OBJECTIVE: The aim of this study was to analyse the burden on caregivers of chronic neurological patients taking part in community neurorehabilitation programmes, and to describe caregivers’ socio-demographic features and needs.
SUBJECTS: A total of 118 pairs of chronic neurological patients and their caregivers.
METHODS: Caregivers completed the Caregiver Burden Inventory, the Beck Depression Inventory, and an ad hoc socio-demographic questionnaire. The EuroQol-5D was used to measure patients’ quality of life. Patients’ cognitive status and functional independence status were assessed using the Mini-Mental State Examination and Barthel Index, respectively.
RESULTS: Data from 105 patient-caregiver pairs were analysed. The majority of caregivers (mean age 63.01 years (standard deviation 12.3)) were women (58%); 72% were spouses/partners. The burden of care was distributed across the 5 domains of the Caregiver Burden Inventory as follows: objective burden (34%), developmental burden (25%), physical burden (22%), social burden (10%), emotional burden (9%). Care burden correlated negatively with patient’s functional independence (p = 0.008) and quality of life (p = 0.000) and positively with caregiver depression (p = 0.000). Of the caregivers, 65.7% requested interventions aimed at reducing their burden.
CONCLUSION: There is a need to define structured interventions for assessing, preventing or managing problems related to stressful caregiving situations across the care continuum.
Key words: caregiver; neurorehabilitation; care burden; chronic diseases; neurological diseases.
J Rehabil Med 2010; 42: 818–822
Correspondence address: Michelangelo Bartolo, Neurorehabilitation 2, Neurological Institute NEUROMED, IRCCS, Via Atinense 18, IT-86077 Pozzilli, Isernia, Italy. E-mail: bartolomichelangelo@gmail.com
Submitted January 31, 2009; accepted July 16, 2010
INTRODUCTION
Neurological damage accounts for approximately 40% of cases of severe disability (in which individuals require daily help) and for the majority of cases of complex disability resulting from combinations of physical, cognitive and behavioural impairments (1). The high prevalence of neurological disorders and related disabilities is fuelling interest in the role of rehabilitation in the treatment of these conditions. In particular, community neurorehabilitation, defined as “specialised neurological rehabilitation for individuals living in their home community, as opposed to inpatients of acute care or rehabilitation institutions” (2), is receiving increasing attention from researchers and health policy makers. Community neurorehabilitation offers a series of advantages: it allows patients to be discharged from hospital earlier (3); it caters for the needs of individuals who do not require intensive hospitalization but would benefit from therapy (4); and it is an approach that allows individuals with chronic, progressive neurological disorders to receive periodic maintenance rehabilitation (5). Moreover, it is feasible on an outpatient basis, and is therefore less costly than traditional rehabilitation, which is provided as a hospital-based specialty (4). In this context, since more rehabilitation is now being delivered in outpatient/clinic settings, family members are having to play a greater and more active role in the coordination and provision of care for these patients. This is increasing the burden on caregivers.
Caregiver burden has been described as the physical, psychological, financial and social problems and disruption experienced by the principal caregiver of a family member (6). Caregivers have often been defined as the second victims of the disease, to underline the level of their involvement in the care of patients and, in particular, the level of stress they are under. It should be appreciated that they often take on this role under sudden and extreme circumstances, with minimal preparation and little guidance and support from healthcare systems (7).
Numerous studies have examined the risks for the psychological wellbeing and quality of life of individuals caring for sick relatives, focusing on different problems associated with caregiving (8): anxiety and depression (9), financial difficulties (10), restriction of daily activities (11), and effects on physical health (12).
As far as caregiving in chronic neurological diseases is concerned, most studies have, to date, focused on the caregivers of patients affected by Alzheimer’s disease and dementia (13), stroke (14) and Parkinson’s disease (15), independently of the rehabilitation setting. As far as we know, no studies have analysed caregiving in the context of community neurorehabilitation, considering chronic disability as a common, unifying element across different neurological diseases. Greater knowledge of caregiver burden and needs in the setting of community neurorehabilitation could be useful for planning, within this area, structured interventions aimed at guaranteeing a global approach to the management of care that takes into account the requirements not only of patients but also of their families. Therefore, the aims of this study were: (i) to describe socio-demographic features of caregivers of outpatients affected by chronic neurological diseases; (ii) to analyse and describe caregiver burden, as perceived by caregivers themselves; (iii) to analyse: (a) the influence of gender on caregiver-perceived burden, (b) the relationship between caregiver burden and caregiver depression, (c) the relationship between caregiver depression and patients’ functional status and quality of life, and (d) the relationship between caregiver burden and patients’ functional status and quality of life; (iv) to identify the possible predictive role of factors such as sex, age and education on caregiver burden; (v) to evaluate caregivers’ need for interventions in order to reduce their perceived burden, identifying the type of intervention preferred.
MATERIAL AND METHODS
Participants and procedures
A total of 118 consecutive pairs of subjects, made up of outpatients affected by chronic neurological diseases (referred to the “Majorana” Neurorehabilitation Service, Consorzio Cooperative Ri.Rei., Rome) and their principal caregivers were originally enrolled in the study. A principal caregiver was defined as “any person who, without being a professional or belonging to a social support network, usually lives with the patient and, in some way, is directly implicated in the patient’s care or is directly affected by the patient’s health problem” (16). Eight of these pairs did not return the questionnaires, while another 5 were excluded because they (n = 3 patients, n = 2 caregivers) failed to complete them. Therefore, the final study participants were 105 pairs of caregivers and neurorehabilitation outpatients. All the caregivers accompanied the patients to the rehabilitation centre where all the patients underwent a rehabilitation programme consisting of neuromotor activities (each session included cardiovascular warm-up activities, stretching exercises, strengthening exercises in a functional context, overground gait training, balance training, postural exercises, and relaxation exercises) and/or speech therapy. The rehabilitation project was based on individual 45-min sessions, 2 or 3 days per week, over a total of 40–60 days. The number of sessions per week and the duration of the rehabilitation project were decided on the basis of the patient’s neurological and functional status by an interdisciplinary rehabilitation team composed of a neurologist, a physiotherapist and a speech therapist.
All data were collected during scheduled neurological follow-up appointments. The clinicians (MB and DD) explained the study to the patients and caregivers (reassuring them that their privacy would be strictly protected), after which a cognitive and functional evaluation was performed and the questionnaires were administered to the participants. The self-report questionnaires were compiled in the waiting-room and posted in a special box. Both patients and caregivers gave their written informed consent to participate in the study, which was approved by the local ethics committee and was conducted in accordance with the revised version of Declaration of Helsinki.
Measurements
In order to measure the level of perceived burden of care, the presence of depressive symptoms and socio-demographic features, all the caregivers enrolled in the study completed the Caregiver Burden Inventory (CBI) (17), the Beck Depression Inventory (BDI) (18), and an ad hoc socio-demographic questionnaire (SDQ). In all the patients, quality of life was measured using the EuroQol-5D (EQ-5D) (19). To evaluate the patients’ cognitive status and functional independence the clinicians administered respectively, the Mini-Mental State Examination (MMSE) (20) and the Barthel Index (BI) (21).
Caregiver Burden Inventory
The CBI is a 24-item multi-dimensional questionnaire in which 5 subscales explore 5 different dimensions of caregiver burden:
• objective burden (which corresponds to the amount of time devoted to caregiving): the burden on the caregiver due to shortage of time (items 1–5);
• developmental burden: the caregiver’s sense of being left behind, unable to enjoy the same expectations and opportunities as his or her peers (items 6–10);
• physical burden: feelings of fatigue and chronic health problems (items 11–14);
• social burden, which results from a perceived conflict of roles (items 15–19);
• emotional burden, which originates from awareness of negative feelings towards the patient that can be induced by the patient’s bizarre and unpredictable behaviour (items 20–24) (17).
Subjects are asked to rate each item on a 5-point Likert scale ranging from 0 (not at all disruptive) to 4 (very disruptive). The global score is obtained by summing the scores of each subscale; higher scores correspond to greater levels of perceived burden.
Beck Depression Inventory
The BDI is a 21-item self-report scale used to assess a subject’s current overall level of depression. For each question, subjects have to choose one among different statements. The cut-off value is 9 and higher scores correspond to more serious depressive symptoms (18).
Socio-demographic questionnaire
Demographic data were collected by means of an ad hoc SDQ that investigated features both of patients and of caregivers, namely patient’s age, gender and diagnosis, caregiver’s age, sex, education, and relationship to the patient, and the presence of other persons who help care for the patient. We also asked the caregivers to express their feelings and preferences with regard to different proposed interventions aimed at reducing their burden.
EuroQol-5D
The EQ-5D is a generic quality of life measure; it comprises 5 questions on mobility, self-care, pain, usual activities, and psychological status with 3 possible answers for each item (1 = no problem, 2 = moderate problem, 3 = severe problem) (19). A summary index with a maximum score of 1 can be derived from these 5 dimensions by conversion with a table of scores. The maximum score of 1 indicates the best health state, by contrast with the scores of the individual questions, where higher scores indicate more severe or more frequent problems (22). In addition, a visual analogue scale (EQVAS) indicates general health status, with 100 corresponding to the best health status.
Statistical analysis
Statistical analysis was performed using descriptive statistics for sociodemographic variables and patient and caregiver measures, and Student’s t-test for comparisons.
Possible correlations between variables were tested using Pearson’s correlation coefficients. Because the EQ-5D score is used for population studies, whereas the EQVAS score is preferred for evaluating the efficacy of quality of life interventions (23), only the EQ-5D score was considered for the statistical analysis. The strength of the association was deemed weak for a correlation coefficient value of r < 0.30, moderate for r = 0.30–0.59, and strong for r ≥ 0.60.
In addition, factors related to each domain of the CBI were explored using multiple regression analysis. The dependent variables were the total scores of each of the CBI domains (in each case obtained by summing all the caregivers’ scores) and the total CBI score (obtained by summing all the caregivers’ total scores); the participants’ characteristics were the explanatory variables. The multiple regression analysis was conducted with a backward variable selection method (p < 0.05).
All analyses were carried out using the statistical package SPSS version 16.0 for Windows.
RESULTS
The socio-demographic characteristics of the patients and caregivers are summarized in Table I.
| Table I. Study population |
| Variables | Patients (n = 105) | Caregivers (n = 105) |
| Gender, n (%) | | |
| Male | 59 (56) | 44 (42) |
| Female | 46 (44) | 61 (58) |
| Age, years, mean (SD) | 66.87 (11.75) | 63.01 (12.39) |
| [range] | [26–83] | [41–83] |
| Education, years, mean (SD) | 8.25 (3.53) | 9.94 (3.34) |
| Diagnosis, n (%) | | |
| Stroke | 47 (45) | |
| Parkinson’s disease and parkinsonisms | 36 (34) | |
| Post-polio syndrome | 9 (8) | |
| Cerebral palsy | 5 (5) | |
| Degenerative ataxia | 3 (3) | |
| Neuro-oncology post-surgery | 3 (3) | |
| Amyotrophic lateral sclerosis | 2 (2) | |
| Disease duration, years, mean (SD) | 13 (13.48) | |
| [range] | [3–59] | |
| Relationship to the patient, n (%) | | |
| Spouse/partner | | 75 (72) |
| Son/daughter | | 13 (12) |
| Parent | | 5 (5) |
| Friend | | 12 (11) |
| Living with the patient | | 80 (76) |
| Additional help, n (%) | | |
| Informal help | | 30 (29) |
| Formal help | | 14 (13) |
| SD: standard deviation. | | |
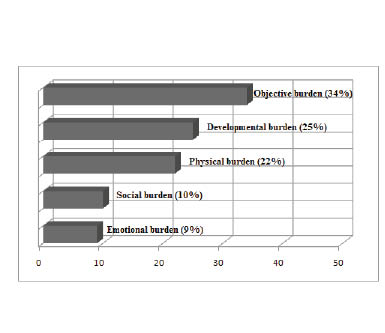
The total score of each CBI subscale (objective, developmental, physical, social, emotional) was calculated and expressed as a relative percentage of the total CBI score: objective burden, 34%; developmental burden, 25%; physical burden, 22%; social burden, 10%; emotional burden, 9% (Fig. 1). Gender differences were also examined: independent samples t-test analysis failed to reveal any statistical difference between caregiver burden perceived by men, mean value 29.56 (standard deviation (SD) 15.50) and by women, mean value 29.17 (SD 22.94) (p = 0.922).
Fig. 1. The distribution of caregiver burden over the 5 domains considered in the Caregiver Burden Inventory, shown as percentage values.
The mean BDI score was 11.37 (SD 7.88) (range 0–22), with no difference found between men and women (p = 0.996). The mean EQ-5D score was 0.39 (SD 0.30) (range 0–0.74) and the mean EQVAS score was 55.39 (SD 21.85) (range 20–100): these two indexes showed a positive relation, albeit not statistically significant (r = 0.429, p = 0.075). A mean Barthel Index score of 79.16 (SD 13.97) (range 47–100) was recorded. The mean score on the Mini-Mental State Examination was 26.68 (SD 2.05) (range 24–30), and it thus excluded the presence of cognitive disturbances among the patients.
Statistically significant correlations were found between the main study variables using Pearson’s correlation coefficients. The presence of depressive symptoms (BDI) in caregivers showed a strong positive correlation with the caregivers’ level of burden (CBI) (r = 0.978, p = 0.000), while BDI correlated negatively with the patients’ functional independence (BI) (r = –0.472, p = 0.041) and the patients’ quality of life (EQ-5D) (r = –0.775, p = 0.000).
Caregiver burden correlated negatively with patients’ functional independence measured by overall BI score (r = –0.444, p = 0.008) and with patients’ quality of life (EQ-5D) (r = –0.774, p = 0.000). A positive correlation was found between BI and EQ-5D (r = 0.660, p = 0.003).
The multiple regression analyses did not identify any factors predictive of caregiver burden, either for the single domains of the CBI or for the total CBI score.
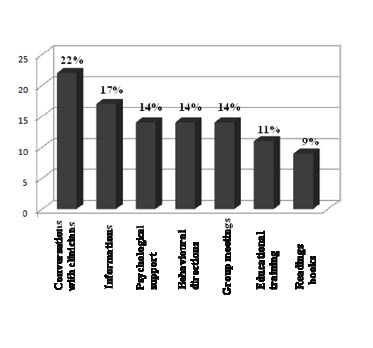
The SDQ revealed that 65.7% of caregivers wanted interventions to reduce their burden. As regards the interventions proposed, 22% wanted more conversations with clinicians; 17% asked to receive more information or pamphlets in order better to understand their relative’s condition; 14% wanted advice on how to behave in certain situations; 14% wanted opportunities to swap experiences with others as a means of psychological support; 14% asked to attend professionally-led group meetings; 11% wanted to take part in educational training; and 9% expressed an interest in receiving suggestions for further reading (e.g. books). No caregiver suggested any kind of intervention different from the ones proposed (Fig. 2).
Fig. 2. Proposed interventions aimed at reducing burden of care: caregivers’ preferences.
DISCUSSION
This study is a first attempt to describe the care burden and needs of those caring for individuals affected by chronic neurological diseases involved in community neurorehabilitation programmes. In agreement with other authors who have shown caring for a disabled relative to be a stressful and burdensome experience (9), we found that family members, particularly spouses/partners, often have to manage the care of these patients alone and experience high levels of burden and mild depressive symptoms. Indeed, in spite of evidence in the literature that suggests that the care of a family member affected by a chronic neurological condition profoundly affects and involves the entire family (24), our data seemed to show that most of the burden of care falls on the principal caregiver. Examining the different domains explored in the CBI, we found that the factors contributing most to caregiver burden were the amount of time devoted to caregiving, the patient’s dependence in activities of daily living and, hence, the caregiver’s lack of time for him- or herself. These findings are consistent with the results of previous studies conducted in different rehabilitation settings, which noted that the intensity of and the time spent on caregiving, together with the restrictions on the caregiver’s personal time, were the main variables related to caregiver burden (11, 25, 26). Caregivers also lament perceived lost opportunities and a curtailed social life, and complain of health problems, including sleep disorders and tiredness. Misunderstandings, arguments and resentment towards relatives over the care of the patient, as well as feelings of being ashamed of or embarrassed by the patient, seemed to account for a smaller part of the burden. Contrary to previous evidence of a higher level of burden in women (27), we did not find any statistical gender difference in caregiver burden. Although this finding could depend on the small group of male caregivers in our sample, other studies, too, have failed to find a gender effect on global measure of burden (28). Thus, the role of gender on perceived burden remains to be clarified.
As expected, the results of our study revealed a negative correlation between caregiver burden (CBI) and the functional independence of the patients (BI) and between caregiver burden (CBI) and patients’ quality of life (EQ-5D); conversely, caregiver burden (CBI) showed a strong and positive correlation with depression in caregivers (BDI).
In our sample, 65.7% of the caregivers expressed an interest in interventions aimed at reducing their burden: the data showed that, more than anything, they felt the need to obtain more clinical information. Given that all the patients in this study had a disease duration of at least 3 years, and thus had long been in regular contact with the medical profession, this finding underlines the importance of improving communication between physicians and patients. Future research should aim to identify what type of information is most wanted (i.e. about symptoms, treatments, rehabilitation interventions, prognosis or management of behavioural disorders). Qualitative SDQ data also highlighted the caregivers’ need for emotional support, both on an individual level and through group sessions. It must be also underlined that the caregiver’s level of involvement will be different in the different phases of the disease, depending on the changes in the patient’s needs; this suggests that the caregiver’s requirements, in terms of education and support, will change, as well. The need for appropriately timed interventions is consistent with the idea that caregivers will benefit more if they receive the right kind of support at the right time (29). In view of the complexity of demands arising from neurological illness and the fact that a global approach to neurorehabilitation is generally preferred, we, like other authors (30), argue that these interventions would be most useful when provided within a multidisciplinary framework in which the various professionals make their own specific contribution to the healthcare needs of patients and caregivers, but as part of an integrated approach.
Our study presents two main limitations. First, the results obtained, despite their consistency with data obtained in different rehabilitation settings (11, 25, 26), cannot be extended to caregivers of institutionalized patients. Secondly, due to the small size of the sample, we were not able to analyse data in relation to different pathologies. Further studies in larger populations should be designed to explore and highlight specific needs of caregivers, according to the diseases affecting their relatives. However, it should be noted that although the correlation between burden and disease depends on many different multidimensional factors, literature data suggest a strong link between burden and functional impairment (31), considering the last one as the main factor, transverse to different pathologies. Finally, the effect of other potentially significant variables on caregiver burden, such as depression in patients and the quality of life and health status of caregivers, must still be investigated.
In conclusion, the results of our study, highlighting the heavy burden borne by caregivers and drawing attention to their often unmet needs, may help to raise awareness within the healthcare community of the impact of chronic neurological diseases on patients’ families. They may also provide a useful resource for defining structured interventions geared at assessing, preventing or managing problems related to stressful caregiving situations across the care continuum. Indeed, although there is evidence that interventions targeting caregivers can decrease their levels of stress, depression and anxiety (32, 33), and increase their sense of being in control and their ability to cope with the burdensome experience of caregiving (34), the potential benefits of person-centred interventions require further evaluation (35). In particular, studies are needed to determine how best to support caregivers in each phase of the disease and which interventions are more effective. These studies should be conducted using empirically validated assessment tools and rigorous outcome measures, and should make provision for a long-term assessment, given that chronic neurological diseases are life-long conditions.
ACKNOWLEDGEMENTS
The authors thank Alberto Virgili, PT, for his technical support.
Conflicts of interest and funding: The authors have no conflict of interest or financial disclosures regarding the current manuscript.
REFERENCES