GEM rehabilitation ward were eligible for inclusion.
METHODS: At hospital admission and discharge, a physical therapist assessed patients with physical performance instruments that included the 6-metre walk test, step test, Clinical Test of Sensory Organization and Balance, Timed Up and Go test, 6-minute walk test and the DEMMI. Consecutively eligible patients were included in an inter-rater reliability study between physical therapists.
RESULTS: DEMMI admission scores were normally distributed (mean 30.2, standard deviation 16.7) and other activity limitation instruments had either a floor or a ceiling effect. Evidence of convergent, discriminant and known groups validity for the DEMMI were obtained. The minimal detectable change with 90% confidence was 10.5 (95% confidence interval 6.1–17.9) points and the minimally clinically important difference was 8.4 points on the 100-point interval DEMMI scale.
CONCLUSION: The DEMMI provides clinicians with an accurate and valid method of measuring mobility for geriatric patients in the subacute hospital setting.
Key words: psychometrics; rehabilitation; geriatric assessment; ageing; validity; reliability; Rasch analysis.
J Rehabil Med 2010; 42: 956–961
Correspondence address: Natalie A de Morton, Musculoskeletal Research Centre, La Trobe University, Plenty Rd, Bundoora, Victoria, 3083, Australia. E-mail: n.demorton@latrobe.edu.au
Submitted February 1, 2010; accepted August 31, 2010
Introduction
One of the key reasons for older adult admission to a Geriatric Evaluation and Management (GEM) rehabilitation hospital ward is to improve their mobility and subsequent functional ability prior to discharge. GEM patients are typically frail with multiple co-morbidities and often have complex discharge planning requirements. Rehabilitation typically involves intervention from a geriatrician, physical therapist and as required by occupational therapy, social work, speech therapy and dietetics in attempt to maximize patient functional capacity.
High-quality outcome measures that support clinical decision-making have been shown to improve patient outcomes (1). Despite GEM patients usually receiving regular physiotherapy intervention and significant costs per hospital bed day, no instrument has been identified as the “gold standard” method for accurately measuring changes in mobility in this patient group. The Functional Independence Measure (2–4) or the Barthel Index (5) are commonly applied at admission and discharge by multidisciplinary teams in the rehabilitation hospital setting. However, the major limitation of multidimensional instruments is that changes in total scores may obscure important changes on the construct of interest, in this case “mobility”, as performance in other domains such as continence or self-care can change concurrently with changing mobility status (6). Currently recommendations do not exist regarding the optimal method for measuring the important construct of mobility for older patients in the rehabilitation hospital setting.
Two comprehensive systematic reviews have identified that no instrument existed that could accurately measure from bed-bound to high levels of independent mobility in the hospital or community settings (7, 8). An instrument that could accurately measure patient mobility across acute and subacute hospital settings would have many advantages for patients, clinicians and researchers. The primary benefit would be enhanced continuity of patient care across clinical settings.
The de Morton Mobility Index (DEMMI) is a new mobility instrument that was developed in the acute hospital setting to overcome the limitations of existing instruments and has face validity for measuring across the broad mobility spectrum in the rehabilitation hospital setting (9). The DEMMI was developed based on the Rasch model and is therefore a unidimensional instrument of mobility (i.e. it measures only one construct). It is administered by clinician observation of performance on 15 hierarchical mobility challenges. It has a broad scale width, includes items that are typically included in a physical assessment, can be performed at the patient’s bedside, takes less than 9 min, on average, to administer in the acute hospital setting, does not require specialized equipment and provides interval level data. The measurement properties of the DEMMI have been extensively investigated in an older acute medical population (9).
Since the DEMMI is appropriate for application in the acute hospital setting and has a broad scale width, it appears to have the properties required for use in the rehabilitation hospital setting. Therefore, the primary aim of this study was to investigate the validity of the DEMMI in a GEM population using a head-to-head comparison design with commonly used measures of activity limitation.
Methods
Participants
Consecutive patients admitted to the GEM ward in a rehabilitation hospital in Victoria, Australia and who were referred for physiotherapy between January and April 2008 were eligible for inclusion in this study. Patients were excluded from this study if they did not assent to their physical therapy assessment, were too confused or agitated to participate in the assessment, were admitted to the ward for convalescence, were identified as requiring interim care (residential placement) or had documented contraindication to mobilization (e.g. due to diagnosed deep venous thrombosis).
Testing procedure
Consecutively eligible GEM patients were assessed within 3 working days (Monday to Friday) of hospital admission and discharge to the ward by the hospital physical therapist. There were two physical therapists on the study ward.
Patient demographic data was collected from the medical history and during the subjective interview with the patient, family or carer. This data included age, gender, diagnosis, primary language, place of prior residence, use of services prior to admission, pre-morbid gait aid and cognition via the abbreviated mental test score (10). Interpreters were employed when required.
Physical performance tests were completed by therapist observation of physical performance during the admission and discharge physical therapy assessments. These measures included the 6-metre walk test (11), modified Clinical Test of Sensory Organization and Balance (12), step test (13), 6-minute walk test (6MWT) (14) and DEMMI (9) and are described in further detail in the outcome measures section below. To avoid the effects of fatigue or practice influencing activity limitation test scores, the order of outcome measure test administration was randomized across participants using computer-generated random numbers (from the random generation function in Microsoft Excel).
After hospital discharge, data was also collected from hospital records regarding discharge diagnosis, length of hospital stay and discharge destination. Ethics approval for this study was obtained from the Northern Hospital and Monash University Human Ethics Committees.
Activity limitation outcome measures
de Morton Mobility Index (DEMMI). The DEMMI is administered by clinician observation of performance on 15 hierarchical mobility challenges, administered from easiest to hardest within 5 practical subsections: bed, chair, static balance, walking and dynamic balance. Interval level total scores ranging from 0 to 100 are obtained, where 0 represents poor mobility and 100 indicates independent mobility.
Six-metre walk test. Using the standardized protocol, the 6-metre walk was used as a performance measure of velocity and stride length (11).
Modified CTSIB. The modified Clinical Test of Sensory Organization and Balance was originally developed by Shumway-Cook & Horak (12) and was later modified to include only 4 conditions (15). The modified Clinical Test of Sensory Organization and Balance is a performance measure of ability to stand and maintain balance under the following conditions of sensory input (maximum 30 s):
• stand on a firm surface with eyes open (condition 1);
• stand on a firm surface with eyes closed (condition 2);
• stand on compliant foam with eyes open (condition 3);
• stand on compliant foam with eyes closed (condition 4).
Step test. The step test is a performance measure that evaluates speed of performing a dynamic single limb stance task (13). Using a stopwatch the number of times the patient could repeat this without losing balance or relying on external support in 15 s was recorded. This process was conducted on the right and left legs.
Timed Up and Go. The Timed Up and Go was designed to measure speed during functional tasks that potentially threaten balance (16). Using the standardized protocol, patients were asked to use their appropriate gait aid and on the command “go” to rise from a standard 45 cm chair, at a comfortable and safe pace, walk to a line 3 m away, turn, return to the chair and sit down.
Six-minute walk test (6MWT). The 6MWT is a simple and quick test to measure gait endurance (14) and has been shown to have high retest reliability in frail older subjects (17). The standardized protocol was applied and the distance that each patient was able to walk in 6 min was recorded.
Inter-rater reliability study
An inter-rater reliability study was conducted to investigate the measurement error associated with the DEMMI in the rehabilitation hospital setting. Consecutively eligible GEM patients were assessed using the DEMMI by two physical therapists (on two days that were planned for data collection prior to conducting the validation study described above). For each patient, one therapist who had extensive experience in conducting the DEMMI (one of two research physical therapists) and the second therapist who had no experience with using the DEMMI prior to the day of testing (one of many therapists at the rehabilitation hospital). The order of therapist test administration was randomized by a coin toss for each patient.
After the first DEMMI assessment and a minimum 30-min rest, the other physical therapist repeated the DEMMI assessment and was blind to the initial assessment score. After each DEMMI assessment the patient was asked if they were fatigued by the assessment.
Data analysis
Data analyses were performed using SPSS version 12.0 (18) and RUMM2020 (19) for Rasch analysis.
Convergent and discriminant validity. Convergent and discriminant validity were investigated with Spearman’s correlation coefficients (and associated 95% confidence intervals (CI)). A moderate to high significant correlation was hypothesized between DEMMI scores and measures of related constructs (Timed Up and Go Test, 6MWT, 6-metre walk test, step test and modified Clinical Test of Sensory Organization and Balance), to provide evidence of convergent validity. A low correlation was hypothesized between DEMMI scores and measures of other constructs (abbreviated mental test score) to provide evidence of discriminant validity.
Known groups validity. To investigate known groups validity, an independent t-test was performed comparing admission DEMMI scores for patients who used no gait aid or only a walking stick for ambulation compared with other walking aids or were non-ambulant and required a mechanical patient lifting device (hoist) for transfers. In addition, an independent t-test was also performed that compared discharge DEMMI scores for patients discharged to their usual place of residence compared with other discharge destinations.
Rasch analysis is a form of instrument validation as it investigates instrument unidimensionality (i.e. whether the instrument is measuring the single construct that it intends to measure, in this case “mobility”). The DEMMI was constructed as a unidimensional measure of mobility, using Rasch analysis, in an older acute medical population. Therefore, Rasch analysis was conducted in this study to investigate the unidimensionality of DEMMI in a rehabilitation GEM population.
Fit of data to the Rasch model would indicate that scale items are measuring one construct of “mobility” (i.e. that some items are not performing differently in a rehabilitation population compared with an older acute medical population). This is indicated by a total-item χ2 probability greater than 0.05 (i.e. no significant deviation of the data from the Rasch model) and a t-test procedure result of less than 5% as recommended by Tennant & Pallant (20). Item misfit was investigated and was considered to have occurred if the χ2 or F statistic probability value was less than the Bonferroni-adjusted α value for multiple testing or the fit residuals were greater than ± 2.5. Differential item functioning was investigated to identify items that operated differently for people of the same level of ability. For example, it is possible that the relative difficulty of a particular item might be different based on another variable such as age or gender. Differential item functioning by age (59–69 years, 70–79 years, ≥ 80 years) and gender were investigated and considered significant if the χ2 probability value was lower than the Bonferroni-adjusted p-value.
The minimally clinically important difference was calculated using the distribution based method recommended by Norman et al. (21). Norman et al. recommend that the minimally clinically important difference can be estimated by calculating half the baseline standard deviation of admission scores.
Responsiveness to change. Measurement responsiveness was calculated using hospital admission and discharge activity limitation scores. The effect size index (22), a distribution based index (and associated 95% CI), was calculated for each activity limitation outcome measure. The effect size index was calculated using the following formula recommended by Kazis et al. (22).
Inter-rater reliability. The minimal detectable change at 90% confidence and accompanying 95% CI was calculated to report measurement error for the DEMMI in the inter-rater reliability study. The minimal detectable change at 90% confidence was calculated from the standard error of measurement (23).
Results
Participant demographics
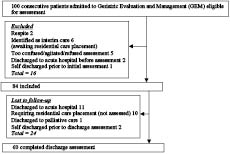
Of the 100 participants admitted to the GEM ward during the study period, 84 were included. The mean age of included participants was 81.8 years (SD 9.0), 57.1% were female and 65.5% were from an English-speaking background. Fig. 1 shows the flow of patients in this study and Table I shows the baseline characteristics of included patients. The average length of stay for patients was 26.5 days (SD 18.3). There were no significant differences for any baseline characteristic between participants who were and were not included in the study and those who did and did not have a discharge assessment.
Fig. 1. Flow of participant inclusion and exclusion in this study.
| Table I. Baseline demographics of eligible participants for the validation study (n = 84) |
| | Participants |
| Age, years, mean (SD) (n = 84) | 81.8 (9.0) |
| Gender, (% female) (n = 84) | 57.1 |
| Race/ethnicity, n (%) (n = 84) English Italian Greek Maltese Other | 55 (65.5) 16 (19.0) 4 (4.8) 2 (2.4) 7 (8.3) |
| Place of prior residence, n (%) (n = 83) Home alone Home with other(s) Hostel (low level of supported care) Nursing home (high level of supported care) | 23 (27.4) 52 (61.9) 7 (8.3) 1 (1.2) |
| Preadmission gait aid, n (%) (n = 83) 2-wheeled frame 4-wheeled frame Single-point stick Nil Other | 10 (11.9) 25 (29.8) 19 (22.6) 23 (27.4) 6 (7.1) |
| Preadmission services, n (% used) (n = 84) Home help Personal care Meals on wheels | 31 (36.9) 25 (29.8) 8 (9.5) |
| GEM LOS, days, mean (SD) (n = 82) | 26.5 (18.3) |
| SD: standard deviation; GEM: Geriatric Evaluation and Management; LOS: length of stay. |
Distribution of scores at admission to Geriatric Evaluation and Management ward
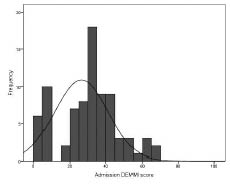
Activity limitation scores at hospital admission are shown in Table II. DEMMI scores at hospital admission were normally distributed without floor or ceiling effects (Fig. 2). The mean DEMMI score was 30.2 (SD 16.7) out of a maximum total possible score of 100.
| Table II. Activity limitation scores at hospital admission and discharge |
| | Admission | Discharge |
| n | Mean (SD) | n | Mean (SD) |
| DEMMI score (0–100) | 81 | 30.2 (16.7) | 56 | 40.9 (19.7) |
| 6-metre walk test Steps Times, s | 47 46 | 24.1 (13.4) 26.9 (24.1) | 49 48 | 20.9 (11.6) 21.9 (17.0) |
| mCTSIB (max of 30 s) C1 C2 C4 C5 | 84 83 81 82 | 16.3 (14.5) 10.9 (12.6) 8.5 (12.5) 2.2 (5.3) | 56 55 52 52 | 21.1 (13.2) 17.1 (13.4) 17.2 (23.2) 5.6 (10.0) |
| Step test, number of steps Left Right | 82 82 | 0.97 (2.4) 1.08 (2.4) | 54 54 | 2.5 (3.9) 2.4 (3.5) |
| Timed Up and Go, s | 28 | 35.3 (16.5) | 39 | 36.7 (26.9) |
| 6MWT, m | 81 | 30.2 (16.7) | 17 | 185.1 (54.0) |
| mCTSIB: modified Clinical Test of Sensory Organization and Balance; SD: standard deviation; DEMMI: de Morton Mobility Index; 6MWT: 6-minute walk test. |
Fig. 2. Distribution of the de Morton Mobility Index (DEMMI) scores at Geriatric Evaluation and Management hospital admission.
The 6-metre walk test, 6MWT and Timed Up and Go test had large floor effects with only 46 (55%), 12 (14.3%) and 28 (33%) patients able to obtain scores on these tests at hospital admission, respectively. The modified Clinical Test of Sensory Organization and Balance showed either a floor or ceiling effects for the different test conditions in this patient population. The step test also had a large floor effect, with 66 (78%) patients scoring zero on the test at hospital admission.
Validity
Evidence of convergent, discriminant and known groups validity for the DEMMI are shown in Table III.
| Table III. Evidence of validity for the de Morton Mobility Index (DEMMI) |
| | n | r (95% CI) | p |
| Convergent validity | | | |
| 6-metre walk test Steps Times, s | 47 46 | –0.42 (–0.63 to –0.15) –0.69 (–0.82 to –0.50) | 0.00 0.00 |
| mCTSIB, (max of 30 s) C1 C2 C4 C5 | 84 83 81 82 | 0.81 (0.72 to 0.87) 0.81 (0.72 to 0.87) 0.76 (0.65 to 0.84) 0.61 (0.45 to 0.73) | 0.00 0.00 0.00 0.00 |
| Step test, number of steps Left Right | 82 82 | 0.60 (0.44 to 0.72) 0.60 (0.44 to 0.72) | 0.00 0.00 |
| Timed Up and Go, s | 28 | –0.48 (–0.72 to –0.13) | 0.01 |
| 6MWT | 81 | 0.57 (0.40 to 0.70) | 0.06 |
| Discriminant validity | | | |
| DEMMI with AMTS | 53 | 0.25 (–0.02 to 0.49) | –0.66 |
| Known Groups Validity | n | Mean (SD) | Indep t-test, p |
| Uses a gait aid at hospital admis-
sion (admission DEMMI score) | |
| No aid or a walking stick | 4 | 58.75 (10.11) | 0.00 |
| Other walking aid/hoist | 77 | 28.75 (15.65) |
| Discharged to usual place of resi-
dence (discharge DEMMI score) | |
| Usual place of residence | 41 | 44.05 (16.55) | 0.05 |
| Other residence at discharge | 15 | 32.33 (25.09) |
| mCTSIB: modified Clinical Test of Sensory Organization and Balance; CI: confidence interval; AMTS: abbreviated mental test score; 6MWT: 6-minute walk test. |
The results of Rasch analysis indicated that the DEMMI is a unidimensional measure of mobility in a GEM rehabilitation population. The DEMMI data showed some mild misfit from the Rasch model at hospital admission (indicated by a significant item-trait χ2 of 51.83, df = 30, p = 0.01) and fitted the Rasch model at hospital discharge (indicated by a significant item-trait χ2 of 40.39, df = 30, p = 0.10). The unidimensionality test recommended by Tennant & Pallant (20) indicated unidimensionality at both hospital admission and discharge.
No items had fit residuals greater than ± 2.5 or disordered thresholds at hospital admission or discharge. At hospital admission some deviation from the Rasch model was identified for the tandem standing eyes closed (χ2 of 14.69, df = 2, p = 0.00) and walk backwards (F stat of 16.85, df = 2, p = 0.00) items, but this finding was not validated in the discharge data-set.
Minimal clinically important difference
The minimal clinically important difference was calculated using the distribution-based method recommended by Norman et al. (21) and was calculated to be 8.4 points on the DEMMI interval scale.
Responsiveness to change
Using the Effect Size Index (Table IV) there was no significant difference in responsiveness to change between the DEMMI and any of the activity limitation measures.
| Table IV. Responsiveness to change for activity limitation measures |
| | n | Effect Size Index (95% CI) |
| DEMMI score (0–100) | 56 | 0.69 (0.43–0.96) |
| 6-metre walk test Steps Times, s | 32 31 | 0.31 (–0.03–0.65) 0.27 (–0.08–0.62) |
| mCTSIB, (max of 30 s) C1 C2 C4 C5 | 56 55 52 52 | 0.27 (0.01–0.53) 0.35 (0.09–0.62) 0.64 (0.37–0.92) 0.53 (0.26–0.80) |
| Step test, number of steps Left Right | 53 53 | 0.50 (0.23–0.77) 0.37 (0.10–0.64) |
| Timed Up and Go | 19 | 0.38 (–0.06–0.84) |
| 6MWT, m | 9 | 1.02 (0.37–1.67) |
| mCTSIB: modified Clinical Test of Sensory Organization and Balance; DEMMI: de Morton Mobility Index; CI: confidence interval; 6MWT: 6-minute walk test. |
Reliability
Of the 30 consecutive GEM patients who participated in the reliability study, one was excluded as they declined to complete the second assessment that was required to be included in the reliability study. Of the 29 patients who were included in the reliability study, 14 reported that they were fatigued after the first assessment.
The mean DEMMI score for the hospital physical therapist was 33.90 (16.08) and the mean score for the research physical therapist was 34.75 (15.59). Correlation between independent assessor DEMMI interval scores was high (Pearson’s r = 0.87, 95% CI 0.76–0.94) and using a pooled SD of 15.84, the standard error of mean was calculated to be 5.49 (95% CI 3.81–7.79). The inter-rater reliability MDC90 was 12.7 points (95% CI 8.84–18.06) on the 100-point DEMMI interval scale. A paired t-test indicated no significant difference between assessor scores (p = 0.55).
Discussion
This study has validated the DEMMI in the subacute hospital setting in a GEM population. The DEMMI can accurately measure changes in mobility across the acute (9) and subacute hospital settings. This study indicates that patients can be measured using the same mobility instrument, the DEMMI, in both acute and subacute hospital settings.
Due to its broad scale width, the DEMMI can be applied to enhance continuity of patient care across acute and subacute clinical settings. The DEMMI overcomes the limitations of other activity limitation measures that are commonly used in the subacute setting. In this study, existing measures of activity limitation had either a floor or ceiling effect at rehabilitation hospital admission, whereas the DEMMI was able to accurately measure changes in mobility for all GEM patients. A previous study by Brusco et al. (24) reported a randomized controlled trial that investigated the effects of 6 days compared with the usual 5 days of physiotherapy provided in the subacute setting. Although a trend towards a reduction in length of stay was identified, no effect was identified on activity limitation outcome measures. It is possible that with a unidimensional measure of mobility such as the DEMMI, that can measure all patients without floor or ceiling effects, that the efficacy of such an intervention on mobility outcomes could be examined more accurately.
A similar estimate of measurement error (minimal detectable change at 90% confidence) and the minimally clinically important difference were identified for the DEMMI in this study, as reported in the multiple reliability studies that were conducted for the DEMMI in the acute hospital setting (9). The results of this study indicate that a change score of approximately 12 points or more on the DEMMI is likely to overcome measurement error (with 90% confidence) and represent a clinically important change in mobility. Although point estimates were higher in this study for the minimal detectable change at 90% confidence compared with the acute hospital setting, 95% confidence bands overlapped between studies and indicate no significant difference. Using Norman’s method to estimate the minimally clinically important difference, it would be expected that a smaller point estimate would be obtained in this study compared with the acute medical setting, as a GEM population is likely to be more homogeneous in their physical ability than an older acute medical population.
No significant difference in responsiveness to change was identified between the DEMMI and existing measures of activity limitation used this study. Except for the 6MWT, the DEMMI had the highest responsiveness point estimate. However, the 6MWT analysis included only 9 participants and highlights the fact that instruments that cannot measure patients at hospital admission and discharge have limited utility for clinicians and researchers, as change cannot be accurately and sensitively measured for individual patients or groups.
Similar evidence of validity was observed for the DEMMI in this study as the acute hospital setting. Evidence of convergent, discriminant and known groups validity were obtained and the results of Rasch analysis indicate that the DEMMI is essentially a unidimensional measure of mobility in a GEM population. Of further interest for the utility of the DEMMI was that a ceiling effect was not identified at hospital discharge in this study and that the DEMMI is likely to have the scale width required to also assess mobility in the community setting after discharge from the rehabilitation hospital setting.
A limitation of this study was that, for some of the tests (e.g. Timed Up and Go and 6-metre walk test), hospital admission assessments could not be performed for a large proportion of patients and limited the ability to accurately perform a direct head-to-head comparison of instruments. However, it was the inherent limitations of these instruments in a GEM population that resulted in this study limitation. A large proportion of GEM patients cannot walk the distance required to perform the 6-metre walk or Timed Up and Go Test at hospital admission and therefore a change score could not be obtained for these patients and significantly limited the clinimetric analyses that could be conducted for these instruments in this study. This further highlights the limitations of these instruments in this population. A second limitation of this study was that 24/84 (30%) participants did not have a discharge assessment conducted, largely due to participants declining in their health status and being transferred elsewhere and discharge assessments were thus not conducted. The impact of these missing data combined with participants who could not perform tests at hospital discharge on the study results is unknown. Lastly, this study was also conducted within the constraints of usual clinical care, but this also provides the advantage of allowing all participants regardless of cognition or spoken language, for example, to be included and thus enhances the generalizability of this study.
In conclusion, GEM patients are particularly vulnerable to declining mobility and adverse events during hospitalization. This study has confirmed that the DEMMI provides an advanced method for accurately measuring and monitoring changes in mobility in the subacute hospital setting. The DEMMI can be applied to identify early signs of decline and prompt early intervention or facilitate goal-setting for therapy. Evidence now supports the application of the DEMMI in the rehabilitation hospital setting. Other studies are now underway in other clinical groups in the rehabilitation hospital setting.
Acknowledgements
The authors are grateful for the support provided by the Broadmeadows Health Service Physiotherapy Department staff and the Northern Clinical Research Centre, Northern Health. Special thanks to Northern Health Physiotherapy Managers Jenni Smith and Sandie Chapman for their support.
This research was funded by a Northern Health small research grant and an NHMRC postdoctoral research fellowship for Dr Natalie de Morton (ID 519555). These funding sources have not had any influence on the interpretation of data or the final conclusions drawn.
REFERENCES