OBJECTIVE: The aim of this study was to investigate patients’ knowledge of the most salient features of complex regional pain syndrome and to identify patient characteristics associated with the patients’ level of knowledge.
METHODS: Questionnaire interview of 101 patients with complex regional pain syndrome in Switzerland (mean age 54 years, 77% female). A questionnaire about patients’ disease-related knowledge was developed and piloted. The level of knowledge was defined by a consensus process among clinical experts and a patient. The questions were based on expert consensus about the minimum knowledge a person affected with complex regional pain syndrome should have.
RESULTS: Only 6 patients (6%) reached the minimum medical knowledge. The mean score for all participants was 7.6 points out of a total score of 11 points (range 3-11, SD 2.1). The scores were slightly higher among patients with higher education (apprenticeship, vocational school +0.38 (95% confidence interval (CI); –0.59 to 1.34: p=0.44), university entrance diploma +1.12 (95% CI–0.16 to 2.49: p=0.08), university diploma, advanced technical college +2.36 (95% CI 1.11–3.61: p<0.001)) compared with mandatory school, and among those with professional medical backgrounds +1.13 (95% CI 0.06–2.20: p=0.04). Most patients received information from their caregivers and wanted to know more about therapy or general aspects of the condition.
CONCLUSION: Many patients with complex regional pain syndrome do not have the minimum knowledge of their disease as defined by clinical experts. Physicians should be aware that patients expect to receive disease-related information primarily from their caregivers. In particular, patients wanted more information about therapy and general aspects of the illness.
Key words: complex regional pain syndrome; survey; patient knowledge.
J Rehabil Med 2010; 42: 458–462
Correspondence address: Florian Brunner, Department of Physical Medicine and Rheumatology, Balgrist University Hospital, Forchstrasse 340, CH-8008 Zurich, Switzerland. E-mail: florian.brunner@balgrist.ch
Submitted April 24, 2009; accepted January 15, 2010
Introduction
The successful management of chronic diseases requires active participation of patients (1, 2). However, active participation requires the patient to have at least a minimum level of understanding of their condition. Lack of knowledge promotes patients’ concerns and fears, and leads to unrealistic expectations about the course of illness (3–6). It has been shown that improving patients’ knowledge can improve health outcomes (7). However, the knowledge must be relevant to the patient and must enable them to assume an important role in control and treatment of their condition.
Complex regional pain syndrome (CRPS) is often a debilitating condition with a high impact on daily functioning and quality of life (8, 9). For many patients, living with CRPS is challenging, since they often have to cope with physical and psychosocial problems (10). Moreover, the pathophysiology and course of the condition is a matter of debate, and it is not possible to predict how patients will respond to treatment (11). Experiences of other chronic illnesses have shown that good communication between practitioners and patients regarding the patients’ perspective of the condition, as well as patient education, are essential for successful management, improvement of daily function and quality of life (12).
In clinical practice, physicians often assume that patients have a certain minimum level of knowledge about their condition (13). However, to date it is unknown whether patients with CRPS 1 meet this expectation. The aim of this study was therefore: (i) to define the minimum knowledge that a lay person affected with CRPS should have about this condition; (ii) to investigate whether patients with CRPS possess this minimum knowledge; and (iii) to identify patient characteristics associated with this level of knowledge.
Methods
The study was approved by the local ethics committee and informed consent was obtained from all participants.
Patient views
Participants were asked where they received information about CRPS from, and from whom they primarily expected to receive disease-related information. In addition, they were asked what more they would like to know about the condition and whether they thought that more knowledge would be related to improved coping.
Defining minimum knowledge
In order to be able to test the patients’ knowledge about CRPS, a panel consisting of 8 clinical experts (2 rheumatologists, 1 physical medicine and rehabilitation specialist, 1 neurologist, 1 orthopaedic surgeon, 1 psychologist, 1 anaesthesiologist and 1 physiotherapist) and 1 patient with CRPS 1, was asked to define the minimum medical knowledge a lay person with CRPS should have. The panel was instructed to take care to state only the most common facts that patients with CRPS should know. Their statements were then transformed into open format questions and implemented in the questionnaire. The panel reached a consensus about the level of knowledge and confirmed the adequacy of the format. The questionnaire was then piloted on 10 patients with CRPS. Based on the feedback from the pilot version a final version of the questionnaire was produced.
The final version of the questionnaire comprised 11 questions. The scoring range was 0–11 points (each correct answer was scored as 1 point). The complete set of questions and the correct answers are shown in Table I.
| Table I. Final version of the questionnaire with correct answers |
| Question | Correct answer |
| Do you know any other names for CRPS? | E.g. algodystrophy, Sudecks’ disease, etc. |
| What is more common in the general population: elevated blood
pressure or CRPS? | Elevated blood pressure |
| What is the difference between CRPS 1 and 2? | CRPS 2 with identifiable nerve injury |
| What are the three stages of CRPS? | Acute (warm), dystrophic (cold) and atrophic stage |
| Do you know any initiating events of CRPS, other than your own? | Trauma, surgery, immobilisation, idiopathic |
| How is CRPS diagnosed? | Clinical diagnosis |
| Do you know any signs and symptoms of CRPS, other than your own? | Sensory, autonomic, motor, trophic changes |
| Do you know any medications used in the treatment of CRPS? | Acetaminophen (paracetamol), non-steroidal anti-inflammatories, opioids, anticonsvulsants, vitamin C, steroids, calcitonin, antidepressants, DSMO, capsaicin |
| What treatments, other than medication, are used in the treatment of CRPS? | Physiotherapy, occupational therapy, psychological and psychiatric interventions |
| What is the main goal in the treatment of CRPS? | Functional restoration, pain reduction |
| Is CRPS a psychological disorder? | No |
| CRPS: complex regional pain syndrome; DSMO: Dimethyl sultoxide. | |
Recruitment sources
Patients were recruited to the study through the outpatient clinic of Balgrist University Hospital, Zurich, Switzerland, through an advertisement on the home-page of a self-help website for patients with CRPS 1 (www.morbus-sudeck.ch), and by contacting 2 regional self-help organizations. Forty-five patients attending the outpatient clinic were invited to participate, and 36 agreed. Fifteen patients replied to the web advertisement and all 15 completed the survey. Forty-five patients out of approximately 60 patients attending 2 regular meetings held by 2 patient self-help organizations agreed to participate. A further 5 patients contacted us directly after hearing about the study. We included all eligible and consenting adult patients who fulfilled the IASP criteria (14) for CRPS, with an illness duration of more than 3 months. Fulfilment of the IASP criteria was confirmed by reviewing the participant’s chart or by clinical examination (for participants from our outpatient clinic). In cases where this was impossible, information was obtained through a telephone interview with the patient.
Data acquisition
Eligible patients were contacted and invited to the interview if they agreed to participate in the survey. In order to minimize the possibility of specific preparation prior to the interview, no details about the content of the questionnaire were provided to the patients. Participants were assured that their individual comments would remain anonymous and were encouraged to express their individual attitudes and expectations.
Interviewer
One interviewer received oral and written instructions on how to conduct the interviews and was trained on 5 subjects. The interviewer was not involved in the patients’ treatment or the development of the questionnaire.
Statistical analysis
First, the total number of correct replies was counted across all questions. Assessment of correct replies was performed in duplicate according to the predefined replies, and any disagreements between the assessors were discussed. In cases of continued disagreement, particularly if the participant used an unusual term, the answer was classified as correct. Secondly, the relationship between level of knowledge and participant’s highest education and possible professional medical background was assessed using 2 regression models, where the cumulative number of correct replies was the dependent variable and the highest education level or possible professional medical background were the independent variables. Independent variables were transformed into dummy variables (indicator variables). The lowest level acted as the baseline category. Statistical analysis was performed using the Stata 10 software package (StataCorp, 4905 Lakeway Drive, College Station, TX, USA).
Results
Study population
The study population comprised 101 patients (77 females (77%), mean age 54 (SD 12) years). Ninety-seven patients (96%) had CRPS 1 with a mean illness duration of 57.2 (SD 48.5) months. The most common initiating event was surgery (n = 57; 56%) followed by trauma (n = 39; 39%). Details of affected body parts, education and medical background are shown in Table II.
| Table II. Characteristics of study population (n = 101) |
| Characteristics | |
| Number of participants (%) | 101 (100) |
| Gender, n (%) Male Female | 24 (24) 77 (77) |
| Age, years, mean (SD) Age range, years | 54 (12) 17–80 |
| CRPS 1, n (%) CRPS 2, n (%) | 97 (96) 4 (4) |
| Affected body part, n (%) Hand Foot Knee Shoulder-hand syndrome, n (%) > 1 limb | 35 (34) 40 (40) 8 (8) 12 (12) 6 (6) |
| Months with CRPS, mean (SD) | 57.2 (48.5) |
| Initiating even, n (%) | |
| Trauma | 39 (39) |
| Surgery | 57 (56) |
| Others | 5 (5) |
| Education, n (%) Mandatory school Apprenticeship, vocational school University entrance diploma University, advanced technical college Others | 37 (37) 32 (32) 11 (11) 14 (14) 6 (6) |
| Medical background, self reported, n (%) Yes No | 20 (20) 81 (80) |
| Medical background, specified, n (%) | |
| Laboratory technician | 1 (5) |
| Nurse | 6 (30) |
| Physician | 3 (15) |
| Medical researcher | 1 (5) |
| Others (e.g. paramedical staff) | 9 (45) |
| CRPS: complex regional pain syndrome; SD: standard deviation. |
Patients’ views
Most patients received information from their physicians and expected to receive disease-related information primarily from their caregivers. In addition, patients wanted to know more about therapeutic strategies or general aspects of the condition. Most participants (84.2%) thought that more knowledge was related to improved coping. Table III shows details of the patients’ views.
| Table III. Questions regarding patient’s views (n = 101) |
| Question | Answer | n | % |
| Where did you obtain information about CRPS? | Physician Internet Self-help organization Paramedical staff Print media Friends Other patients None | 57 54 30 11 14 6 2 1 | 56 54 30 11 14 6 2 1 |
| Through what source would you like to receive more information about CRPS? | Physician Print media Patients concerned Self help organization Various | 58 15 3 1 28 | 57 15 3 1 28 |
| On what topics would you like to get more information? | Therapy General aspects Prognosis Pathophysiology Results from research Psychological aspects | 39 35 25 10 2 3 | 39 35 25 10 2 3 |
| Do you think that more knowledge is related to improved coping? | Yes No Not sure | 85 13 3 | 84 13 3 |
Minimum CRPS-related knowledge
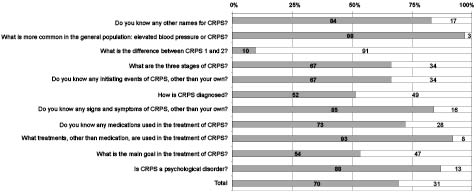
Only 6 patients (6%) had the minimum medical knowledge of CRPS. Only 10 patients knew the difference between CRPS 1 and CRPS 2. Most patients (n = 98) gave the correct answer to the question: “What is more common in the general population: elevated blood pressure or CRPS?”. The detailed results are shown in Fig. 1.
Fig. 1. Disease-related knowledge. Dark bars indicate correct replies.
The scores were slightly higher among patients with higher education (apprenticeship, vocational school +0.38 (95% confidence interval (CI); –0.59 to 1.34: p = 0.44), university entrance diploma +1.12 (95% CI–0.16 to 2.49: p = 0.08), university diploma, advanced technical college +2.36 (95% CI 1.11–3.61: p < 0.001)) compared with mandatory school, and among those with professional medical backgrounds +1.13 (95% CI 0.06–2.20: p = 0.04).
Discussion
The results of this survey are two-fold: first, only a small minority of participants had a minimum CRPS knowledge as defined by clinical experts. The level of knowledge was slightly higher among those patients with higher education or with a medical background. The results remained largely unchanged when correcting for potential confounders such as duration of symptoms, patients’ age and gender. The low number of patients with the minimum level of knowledge highlights the need for specific educational programmes for our surveyed sample of patients. Secondly, most patients received disease-related knowledge from their caregivers and were concerned to know more about therapy and general aspects of the condition.
A review of the English literature did not disclose any survey assessing patient knowledge of CRPS. This study is the first attempt to determine the level of disease-related knowledge in patients with CRPS and to identify information sources. The strengths of this study include the definition of the minimum medical knowledge by various experts in the field of CRPS, and the relatively large number of participants. In order to minimize enrolment bias, we considered the level of education and possible medical background in our analysis.
This study has several limitations: first, the recruitment process may be associated with a certain selection bias. We did not include data from patients who were given the survey but did not return it, and this may have introduced bias. Since our invitation to participate was also disseminated via the internet it is likely that our sample included patients who were familiar with using the internet. Arguably, patients with internet access may be more motivated to learn about the disease, thus our sample might not be representative of typical CRPS patients. Secondly, to overcome the issue of validity and reliability, we propose using a validated instrument to measure illness perception (e.g. the Illness Perception Questionnaire) in a continuation of this study. Thirdly, we had to develop a new assessment instrument rather than using an already established questionnaire. To our knowledge no such instrument is currently available. Arguably, other expert panels might have set different knowledge dimensions and questions, and this would limit the generalizability of our findings. Moreover, we compiled a group of experts of various clinical specialities and a patient with CRPS. Fourthly, for those participants who were not patients at our clinic, we confirmed the diagnosis by applying the IASP criteria by telephone and we did not verify the diagnosis clinically.
Further research should aim to replicate our findings. Moreover, the assumption that increased knowledge has a positive effect on coping strategies and self-management needs to be explored further, and underlying mechanisms should be identified. If the findings of this study are confirmed, future research should be directed towards improving patient education.
In order to identify specific needs we see a clear role for validated instruments such as the Illness Perception Questionnaire. Complementary to this we believe that a simple and rapid baseline assessment of disease-related knowledge can be a helpful and useful further input when tailoring educational interventions, particularly when they refer directly to the underlying illness (CRPS). However, before replicating this study in a larger (and more representative) context, we require a more specific consensus regarding the content of the questionnaire.
Self-management programmes for type 1 diabetes (15) and severe asthma (16) are examples of complex interventions in which patient knowledge gave promising results towards a improving treatment outcome. Only an educational intervention trial will indicate to what extent educational measures provided to patients with CRPS can have a sustained effect on treatment outcome or quality of life. On the other hand, in 2001 Norris et al. (17) published a systematic review assessing the effectiveness of self-management training in type 2 diabetes. In a thorough examination they found that didactic interventions focusing only on the acquisition of knowledge and information, despite having some positive effects on knowledge showed only mixed results on clinically relevant outcomes such as glycaemic control and blood pressure. They concluded that behavioural theory must have a more explicit role in future studies, and highlighted the importance of programmes aiming at behavioural change, rather than isolated educational programmes focusing on improvement in patients’ knowledge.
In our view one important consequence emerges from our study. Physicians looking after patients with CRPS should address the topics covered within our minimum CRPS knowledge questionnaire. We believe that experience in other illnesses, such as asthma and irritable bowel syndrome, could serve as valuable role models when developing these programmes. The example of asthma has repeatedly shown that informed patients take more care of themselves, have lower exacerbation rates, and feel happier (18, 19). Even small improvements in treatment outcome or quality of life, as shown in this study, can play an important role for patients, particularly if treatment options have only a limited effect on the course of debilitating symptoms.
The findings of this study raise awareness that although patients with CRPS have a fairly high knowledge of their disorder, only a minority reach the minimum medical knowledge as defined by experts. Physicians should be aware that patients with CRPS expect disease-related information first and foremost from their caregivers. In particular, the patients wanted more information about therapy and general aspects of the illness.
References