OBJECTIVE: To describe pain and recovery of physical functioning after total knee arthroplasty.
DESIGN: A longitudinal design with assessments preoperatively, and 1 week, 3 and 9 months postoperatively.
SUBJECTS: Sixty-three patients participated.
METHODS: Pain was assessed by visual analogue scale. Physical functioning was measured by 40-metre timed walking, timed stair-climbing and goniometry. At 9 months the Short Form-36 pain and physical function scales were added to make comparisons with the general population.
RESULTS: Pain score one week after surgery was 40 (standard deviation (SD) 23) vs 24 (SD 19) at 3 months (p < 0.001). At 9 months the pain score was 22 (SD 23) vs 49 (SD 18) preoperatively (p < 0.001). Knee extension did not differ from preoperative scores, but knee flexion reduced from 124 (SD 13) to 112 (SD 12) (p < 0.001). Forty-metre walking time improved from 37 s (SD 13) to 34 s (SD 11) (p < 0.001), while the number of patients able to climb stairs was unchanged (p > 0.05). The patients’ Short-Form 36 pain score did not differ from the general population, while the physical function score was 60 (SD 24) vs 75 (SD 24) (p < 0.001).
CONCLUSION: Early pain reduction was registered. At 9 months, pain was equal to that in the general population, but a considerable number of patients still had problems in performing strenuous activities.
Key words: total knee arthroplasty; recovery; clinical course; physical functioning; pain; general population.
J Rehabil Med 2010; 42: 614–619
Correspondence address: Kristi Elisabeth Heiberg, Department of Nursing and Health Sciences, Institute of Health and Society, University of Oslo, PO Box 1153 Blindern, NO-0318 Oslo, Norway. E-mail: k.e.heiberg@medisin.uio.no
Submitted July 1, 2009; accepted March 10, 2010
INTRODUCTION
Osteoarthritis (OA) of the knee often leads to pain and impaired physical functioning (1–6). Total knee arthroplasty (TKA) is the treatment of choice when other conservative therapeutic approaches have failed (7). Undergoing TKA implies a long period of rehabilitation. During their hospital stay, patients perform exercises from the first postoperative day. After discharge from hospital, most Norwegian patients with TKA continue their rehabilitation for several months in rehabilitation centres or in outpatient physiotherapy clinics. For the field of rehabilitation, knowledge of how much and when recovery can be expected is of interest.
The results of previous studies indicate that considerable pain reduction is obtained within the first months postoperatively (1, 8–12), with the greatest improvement between 3 and 6 months after surgery (13). In the recovery of physical functioning, however, the results are less clear. In general, self-report assessments showed that patients seemed to be rather satisfied with their early recovery 2–3 months after surgery (1, 8–10, 14). Performance-based measures indicated an improvement in timed ambulation within the first 6 months (3, 15), but in other studies impaired physical function was reported both early (5, 11) and up to one year postoperatively (16). In the referred studies, the assessments were performed preoperatively and at few, but different, time-points within the first year after surgery. In order to examine both course and outcome of recovery, we assessed pain and physical functioning at several time-points, including assessments before surgery, and 1 week, 3 and 9 months postoperatively.
Performance-based measures of physical functioning including assessments of knee flexion and extension, muscle control, strength and ambulation attach closely to aims of exercise, and self-reports mirror the patients’ own evaluation of their abilities and satisfaction with performing physical activities. An observed and measured performance may differ from self-report of physical functioning. Furthermore, the performance-based measures and the items in questionnaires often assess different issues. As an example, the performance-based measures evaluate timed walking indoors over a short distance (11), while self-reports assess the ability to walk long distances exceeding 2 km outdoors (4, 8). Thus, the different demands put on the patient may explain the diversity in conclusions related to the recovery of, for example, walking ability after TKA. In order to obtain a broader picture of the recovery during the first postoperative months, both performance-based and self-report measures were included in the present study.
Most studies evaluate outcomes in pain and physical functioning by comparing them with preoperative measures (2, 5, 7–8, 10–11, 13–14). This can be relevant for pain evaluation. However, with respect to physical functioning the patients undergoing TKA often have great limitations at the time of surgery. In anticipating a successful recovery from TKA, it could be relevant to expect physical functioning to recover beyond the preoperative state and possibly approach a premorbid state (17). An individual’s premorbid measures, however, are not likely to be available. Alternatively, the patients’ outcomes can be compared with comparable groups in the general population. The results of prior studies indicate that patients may have more limitations in performing strenuous activities than their peers (16–20). Thus, additionally at 9 months, pain and physical function scales from generic health-related quality of life Short Form-36 (SF-36) were used and the scores compared with those of the general population.
The aims of this study were two-fold: primarily, to describe the postoperative course of recovery in pain and physical functioning during a period of 9 months after TKA by including postoperative assessments at 1 week, 3 and 9 months; secondly, to compare the patients’ outcomes of pain and physical functioning at 9 months postoperatively with their preoperative scores and with data from the Norwegian general population in the same age-group.
METHODS
Design and ethics
Originally, the patients participated in a randomized, controlled trial where the effect of continuous passive motion (CPM) was investigated during the first week after surgery (11). No differences were found between the groups, and therefore the data from the total group was used in a follow-up study. The longitudinal observational study comprised assessments before surgery (baseline), and at 1 week, 3 and 9 months after TKA. Two experienced physiotherapists blinded to previous scores performed the performance-based measures. In addition, at 9 months self-reported pain and physical functioning were assessed and compared with data from the Norwegian “Level of Living 2002” survey of the general population (21). The study was approved by the Regional Committee for Medical Research Ethics and the Norwegian Social Sciences Data Inspectorate.
Recruitment and inclusion
During a period of 15 months all patients admitted to an orthopaedic ward for elective primary TKA were considered as potential participants in the study. Written information about the study with an invitation to participate was sent to the subjects’ home address before hospitalization. On the day of admission the patients were asked again if they wanted to participate, and their written consent was obtained. Only 5 of 72 patients declined the invitation. Those willing and fulfilling the criteria were enrolled consecutively. The inclusion criteria were primary knee OA. OA of the knee was diagnosed by the orthopaedic surgeon after the following criteria: knee pain, osteophytes seen on X-ray and one of the following: age above 50 years, stiffness for less than 30 min, and/or crepitus (22). Patients with rheumatoid arthritis, ankylosing spondylitis, impaired cognitive function, known substance abuse and/or little knowledge of spoken and written Norwegian language were excluded.
Total knee replacement and rehabilitation
All patients received the knee prosthesis type LCS (DePuy, Leeds, UK) with rotating platform without patellar component. The average length of hospital stay was one week. During the hospital stay one patient had deep vein thrombosis, while 18 patients had other minor complications, such as reduced haemoglobin, urinary infection, nausea and pneumonia.
While in hospital, all participants received daily physiotherapy with exercises for approximately 30 min, consisting of strengthening and mobility exercises, transfer and gait training with an assistive device. They were instructed to perform exercises 2–3 times a day. Progression was made according to the tolerance of the patients. After discharge from hospital, the patients participated in at least 12 individualized physiotherapy sessions twice a week, consisting mainly of strengthening and mobility exercises, gait training and education in walking. The intensity, frequency, progression and duration of the supervised training were individually adjusted to each patient.
Performance-based measures
Ambulation was measured by timed walking 40 m on flat floor at a rapid and safe speed. The patients were allowed to use walking aids if necessary. The timed stair-climbing test comprised walking up and down a flight of stairs consisting of 8 steps with a height of 16 cm, using alternate legs, with no support from a rail or walking aid. Those who were unable to perform the stair-climbing test according to the protocol were classified as unable to climb stairs.
Knee flexion and extension was measured with a 1-degree-increment goniometer measuring degrees. The patient lay in a supine position on a bench (23). Active knee flexion was measured with the hip in a position of 90º of flexion and the knee actively bent to maximal flexion. Active extension was measured with the ankle resting on a bolster, and the knee was actively extended to its maximal range (23). To obtain the best possible reliability, the physiotherapists rehearsed the procedure beforehand by measuring 10 persons at 2 different times. Discrepancies in measurements between the 2 physiotherapists and between the measurement times were discussed, and the procedure was refined to ensure greater precision.
Self-report measures
Pain intensity was measured by means of a visual analogue scale (VAS), where 0 mm indicated no pain and 100 mm unbearable pain (24). The subjects were asked to estimate the average pain intensity in the knee over a single day. The VAS is a valid and reliable measure for pain, and changes of 20 mm or more were considered as clinically relevant differences (24).
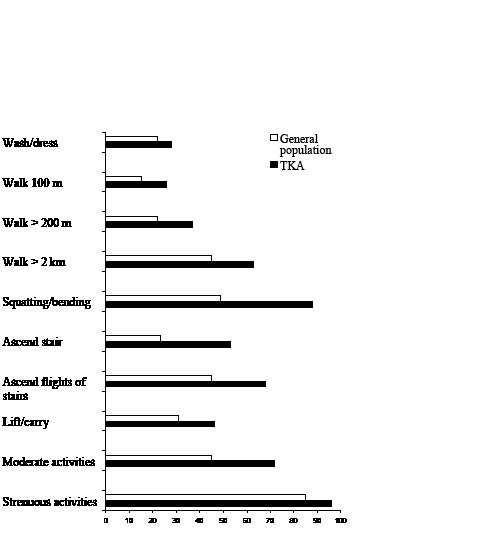
Pain and physical function compared with the general population were measured by the scales of the SF-36, Norwegian version (25), at 9 months. The SF-36 questionnaire is a generic health status instrument widely used in health surveys in the general population as well as in patient groups (26). It yields a profile of 8 domains. The domains pain and physical function were assessed at 9 months in order to evaluate whether the patients approached the scores of the general population. The pain domain consists of 2 questions on the amount of pain intensity in the last 4 weeks and its impact on life and daily work. The domain of physical function consists of 10 items on the subjects’ self perceived limitations in washing/dressing, walking 100 m, walking more than 200 m, walking more than 2 km, bending/kneeling, ascending 1 stair and several flights of stairs, lifting/carrying and in performing moderate and strenuous activities. The raw scores for pain and physical function were coded and recalibrated following the standard guidelines (26). Our data were compared with data from the age group 59–79 years (n = 1190 for pain and n = 1175 for physical function) from the general population of Norway (21). We controlled for sample differences in age, sex and educational level. A difference in scores of above 10 was regarded a clinically relevant difference (27).
Data analysis
The data were analysed using SPSS for Windows version 14. Descriptive statistics for continuous data are given as means and standard deviations (SD). The difference between scores at the different time-points were analysed by the paired sample Student t-tests. Due to multiple comparisons the statistical significance level of these tests was set to 1%. The comparisons between the patients and the general population were examined by linear regression analysis with, respectively, pain and physical function as dependent variables and patient/general population, age, sex and educational level below and above 10 years as independent variables. The p-value was set at 5%.
RESULTS
Subjects
Sixty-seven patients with a mean age of 69 (SD 10) years were included and assessed preoperatively. Four patients were not assessed at 3 months: 2 had died due to heart and lung problems, and 2 did not attend the visit due to long travelling distance. These 4 patients were excluded from the data analysis. The characteristics of the study sample (n = 63) are given in Table I. At 9 months, 5 patients did not attend, and their data at 3 months were carried forward to reflect their 9 months data as well. The analysis was performed both with and without the carried forward data, and the results did not differ. One patient had not fully completed the SF-36 questionnaire and was excluded. Thus, the SF-36 scores are given for 57 patients.
| Table I. Characteristics of 63 patients undergoing total knee arthroplasty |
| | Mean (SD) | n (% of total sample) |
| Age (years) | 69 (10) | |
| Female | | 44 (70) |
| Male | | 19 (30) |
| Education | 12 (3) | |
| Educated ≤ 10 years | | 24 (38) |
| Educated > 11 years | | 39 (62) |
| SD: standard deviation. |
Postoperative course of recovery
The data are shown in Table II.
| Table II. Pain and recovery of physical functioning in patients undergoing total knee arthroplasty |
| | Preoperative mean (SD) | 1 week postoperative mean (SD) | 3 months postoperative mean (SD) | 9 months postoperative mean (SD) |
| Pain intensity, 0–100, mean (SD) | 49 (18) | 40 (23) | 24 (19)* | 22 (23)# |
| Active flexion (degrees) | 124 (13) | 84 (14) | 107 (16)* | 112 (13)†# |
| Active extension (degrees) | –4 (6) | –10 (6) | –6 (5)* | –3 (5)† |
| 40-metre walking test (s) | 37 (13) | | 38 (15) | 34 (11)†# |
| Stairs – ascend duration (s) | 7 (2) | | 6 (2) | 5 (2)†# |
| Stairs – descend duration (s) | 7 (3) | | 6 (2) | 5 (2)†# |
| *Difference between 1 week and 3 months, p-value < 0.001. †Difference between 3 and 9 months, p-value < 0.001. #Difference between preoperative and 9 months, p-value < 0.001. SD: standard deviation. |
Pain intensity. A significant decline in VAS scores was found between 1 week and 3 months after surgery (p < 0.001), and no further reduction in pain was observed from 3 months to 9 months (p = 0.4).
Physical functioning. From 1 week to 3 months after surgery there was a statistically significant increase in active knee flexion (p < 0.001) and extension (p < 0.001). Both did further improve at 9 months (p < 0.001). The 40-m timed walking test improved from 3 to 9 months (p < 0.001). Those managing the stair-climbing test had improved stair-climbing time from 3 to 9 months (p < 0.001), and the number of patients able to descend stairs increased from 3 (n = 29) to 9 months (n = 42) (p < 0.01).
Outcomes at 9 months
In comparison with preoperative assessments a statistically significant pain reduction was found on VAS at 9 months (p < 0.001). Knee flexion had not returned to preoperative measures at 9 months (p < 0.001), while knee extension did not differ from baseline (p = 0.07). Timed walking 40 m on flat floor had improved compared with baseline (p < 0.001). Forty-five out of 63 patients were able to ascend one flight of stairs both preoperatively and at 9 months, and their stair-climbing time had improved (p = 0.001) (Table II). There were no statistically significant differences in the number of patients able to ascend stairs preoperatively (n = 49) vs 9 months postoperatively (n = 49) (p > 0.05) or to descend stairs preoperatively (n = 40) vs after 9 months (n = 42) (p > 0.05).
Self-report on pain and physical functioning at 9 months in comparison with the general population. The mean score on the SF-36 pain scale was 58 (SD 28) in the TKA group (n = 57) and 67 (SD 27) in the general population group (n = 1190). This difference was statistically significant, but was not considered clinically relevant (p = 0.03). With respect to the SF-36 physical function scale, the mean score of the patients with TKA was 60 (SD 24) (n = 57) vs 75 (SD 24) in the general population (n = 1175) (p ≤ 0.001). According to Spilker (26) a difference of more than 10 is considered clinically relevant.
The responses of the patients and the general population to single items in the SF-36 physical function scale are shown in Fig. 1. The figure illustrates that a high percentage of both patients and individuals in the general population report great limitations in performing strenuous activities. In moderate activities 72% of the patients had difficulties vs 45% in the general population. Sixty-eight percent reported difficulties in ascending several flights of stairs vs 45% in the general population. Sixty-three percent had difficulties in walking distances exceeding 2 km vs 45% in the general population. Eighty-eight percent of the TKA patients reported problems with bending and squatting vs 49% in the general population.
Fig. 1. Percentage of patients with total knee arthroplasty (TKA) and those in the general population reporting great/moderate limitations on single items of physical function in the Short-Form-36 (SF-36).
DISCUSSION
During the first 3 postoperative months a considerable reduction in pain was measured, which persisted at 9 months, and improvements in physical functioning were observed throughout the whole 9-month period. Compared with preoperative measures, a statistically significant pain reduction was found, but knee flexion was not regained. Those patients who were unable to ascend stairs both preoperatively and at 9 months had improved their stair-climbing time. However, the total number of patients able to ascend/descend stairs was unchanged. In comparison with the general population, the patients reported impaired physical functioning at 9 months, especially in stair-climbing, squatting and bending. Both groups reported difficulties in strenuous activities and walking distances exceeding 2 km.
Pain is usually the primary criterion of success or failure after undergoing TKA. In the course of recovery the pain intensity score at 3 months was reduced by approximately 50% compared with before surgery and remained at the same level when assessed at 9 months. This difference is considered to be clinically relevant (24). Our results are in line with previous studies and confirm that TKA leads to less pain (8, 28–29). The improvements in physical function seem to take place later throughout the course. Studies of physical functioning following TKA with measures at shorter intervals in the early postoperative stage showed that the greatest change in recovery occurred within the first 9 weeks, with little improvement after 6 months (3, 15). In the present study there was a significant improvement in knee flexion and timed walking from 3 to 9 months. As there were no measurements within this time-span, we do not know at what time the greatest improvements took place.
Less knee pain is likely to make walking easier and timed walking over short distances improved from baseline to 9 months. However, the patients still reported difficulties in walking longer distances. These findings are interesting and may relate to factors such as lack of endurance, muscular strength or balance. Our study also showed that patients who were able to climb stairs preoperatively improved their stair-climbing time at 9 months, while patients who were unable to climb stairs preoperatively were to a large extent still unable to do so after 9 months. In spite of the reduced knee flexion, the range of motion in flexion should be large enough to enable the patients to climb stairs. The inability to climb stairs with alternate legs without using a rail might be due to lack of muscle strength or balance, and hence little trust in the operated knee. The number of patients able to descend stairs was smaller than the number of patients able to ascend. While ascending stairs requires mainly concentric muscular work, descending stairs requires eccentric muscular work, which is considered more challenging. This might be a possible explanation for the larger number of patients unable to descend stairs.
Our performance-based measures on stair-climbing are in accordance with the self-reported assessments showing that 68% of patients reported problems when ascending several flights of stairs after 9 months. Stair-climbing is an everyday activity, and it is striking that a large percentage of the patients still reported problems as long as 9 months after the operation. It is a challenge for physiotherapists to include exercises, such as stair-climbing, as part of the postoperative physiotherapy programme. Physiotherapy in the postoperative period is a common practice, but is largely understudied (2). In further research it is of interest to investigate the effect of physiotherapy after TKA.
Physical functioning is often impaired by age. The decline in physical functioning, however, is reported to be less in highly educated people than in those with a lower educational level, and women seem to report more impaired SF-36 physical function than men in population-based surveys (30). However, in spite of controlling for age, gender and educational level in the present study, an impaired SF-36 physical function was found compared with the general population. Both groups reported problems with especially strenuous activities and walking more than 2 km. According to the responses to single items of the SF-36 physical function scale, the patients with TKA reported more difficulties than the general population in bending, squatting, stair-climbing and performing moderate activities such as gardening. These findings are supported by previous studies (17–18). The fact that patients with TKA have problems with moderately strenuous activities, raises the question as to whether these patients might have the potential to improve to a premorbid state with a more appropriate physiotherapy programme.
To nuance the picture of recovery in the first months after TKA, both performance-based and self-reported measures were applied. Thus, timed walking and stair-climbing as well as self-perceived ability to walk and stair-climb were assessed. In this study the results of performance-based and self-reported measures appeared to agree. This supports the validity of the conclusion that the patients with TKA may have impaired physical function and difficulties in several activities for as long as 9 months after the operation. In this study we measured walking with a 40-m walking test. There are several tests that measure walking ability either by measuring time required to walk a defined distance or how far an individual can walk in a defined time. Timed walking distances of, for example, 10 (31) or 160 m (16) have been applied in previous studies and are considered valid and reliable. We considered 10 m to be too short a distance. Our corridor was 40 m long, which meant that the patients would have had to turn if we had used a 60-m walking test. A turn might have hampered the reliability of the test. Consequently, we measured 40 m timed walking and considered it likely to be both valid and reliable.
A question to be discussed is whether the sample size is large enough to detect a true difference between the times of measurements, i.e. type 2 errors. Our results, however, mostly showed statistically significant differences at the 0.1% level. Therefore the results appear to be robust. If we examine the non-significant results, the descriptive statistics suggest that the changes are so small that they are unlikely to be of great significant clinical importance, e.g. changes in the number of patients being able to perform the stair-climbing test preoperatively compared with after 9 months.
Another important issue is whether our results can be generalized. It is therefore essential to consider whether the sample is representative. Only 5 patients who fulfilled the inclusion criteria were unwilling to participate, and only 4 patients dropped out during the study period. Thus, the sample is unlikely to be a selected group of patients undergoing TKA at this particular hospital. However, in spite of the hospital being a Norwegian community hospital that recruits patients from all parts of the country, it might be that these patients differ from patients in other hospitals. For example, we do not know whether the patients were likely to have more or less severe knee OA than patients in other hospitals. Unfortunately, we did not register comorbidities, and the amount and severity of diseases/illnesses may especially influence recovery of physical function. At inclusion we excluded patients with diseases that could have a severe impact on the recovery process, such as rheumatoid arthritis and stroke. Thus, we believe that our results can be generalized to other groups of TKA patients without severe diseases.
In conclusion, TKA leads to considerable reduction in pain, but aspects of physical functioning are not restored to preoperative status or to the level of the general population. Both the TKA patients and the age-matched group from the general population had problems with strenuous activities. In moderate activities, such as gardening and going for walks, the TKA patients were more impaired than the age-matched group. These findings may have clinical implications for the information given to the patients related to their level of recovery, and may stimulate further research into the effect of physiotherapy after TKA.
ACKNOWLEDGEMENTS
The authors are grateful for permission to apply the data from a survey of the general population in Norway. The data in the analysis in this publication are based on “Level of Living 2002 – Cross-sectional Study – Health”. The “Level of Living 2002” survey was financed by Statistics Norway, The Norwegian Institute of Public Health and Department of Community Medicine, UiO. The data are provided by Statistics Norway, and prepared and made available by the Norwegian Social Science Data Services (NSD). Neither Statistics Norway, the Norwegian Institute of Public Health, the Department of Community Medicine, UiO nor NSD are responsible for the analyses/interpretation of the data presented here (21).
We gratefully acknowledge the patients who agreed to participate in the present longitudinal study. Further acknowledgements are due to the physiotherapy staff at the Hospital of Asker and Baerum. A grant for the study was received from The Norwegian Foundation of Postgraduate Physiotherapists.
REFERENCES