Corrado Marchini, MD1, Michele Acler, MD6, Marco A. Bolognari, MD2, Araldo Causero,MD2, Daniele Volpe, MD4, Dario Regis, MD5, Alessandra Rizzo, MD5, Raffaella Rosa, MD5, Roberto Eleopra, MD3 and Paolo Manganotti, MD, PhD6
From the 1Neurology, City Hospital San Martino, ULSS 1 Belluno, 2Department of Surgical Sciences, Institute of Orthopedic Surgery, University of Udine, 3Neurology, City Hospital All’Angelo di ULSS 12 Mestre-Venezia, 4Rehabilitation Unit, Fatebenefratelli Hospital, Venezia, 5Department of Orthopaedic Surgery, University of Verona and 6Department of Neurological and Visual Sciences, Section of Neurological Rehabilitation University of Verona, Verona, Italy
OBJECTIVE: The aim of this study was to investigate the effect of botulinum toxin type A injection into the adductor muscles in reducing pain and improving joint mobility and quality of life in patients affected by hip osteoarthritis.
METHODS: A total of 39 outpatients, mean age 68 years (age range 41–82 years), were evaluated using the Harris Hip Score to test hip function, a visual analogue scale to measure pain intensity and the Short Form 36 (SF-36) questionnaire to assess patient well-being and quality of life at baseline, 2, 4 and 12 weeks after treatment with botulinum toxin type A. A total of 400 U of botulinum toxin type A (Dysport) was injected into the adductor longus muscle and the adductor magnus muscle.
RESULTS: The Harris Hip Score increased significantly after 2, 4 and 12 weeks (df 3, χ2 = 45.1; p < 0.0001). A significant decrease in pain intensity was detected at all the follow-up visits, after 2, 4 and 12 weeks (df 3; χ2 = 27.8; p < 0.001). The SF-36 score was significantly higher 4 and 12 weeks after treatment. At each evaluation visit a significant correlation was detected between decreased pain and improved hip mobility.
CONCLUSION: Botulinum toxin type A induced a reduction in pain, indicating that this might be an innovative, less invasive treatment in patients affected by severe hip osteoarthritis, with remarkable effects on the clinical management of this disease.
Key words: botulinum toxin; hip osteoarthritis; muscle; pain.
J Rehabil Med 2010; 42: 691–693
Correspondence address: Paolo Manganotti, Sezione Neurologia Riabilitativa, Dipartimento di Scienze Neurologiche e della Visione, Universita’ di Verona. Policlinico “Gianbattista Rossi”, P.zz.le LA Scuro, IT-37100 Verona, Italy. E-mail: paolo.manganotti@univr.it
Submitted October 12, 2009; accepted January 28, 2010
Introduction
The prevalence of hip osteoarthritis (HOA) is approximately 3–6% in the Caucasian population, worldwide (1). In the last 40 years, the surgical treatment of HOA has undergone rapid and remarkable development by means of total hip arthroplasty (THA) and established a definitive course in the treatment of coxarthritis (2). Failure of THA requires further operation, consisting in replacement of loosened components, and revision surgery is very difficult. It is therefore useful to delay the implantation of THA, as well as to ensure that patients waiting for operation can enjoy a high quality of life (with absence of pain and a wide range of motion). Systematic reviews suggest that conservative treatment is effective and advisable in mild-to-moderate cases (3, 4). Conservative therapy includes both pharmacological and non-pharmacological treatments, aimed at either decreasing the mechanical stress across the joint or increasing the stress the joint can withstand (5). In patients with HOA, pain may be a consequence of prolonged or excessive contraction of the adductor muscles. Botulinum toxin (BoNT) is an effective treatment for spasticity of the hip adductors (6). Moreover, injection of BoNT has been used as an adjunctive measure to prevent or delay lateral migration of the femoral head in children with cerebral palsy, which is caused by a biomechanical pulse of the spastic adductor muscle (7). The rationale for BoNT-A injection into selected muscles involved in hip movements is a drastic reduction in the pressure transferred by the femoral head against the acetabulum, as obtained with Voss operation (8), achieving the purpose of breaking, in an efficient and lasting manner, the vicious circle induced by the combination of pain–contraction and contraction–pain (9). The aim of this study was to investigate the effect of BoNT-A injection into the adductor muscles in patients affected by HOA in order to reduce pain and muscle contractures and improve mobility of the hip joint.
Material and methods
This was a prospective, open-labelled, not controlled, multicentre study conducted to assess the effect of the administration of BoNT-A (Dysport®) on hip function, pain and quality of life in outpatients affected by HOA.
Subjects and methods
Adults with X-ray-confirmed HOA referred for pain were recruited from 4 different centres at rehabilitation/orthopaedics units. Radiological classification was assessed using the Kellgren-Lawrence grading scale (10). Patients with previous THA or who had been treated with physiotherapy or analgesic/corticosteroids intra-articular infiltrations during the previous 3 months were excluded, as were patients affected by neurological or neuromuscular diseases or previously treated with BoNT-A. Subjects were evaluated during recruitment and at entry into the study (the mean value of 2 evaluations represents the baseline, V0), and 2 (V1), 4 (V2) and 12 (V3) weeks after treatment. All the subjects were evaluated with the Harris Hip Score (HHS) to test hip function (11). Pain score was assessed using the visual analogue scale (VAS) (12). Every patient had to complete the Short Form 36 (SF-36) test (13) to assess quality of life at baseline, and after 2, 4 and 12 weeks after treatment.
In the presence of bilateral arthritis of the hip only the most symptomatic side was treated. A total of 500 U BoNT-A were diluted in 2 ml physiological solution to a concentration of 250 U/ml. Each subject received a total dose of 400 U; 250 U in the adductor longus muscle and 150 U in the adductor magnus muscle of the thigh ipsilateral to the HOA-affected side, injected slowly at 2 different sites under electromyographic guide. All participants were informed about the aim of the study, signed an informed consenteducated on possible adverse reactions, and were requested to inform the treating physician in case of any complication. The experimental protocol was approved by the local ethics committee.
Statistical analysis
To test changes across different evaluations sessions an analysis of variance was performed through the Friedman test. The Wilcoxon signed-rank test was used to compare paired samples. Spearman’s correlation coefficient was used to examine the relationship between pain symptoms and hip motility. p < 0.05 was taken as statistically significant.
Results
A total of 39 subjects (20 men and 19 women), mean age 68 years, with primary HOA, met the inclusion criteria and were eligible for the study. The mean time from onset of pain was 6.7 months (range 1–39 months). Clinical and demographic data are reported in Table I.
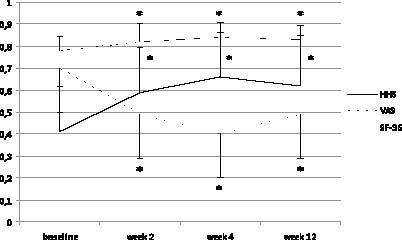
All patients completed VAS, HHS and SF-36 assessment as per protocol. At baseline prior to BoNT-A injection the HHS was 40.9 (standard deviation (SD) 21.0) and this score increased significantly after 2, 4 and 12 weeks (df 3, χ2 = 45.1; p < 0.0001). A significant increase in score was detected between all the recording visits (V0–V1, p < 0.001; V1–V2, p < 0.01; V2–V3, p < 0.01). Before treatment the intensity of pain was 7.0 (SD 2.1) (range 3–10), which was significantly higher than that recorded 2, 4 and 12 weeks after treatment (df 3; χ2 = 27.8; p < 0.001). In particular, pain decreased significantly between baseline, 2 (p < 0.001), 4 (p < 0.001) and 12 (p < 0.01) weeks. Between weeks 2 and 4 pain intensity did not show relevant changes (p = 0.18), but it worsened significantly between weeks 4 and 12 (p ≤ 0.01). At each evaluation a significant correlation between decrease in pain and improved hip mobility was detected (Fig. 1), this correlation being present at baseline (R = 0.7; p < 0.01), 2 (R = 0.7; p < 0.01), 4 (R = 0.77; p < 0.01) and 12 weeks (R = 0.79; p < 0.01) (Table II).
Fig. 1. Time course of the different clinical scales after botulinum toxin type A injection. All the scores were reported as fraction of maximum obtainable score (y-axis). HHS: Harris Hip Score; VAS: visual analogue scale; SF-36: Short Form 36. *p < 0.05 between baseline and different recording sessions.
SF-36 score at study entry was 93.7 (SD 7.8) and showed a significant difference after 4 and 12 weeks (df 2, χ2 = 33.5; p < 0.0001). At 4 weeks the score had improved significantly (p < 0.001), but did not show relevant changes between 4 and 12 weeks (p = 0.1).
BoNT-A administration was well-tolerated and no patients reported adverse effects, except for local reaction at the site of injection. No withdrawals due to adverse events or other reasons occurred.
DISCUSSION
In this multicentre study BoNT-A treatment induced a long-lasting decrease in pain in patients affected by HOA. The novelty of this clinical study is that a single treatment with BoNT-A injected in the adductor muscles improved joint mobility as well as pain and quality of life of the patients. These significant clinical effects are documented by clinical scales in motility as the HHP scores, in pain by the VAS scales and, most importantly, on the quality of life of the patients by SF-36. These clinical effects were observed across the patients treated at the different centres participating in this study and lasted for 12 weeks. According to patients the positive clinical effects were observed starting a few days after BoNT-A injection, and these were documented as per the study protocol assessments after 2 weeks. Despite the open-label design and lack of randomization, lack of a control group and a placebo group to confound the possible placebo effect, which is often strong in patients with pain, and bearing in mind that this is only a preliminary study, the clinical effects were so significant and consistent in all the treated patients that we note that the results indicate the possible importance of this new application of BoNT-A in the orthopaedic field. The main action of BoNT-A treatment is a focal chemical denervation (14) to release contracture of the adductor muscles, leading to a drastic reduction in the pressure transferred by the femoral head against the acetabulum; this reduction allows a substantial restoration of the best functional activity of the hip, with remarkable benefits for mobility of the joint and reduction in pain. It therefore seems that the rationale of the study to decrease contracture of the painful adductors in order to improve mobility in abduction of the leg, as obtained with the Voss operation, may be correct. Other mechanisms could be advocated to explain the clinical effects. Through a reduction in tone in the affected muscles, BoNT-A injection breaks the vicious circle induced by the combination of pain–contraction and contraction–pain (9). Finally, we cannot exclude a direct effect of BoNT-A on sensory receptors, muscle spindle, or pain receptors, as reported in cerebral palsy (15,), diabetic foot pain (16) and arthritis joint pain (17). The relatively transitory effects of BoNT-A are not an alternative to THA, but in our opinion could decrease most of the disabling symptoms, improve quality of life and assist in the clinical management of patients awaiting surgery. In addition, injections could be repeated after 3 months without significant side-effects, as largely documented in the treatment of hypertonia in neurological diseases (18). The long-lasting effect of BoNT-A, particularly in young patients with mild HOA, means that it may be an important additional therapy in the management of this degenerative disease. Finally, BoNT-A might be an effective therapeutic option in higher-risk surgical patients.
More extensive clinical randomized, placebo-controlled and controlled studies are necessary to confirm the results of this preliminary study.
References