OBJECTIVES: To determine whether exercise is more effective than usual care to reduce work disability in patients with non-acute non-specific low back pain, and if so, to explore which type of exercise is most effective.
METHODS: Systematic review and meta-analysis of randomized controlled trials investigating the effectiveness of exercise in non-acute non-specific low back pain, and reporting on work disability. DATA SOURCES: MEDLINE, EMBASE, PEDro, Cochrane Library databases, NIOSHTIC-2, and PsycINFO until August 2008. Work disability data were converted to odds ratios. Random effects meta-analyses were conducted.
RESULTS: A total of 23 trials met the inclusion criteria, 20 of which were suitable for inclusion in meta-analysis allowing 17 comparisons of exercise interventions with usual care and 11 comparisons of 2 different exercise interventions. A statistically significant effect in favour of exercise on work disability was found in the long term (odds ratio (OR) = 0.66, 95% confidence interval (CI) 0.48–0.92) but not in the short (OR = 0.80, 95% CI 0.51–1.25) and intermediate term (OR = 0.78, 95% CI 0.45–1.34). Meta-regression indicated no significant effect of specific exercise characteristics.
CONCLUSION: Exercise interventions have a significant effect on work disability in patients with non-acute non-specific low back pain in the long term. No conclusions can be made regarding exercise types.
Key words: low back pain; exercise; meta-analysis; vocational rehabilitation; sick leave.
J Rehabil Med 2010; 42; 193–205
Correspondence address: Peter Oesch, Research Department, Rehabilitation Centre Valens, CH-7317 Valens, Switzerland. E-mail: p.oesch@klinik-valens.ch
Submitted April 7, 2009; accepted December 8, 2009
INTRODUCTION
Low back pain is the most prevalent of musculoskeletal conditions. It affects almost everyone during their lifetime and has become a major socioeconomic problem in western countries (1). Exercise is consistently recommended in modern treatment guidelines for non-acute non-specific low back pain (NSLBP) defining return to work as the primary treatment goal (2, 3). Exercises applied in the treatment of patients with NSLBP encompass a wide variety of interventions and are applied with different rationales. The sports medicine approach applies exercise based on the principles of exercise physiology, and is used in functional restoration programs with the goal of restoring physical function and thereby enabling patients to return to work (4). Behavioural treatment programmes use exercise with the aim of modifying pain behaviour. Patients learn that it is safe to move, while restoring function by receiving continuous feedback and positive reinforcement (5).
Until the year 2000 no evidence was found for the effectiveness of specific exercises in the management of chronic low back pain. Abenhaim et al. (2) state: “it appears that the key to success is physical activity itself, i.e. activity of any form, rather than any specific activity”. A later review revealed that individually designed stretching or strengthening exercises delivered with supervision may improve pain and function in chronic NSLBP. The authors recommended further testing with this multivariable model and further assessment with specific patient-level characteristics and exercise types (6). A systematic review of trials with positive outcomes on work disability revealed that all had significant cognitive behavioural components combined with intensive physical training. The authors, however, advised caution when interpreting this post-hoc analysis and recommended further investigation into the contribution of these exercise characteristics (7). Whereas additional reviews found limited evidence for the effectiveness of behavioural graded activity in improving absenteeism outcomes (8, 9), strong evidence has been found that exercise reduces work disability in patients with NSLBP (7, 10, 11). These reviews were based on studies published prior to 2004 that did not evaluate the effectiveness of different exercise characteristics.
Although new studies have been published in the meantime, the effect of specific exercise characteristics on work disability is still unclear; a more up-to-date review is required. The objective of this review is to use recent research results to determine whether exercise is more effective than usual care to reduce work disability in patients with non-acute NSLBP, and if so, to explore which type of exercise is most effective.
METHODS
Searching
The search strategy was based on the recommendations of the Cochrane Back Review Group (12). We searched MEDLINE, EMBASE, PEDro, the Cochrane Library, PsycINFO (2002–August 2008) and NIOSHTIC-2 (until August 2008). This search was combined with a previous search performed in December 2002 covering MEDLINE (1966–October 2002), EMBASE (1988–October 2002), PEDro (until December 2002), the Cochrane Library (2002, Issue 4) and PsycLIT (1984–December 2002) (10). References were checked for further trials.
Selection, validity assessment, and data abstraction
Studies were included if randomized controlled trials were performed, the primary diagnosis in all patients was non-acute NSLBP with a duration of at least 4 weeks, the experimental treatments used exercise alone or as a part of a multidisciplinary treatment, work disability was the primary outcome, and if at least 90% of the patients under treatment were available for the job market, in that they were either employed or unemployed but seeking work. Excluded were studies that did not report work disability, investigated the effect of treatments that did not contain any form of exercise such as respondent psychological interventions, included patients with thoracic pain, cervical pain or specific low back pain, such as nerve root compression, vertebral fracture, tumour, infection, inflammatory diseases, spondylolisthesis, spinal stenosis and definite instability, and studies that included pregnant women with low back pain.
Two authors (PO and JK) independently applied the admission criteria for the studies and assessed risk of bias. Disagreements were solved through discussion involving a third researcher (StB). Authors were contacted if the information regarding the eligibility of a trial, quality criteria, or work disability were unclear.
Study quality was assessed according to Juni et al. (13), who stated that the internal validity of a study was threatened by detection bias, attrition bias, selection bias, and performance bias. Thus, the following 3 criteria were rated as “met”, “unclear” or “not met”: Concealed allocation, blinding of the outcome assessor, and intention to treat analysis. Performance bias was not assessed as it is not strictly possible to blind the treatment provider and recipient in clinical trials investigating the effect of exercise to treatment allocation. The internal validity of the included studies were then evaluated on methodological overall assessment. Studies were classified as high-quality studies if 2 or 3 of the criteria were met, while studies were classified as of low quality if one or none of the criteria were met.
For each study, 2 of the authors (PO and StB) independently extracted data from all included studies and defined exercise characteristics. Four criteria designed by Hayden et al. (6) were used, namely programme design, delivery type, dose, and type. Additionally, 2 criteria proposed by Schonstein et al. (14) were used, namely work context and exercise administration within a cognitive behavioural approach. A further criterion was the setting in which exercise was applied (see Table I).
| Table I. Exercise intervention characteristics |
| Programme design (according to Hayden et al. (6)) |
| - “Individually designed”, in which the treating therapist completed a clinical history and physical examination and delivered an exercise programme specifically designed for the individual participant. |
| - “Standard design”, in which a fixed exercise programme was delivered to all participants. |
| Delivery type (according to Hayden et al. (6)) |
| - Home exercises: participants performed their exercises at home with no direct supervision by the therapist. |
| - Supervised exercises: participants performed their exercises either under 1-on-1 supervision or attended exercise therapy sessions with 2 or more participants. |
| - Exercise therapy programmes that included both types of delivery will be classified according to their main delivery type. |
| Exercise dose (hours of intervention time) (according to Hayden et al. (6)) |
| - We will calculate the exercise dose from the exercise duration and the number of treatment sessions received. Home exercise dose will only be included in exercise dose calculation if the home training was controlled (i.e. by using an exercise diary or by follow-up visits). If the study adherence information is not reported, we will assume an adherence rate of 50%. We will then dichotomize the exercise interventions into high- and low-dose exercise. |
| Types of exercises (according to Hayden et al. (6)) |
| - Strengthening exercises - Stretching exercises - Mobilizing or flexibility exercises - Aerobic exercises - Stabilization exercises |
| - Programmes that included different exercise types will be classified as mixed exercises. |
| Setting |
| - Inpatient |
| - Outpatient |
| Work context (proposed by Schonstein et al. (14)) |
| - Exercises will be classified as work-related if these were specifically designed to restore work-related physical capacity. |
| Behavioural treatment approach (proposed by Schonstein et al. (14)) |
| - Exercises will be considered as administered within a behavioural treatment approach if this was specifically stated or if at least 3 of the following behavioural treatment modalities were applied: positive reinforcement of healthy behaviours (i.e. reassurance that it is safe to move, encouragement for early return to work); goal-contingent instead of pain-contingent exercise administration (i.e. exercise intensity was progressively increased to pre-set goals despite pain provocation); patients were given self-responsibility for treatment; patient education about a multidimensional view of pain (i.e. explanation of pain mechanisms); pain-coping strategies were applied (i.e. relaxation techniques were a consistent feature of the exercise programme). |
Quantitative data synthesis
Work-related outcomes were converted into odds ratios (OR) using the method described by Chinn (15) and Hasselblad & Hedges (16). This method is based on the fact that, when assuming logistic distributions and equal variances in the 2 treatment groups, the log OR corresponds to a constant multiplied by the standardized difference between means. The ‘’metan’’ command for Stata statistical software (Stata Corporation, College Station, TX V10) was used to conduct DerSimonian and Laird random effects meta-analyses (17). To use all available means, we estimated missing standard deviations (SD) from other included studies. We assessed treatment effects at 3 different times of follow-up (short-term = closest to 4 weeks, intermediate-term = closest to 6 months, long-term = closest to 12 months). Between-trial heterogeneity was quantified using the I2 statistic, which can be understood as the proportion of the total variation in estimated ORs that is due to between-trial heterogeneity rather than chance (18). The extent to which one or more study characteristics explained between-trial heterogeneity was explored using meta-regression. The following explanatory variables were considered according to an a priori statistical analysis plan: exercise design (individual vs standard care), dose (high- vs low-dose exercise), delivery type (home-based exercises vs supervised exercises), type (specific vs mixed), administration within a cognitive behavioural approach (yes/no), work context (yes/no), and setting (in- vs outpatient) in bivariate models. In addition, we assessed the effect of methodological quality (low vs high). For work disability we included the variables above in meta-regression models and conducted random effects meta-analyses within each subgroup. Differences between small and large trials were assessed using funnel plots (19).
RESULTS
Trial flow
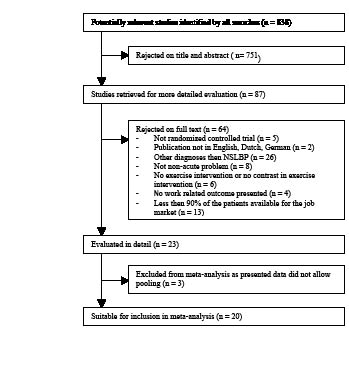
Of the 838 articles retrieved from the literature search, we evaluated 87 articles in detail, of which 64 did not meet the inclusion criteria. Consequently, we included 23 studies in this review. Sixteen were trials with 2 study arms and 7 were trials with 3 study arms. Table II summarizes the characteristics of the included studies. Twenty studies were included in the meta-analysis, allowing 17 comparisons of exercise interventions with usual care (5, 27, 29, 31, 32, 35, 41, 46, 47, 50, 52–54) and 11 comparisons of 2 different exercise interventions (20, 21, 29, 31, 33, 34, 37, 43, 45, 46, 53). Three studies (22, 25, 26) were excluded from meta-analysis as “days of sick leave” were presented as median and interquartile range, thereby preventing pooling (Fig. 1).
| Table II. Study characteristics |
| Study | Participants | Interventions (exercise characteristic classification) | Work disability outcomes and terms of follow-up | Results |
| Alaranta et al., 1994 (Finland) (20) | 293 patients with NSLPB > 6 months, age 30–47 years | A: Akseli Programme: 3 weeks, 37 h/week of guided or self-controlled physical exercise, 5 h/week cognitive-behavioural disability management groups, no passive treatments: (ID, SE, HD, MxE, IP, WCy, Bty) B: Current national type of inpatient rehabilitation: 3 weeks, 15–20 h/week physical activity, large amount of passive treatments: (ID, SE, HD, MxE, IP, WCn, BTn) | Number of subjects with more than 30 sick days at one year FU | No difference regarding sick leave (A: 26%, B: 23%) after one year |
| Aure et al., 2003 (Norway) (21) | 49 patients sick-listed 8–24 weeks due to NSLPB, age 20–60 years | A: Manual therapy and specific exercise: 16 session lasting 45 min including spinal manipulation, specific mobilization, and stretching techniques as well as 5 general and 6 specific localized exercises for spinal segments and pelvic girdle, individual home exercises: (ID, SE, LD, SaE, OP, WCn, BTn) B: Supervised exercise therapy: 16 sessions consisting of 10 min warm-up on an exercise bicycle and 35 min. exercise session for the trunk, and lower limb muscles, suited to the clinical findings, individual home exercises: (ID, SE, LD, MxE, OP, WCn, BTn) | Proportion of partly or fully sick-listed patients at 4 weeks, 6 and 12 months FU | Significant advantage at 4 weeks FU for A vs B (30% vs 57%), at 6 months (11% vs 62%), and at 12 months (19% vs 59%). |
| Bendix et al., 1995, 2000, 1998 (Denmark) (22–24) | 132 patients with disabling NSLPB > 6 months, threatened job situation or out of work | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-h day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Active physical training: Two sessions a week for 6 weeks, consisting of 45 min aerobics class, 45 min progressive resistance training, and 1 h of theoretical back lessons every second session: (SD, SE, LD, MxE, OP, WCn, BTn) C: Psychological pain management: 2 sessions lasting 75 min, twice a week for 6 weeks., combining active physical training of 15 min warm-up exercises, and 30 min progressive resistance training with psychological pain management: (SD, SE, LD, MxE, OP, WCn, BTy) | Sick days (median, IQR) and work capability as judged by a physician at 4 and 13 months FU | Sick days: significant advantage after 4 months for A and B vs C. A: 25 (0–103), B: 13 (0–122), C: 122 (60–122), and after 13 months for A vs B and C and for B vs C. A: 52 (0–127), B: 100 (0–390), C: 295 (0–390). Significantly better work capability in A vs B and C after 4 months (A: 75%, B: 48%, C: 40%) and 2 years (A: 80%, B: 55%, C: 44%) |
| Bendix et al., 1998, 1996 (Denmark) (24, 25) | 106 patients with
> 6 months of disabling back pain, age 18–59 years | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by 1 6-hour day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Usual care | Sick days (median, IQR) and work capability as judged by a physician at 4 months and 2 years FU | Sick days: significant difference at 4 months FU. A: 10 (0–122), B: 122 (24.5–122). Work capability: significantly larger improvement at 4 months. A: from 27% to 64%, B: from 16% to 29%. No difference after 2 years. A: 52%, B: 51% |
| Bendix et al., 2000 (Denmark) (26) | 138 patients, precarious work situation due to NSLPB | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-hour day weekly for the subsequent 2 weeks, and a third day after 2nd month: (ID, SE, HD, MxE, OP, WCy, BTy) B: Outpatient intensive physical training: aerobics and strengthening exercises for 1.5 h 3 times/week for 8 weeks: (SD, SE, HD, MxE, OP, WCn, BTn) | Sick days (median, IQR) and work capability as judged by a physician at one year FU. No statistical comparison between groups. Results disregard 32 of 138 randomized patients who did not finish treatment | Sick days: No difference at 1 year FU. A: median in 34/48 patients 5.5 (0–113), B: median in 40/50 patients 2.5 (0–301). Work capability: pre-post A: from 28 to 36/48, B: from 21 to 35/51 |
| Hagen et al., 2000, 2003 (Norway) (27, 28) | 457 patients with NSLPB and sick leave 8–12 weeks, age 18–60 years | A: Light mobilization programme: examination at spine clinic for 1 hour, information, advice to stay active and go on daily walks; individual instructions lasting 1–1.5 h on stretching and training at home by the physical therapist: (ID, HE, LD, ScE, OP, WCn, BTy) B: Usual care by GP | Days of sickness compensation (mean, 95% CI), numbers of workers returning to full-duty work at 3, 6, 12, 24, and 36 months FU | Significant fewer sick days at one year FU in A vs B (A: 95.5, 104.5, B: 133.7, 112). RTW: significant improvement after 6 months in A vs B (A: 61.2 %, B: 45.0 %) and 1 year (A: 68.4 %, B: 56.4 %). No significant difference at 3-year FU (A: 36.2%, B: 38.2%) |
| Table II. Study characteristics |
| Study | Participants | Interventions (exercise characteristic classification) | Work disability outcomes and terms of follow-up | Results |
| Alaranta et al., 1994 (Finland) (20) | 293 patients with NSLPB > 6 months, age 30–47 years | A: Akseli Programme: 3 weeks, 37 h/week of guided or self-controlled physical exercise, 5 h/week cognitive-behavioural disability management groups, no passive treatments: (ID, SE, HD, MxE, IP, WCy, Bty) B: Current national type of inpatient rehabilitation: 3 weeks, 15–20 h/week physical activity, large amount of passive treatments: (ID, SE, HD, MxE, IP, WCn, BTn) | Number of subjects with more than 30 sick days at one year FU | No difference regarding sick leave (A: 26%, B: 23%) after one year |
| Aure et al., 2003 (Norway) (21) | 49 patients sick-listed 8–24 weeks due to NSLPB, age 20–60 years | A: Manual therapy and specific exercise: 16 session lasting 45 min including spinal manipulation, specific mobilization, and stretching techniques as well as 5 general and 6 specific localized exercises for spinal segments and pelvic girdle, individual home exercises: (ID, SE, LD, SaE, OP, WCn, BTn) B: Supervised exercise therapy: 16 sessions consisting of 10 min warm-up on an exercise bicycle and 35 min. exercise session for the trunk, and lower limb muscles, suited to the clinical findings, individual home exercises: (ID, SE, LD, MxE, OP, WCn, BTn) | Proportion of partly or fully sick-listed patients at 4 weeks, 6 and 12 months FU | Significant advantage at 4 weeks FU for A vs B (30% vs 57%), at 6 months (11% vs 62%), and at 12 months (19% vs 59%). |
| Bendix et al., 1995, 2000, 1998 (Denmark) (22–24) | 132 patients with disabling NSLPB > 6 months, threatened job situation or out of work | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-h day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Active physical training: Two sessions a week for 6 weeks, consisting of 45 min aerobics class, 45 min progressive resistance training, and 1 h of theoretical back lessons every second session: (SD, SE, LD, MxE, OP, WCn, BTn) C: Psychological pain management: 2 sessions lasting 75 min, twice a week for 6 weeks., combining active physical training of 15 min warm-up exercises, and 30 min progressive resistance training with psychological pain management: (SD, SE, LD, MxE, OP, WCn, BTy) | Sick days (median, IQR) and work capability as judged by a physician at 4 and 13 months FU | Sick days: significant advantage after 4 months for A and B vs C. A: 25 (0–103), B: 13 (0–122), C: 122 (60–122), and after 13 months for A vs B and C and for B vs C. A: 52 (0–127), B: 100 (0–390), C: 295 (0–390). Significantly better work capability in A vs B and C after 4 months (A: 75%, B: 48%, C: 40%) and 2 years (A: 80%, B: 55%, C: 44%) |
| Bendix et al., 1998, 1996 (Denmark) (24, 25) | 106 patients with
> 6 months of disabling back pain, age 18–59 years | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by 1 6-hour day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Usual care | Sick days (median, IQR) and work capability as judged by a physician at 4 months and 2 years FU | Sick days: significant difference at 4 months FU. A: 10 (0–122), B: 122 (24.5–122). Work capability: significantly larger improvement at 4 months. A: from 27% to 64%, B: from 16% to 29%. No difference after 2 years. A: 52%, B: 51% |
| Bendix et al., 2000 (Denmark) (26) | 138 patients, precarious work situation due to NSLPB | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-hour day weekly for the subsequent 2 weeks, and a third day after 2nd month: (ID, SE, HD, MxE, OP, WCy, BTy) B: Outpatient intensive physical training: aerobics and strengthening exercises for 1.5 h 3 times/week for 8 weeks: (SD, SE, HD, MxE, OP, WCn, BTn) | Sick days (median, IQR) and work capability as judged by a physician at one year FU. No statistical comparison between groups. Results disregard 32 of 138 randomized patients who did not finish treatment | Sick days: No difference at 1 year FU. A: median in 34/48 patients 5.5 (0–113), B: median in 40/50 patients 2.5 (0–301). Work capability: pre-post A: from 28 to 36/48, B: from 21 to 35/51 |
| Hagen et al., 2000, 2003 (Norway) (27, 28) | 457 patients with NSLPB and sick leave 8–12 weeks, age 18–60 years | A: Light mobilization programme: examination at spine clinic for 1 hour, information, advice to stay active and go on daily walks; individual instructions lasting 1–1.5 h on stretching and training at home by the physical therapist: (ID, HE, LD, ScE, OP, WCn, BTy) B: Usual care by GP | Days of sickness compensation (mean, 95% CI), numbers of workers returning to full-duty work at 3, 6, 12, 24, and 36 months FU | Significant fewer sick days at one year FU in A vs B (A: 95.5, 104.5, B: 133.7, 112). RTW: significant improvement after 6 months in A vs B (A: 61.2 %, B: 45.0 %) and 1 year (A: 68.4 %, B: 56.4 %). No significant difference at 3-year FU (A: 36.2%, B: 38.2%) |
| Table II. Study characteristics |
| Study | Participants | Interventions (exercise characteristic classification) | Work disability outcomes and terms of follow-up | Results |
| Alaranta et al., 1994 (Finland) (20) | 293 patients with NSLPB > 6 months, age 30–47 years | A: Akseli Programme: 3 weeks, 37 h/week of guided or self-controlled physical exercise, 5 h/week cognitive-behavioural disability management groups, no passive treatments: (ID, SE, HD, MxE, IP, WCy, Bty) B: Current national type of inpatient rehabilitation: 3 weeks, 15–20 h/week physical activity, large amount of passive treatments: (ID, SE, HD, MxE, IP, WCn, BTn) | Number of subjects with more than 30 sick days at one year FU | No difference regarding sick leave (A: 26%, B: 23%) after one year |
| Aure et al., 2003 (Norway) (21) | 49 patients sick-listed 8–24 weeks due to NSLPB, age 20–60 years | A: Manual therapy and specific exercise: 16 session lasting 45 min including spinal manipulation, specific mobilization, and stretching techniques as well as 5 general and 6 specific localized exercises for spinal segments and pelvic girdle, individual home exercises: (ID, SE, LD, SaE, OP, WCn, BTn) B: Supervised exercise therapy: 16 sessions consisting of 10 min warm-up on an exercise bicycle and 35 min. exercise session for the trunk, and lower limb muscles, suited to the clinical findings, individual home exercises: (ID, SE, LD, MxE, OP, WCn, BTn) | Proportion of partly or fully sick-listed patients at 4 weeks, 6 and 12 months FU | Significant advantage at 4 weeks FU for A vs B (30% vs 57%), at 6 months (11% vs 62%), and at 12 months (19% vs 59%). |
| Bendix et al., 1995, 2000, 1998 (Denmark) (22–24) | 132 patients with disabling NSLPB > 6 months, threatened job situation or out of work | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-h day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Active physical training: Two sessions a week for 6 weeks, consisting of 45 min aerobics class, 45 min progressive resistance training, and 1 h of theoretical back lessons every second session: (SD, SE, LD, MxE, OP, WCn, BTn) C: Psychological pain management: 2 sessions lasting 75 min, twice a week for 6 weeks., combining active physical training of 15 min warm-up exercises, and 30 min progressive resistance training with psychological pain management: (SD, SE, LD, MxE, OP, WCn, BTy) | Sick days (median, IQR) and work capability as judged by a physician at 4 and 13 months FU | Sick days: significant advantage after 4 months for A and B vs C. A: 25 (0–103), B: 13 (0–122), C: 122 (60–122), and after 13 months for A vs B and C and for B vs C. A: 52 (0–127), B: 100 (0–390), C: 295 (0–390). Significantly better work capability in A vs B and C after 4 months (A: 75%, B: 48%, C: 40%) and 2 years (A: 80%, B: 55%, C: 44%) |
| Bendix et al., 1998, 1996 (Denmark) (24, 25) | 106 patients with
> 6 months of disabling back pain, age 18–59 years | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by 1 6-hour day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Usual care | Sick days (median, IQR) and work capability as judged by a physician at 4 months and 2 years FU | Sick days: significant difference at 4 months FU. A: 10 (0–122), B: 122 (24.5–122). Work capability: significantly larger improvement at 4 months. A: from 27% to 64%, B: from 16% to 29%. No difference after 2 years. A: 52%, B: 51% |
| Bendix et al., 2000 (Denmark) (26) | 138 patients, precarious work situation due to NSLPB | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-hour day weekly for the subsequent 2 weeks, and a third day after 2nd month: (ID, SE, HD, MxE, OP, WCy, BTy) B: Outpatient intensive physical training: aerobics and strengthening exercises for 1.5 h 3 times/week for 8 weeks: (SD, SE, HD, MxE, OP, WCn, BTn) | Sick days (median, IQR) and work capability as judged by a physician at one year FU. No statistical comparison between groups. Results disregard 32 of 138 randomized patients who did not finish treatment | Sick days: No difference at 1 year FU. A: median in 34/48 patients 5.5 (0–113), B: median in 40/50 patients 2.5 (0–301). Work capability: pre-post A: from 28 to 36/48, B: from 21 to 35/51 |
| Hagen et al., 2000, 2003 (Norway) (27, 28) | 457 patients with NSLPB and sick leave 8–12 weeks, age 18–60 years | A: Light mobilization programme: examination at spine clinic for 1 hour, information, advice to stay active and go on daily walks; individual instructions lasting 1–1.5 h on stretching and training at home by the physical therapist: (ID, HE, LD, ScE, OP, WCn, BTy) B: Usual care by GP | Days of sickness compensation (mean, 95% CI), numbers of workers returning to full-duty work at 3, 6, 12, 24, and 36 months FU | Significant fewer sick days at one year FU in A vs B (A: 95.5, 104.5, B: 133.7, 112). RTW: significant improvement after 6 months in A vs B (A: 61.2 %, B: 45.0 %) and 1 year (A: 68.4 %, B: 56.4 %). No significant difference at 3-year FU (A: 36.2%, B: 38.2%) |
| Table II. Study characteristics |
| Study | Participants | Interventions (exercise characteristic classification) | Work disability outcomes and terms of follow-up | Results |
| Alaranta et al., 1994 (Finland) (20) | 293 patients with NSLPB > 6 months, age 30–47 years | A: Akseli Programme: 3 weeks, 37 h/week of guided or self-controlled physical exercise, 5 h/week cognitive-behavioural disability management groups, no passive treatments: (ID, SE, HD, MxE, IP, WCy, Bty) B: Current national type of inpatient rehabilitation: 3 weeks, 15–20 h/week physical activity, large amount of passive treatments: (ID, SE, HD, MxE, IP, WCn, BTn) | Number of subjects with more than 30 sick days at one year FU | No difference regarding sick leave (A: 26%, B: 23%) after one year |
| Aure et al., 2003 (Norway) (21) | 49 patients sick-listed 8–24 weeks due to NSLPB, age 20–60 years | A: Manual therapy and specific exercise: 16 session lasting 45 min including spinal manipulation, specific mobilization, and stretching techniques as well as 5 general and 6 specific localized exercises for spinal segments and pelvic girdle, individual home exercises: (ID, SE, LD, SaE, OP, WCn, BTn) B: Supervised exercise therapy: 16 sessions consisting of 10 min warm-up on an exercise bicycle and 35 min. exercise session for the trunk, and lower limb muscles, suited to the clinical findings, individual home exercises: (ID, SE, LD, MxE, OP, WCn, BTn) | Proportion of partly or fully sick-listed patients at 4 weeks, 6 and 12 months FU | Significant advantage at 4 weeks FU for A vs B (30% vs 57%), at 6 months (11% vs 62%), and at 12 months (19% vs 59%). |
| Bendix et al., 1995, 2000, 1998 (Denmark) (22–24) | 132 patients with disabling NSLPB > 6 months, threatened job situation or out of work | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-h day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Active physical training: Two sessions a week for 6 weeks, consisting of 45 min aerobics class, 45 min progressive resistance training, and 1 h of theoretical back lessons every second session: (SD, SE, LD, MxE, OP, WCn, BTn) C: Psychological pain management: 2 sessions lasting 75 min, twice a week for 6 weeks., combining active physical training of 15 min warm-up exercises, and 30 min progressive resistance training with psychological pain management: (SD, SE, LD, MxE, OP, WCn, BTy) | Sick days (median, IQR) and work capability as judged by a physician at 4 and 13 months FU | Sick days: significant advantage after 4 months for A and B vs C. A: 25 (0–103), B: 13 (0–122), C: 122 (60–122), and after 13 months for A vs B and C and for B vs C. A: 52 (0–127), B: 100 (0–390), C: 295 (0–390). Significantly better work capability in A vs B and C after 4 months (A: 75%, B: 48%, C: 40%) and 2 years (A: 80%, B: 55%, C: 44%) |
| Bendix et al., 1998, 1996 (Denmark) (24, 25) | 106 patients with
> 6 months of disabling back pain, age 18–59 years | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by 1 6-hour day weekly for the subsequent 3 weeks: (ID, SE, HD, MxE, OP, WCy, BTy) B: Usual care | Sick days (median, IQR) and work capability as judged by a physician at 4 months and 2 years FU | Sick days: significant difference at 4 months FU. A: 10 (0–122), B: 122 (24.5–122). Work capability: significantly larger improvement at 4 months. A: from 27% to 64%, B: from 16% to 29%. No difference after 2 years. A: 52%, B: 51% |
| Bendix et al., 2000 (Denmark) (26) | 138 patients, precarious work situation due to NSLPB | A: Functional restoration: full-time intensive 3-week multidisciplinary programme for 39 h per week, including active physical and ergonomic training and psychological pain management, followed by one 6-hour day weekly for the subsequent 2 weeks, and a third day after 2nd month: (ID, SE, HD, MxE, OP, WCy, BTy) B: Outpatient intensive physical training: aerobics and strengthening exercises for 1.5 h 3 times/week for 8 weeks: (SD, SE, HD, MxE, OP, WCn, BTn) | Sick days (median, IQR) and work capability as judged by a physician at one year FU. No statistical comparison between groups. Results disregard 32 of 138 randomized patients who did not finish treatment | Sick days: No difference at 1 year FU. A: median in 34/48 patients 5.5 (0–113), B: median in 40/50 patients 2.5 (0–301). Work capability: pre-post A: from 28 to 36/48, B: from 21 to 35/51 |
| Hagen et al., 2000, 2003 (Norway) (27, 28) | 457 patients with NSLPB and sick leave 8–12 weeks, age 18–60 years | A: Light mobilization programme: examination at spine clinic for 1 hour, information, advice to stay active and go on daily walks; individual instructions lasting 1–1.5 h on stretching and training at home by the physical therapist: (ID, HE, LD, ScE, OP, WCn, BTy) B: Usual care by GP | Days of sickness compensation (mean, 95% CI), numbers of workers returning to full-duty work at 3, 6, 12, 24, and 36 months FU | Significant fewer sick days at one year FU in A vs B (A: 95.5, 104.5, B: 133.7, 112). RTW: significant improvement after 6 months in A vs B (A: 61.2 %, B: 45.0 %) and 1 year (A: 68.4 %, B: 56.4 %). No significant difference at 3-year FU (A: 36.2%, B: 38.2%) |
| Härkäpää et al., 1989, 1990 (Finland) (29, 30) | 476 blue-collar workers, age 35–54 years, sick leave due to NSLPB during
the last 2 years | A: Inpatient rehabilitation: groups of 6–8 patients, 3 weeks, 4 sessions Swedish back school, 15 back exercise sessions, 9 relaxation sessions, heat or electrotherapy prior to exercise, 2 structured group discussions, home programme, rehearsal after 1.5 years (2 weeks): (SE, MxE, IP, WCn, BTn) B: Outpatient treatment at the workplace or local health centre: 15 sessions in 2 months, groups of 6–8 patients, 4 sessions Swedish back school, 15 back exercise sessions, 9 relaxation sessions, heat or electrotherapy prior to exercise, 2 structured group discussions, home programme, rehearsal after 1.5 years (8 sessions): (SE, MxE, OP, WCn, BTn) C: Physician examination: no systematic treatment, written and oral instructions on back exercises and ergonomics. | Sick days at 15 months FU disregarding the first 7 days of each episode of sickness absence leading to a considerable underestimation of the days lost from work | Sick days after 1.5 years: A vs C no difference. (A: 5.5, 25; C: 7.5, 25). B vs C no difference (B: 5.8, 25, C: 7.5, 25.0). A vs B no difference (A: 5.5, 25.0, B: 5.8, 25.0) |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| |
Fig. 1. Trial flow diagram to summarize the stages of the systematic review.
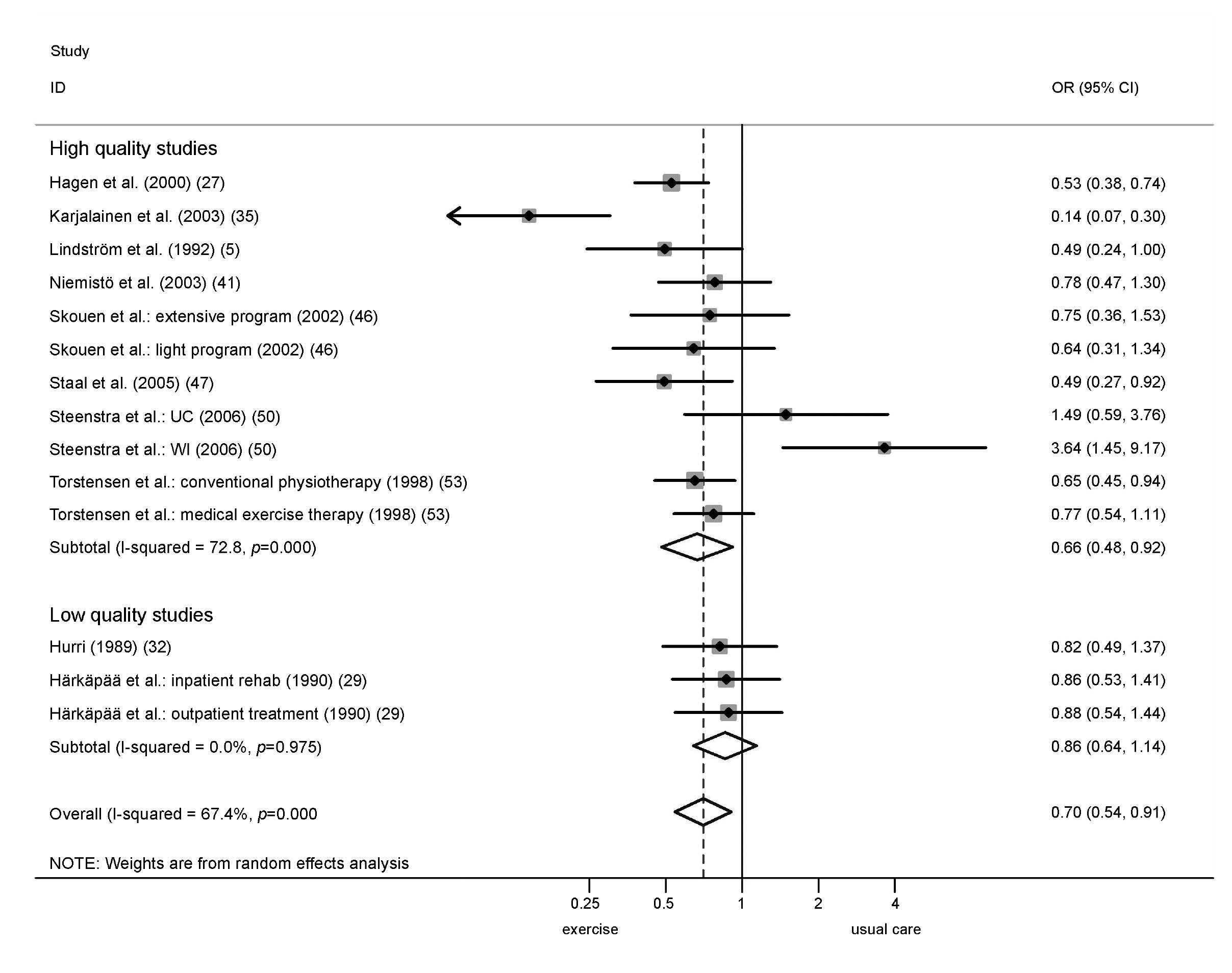
Trials comparing 2 different exercise interventions with usual care were treated as 2 trials with the sample size of the usual care group equally divided between the 2 exercise intervention groups: inpatient rehabilitation and outpatient treatment (29); low and high intensity back school (31); light and extensive multidisciplinary programme (46); conventional physiotherapy and medical exercise therapy (53). One study (50) presented results of 2 patient groups defined by the previous intervention (UC: usual care; WI: workplace intervention) receiving the same exercise intervention.
Validity assessment
According to the previously mentioned criteria, 14 (61%) of the studies were found to be of high quality and 9 (39%) of low quality (Table III). The 3 studies excluded from meta-analysis were all of low quality.
| Table III. Risk of bias and study quality |
| Study, reference | Risk of bias | Study quality |
| Selection bias | Detection bias | Attrition bias |
| Alaranta et al., 1994 (20) | Yes | No | Yes | Low |
| Aure et al., 2003 (21) | No | Yes | No | High |
| Bendix et al.,1995 (22–24) | Yes | Yes | Yes | Low |
| Bendix et al.,1996 (24, 25) | Yes | Yes | Yes | Low |
| Bendix et al., 2000 (26) | Yes | Yes | Yes | Low |
| Hagen et al., 2000 (27, 28) | No | No | No | High |
| Härkäpää et al., 1989 (29, 30) | Yes | No | Yes | Low |
| Heymans et al., 2006 (31) | No | No | No | High |
| Hurri, 1989 (32) | Yes | Yes | No | Low |
| Jousset et al., 2004 (32) | Yes | Yes | Yes | Low |
| Kääpa et al., 2006 (34) | No | Yes | No | High |
| Karjalainen et al.,2003 (35, 36) | No | Yes | No | High |
| Kool et al., 2005 (37, 38) | No | No | No | High |
| Lindström et al., 1992 (5, 39, 40) | No | No | No | High |
| Niemisto et al., 2003 (41, 42) | No | Yes | No | High |
| Petersen et al. 2002 (43, 44) | No | Yes | No | High |
| Roche et al., 2007 (45) | Yes | Yes | No | Low |
| Skouen et al., 2002 (46) | No | No | Yes | High |
| Staal et al., 2004 (47–49) | No | No | No | High |
| Steenstra et al., 2006 (50, 51) | No | No | No | High |
| Storheim et al., 2003 (52) | No | No | No | High |
| Torstensen et al., 1998 (53) | No | No | No | High |
| White, 1966 (54) | Yes | Yes | Yes | Low |
Work disability data
Data on work disability varied between the different studies and included self-assessed work ability, days of sick leave, days at work, physician’s judgement of work capability, and days of sickness compensation or numbers of workers returning to full-duty work. These were obtained from insurance databases whereby national legal requirements may have influenced the recordings. The data used for pooling were the number of people who returned and did not returned to work at the time of the follow-up, or the total number of sick days within the follow-up period (Table II).
Exercise characteristics
Thirty-five different exercise interventions were used. Exercise design, dose and setting were reported unclear in 6% of the investigated exercise interventions. Twenty-six (74%) of the exercise interventions were individually designed; 32 (91%) were primarily performed as supervised exercise; 28 (80%) interventions used mixed exercise types, 2 stabilization, 3 strengthening, 1 mobilization, and 1 stretching exercise; 27 (77%) were conducted in an outpatient setting; 10 (29%) were work-related; and 14 (40%) of the exercise interventions were administered within a cognitive behavioural approach (Table II).
Unfortunately, none of the studies using home exercise reported adherence rate or sufficient information to estimate home exercise dose. Therefore, the calculation of the exercise dose is based on the number of the supervised treatment sessions and their duration only. Such calculated exercise dose varied widely between the different exercise interventions, ranging between 1.5 and 210 h. The median exercise dose was 17 h. We classified exercise interventions with ≥ 17 h of contact time as high-dose exercise (n = 18), and those with less than 17 h of contact time into low-dose exercises (n = 17). A cut-off point of 14 and 20 h resulted in less than a 10% change in exercise dose classification.
Qualitative comparison of exercise interventions and usual care
Seven studies reported work disability data on a short-term follow-up. Two high-quality studies (5, 27) and 2 low-quality studies (25, 54) reported a positive effect, 1 high-quality study no effect (52) and 2 high-quality studies a negative effect (31, 50). Five studies reported work disability data on an intermediate-term follow-up. Three high-quality studies (5, 27, 47) reported a positive effect. This was observed in the study by Staal et al. (47) from approximately 50 days after randomization onwards. Two high-quality studies reported a negative effect (31, 50). Long-term results were presented by 11 studies. Positive effects were found in 3 high-quality studies (5, 27, 35). No significant effects were observed in 3 low-quality studies (25, 29, 32) and 4 high-quality studies (41, 46, 47, 53). One high-quality study reported a negative effect (50).
Quantitative data synthesis
Comparison of exercise interventions vs usual care. Thirteen studies allowing 17 comparisons between an exercise intervention and usual care with a total of 3181 patients were available for pooling.
Comparison 01: Short-term follow-up. Short-term results were available for pooling from 5 high-quality studies (6 comparisons, 1030 patients) (5, 27, 31, 50, 52), showing no significant effect of exercise reducing work disability (OR = 0.80, 95% confidence interval (CI) 0.51–1.25). The addition of one low-quality study (54) did not substantially change the overall effect estimate (OR = 0.68, 95% CI 0.42–1.10)
Comparison 02: Intermediate-term follow-up. Four high-quality studies (5 comparisons, 971 patients) (5, 27, 31, 50) provided results for pooling at the intermediate-term follow-up showing no significant effect of exercise in reducing work disability (OR = 0.78, 95% CI 0.45–1.34).
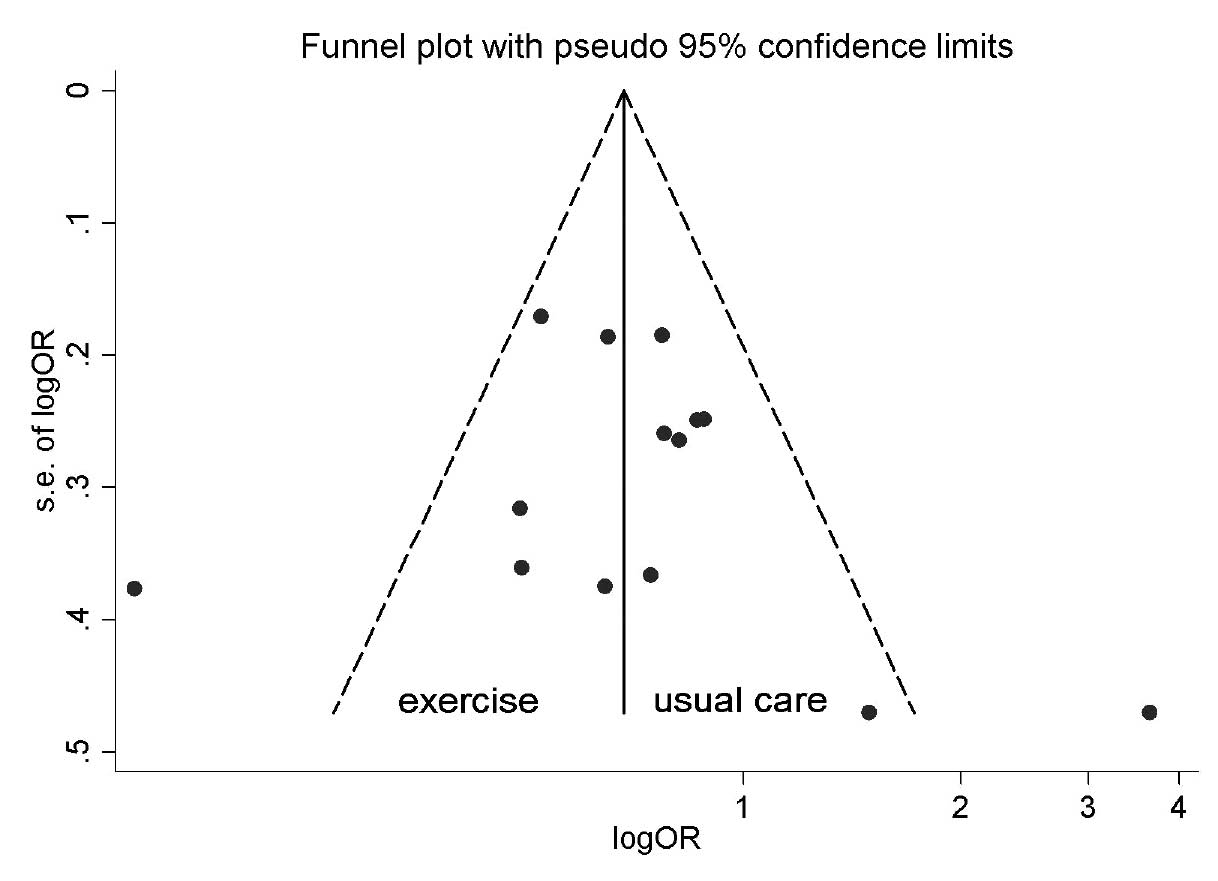
Comparison 03: Long-term follow-up. Eight high-quality studies (10 comparisons, 1992 patients (5, 27, 35, 41, 46, 47, 50, 53) presented long-term follow-up results showing a statistically significant overall effect in favour of exercise on work disability (OR = 0.66, 95% CI 0.48–0.92). The addition of 2 low-quality studies (29, 32) did not substantially change the overall effect estimate (OR = 0.70, 95% CI 0.54–0.91) (Fig. 2). The funnel plots did reveal evidence of asymmetry at short- and intermediate-term follow-ups but not at long-term follow-up (Fig. 3).
Fig. 2. Meta-analysis of 10 trials with long-term follow-up comparing exercise interventions with usual care.
Fig. 3. Funnel plot of 10 trials with long-term follow-up comparing exercise interventions with usual care.
Comparison 04: Influence of exercise characteristics in high-quality trials with long-term follow-up. The 8 high-quality studies (5, 27, 35, 41, 46, 47, 50, 53) providing data on 1149 patients receiving an exercise intervention and 843 patients receiving usual care were included for this analysis. All comparisons were between different outpatient rehabilitation programmes, and all used individually designed exercises, in one comparison stretching exercises were instructed, another used stabilization exercise, and in the remaining 8 comparisons mixed exercises were used. A second overall analysis, which did not include the patient sample from the trial of Steenstra et al. (50) that had already received a workplace intervention (WI group), showed reduced statistical heterogeneity (I2 = 60.4%, p = 0.007) and increased the effect estimate (OR = 0.59, 95% CI 0.45–0.78). The effect of delivery type, exercise dose, work context and behavioural treatment approach was analysed with and without the WI group showing different results, although within the statistical error margin. Pooled effects for the 4 exercise characteristics hypothesized to influence work disability (delivery type, exercise dose, work context, behavioural treatment approach) became higher and more significant for supervised exercise, and a behavioural treatment approach. However, none of the variables were statistically significant in meta-regression analysis, although there was a trend observed favouring home exercises (p = 0.11) (Table IV).
| Table IV. Odds ratios for work disability stratified by exercise characteristics in 8 high-quality randomized controlled trials comparing exercise intervention with usual care |
| Exercise characteristics | Work disability
(WI group included) OR (95% CI) | Work disability
(WI group excluded) OR (95% CI) | Meta-regression
(WI group excluded) logOR (95% CI), p-value |
| Delivery type |
| Home exercises | 0.38 (0.17–0.84) | 0.38 (0.17–0.84) | 1.74 (0.86–3.55), p = 0.11 |
| Supervised exercise | 0.80 (0.58–1.11) | 0.70 (0.58–0.85) | |
| Exercise dose |
| Low dose (< 17 hours) | 0.51 (0.35–0.73) | 0.51 (0.35–0.73) | 1.52 (0.71–3.27), p = 0.24 |
| High dose (> 17 hours) | 1.01 (0.57–1.78) | 0.76 (0.56–1.05) | |
| Work context |
| No | 0.65 (0.54–0.77) | 0.65 (0.54–0.77) | 0.66 (0.27–1.59), p = 0.31 |
| Yes | 0.77 (0.21–2.85) | 0.46 (0.41–1.55) | |
| Behavioural treatment approach |
| No | 0.72 (0.57–0.91) | 0.72 (0.57–0.91) | 0.72 (0.33–1.56), p = 0.35 |
| Yes | 0.65 (0.39–1.10) | 0.52 (0.34–0.80) | |
| CI: confidence interval; OR: odds ratio; WI: workplace intervention. |
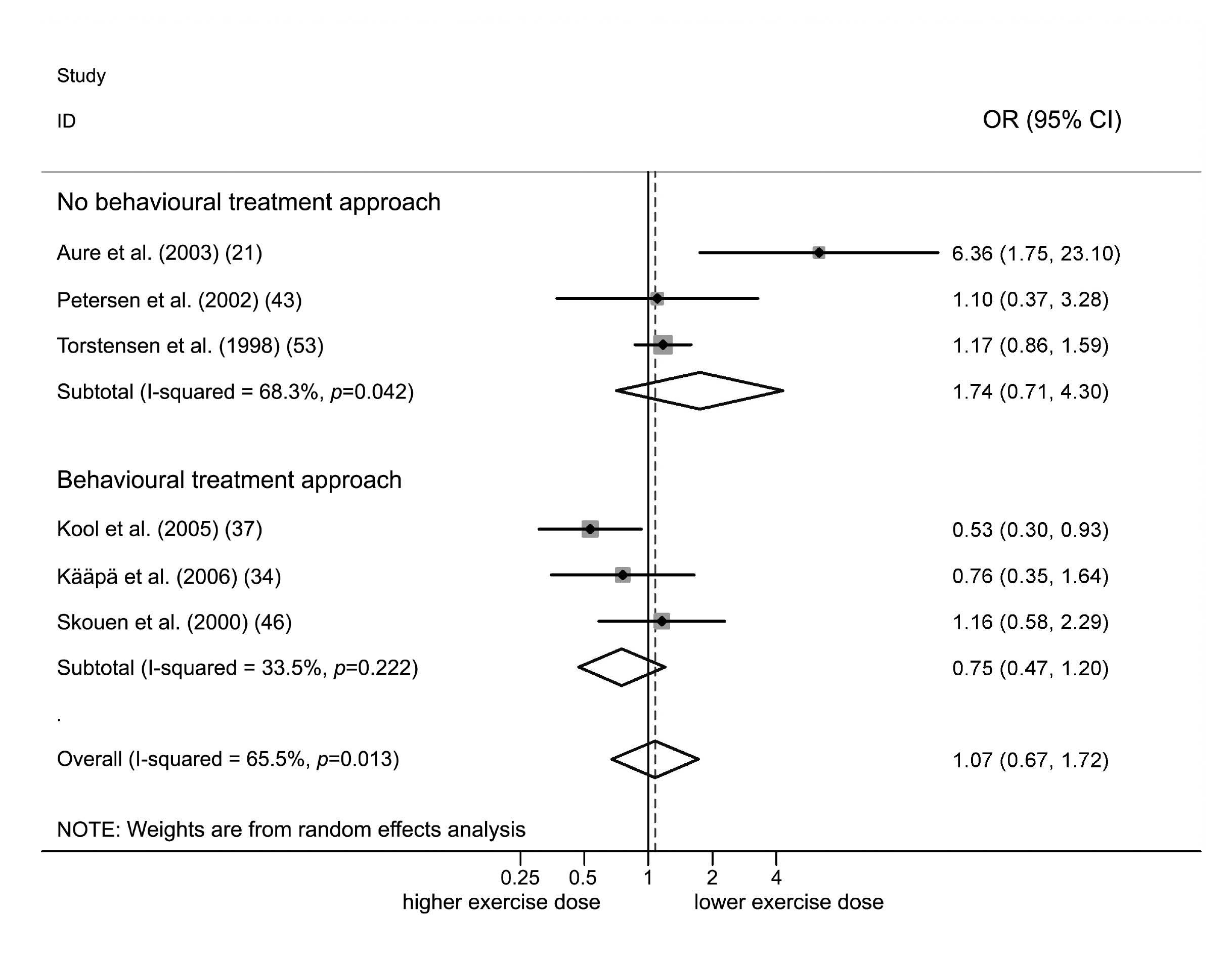
Comparison of different exercise interventions. Of the 13 studies comparing 15 different exercise interventions, 6 were of low quality (20, 22, 26, 29, 33, 45) and 7 were of high quality. Six high-quality studies presented long-term follow-up data and were used for pooling (21, 34, 37, 43 46, 53). We defined the exercise intervention with more contact hours as the standard intervention. All standard interventions used individually designed supervised exercises, 5 of them with mixed exercises, and 5 were conducted in an outpatient setting.
There was significant statistical heterogeneity in these trials (I-squared = 65.5%, p = 0.013). The overall effect of exercise interventions with more contact hours was not significant (OR = 1.07, 95% CI 0.67–1.72). Three trials applying exercise within a behavioural treatment approach showed some benefit (OR = 0.75, 95% CI 0.47–1.20) compared with the trials without this characteristic (OR = 1.74, 95% CI 0.71–4.30) (Fig. 4). One trial applying work-related exercise in an inpatient setting (42) showed a significant effect on work disability (OR = 0.53, 95% CI 0.30–0.93) compared with exercise not specifically designed to restore work-related physical capacity (OR = 1.25, 95% CI 0.80–1.97). None of these characteristics showed statistical significance in meta-regression analysis. The funnel plots that were conducted did not reveal evidence of funnel plot asymmetry.
DISCUSSION
This meta-analysis provides continuous support for the use of exercise interventions to achieve long-term benefits on work disability in patients with non-acute NSLBP. The OR of 0.66 suggests that the odds of “improvement” in work disability are in the long-term 34% lower if only usual care (rather than exercise) is given. No significant effect was observed in short- and intermediate-term follow-ups. Meta-regression showed no significant differences between different exercise types. Interestingly, home exercises seem to be at least as effective as supervised programmes. As the meta-regression is only explorative, no conclusions can be made regarding exercise types.
Our study has several strengths. The search strategy was based on the recommendations of the Cochrane Back Review Group. We planned the analysis a priori based on the findings of previous meta-analyses and assessed study quality based on key components of methodological quality (concealed allocation, blinded assessor, intention to treat analysis) as recommended by Juni et al. (13). Studies affected by biases have previously been shown to exaggerate treatment effects (13). We, therefore, excluded low-quality studies from meta-regression analysis in order to avoid a possible overestimation of the effect of different exercise characteristics.
A weakness of this study is the high proportion of total unexplained variance that could be attributed to study heterogeneity. We considered this weakness thoroughly, but concluded that patients, social support and outcomes showed satisfactory homogeneity. All but one of the studies were performed in Europe, in countries with comparable social systems. All patients were diagnosed with non-acute NSLBP, were of working age and available for the job market. Despite the wide variety of used work disability outcomes, this meta-analysis is based on the pooled results of just 2 different outcome measures. We performed a stratified analysis in 3 studies providing both outcome measures and found no relevant differences in ORs, both in favour of exercise. Furthermore, using mean values and standard deviations for further statistical analysis in data with a skewed distribution is usually regarded as inappropriate. Data regarding sick days have a skewed distribution, but this was similar in both groups in treatment comparisons that reduces the risk of systematic bias (55). To address the problem of statistical heterogeneity, we performed a random effects meta-analysis. There remains the possible error of substantial variation in standard deviations across studies leading to an over- or underestimation of the ORs.
Exercise interventions did not show a significant effect on work disability at short- and intermediate-term follow-up. However, these findings are not conclusive. The mean odds ratios for short- and intermediate-term results were both below unity, but with wide CI. Therefore, a significant effect might remain undetected based on ineffectiveness, heterogeneity or limited power of the pooled studies. Possible explanations for a lack of effect at short- and intermediate-term follow-up are the required time needed to improve physical capacity, to modify pain behaviour, or to search for work. Furthermore, the process of care has a substantial effect on work disability, as shown in a recent study comparing a graded activity programme with usual care (50). The interaction between a prior WI and graded activity, together with a delay in the start of the graded activity intervention, explained most of the delay in return to work (RTW) (50). This study introduced relevant clinical heterogeneity in this meta-analysis. All of the other trials investigated the primary treatments for this occurrence of back pain, while half of the patients in the trial from Steenstra et al. (50) had already received a WI, which has been shown to be effective on return to work (56). Herbert & Bo (57) propose that study quality can also be assessed on how interventions are administered. There were obviously problems in the implementation of the graded activity programme in the trial of Steenstra et al. (50), leading to a potentially false conclusion if the whole patient sample had been included in this meta-analysis. In view of these considerations we feel it legitimate to interpret the findings without the results of the WI group. The author’s recommendation of paying special attention to the structure and process of care in implementing graded activity (50) does have clinical relevance when conducting medical interventions aiming for early RTW. An open and fast access to such interventions prevents unnecessary waiting time before a RTW can be attempted. This might also be a possible explanation for why individually designed home exercises seem to be more effective than supervised exercise interventions in reducing work disability. Home exercise may facilitate RTW, as the patients are able to continue their daily routine without spending extra time on medical intervention.
Interestingly, this meta-analysis did not show a greater effect of higher dose exercise interventions (≥ 17 contact h) compared with lower dose exercise interventions on work disability (< 17 contact h). This finding is contrary to exercise physiology postulating a dose and effect relation (58), as well as to previous findings that only intensive (> 100 h of therapy) multidisciplinary biopsychosocial rehabilitation with functional restoration improves function in patients with chronic low back pain, whereby inconclusive results were found on vocational outcomes (59). The only study included in the systematic review by Guzman et al. (59) supporting the use of functional restoration to reduce work disability (25) is not included in the performed meta-regression, as only high-quality studies were used. Moreover, in the meantime new studies with low contact hours administering home exercise have been published showing a positive effect on work disability. This might, from our point of view, be an explanation for the different findings. However, a cautionary comment must be made on the missing effect of exercise dose found in this review. As in other systematic reviews, incomplete reporting in the primary studies present important limitations and prevented the calculation of the exercise dose in home exercise programmes. It must be assumed that the actual exercise dose in home exercise interventions was higher than the calculated dose.
We have not been able to confirm the positive effects of exercises performed within a behavioural treatment approach on work disability postulated in previous reviews (8, 9, 14). In the comparison of exercises with usual care we found stronger treatment effects for such exercises. However, this was not statistically significant in the meta-regression (Table IV). The missing confirmation might be due to the differing study inclusion criteria and the analysis performed. All previous reviews based their conclusion on a qualitative assessment, at least partly based on the evidence found by Lindström et al. (5). Hayden et al. (9) also included the results of Staal et al. (47), while Schonstein et al. 2003 (14) included the results of 3 more studies that were excluded from this analysis because of the risk of bias or missing inclusion criteria. We included in addition to the studies of Staal et al. (47) and Lindström et al. (5) the findings of 6 more studies (27, 31, 35, 47, 50, 52) that contained 9 treatment comparisons with a total of 1316 patients providing sufficient power for the meta-regression. However, it must be emphasized that the presented meta-regression analyses is only explorative and does not allow any conclusions too be drawn.
Fig. 4. Meta-analysis of 6 high-quality trials comparing lower and higher dosed exercises at long-term follow-up without and with a behavioural treatment approach.
The comparison of different exercise interventions also did not reveal a significant effect of a behavioural treatment approach (Fig. 4). There might be a superior effect if exercises are performed within a behavioural treatment approach and are specifically designed to restore work-related capacity, as shown by the study of Kool et al. (38). This is also in line with Schonstein et al. (7), who hypothesize a positive effect of such a combination.
We recommend further evaluation of the combined effects of individually designed home exercises applied within a behavioural treatment approach aiming to specifically restore work-related physical capacity. Special attention must be given to an effective implementation process of exercise interventions aiming for early RTW.
ACKNOWLEDGEMENTS
This project was supported by the Swiss National Research Program NRP 53 “Musculoskeletal health – Chronic pain” of the Swiss National Research Foundation (Project 405340 – 111500/2). We thank all the authors of the primary papers who supplied additional information and Ariane Knüsel for her assistance in preparing the manuscript.
REFERENCES