OBJECTIVE: The aim of this study was to compare the interstitial concentrations of pyruvate, lactate and glutamate in the trapezius muscle between patients with fibromyalgia syndrome and healthy controls.
DESIGN: Comparative cross-sectional study.
SUBJECTS: Patients with fibromyalgia (n = 19) and healthy controls (n = 19); all women.
METHODS: Subjects answered a questionnaire about different aspects of pain. Pressure pain thresholds over the trapezius and tibialis anterior muscles were determined. The interstitial concentrations of pyruvate, lactate and glutamate were determined in the resting trapezius muscle by the microdialysis technique, with samples collected every hour for 5 consecutive hours. Pain intensity was also rated.
RESULTS: Significantly higher interstitial concentrations of pyruvate and lactate were found in patients with fibromyalgia syndrome. The multivariate regression analyses of group membership and pressure pain thresholds of the trapezius confirmed the importance of pyruvate and lactate.
CONCLUSION: Different mechanisms that may increase pyruvate and lactate in patients with fibromyalgia syndrome are discussed. Improved understanding of peripheral muscle alterations in patients with fibromyalgia syndrome could lead to mechanism-based rehabilitation.
Key words: fibromyalgia; microdialysis; lactate; pyruvate; glutamate; trapezius muscle.
J Rehabil Med 2010; 42: 679–687
Correspondence address: Björn Gerdle, Rehabilitation Medicine, Department of Clinical and Experimental Medicine, Linköping University, SE-581 85 Linköping, Sweden. E-mail: Bjorn.gerdle@inr.liu.se
Submitted January 28, 2010; accepted April 14; 2010
INTRODUCTION
Fibromyalgia syndrome (FMS) affects approximately 2% of the population, with a 7 times higher prevalence among females (1). The currently used criteria of the American College of Rheumatology (2) include that the patient should have experienced at least 3 months of pain in all 4 body quadrants, together with spinal pain, and have at least 11 out of 18 painful standardized tender points. Such signs and symptoms indicate widespread hyperalgesia/allodynia. In addition to chronic pain, other symptoms are also common in FMS. Activities of daily living, quality of life, and the possibility of remaining at a previous level of employment are often affected negatively (1).
The aetiology of FMS is largely unknown. There seem to be different ways into FMS; for example, from local pain conditions, as consequences of certain infections, and due to severe stress. Some researchers suggest FMS is a complex hyperalgesic pain syndrome in which abnormalities of central sensory processing interact with peripheral pain generators and psychoneuroendocrine dysfunction to generate a wide spectrum of patient symptomatology and distress (3). Other authors emphasize the complex interplay between peripheral input and altered central processing in FMS (4).
Microdialysis can be used to analyse the interstitium of the muscle and its metabolic markers. We have used this technique in local/regional chronic pain conditions. In chronic severe work-related trapezius myalgia (CSTM) higher interstitial concentrations of lactate, pyruvate and glutamate were found in the trapezius compared with healthy controls (5). In contrast, chronic whiplash-associated disorders that also involved painful trapezius (WAD) had significantly lower concentration of pyruvate than controls, and with lactate it showed another time-pattern throughout the experiment (6–7). Based on these 2 studies it can be concluded that different metabolic alterations can be present in chronic local/regional pain conditions with involvement of a painful trapezius muscle. The question arises as to whether metabolic alterations exist in the aching trapezius muscle in a chronic widespread pain condition associated with central hyperexcitability and widespread hyperalgesia/allodynia (i.e. FMS). If such alterations are related to the chronic pain it is reasonable, according to a mechanism-based treatment strategy, to try to target these alterations in treatment and rehabilitation interventions. The trapezius muscle is generally affected clinically in FMS. Bengtsson reviewed the current knowledge of the muscle in FMS (8); biopsy studies of the trapezius muscle have shown mitochondrial disturbances (i.e. ragged-red fibres, moth-eaten fibres) in type-I muscle fibres, hypotrophy of type-II fibres, reduced capillarization, and greater thickness of the endothelium of the capillaries. Lowered tissue oxygenation and altered microcirculation have also been described (8). Voluntary muscle strength is reduced in FMS (8). Electromyographic (EMG) activity of the trapezius in supposed pauses of standardized dynamic work cycles is increased, indicating a relative inability of the muscle to relax (9).
Hence, we hypothesized, based on our previous research concerning local/regional pain conditions and the literature, that metabolic alterations exist in the trapezius muscle of female patients with FMS compared with healthy female controls (CON). Furthermore, that these alterations correlate more strongly with pressure pain thresholds (PPT) of the trapezius than with PPT of the tibialis anterior, i.e. indicating that the metabolic alterations are local and exert local effects.
To test this hypothesis, we compared the interstitial concentrations of lactate, pyruvate and glutamate in the trapezius muscle between patients with FMS who experience pain in the trapezius muscle and controls. In addition, we analysed whether the concentrations of these metabolites correlated with PPT of the trapezius and the tibialis anterior.
METHODS
Subjects
Nineteen female subjects with a clinical diagnosis of FMS, ranging in age between 25 and 55 years, were recruited for the study. They all had been patients at the Pain and Rehabilitation Centre of the University Hospital, Linköping, Sweden. They had had their persistent pain condition for a mean of 7.2 years (standard deviation (SD) 4.9).
Nineteen healthy female controls in the same age range were recruited through advertisement in the local newspaper. Some background and anthropometric data are given in Table I. Participants completed a brief questionnaire with questions regarding health, functional level regarding activities of daily living, experiences of pain, and how they coped with pain (Table I). A medical history, including any current or previous presence of pain or discomfort in the neck and shoulder region, was taken. Exclusion criteria in both groups included taking any kind of anti-coagulatory, anti-inflammatory, or steroidal medication.
All participants gave their informed written consent before the start of the study. The study was approved by the ethics committee of Linköping University (M88-04, addition 55-06).
| Table I. Background and anthropometric data, together with data from the questionnaire for the healthy controls (CON) and the fibromyalgia patients (FMS); mean and 1 standard deviation (SD) are given. Right-hand column shows the statistical comparison between the 2 groups (p-value) |
| Variables | CON (n = 19) | FMS (n = 19) | Statistics (p-value) |
| Age (years) | 41.9 (5.5) | 40.4 (5.4) | 0.391 |
| Height (cm) | 167.6 (7.3) | 166.2 (5.9) | 0.505 |
| Weight (kg) | 65.4 (10.9) | 76.7 (12.7) | 0.006* |
| Questionnaire |
| VAS neck (mm) | 2 (7) | 29 (20) | < 0.001* |
| ASI | 9.5 (7.3) | 17.6 (9.8) | 0.011* |
| PASS-20 | 22.8 (17.9) | 42.2 (16.5) | 0.003* |
| PCS | 8.6 (7.5) | 19.0 (10.8) | 0.002* |
| HADS-ANXIETY | 2.9 (2.2) | 6.9 (4.8) | 0.007* |
| HADS-DEPRESSION | 1.6 (2.4) | 7.6 (3.9) | < 0.001* |
| SE-PAIN | 85.0 (18.0) | 54.7 (47.0) | < 0.001* |
| SE-FUNCTION | 99.8 (0.6) | 76.8 (16.2) | < 0.001* |
| SE-SYMPTOM | 90.4 (9.0) | 57.9 (15.3) | < 0.001* |
| PDI | 11.2 (7.8) | 38.6 (10.0) | < 0.001* |
| QOL-S | 99.2 (11.4) | 72.5 (14.0) | 0.002* |
| *significant; VAS: visual analogue scale; ASI: Anxiety Sensitivity Index; PASS-20: Pain Anxiety Symptoms Scale-20; PCS: Pain Catastrophizing Scale; HADS-ANXIETY: Hospital Anxiety and Depression Scale – subscale anxiety; HADS-DEPRESSION: Hospital Anxiety and Depression Scale – subscale depression; SE-PAIN: The arthritis self-efficacy scale – subscale pain; SE-FUNCTION: Arthritis self-efficacy scale – subscale function; SE-SYMPTOM: Arthritis self-efficacy scale – subscale symptoms; PDI: Pain Disability Index; QOL-S: Quality of Life Scale. |
Questionnaire
The questionnaire included the following items and instruments (Swedish validated versions); for references concerning the different instruments including their psychometric properties (10–11).
Background data. Age and anthropometric data.
Habitual pain intensity rating. For the rating of habitual pain intensity in the neck, a visual analogue scale (VAS) was used; the scale was 100 mm long with defined end-points (“no pain” and “worst pain imaginable”), but without marks in between (results in cm). All the questions regarding pain concerned the previous 7 days.
Anxiety Sensitivity Index (ASI). A 16-item self-reported questionnaire. Each item asks about the amount of fear the participant experiences in regard to bodily sensations commonly associated with anxiety. Participants are asked to rate each item on a 5-point Likert-like scale, ranging from “very little (0)” to “very much (4)”. The ratings on the 16 items are summed for a total, ranging from 0 to 64. Studies have found support for test-retest reliability, criterion validity, and construct validity (e.g. support for the distinction between anxiety sensitivity and trait anxiety).
Pain Anxiety Symptoms Scale-20 (PASS-20). A short version of the 40-item PASS that measures fear and anxiety responses specific to pain. The PASS-20 has 4 5-item subscales that measure Avoidance, Fearful Thinking, Cognitive Anxiety, and Physiological Responses to Pain. Participants rate each item on a 6-point scale, ranging from “never (0)” to “always (5)”. Reliability analyses with PASS-20 indicate good internal consistency akin to the PASS-40. Psychometric analyses reveal good convergent, discriminant, predictive, and construct validity.
Pain Catastrophizing Scale (PCS). A 13-item self-report measure designed to assess catastrophic thoughts or feelings accompanying the experience of pain. Respondents are asked to reflect on past painful experiences and to indicate the degree to which each of the 13 thoughts or feelings are experienced when in pain. The questionnaire uses a 5-point scale ranging from “0 (not at all)” to “4 (all the time)”. Subscales for rumination, magnification, and helplessness plus a total score are added up. In this study, we used the total score.
Hospital Anxiety and Depression Scale (HADS). A self-rating scale in which the severity of anxiety and depression is rated on a 4-point scale. Seven questions are related to anxiety (HADS-ANXIETY) and 7 to depression (HADS-DEPRESSION), both with a score range of 0–21. A score of 7 or less indicates a non-case, a score of 8–10 a doubtful case, and 11 or more a definite case. The instrument is widely used in clinical practice and research. In this study, we used both subscales. Investigations have shown that the HADS is a psychometrically sound instrument.
The arthritis self-efficacy scale (SE). A standardized questionnaire with 20 items that measure an individual’s perceived self-efficacy to cope with the consequences of chronic arthritis. In this study, a validated Swedish version for chronic pain was used. The only modification made was to change the words “arthritis pain” and “arthritis” to “pain”. The first 5-item subscale assesses self-efficacy perception for controlling pain (SE-PAIN). The second 9-item subscale assesses self-efficacy for performing functions in daily living (SE-FUNCTION). The 6-item subscale measures self-efficacy for controlling other symptoms related to chronic pain (SE-SYMPTOM). Each question is followed by a scale for marking the answer from 10 to 100. Each subscale is scored separately by taking the mean of the subscale items.
Pain Disability Index (PDI). A 7-item self-report instrument based on a 10-point scale that assesses perception of the specific impact of pain on disability that may preclude normal or desired performance of a wide range of functions, such as family and social activities, sex, work, life-support (sleeping, breathing, eating), and daily living activities. The PDI has shown good reliability and validity in several studies.
Quality of Life Scale (QOLS-S). This comprises 16 items that together describe the quality of life concept: (i) Material comforts; (ii) Health; (iii) Relationships with parents, siblings and other relatives; (iv) Having and rearing children; (v) Close relationships with spouse or significant others; (vi) Close friends; (vii) Helping and encouraging others, participating in organizations, volunteering; (viii) Participating in political organizations or public affairs; (ix) Learning; (x) Understanding yourself; (xi) Work; (xii) Expressing yourself creatively; (xiii) Socializing; (xiv) Reading, music or watching entertainment; (xv) Participating in active recreation; and (xvi) Independence, being able to do things for yourself. A 7-point satisfaction scale is used. Clients estimated their satisfaction with their current situation. A higher total score shows higher satisfaction. The item scores are added to a total score, ranging from 16 to 112.
Clinical examination
The trapezius muscles, the supraspinatus muscles, the extensor muscles of the neck, and the muscles of the upper arms were examined regarding tightness, range of motion, and tenderness. The 18 tender points according to the fibromyalgia classification criteria of American College of Rheumatology (ACR) 1990 (2) were clinically examined for sensitivity to pressure.
Algometry
Algometry was performed using an electronic pressure algometer (Somedic, Hörby, Sweden) as previously described (6) and was done as a part of the clinical examination approximately one week before the microdialysis. The diameter of the contact area was 10 mm and the pressure was applied perpendicularly to the skin at a speed of 30 kPa/s. The subjects were instructed to mark the PPT by pressing a signal button as the sensation of “pressure” changed to “pain”. Algometry was performed bilaterally over the medial, middle and lateral part of the descending part of the trapezius muscle, and over the tibialis anterior to determine the PPT. All PPT measurements were conducted twice in approximately 5 min intervals. The PPT values presented in Table II are the mean of these 2 measurements of lateral, middle and medial site on the right and left trapezius muscle and of right and left tibialis anterior muscles, respectively. In the regression analyses the mean values of the right and left trapezius were used.
| Table II. Pressure pain threshold (mean and 1 standard deviation (SD)) of trapezius and tibialis anterior in healthy controls (CON) and fibromyalgia patients (FMS). Right-hand column shows the result of the statistical comparison between the 2 groups (p-value) |
| Variables | CON (n = 19) Mean (SD) | FMS (n = 19) Mean (SD) | Statistics (p-value) |
| PPT of trapezius (kPa) |
| Trapezius left lateral | 400 (139) | 98 (50) | < 0.001* |
| Trapezius left middle | 339 (125) | 104 (42) | < 0.001* |
| Trapezius left medial | 342 (124) | 109 (63) | < 0.001* |
| Trapezius right lateral | 329 (125) | 88 (42) | < 0.001* |
| Trapezius right middle | 309 (79) | 92 (41) | < 0.001* |
| Trapezius right medial | 388 (114) | 95 (52) | < 0.001* |
| PPT of tibialis anterior (kPa) |
| Tibialis anterior left | 495 (155) | 156 (71) | < 0.001* |
| Tibialis anterior right | 505 (153) | 164 (96) | < 0.001* |
*Significant group difference; PPT: pressure pain threshold.
Microdialysis of the trapezius
Microdialysis mimics the function of a capillary blood vessel by perfusing a thin dialysis tube implanted in the tissue with a physiological saline solution. Substances can pass, by simple diffusion, across the dialysis membrane along the concentration gradient. The dialysate is analysed chemically and reflects the composition of the extracellular fluid. Microdialysis allows for continuous sampling of compounds in the muscle interstitial space, where nociceptor-free nerve endings terminate, and in close proximity to the muscle fibres, providing accurate information on local biochemical changes before such compounds are diluted and cleared by the circulatory system.
The participants were asked not to use any medications except for paracetamol preparations for 3 days before the experimental day, and not to perform any strenuous exercise for 2 days before the study. They were also instructed not to drink any caffeine-containing beverages on the day of the study, as well as not to smoke, and avoid non-steroidal anti-inflammatory (NSAID)-medication the week before the study. The participants arrived at the clinic in the morning after having eaten breakfast. A brief interview was then carried out by one of the physicians (BG or BL) checking that the instructions with respect to the different instructions had been followed. All subjects reported that they had followed the instructions. During the study, they were not allowed to eat, but they could drink water.
The descending (upper) part of the trapezius muscle on the dominant side was investigated. Using the surface electro myography for the non-invasive assessment of muscles (SENIAM) landmarks the midpoint of the line between the spine of 7th cervical vertebra and the acromion was defined as the midpoint of the descending trapezius. The skin overlying the midpoint of the muscle, as well as the point 2 cm laterally of the midpoint, were marked and examined using ultrasonography to measure and visualize the underlying muscle and surrounding structures. To monitor the subjects during the invasive procedures, the pulse and oxygenation were measured on a finger with a pulse oximeter, and as a safety precaution an intravenous cannula was placed in either the arm or the hand. Two catheters (CMA 60; CMA Microdialysis AB, Solna, Sweden) were inserted (parallel with 1 cm inter-catheter distance) 2 cm laterally of the midpoint of the transverse part of the trapezius muscle depending on the size of the muscle so the membrane of each catheter was in the middle of the trapezius muscle. Typically, a brief involuntary contraction and change of resistance were perceived when the tip of the insertion needle of the catheter entered the fascia and muscle. The catheter was placed toward the vertebrae and lengthwise in the muscle. Before the catheter insertion, the skin and subcutaneous tissue were anaesthetized with a local injection (0.2–0.5 ml) of xylocaine (20 mg/ml) without adrenaline, and care was taken not to anaesthetize the underlying muscle. After the catheter placement in the trapezius, a pump (CMA 107) was connected to the catheter and the system was perfused with perfusion fluid T1 (CMA, Microdialysis AB). The perfusion velocity was set to 0.3 µl/min (generating 100% recovery) (12). The first 2 h were considered as a trauma phase and therefore not included in the analyses (7).
The microvials collecting the dialysate were changed once every 60 min. At the same time the subjects were asked to rate the pain intensity of the trapezius of the dominant side using a visual analogue scale (VAS; ranging from 0 mm (no pain) to 100 mm (worst possible pain)). The vials were then placed in a freezer at a temperature of –20°C. Dialysate was collected for 7 h while the participants had to lie or sit still and not perform any physical activity; a research nurse regularly checked that this instruction was followed.
After approximately one week, the dialysate was thawed, centrifuged and analysed for the concentrations of pyruvate, lactate and glutamate (abbreviated as [pyruvate], [lactate] and [glutamate]) with the CMA 600 Microdialysis Analyser (CMA Microdialysis; standard range). In the FMS group the dialysate from one of the catheters (chosen in random order) was used for analyses of the metabolites (dialysate from the other catheter was used for other analyses; not presented here), while in CON the mean value of the concentrations of the 2 catheters at each time-point was used. The CMA 600 detection intervals are as follows: 0.1–12 mmol l–1 for lactate, 10–1500 µmol l–1 for pyruvate and 1.0–150 µmol l–1 for glutamate. Concentrations below the level of detection were replaced with a value corresponding to the lower level of detection and divided by 2 (13). For values over the level of detection, the upper limit of detection was used. For lactate, 3 (1.6%) out of 190 samples had a value lower than the lower detection level; corresponding values for both pyruvate and glutamate were 1 (0.5%) out of 190 samples. For glutamate, 3 (1.6%) out of 190 samples had a value higher than the upper detection level.
Statistics
Statistical analyses were made using SPSS (version 15.0; SPSS Inc, Chicago, USA) and SIMCA-P+ (version 11.0; Umetrics Inc, Umeå, Sweden) and p ≤ 0.05 was used as level of significance in all analyses. Data are presented as mean 1 SD. The samples of dialysate from the 2 initial h (i.e. trauma phase) were not used in the statistical analyses. For comparisons between groups concerning background data and data from the questionnaire, Student's t-test (for un-paired comparisons) was used. For general analyses of the microdialysis data (i.e. concentrations of lactate, pyruvate and glutamate) at the different time-points repeated measures analysis of variance ANOVA (mixed-model factorial ANOVA) was used. We also determined the area under the curve (AUC) for the concentrations of the 3 metabolites. This was used as a comprehensive measure of the concentration of the metabolite throughout the test. The AUC variables were compared with respect to group belonging using Student’s t-test (for un-paired comparisons). For bivariate correlation analysis Pearson’s correlation was used.
When investigating the correlations between the concentrations of lactate, pyruvate and glutamate and pain intensities, PPT and group membership, principal component analysis (PCA) and partial least squares or projection to latent structures (PLS) were applied (14). PCA using SIMCA-P+ was used to extract and display systematic variation in a data matrix. A cross-validation technique was used to identify non-trivial components (p). Variables loading upon the same component are correlated and variables with high loadings, but with different signs are negatively correlated. Variables with absolute loadings ≥ 0.20 and that had a 95% confidence interval not equal to zero were considered significant. Significant variables with high loadings (positive or negative) are more important for the component under consideration than variables with lower absolute loadings (14). The obtained components are per definition not correlated and are arranged in decreasing order with respect to explained variation. R2 describes the goodness of fit – the fraction of sum of squares of all the variables explained by a principal component (14). Q2 describes the goodness of prediction – the fraction of the total variation of the variables that can be predicted by a principal component using cross-validation methods (14). Outliers were identified using the 2 powerful methods available in SIMCA-P+: (i) score plots in combination with Hotelling’s T2 (identifies strong outliers) and (ii) distance to model in X-space (identifies moderate outliers).
Partial least squares or projection to latent structures was used for the multivariate regression analysis of PPT, pain intensity (VAS), and group membership (CON or FMS; i.e. PLS-discriminant analysis; PLS-DA) using the interstitial concentrations (AUC) of the 3 metabolites (14). The variable influence on projection (VIP) indicates the relevance of each X-variable pooled over all dimensions and Y-variables – the group of variables that best explain Y. VIP ≥ .8 was considered significant. Coefficients (PLS scaled and centred regression coefficients) were used to note the direction of the relationship (positive or negative). Multiple linear regression (MLR) could have been an alternative when regressing pain intensity and PPT, but it assumes that the regressor (X) variables are independent. If such multi-collinearity occurs among the X-variables, the regression coefficients become unstable and their interpretability breaks down. MLR also assumes that a high subject-to-variables ratio is present (e.g. > 5) and such requirements are not required for PLS. PLS, in contrast to MLR, can handle several Y-variables simultaneously.
RESULTS
Questionnaire and clinical examination
According to the questionnaire answered in connection with the clinical examination, the habitual pain intensity of the neck, as expected, was significantly higher in FMS than in CON (Table I). FMS also showed significantly more other symptoms (e.g. depressive symptoms, aspects of anxiety, catastrophizing), more negative consequences (i.e. PDI, SE) and perceived quality of life lower than CON (Table I).
The clinical examination revealed significantly higher number of tender points in FMS than in CON (11.5 (1.5) vs. 0.2 (0.5); p < 0.001). FMS also had significantly lower PPT than CON, both in the upper and lower parts of the body (Table II).
Pain intensity throughout the microdialysis experiment
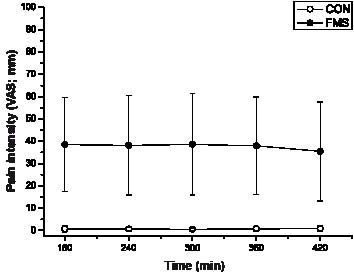
A significant difference in pain intensity of the trapezius existed between FMS and CON throughout the experiment (after the trauma phase), both at every hour after the trauma phase (i.e. the initial 2 h were not included in the biochemical analyses presented below) and for the area under the pain intensity curve (both p < 0.001). The pain intensity in FMS was relatively constant throughout the experiment (Fig. 1).
Fig. 1. Pain intensity ratings (mean and 1 standard deviation) at the different time-points (the trauma phase (0–2 h) excluded) in healthy subjects (CON) and in patients with fibromyalgia (FMS). See text for statistics.
Interstitial concentrations of metabolites
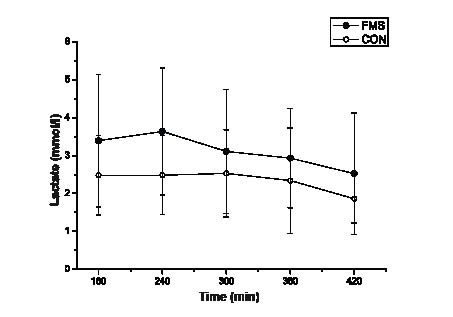
Lactate
There was a significant group effect (p = 0.039) with higher interstitial lactate concentrations in FMS compared with CON (Fig. 2a). Also, lactate AUC showed a significant group difference, with significantly higher concentration in FMS (758 (319) vs. CON: 571 (227) (mmol/l × min); p = 0.046). There was a significant effect of time (p = 0.001).
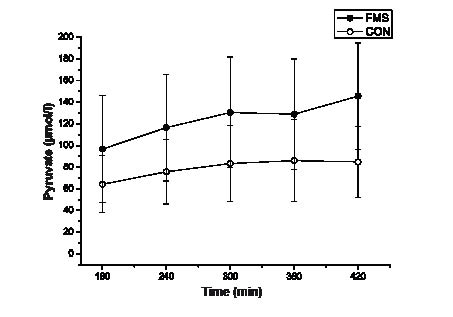
Pyruvate
There was a highly significant difference in interstitial concentration of pyruvate (p < 0.001) between the 2 groups; the concentrations were higher among the FMS patients (Fig. 2b). This group difference was confirmed using the AUC variable of pyruvate (FMS: 29812 (9945) vs. CON: 19167 (7469) (µmol/l × min); p = 0.001). There was a significant effect of time (p < 0.001); i.e. an increase during the experiment.
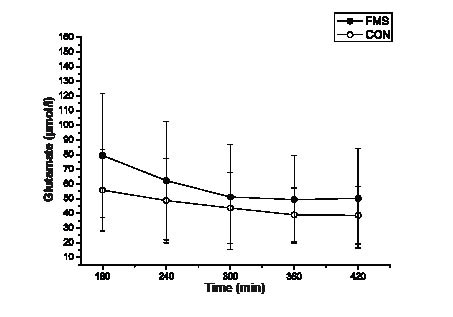
Glutamate
There was no significant difference in interstitial glutamate (p = 0.118) or in glutamate AUC (FMS: 13645 (7218) vs. CON: 10710 (4949) (µmol/l × min); p = 0.152) between FMS and CON (Fig. 2c). There was a significant effect of time (decrease; p < 0.001).
Fig. 2. Interstitial concentrations (mean and 1 standard deviation) of (a) lactate, (b) pyruvate and (c) glutamate at the different time-points (the trauma phase (0–2 h) excluded) in healthy subjects (CON) and in patients with fibromyalgia (FMS). See text for statistics.
Correlations between the 3 substances
The AUC values of the 3 substances intercorrelated positively in the 2 groups of subjects taken together (r = 0.42–0.69; p: 0.009 – < 0.001). A very similar pattern was found in FMS (r = 0.56–0.78; p: 0.013 – < 0.001) even though the correlation between AUCs of pyruvate and glutamate did not reach significance (r = 0.44; p = 0.059). The correlations were lower and non-significant in CON (r = 0.20–041; p = 0.08–0.42).
Multivariate analyses
Regressions of group membership and pain intensity.
Using the AUC variables of the 3 metabolites as regressors, it was possible to significantly regress group membership (FMS (denoted 1) or CON (denoted 0)) (R2 = 0.23, Q2 = 0.20). Hence, this analysis confirmed that the FMS generally had higher levels of pyruvate and lactate. The metabolites had the following importance in descending order: pyruvate AUC (VIP = 1.38), lactate AUC (VIP = 0.85) and glutamate AUC (VIP = 0.62).
In all subjects taken together it was possible to regress pain AUC (R2 = 0.16, Q2 = 0.10); the metabolites had the following importance in descending order: pyruvate AUC (VIP = 1.23), glutamate AUC (VIP = 0.89) and lactate AUC (VIP = 0.84). It was not possible to regress pain AUC for only FMS.
Regression of pressure pain thresholds
Pressure pain threshold of trapezius. For both groups taken together it was possible to significantly regress PPTs of the trapezius (i.e. 2 Y-variables) even though explained variance was low (R2 = 0.12, Q2 = 0.05). The metabolites had the following importance in descending order: pyruvate AUC (VIP = 1.51), glutamate AUC (VIP = 0.65) and lactate AUC (VIP = 0.52). Negative correlations existed between the 3 metabolites and PPTs of the trapezius. Thus, the concentration of pyruvate had the greatest importance for PPT of trapezius.
We also regressed PPT of trapezius separately for the 2 groups.
The significant model in CON (R2 = 0.49, Q2 = 0.18) had the 3 metabolites in the following descending order: lactate AUC (VIP = 1.45), glutamate AUC (VIP = 0.67) and pyruvate AUC (VIP = 0.66). Lactate showed a positive correlation with PPTs of the trapezius in CON.
In FMS lactate AUC tended (the model was not significant) to correlate negatively with PPT of the trapezius according to the model obtained (R2 = 0.35, Q2 = –0.19). The 3 metabolites had the following importance in FMS (in descending order): lactate AUC (VIP = 1.31), pyruvate AUC (VIP = 1.14) and glutamate AUC (VIP = 0.01). Lactate showed a negative (non-significant) correlation with PPTs of the trapezius in FMS, while the pyruvate had a positive (non-significant) correlation.
Pressure pain threshold of tibialis anterior
It was not possible to regress PPT of the tibialis anterior (i.e. 2 Y-variables) using AUC of the 3 metabolites as regressors in all subjects taken together (i.e. a non-significant model, R2 = 0.06, Q2 = –0.04).
DISCUSSION
Significantly higher interstitial concentrations of pyruvate and lactate were found in the resting trapezius muscle in FMS patients than in CON subjects. The multivariate analyses showed that especially the interstitial concentration of pyruvate correlated with PPT of trapezius.
Habitual situation
The different instruments of the questionnaire confirmed earlier reports that FMS perceive their situation very negatively from several point of views when compared with healthy subjects (Table I) (1, 15).
Pyruvate and lactate
As in a laboratory study of CSTM, we found significantly and markedly increased [pyruvate] compared with controls (5). Similar results were also found in a field study during a working day of occupationally active women with trapezius myalgia (16). Flodgren et al. reported significant increases in [pyruvate] during brief laboratory work in patients with trapezius myalgia (17). In contrast, WAD showed significantly lower [pyruvate] and another time pattern than in controls (6). These results taken together indicate that CSTM, WAD and FMS are associated with different alterations in pyruvate metabolism compared with healthy pain-free subjects.
One possible explanation for the higher [pyruvate] in FMS of the present study is changes in the lactate-pyruvate metabolism via lactate dehydrogenase isoforms (18). Another alternative is that a reduction in tissue oxygenation in FMS (8) may result in higher [pyruvate] due to a shift towards an anaerobic state. Such a circumstance might also cause the significantly higher [lactate]. Fitness level, including the capacity of the neck and shoulder muscles, was not investigated, although higher body weight in FMS (Table I) may indicate a difference in fitness and, thereby, a more frequent reliance on anaerobic metabolism in FMS (19).
The aerobic capacity of the muscle is largely governed by the number of mitochondria and their enzymes (20). Lindh et al. reported lower capillary density and enzymes associated with aerobic metabolism in FMS (21); however, it is unknown if a general deconditioning in FMS involves the postural trapezius. The mitochondrial density increases as result of exercise (see (22) for references) and affects the level of metabolites (i.e. enhanced aerobic capacity). In patients with mitochondrial myopathies, a reduced muscle function is evident (22). Moreover, both trapezius of CSTM and FMS have muscle fibres with different types of alterations in mitochondrial content, such as moth-eaten fibres and ragged red-fibres (8, 23–25); changes that indicate uneven distribution and proliferation of mitochondria (8). This study was conducted during rest, but it cannot be excluded that there was an increased muscle activity in FMS when changing and correcting body positions due to hyperalgesia/allodynia during the rest in the laboratory. A higher EMG activity during supposed pauses between muscle contractions in FMS have been reported (9).
We noted a significantly higher concentration of lactate in FMS, although the difference not was as prominent as for pyruvate. The roles of lactate are complex. Lactate may assist in the detection of exercise stress before tissue damage occurs (18) and can be exchanged rapidly among tissue compartments where it may be oxidized as a fuel or reconverted to form pyruvate or glucose (18, 26–28). Lactate is also involved in peripheral nociception, and it appears to facilitate the response of acid-sensing ion channel 3 (ASIC-3) to low pH (26). Such ASIC channels are considered as molecular transducers for nociception and mechanosensation (26). In all subjects taken together we did not confirm such a role for interstitial concentration of lactate in the multivariate regressions of PPT. However, separate analyses of the 2 groups indicated opposite roles of lactate with respect to PPT in the 2 groups, and thereby a role in mechanosensation.
Our results concerning [lactate] are not in agreement with the results of McIver and colleagues (29). They found no difference in [lactate] between FMS and controls in the vastus lateralis during rest (29). However, on other hand, our results are in consensus with our earlier study of CSTM, which reported significantly higher [lactate] in trapezius than controls but with overall identical blood flow (5). In the field study of female workers with and without chronic trapezius myalgia, we found no significant difference in [lactate] throughout the working day, but significantly higher blood flow in myalgia (16). These subjects with trapezius myalgia were reasonably better with the respect to their pain condition than CSTM and the present FMS, which might explain the lack of difference in [lactate].
Muscle [lactate] increases with exercise intensity (7, 16–17, 30). Increased [lactate] can indicate tissue hypoxia, e.g. experiments with myocutaneous flaps reported that muscle [lactate] increases due to ischaemia (31). Alterations in the control of muscle blood flow have been reported in FMS (32–34). Blood flow in vastus lateralis of FMS decreased during 3 h resting and a poor circulatory control was suggested (29). Although both present groups were resting in a laboratory, it cannot be ruled out that the subjects perceived stress. It has been reported that FMS has abnormal cardiovascular responses to low-grade mental stress (35). Several studies indicate altered sympathetic activation in FMS (36–39), which in turn may affect [lactate] (40). Sympathetic activation may also cause decreased blood flow even without hypoxia (26, 41).
To summarize, a lower fitness level, a reduced tissue oxygenation, increased muscle activation and/or dysfunctional state of the mitochondria might explain our results of increases in [pyruvate] and [lactate] in the trapezius of patients with FMS.
Glutamate
Glutamate is a pain mediator and an excitatory neurotransmitter that acts on N-metyl-D-aspartate receptors in the CNS (42) and influences peripheral pain processing (43–44). Data exist that link glutamate to peripheral pain processing (45–49), muscle inflammation (50), delayed onset muscle soreness (51) and painful tendon (52). A recent review concluded that elevation of interstitial glutamate in skeletal muscle alter pain sensitivity in healthy humans and is associated with pain symptoms in some chronic non-inflammatory muscle pain conditions (53); probably mediated through activation of peripheral excitatory amino acid receptors located on the terminal endings of nociceptors. Our group have reported elevated [glutamate] of the trapezius, both in the study of CSTM and in women with chronic work-related trapezius myalgia who were still occupationally active (5, 16). On the other hand, the present study of FMS and a recent study of chronic WAD have not found significant increases in [glutamate] (6). Flodgren et al. reported no difference in [glutamate] between subjects with chronic muscle pain and healthy subjects (54). However, their definition of the patient group was vague and the relative recovery was not controlled for, 2 considerations that might have influenced and biased the results and conclusions.
General methodological considerations
[Pyruvate] increased throughout the experiment despite the resting situation. In earlier laboratory studies of trapezius myalgia and WAD (but not in controls), changes were found in [pyruvate] as a consequence of brief work (5–6, 55), while in our field study no effect of time was noted (16). The increasing [pyruvate] over time in both our groups may be related to the fasting during the experiment. On the other hand, both [glutamate] and [lactate] showed other time-dependencies. We noted that [glutamate] did not reach a steady state until 4 h after insertion of the catheter, and that the differences between the groups lessened over time. In this study and in another study (5), it has been assumed that the trauma phase lasts for ≤ 2 h based on reports that [glutamate] stabilized 1–2 h after catheter insertion (51, 54). An alternative explanation is that the tissue in FMS is more sensitive to minor tissue trauma than in CON. Moreover, the influence of food intake and fasting as well as diurnal fluctuations of the metabolites should be investigated in future studies.
When encountering values below the level of detection, it was substituted by the lower level of detection and divided by 2. When above the level of detection, the upper level of detection was chosen. This may have made the difference between the groups smaller or larger than it actually was. Unfortunately, several months passed between the time of the chemical analyses and the scrutinizing of the results, i.e. it was not possible to reanalyse the samples due to lack of analyte stability for this period. However, the number of samples with such problems was low.
Relevance for rehabilitation of patients with fibromylagia syndrome
It is important to understand the role of the periphery for maintenance of pain in FMS when designing treatment and rehabilitation. Microdialysis offers a relatively new possibility to investigate concentrations of metabolic and algesic substances in muscle tissue and their relevance for aspects of pain in FMS and in other chronic pain conditions. Our results indicate, in agreement with studies in the literature based on other techniques (see (8) for references), peripheral alterations that might contribute to a maintenance of nociceptive processes in the central nervous system (CNS) and perception of pain. However, in future studies of FMS it is also important to investigate the interstitial concentrations of “classic” algesic substances, such as serotonin (5-HT), cytokines, substance P, bradykinin, kallidin, nerve growth factor (NGF) and calcitonin gene-related peptide (CGRP). Some of these (i.e. 5-HT, IL-6 and kallidin) have been significantly increased in chronic local/regional pain conditions (13, 16, 56). Also, it is important to investigate the concentrations of anti-nociceptive substances (e.g. endogenous opioids and endocannabionoids) in order to understand if the balance between pro- and anti-nociceptive substances around the nociceptors is altered in the myalgic muscle of FMS.
Hence, a detailed knowledge of alterations in metabolic and pro- and anti-nociceptive substances and how they relate to the chronic pain can, according to a mechanism-based treatment strategy, increase the possibility to design effective rehabilitation interventions.
In conclusion, there was a significantly higher interstitial concentration of pyruvate and lactate in FMS compared with CON. Multivariate analyses confirmed the importance of pyruvate and lactate. These metabolic alterations correlated more strongly with PPT of the trapezius than with PPT of the tibialis anterior. Different mechanisms might increase [pyruvate] and [lactate] in FMS. Improved understanding of peripheral muscle alterations and their relevance for aspects of pain in FMS may lead to mechanism-based rehabilitative and other interventions and, it is hoped, to better outcomes.
ACKNOWLEDGEMENTS
This study was supported by the Swedish Council for Working Life and Social Research (2007–0760).
The authors declare no conflicts of interest.
REFERENCES