As any patient may require rehabilitation and physical therapies, all physicians need to acquire at least a basic knowledge of Physical and Rehabilitation Medicine (PRM). In 2005 PRM teaching was implemented in all phases of the curriculum for medical students in Germany. The curriculum includes, among others, the following topics: principles of rehabilitation; the model of the International Classification of Functioning, Disability and Health (ICF); principles and effects of physiotherapy and occupational therapy; indications and contraindications for PRM interventions. Teaching of PRM topics is implemented from the first week in all phases of the curriculum, as: (i) lectures in the module “Introduction to Medicine (Propaedeuticum)”; (ii) a cross-sectional course entitled “Rehabilitation, Physical Medicine and Naturopathic Treatment (RPMN)”; (iii) single lectures on PRM in other fields; (iv) elective mandatory courses on the social model of rehabilitation, balneology, and others; and (v) the option to choose PRM as a subject for practical training. All modules are evaluated regularly by the students. Global ratings of the module “Propaedeuticum” were good, and of the cross-sectional course “RPMN” very good. The advanced part of the practical training was rated highly by the students. In conclusion, the implementation of teaching of PRM and other rehabilitation topics in undergraduate medical education is a successful concept that fulfils the criteria for education in medical school set out by the American Association of Academic Physiatrists.
Key words: undergraduate medical education; medical school; curriculum; rehabilitation; physical and rehabilitation medicine; programme evaluation.
J Rehabil Med 2010; 42: 206–213
Correspondence address: Prof. Dr. Christoph Gutenbrunner, Department for Rehabilitation Medicine, Coordination Centre for Rehabilitation Research, Hannover Medical School, Carl-Neuberg-Str. 1, D-30625 Hannover, Germany. E-mail: gutenbrunner.christoph@mh-hannover.de
Submitted August 19, 2009; accepted November 25, 2009
INTRODUCTION
Rehabilitation plays an increasing role in the medical system. According to the World Health Organization (WHO) definition, rehabilitation comprises: “the use of all means aimed at reducing the impact of disabling and handicapping conditions and at enabling people with disabilities to achieve optimal social integration” (1). In medicine, rehabilitation provides interventions to promote physical and cognitive functioning, activities and behaviour, participation and health-related quality of life, as well as modifying personal and environmental factors (1, 2). This requires preventive measures, setting a diagnosis, assessing functions, providing treatments and rehabilitation management, and is needed for people with disabling medical conditions and co-morbidities across all age groups (1). Modern concepts of rehabilitation make clear that rehabilitation may be necessary in all kinds of medical conditions, and is of importance in almost all medical care settings (e.g. acute hospitals, post-acute care, out-patient services, general practice, nursing homes) (3).
As any patient may require rehabilitation, all physicians need to acquire at least a basic knowledge of rehabilitation, whilst recognizing that most will not practise as specialists in the field or carry out specific rehabilitation measures (2). Another important aspect is the prescription of physiotherapy, occupational therapy and other physical therapies, which will be a task performed by most doctors. For this, knowledge of mechanisms, effects, indications, contraindications and dosage is essential. It is thus important that Physical and Rehabilitation Medicine (PRM) is taught in all undergraduate medical faculties (4–9).
The White Book for Physical and Rehabilitation Medicine in Europe (2) defines a number of topics as minimum requirements. These topics should be taught systematically by experienced academic specialists in PRM (10, 11). Of course, rehabilitation issues are also of relevance in other fields of medicine and should be included in the teaching of concepts in these fields. Until 2009 in Germany PRM as a medical field has not been an obligatory part of medical training at all universities and medical schools and no standardized concepts and curricula exist (12–14). However, in some countries PRM is already an obligatory part of medical training (e.g. Australia, Belgium, Canada, France, Spain, Sweden, UK, USA), and some publications suggest standardization of the curricula at a national level (15).
In Germany PRM was not a mandatory or specific topic in medical faculties for many years. However, since the 9th revision of the national rules for undergraduate medical education (Approbationsordnung) in 2003 (16), rehabilitation and physical medicine have been mandatory subjects in undergraduate medical education. They are included as the (main) part of a cross-sectional field called “Rehabilitation, Physical Medicine and Naturopathic Treatment” (RPMN)1. At the same time, knowledge of rehabilitation is defined as a global aim of the medical curriculum, together with prevention, knowledge of body functions, psycho-social influences on health, and coping with the consequences of diseases (16). Thus, in 2004, after implementation of the new rules at Hannover Medical School, a concept of teaching a cross-sectional field of RPMN was developed, and 2 years later, when a model curriculum had been implemented, the more comprehensive concept of implementing the teaching of rehabilitation issues in all stages of the curriculum was put into practice (17). The aim of this paper is to describe this concept, and discuss the results of evaluation of the classes.
1The term “naturopathic therapies” in Germany is used for a wide range of therapies, including thermotherapy, massage, herbal medicine, acupuncture and others.
Aims and concept
The aim of the concept is to implement the subject of PRM teaching into all phases of the curriculum for medical students, in mandatory and elective lectures and courses. The teaching programme should include both theoretical knowledge and practical skills. The concept focuses on patient-orientated learning, but must also be based on scientific evidence. The concept has to be developed within the framework of the Hannover model curriculum “Medicine”, as described below. As the classes in rehabilitation are part of the main curriculum, and students have to undergo a written examination after the end of each course or module. All courses are evaluated with a standardized questionnaire.
In line with the White Book for Physical and Rehabilitation Medicine in Europe (2) the objectives for the curriculum were defined as:
• principles of rehabilitation based on the model of the International Classification of Functioning, Disability and Health (ICF);
• principles and effects of physiotherapy, occupational therapy and other physical therapies (including an overview of methods used by therapists);
• teamwork and communication with therapists;
• indications and contraindications for PRM interventions in patients with special conditions (e.g. stroke, multiple trauma, low-back pain, arthritis, cancer, etc.);
• principles, effects, indications and contraindications for comprehensive rehabilitation programmes;
• organization and practice of rehabilitation system (acute and post-acute rehabilitation, as well as rehabilitation programmes for patients with chronic conditions);
• knowledge of the social system and legislation concerning disability and rehabilitation at the national level, as well as ethical and human rights issues in rehabilitation.
These topics should not only be taught in theoretical lessons, but based on practical experience and active participation in therapeutic techniques. The students should actively apply the knowledge in patient cases and learn to make patient-centred decisions in the rehabilitation process. All of these courses are given by, or are under the supervision of, the chair of rehabilitation medicine of Hannover Medical School.
HANNOVER MEDICAL CURRICULUM
The German rules for undergraduate medical education (16) include an option to establish so-called model-curricula for single faculties or medical schools. These model-curricula require the approval of the state’s ministry for education. In the academic year 2005/2006 a model curriculum was developed and implemented in Hannover Medical School (16). The model curriculum “Medicine” is based, among others, on the following basic principles:
• training for professional practice in medicine;
• integration of theoretical (e.g. physics, chemistry, physiology, anatomy) and clinical (e.g. internal medicine, surgery, paediatrics, rehabilitation medicine) subjects;
• spiral of learning (repetition of subjects at increasingly advanced levels);
• learning from example (lessons do not include all subject matter; some of it has to be learned by the students on their own);
• patient-orientated learning and bedside teaching even at an early stage;
• examinations integrated into each module (or, in longer modules, repeatedly within the module).
Of course, the principles of any academic curriculum are retained, e.g. the focus on scientific evidence and the goal of enabling the students to achieve independent and discriminating learning. The topics and subjects covered are in agreement with the national rules for undergraduate medical education (16). Due to the national rules, the sixth year of the course of studies is dedicated to practical training in the departments of the Hannover Medical School or other hospitals approved as so-called academic hospitals.
Rehabilitation courses in the Hannover medical curriculum
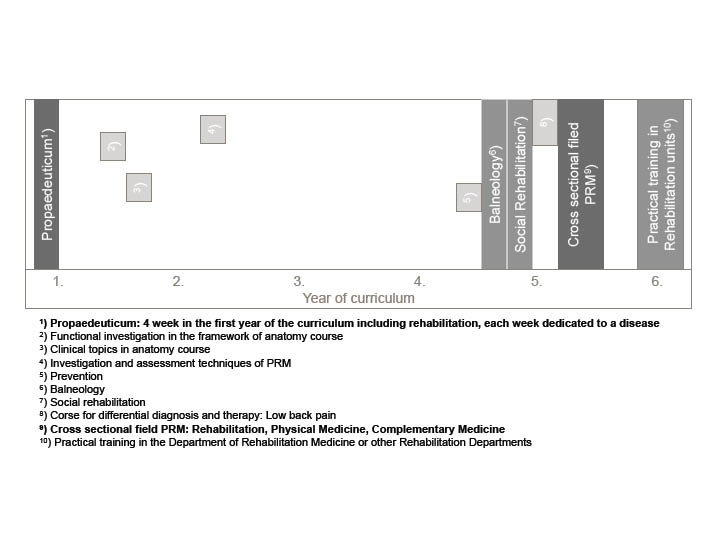
As mentioned above, the concept of implementing teaching of the field of rehabilitation medicine in the Hannover model curriculum “Medicine” aimed, on the one hand, to introduce the principles of rehabilitation as early as possible and with repeated reference to the subject, and, on the other hand, to provide in-depth work and some practical training in PRM. In addition, some courses for students with special interests were offered within the system of elective mandatory courses2. Fig. 1 provides an overview of the sequence.
2Each student must complete at least 2 elective mandatory courses during his or her degree.
Fig. 1. Overview of lectures and courses in the field of rehabilitation in the Hannover medical curriculum. PRM: Physical and Rehabilitation Medicine.
The Hannover medical curriculum includes the following courses and lectures in the field of PRM and related topics (Table I):
| Table I. Overview of lectures and courses in the field of rehabilitation in the Hannover medical curriculum. PRM: Physical and Rehabilitation Medicine. (Bold text: key course) |
| Year | Name | Course/ seminar/ lecture/ | Duration | Mandatory/ elective | Number of students | Examination | Remarks |
| 1 | Introduction to medicine (“Propaedeuticum” | Course | 4 weeks | Mandatory | ~ 260 | Written | Only part of it dealing with rehabilitation topics (see text) |
| Physical examination of the spine | Workshop | 3 hours | Mandatory | ~ 2 × 40 | No | Part of anatomy course |
| Shoulder pain | Lecture | 1 hour | Elective | ~ 260 | No | Part of anatomy course |
| 2 | Assessment in PRM | Lecture | 1 hour | Mandatory | ~ 260 | No | Part of course on diagnostic methods |
| 4 or
5 | Social rehabilitation | Course | 1 week | Elective mandatory course | ~ 10–12 | Written | |
| Balneology and medical climatology | Course | 1 week | Elective mandatory course | ~ 10–12 | Written | |
| Complementary medicine | Course | 1 week | Elective mandatory course | ~ 30–50 | Written | |
| 5 | Rehabilitation, physical medicine, naturopathic treatment | Cross-sectional course | 2 weeks | Mandatory | ~ 90, 3 times/year | Written | Theoretical teaching and hands-on workshops |
| Prevention of disabling conditions | Lecture | 1 hour | Mandatory | ~ 90, 3times/year | Part of examination | Part of course on prevention and health promotion |
| Treatment and rehabilitation of low-back pain | Lecture | 4 hours | Mandatory | ~ 90, 3 times/year | Part of examination | Part of course on differential diagnosis and differential therapy |
| 6 | PRM | Practical training | 4 months | Elective | ~ 6 per year | Practical and oral examination | For the students choosing this, PRM is part of the final examination |
• lectures on rehabilitation and PRM in the course “Introduction to medicine (Propaedeuticum)”, which teach the basic principles (including the ICF model) and some aspects of functional assessments and non-pharmacological treatments;
• a comprehensive cross-sectional course3 “Rehabilitation, Physical Medicine, Naturopatic Treatment”, which is a 2-week course including lectures, hands-on seminars and bedside teaching;
3The national rules for undergraduate medical education include 2 types of subjects: “fields”, e.g. internal medicine, dermatology, surgery, and “cross-sectional areas (or fields)”, e.g. prevention, epidemiology, emergency medicine.
• single lectures on PRM in other fields, such as anatomy, diagnostic methods, prevention, and clinical reasoning;
• elective mandatory 1-week courses on the social model of rehabilitation, balneology, and complementary medicine;
• the option to choose PRM as a subject for clinical training for one-third of the final year of the course of studies (at the Department for Rehabilitation Medicine of Hannover Medical School or other in-patient rehabilitation centres approved as academic training centres).
Introduction to medicine (“Propaedeuticum”)
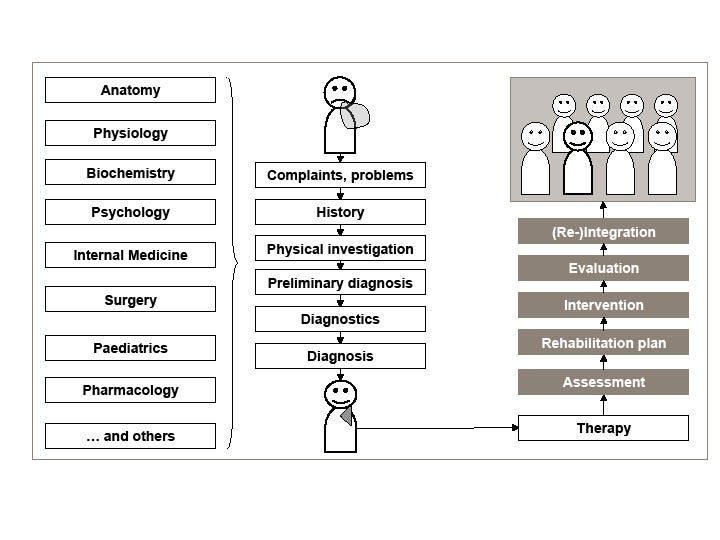
The course “Introduction to medicine” is the first module of the curriculum. The philosophy is to show students the blueprint of the entire curriculum and to demonstrate, by example, how a doctor solves a patient’s problem. This is done by demonstrating patients and taking their history. Additionally the need to study basic natural sciences as well as anatomy and physiology is demonstrated to the students (Fig. 2). Thirdly, the psycho-social context of the patient and his or her problems, and the rehabilitation and re-integration of the patient into life as core strategies of medicine, are discussed. The course is highly interdisciplinary, and each week is chaired by a specialist in the disease used as an example4. The topics covered during the 4 weeks are kidney disease, low-back pain, breast cancer and lung disease5.
Fig. 2. Scheme of the medical problem-solving process as shown to the students in the introduction to medicine.
4The professor for PRM is responsible for the overall organization.
5Chairpersons for each of the weeks are: Professor Hermann Haller, Nephrology (kidney diseases), Professor Christoph Gutenbrunner, PRM & Professor Reinhard Pabst, Anatomy (low-back pain), Professor Peter Hillemanns, Gynaecology and Obstetrics, & Professor Christoph Gutenbrunner, PMR (breast cancer), and Professor Tobias Welte, Pneumology (lung diseases).
Each topic is introduced by taking a patient’s history in front of the students, who are also encouraged to ask questions. The medical approach is then demonstrated, using a series of lectures given by experts in their fields. Basic sciences in relation to the disease are also taught. Students are set homework related to the main topic and to their own investigation into specified topics. From the second week students are involved in hands-on workshops and patient-centred seminars, e.g. on the first steps in clinical investigation (low-back pain), pain assessment (cancer), group-discussions with patients (cancer) and first steps towards bedside patient-interviews and assessment (lung diseases). Each week is followed by a written test (30 multiple-choice questions each) that must be passed before students enter the second year of the curriculum.
The following topics in rehabilitation medicine were included:
• basic principles of rehabilitation;
• the patients’ view of rehabilitation (patient interview);
• the ICF model;
• physical medicine interventions in low-back pain;
• experience with physical medicine interventions;
• rehabilitation in breast cancer.
In addition, a 2-page questionnaire is handed to the students to be used as the basis of an interview with a patient. The questionnaire contains 4 items, on each of the ICF categories: body functions, activities, participation, and contextual factors. Simple 2-step (contextual factors) or 3-step scales are given. The students can also add other domains and give comments on the questionnaire. The students are not restricted as to the type of patient they interview, but have to indicate diagnosis and type of interview (face-to-face, telephone). The results of the questionnaire are discussed in the lecture hall the following day.
Cross-sectional course on PRM
The cross-sectional course on RPMN deals mainly with PRM (the topics of complementary medicine and balneology are taught in separate elective mandatory courses (Table I). The contents are in line with the catalogue published by the national PRM society (19). A textbook written specifically for this course is available (20). However, due to the rules of the Hannover model curriculum not all of the topics relevant for the examination are discussed in detail within the lectures and seminars, but the students receive a catalogue covering all subjects included in the final examination.
The module is a 2-week course, with lectures in the morning and hands-on workshops (6–9 students) in the afternoon. Examples of some of the mandatory topics included in the lectures are:
• pain;
• de-conditioning;
• physical treatments, such as lymphotherapy, electrotherapy;
• rehabilitation in acute hospitals;
• dysphagia management;
• types of rehabilitation measures in Germany;
• assessments in rehabilitation.
The hands-on workshops deal with topics such as:
• evaluation of muscle problems and treatment of trigger points;
• manual medicine;
• medical training;
• pool exercise;
• acupuncture;
• patient demonstrations;
• elective workshops (e.g. on hydrotherapy, relaxation techniques, PRM in incontinence).
These workshops are mandatory for all students and are organized in a rotation system. They are leaded by academic professors, other PRM specialists and residents.
In the second week a mandatory excursion to other specialized rehabilitation centres is part of the curriculum. This is of importance, as rehabilitation for patients with chronic conditions in Germany is performed mainly in such rehabilitation departments (21). Groups of 18–20 students visit departments for orthopaedic rehabilitation, rheumatological rehabilitation, cancer rehabilitation or psychosomatic rehabilitation. In the course of these visits, besides lectures on the specific topic, the students evaluate patients, see group interventions and experience some specific treatment methods.
Elective mandatory courses and additional lectures in other disciplines
The elective mandatory 1-week courses and additional lectures in other disciplines cannot be discussed in detail here. Each course concludes with an examination. Topics included in the elective mandatory courses are:
• the social model of rehabilitation;
• rehabilitation in acute settings;
• balneology and medical climatology;
• complementary medicine.
Practical training in rehabilitation departments
As mentioned above, during the final year of the curriculum, practical training can be chosen in the Department for Rehabilitation Medicine of the Hannover Medical School or in-patient rehabilitation centres located in the Hannover area. These are specialized departments in the fields of rheumatology, orthopaedic surgery, oncology and psychosomatic medicine. The curriculum for the practical training includes:
• indications, contraindications and prescription of physical therapies (including physiotherapy, occupational therapy and others);
• rehabilitation system in Germany and advice to patients;
• investigation and assessment in PRM (history, physical investigation, imaging, laboratory tests, functional assessments and questionnaires as Barthel-Index, SF-36, Disability of the Arm, Shoulder and Hand Questionnaire (DASH), and others);
• set-up of an individual rehabilitation plan (including a written report);
• PRM in specific conditions.
The 4 months are structured in a standardized schedule, including practical experience with therapies, acute rehabilitation, PRM-consulting in intensive care units (ICUs) and other departments, out-patient care (musculoskeletal conditions, neurology and at least one of the special programmes performed in the department, e.g. hand rehabilitation, pelvic floor rehabilitation, vocational rehabilitation). The programme includes supervised care of at least 5 out-patients, including report, one case-report in the weekly seminars and a contribution to the journal club. Of course, the students also participate in all other conferences and seminars in the department.
As mentioned above, after every module students have to pass an examination in the topics of the lectures and seminars, as well as other topics listed in the curriculum. In order to continue their studies they must pass these examinations (the failure rate is 5–10%, and the examinations can be repeated). However, PRM (besides internal medicine and surgery) is part of the final examination only for students who undertook practical training in PRM. This examination includes history-taking and investigating a real patient, and a systematic oral examination with one-third of questions on the subject of PRM.
EVALUATION
Evaluation methods
All courses are evaluated using a standardized student questionnaire. This questionnaire must be completed after the written examination using the same electronic evaluation system used for the examination itself. However, students have the option to refuse to complete the evaluation questionnaire and the analysis of the data is anonymous. In courses without electronic examination a similar paper questionnaire is used. The questionnaire includes 7 questions, which are answered on a 6-point scale (1 = “I totally agree” to 6 = “I totally disagree”) and 2 15-point-scales (0 = “insufficient” to 15 = “very good”) (22). Among others questions the 6-point scales included, whether:
• the course/module helped me (e.g. by giving me new ideas);
• the course/module was efficient (compared with self-studies);
• complex problems had been explained in a clear way;
• the course/module referred well to practice/had enough practical elements;
• critical aspects have been mentioned.
The 15-point rating scales concerned a judgement of the lecturers and the global quality of the course or module. Free-text comments could be given via an internet platform (linked to the e-learning system).
Introduction into medicine (“Propaedeuticum”)
The global ratings of the module “Introduction into medicine (Propaedeuticum)” were good; 58.8% gave the module 11–15 points (“good”), 35.4% 6–10 points (“medium”), and 5.8% 0–5 points (“bad”). Although there were some differences between the 4 weeks of the module, these differences were small (medium differences below 1.0 points). The majority of critical comments on the internet platform concerned problems with organization (e.g. late issuing of learning material), the high level of the examination, or unclear questions. Some comments concerned an insufficient quality of single presentations and too high an amount of psychosocial aspects within the curriculum. The answers on the efficiency of the course showed good effects in all 4 weeks of the module.
Cross-sectional course on PRM
This course was rated even more positively; 73.0% rated it as “good” (11–15 points), 26.0 as “medium” (6–10 points) and 1.0% as “bad”. The advanced part of the practical training was highly rated by the students. The strong commitment of the teaching staff was stressed repeatedly in the internet forum. The 1-day visits to external rehabilitation centres were more controversial; some students stated that the time involved was too great compared with the outcome; others spoke very positively about the practical aspects learned on the visits. Due to an improvement in the organization of the course in December 2006 (e.g. clearer instructions for the excursions, an overview-lecture at the start, and a guided tour through the department) and more time for the hands-on workshops (including the possibility of choosing special-interest workshops) the ratings improved significantly. The examination level was rated as medium.
DISCUSSION
The need to implement rehabilitation in undergraduate medical education has been emphasized by international organizations (2, 4–11). Among the core arguments are the potential need for rehabilitation of large groups of patients to be cared for by doctors, and the human rights aspects of equal access to rehabilitation for people with disabilities. Studies show that, in many countries, rehabilitation is under-represented in undergraduate medical education (23–25). This is in coincidence with a lack of knowledge of PRM among general practitioners and insufficient awareness of the problems of people with disabilities (5, 9, 26). Studies show that knowledge of the potential of rehabilitation, as well as attitudes towards people with disabilities, can be improved by systematic teaching within medical schools (23, 27–30). However, theoretical courses alone are not appropriate to achieve such changes (26).
In Germany, the 9th revision of the rules for undergraduate medical education defined the acquisition of knowledge about rehabilitation as a general goal of medical education, and a mandatory so-called cross-sectional field “Rehabilitation, Physical Medicine, Natural Therapy” was defined. However, the way this has to be realized has not been defined up to now, and surveys show that the ways it is realized varies enormously from faculty to faculty (10). Some universities (e.g. Hannover, Munich, Jena, Freiburg, Halle, and Hamburg) developed systematic teaching concepts for the cross-sectional area, in many others the field is presented by external lecturers or specialists in other fields (e.g. orthopaedic surgery, trauma surgery, internal medicine).
In the international literature a few concepts for teaching rehabilitation issues and PRM in medical schools have been published, and the inclusion of PRM in all phases of the curriculum is called for (11). Most of them deal with the implementation of modules with theoretical and practical teaching (ranging from 1 to 4 weeks) (23, 27, 30). Some others implement PRM in clinical training programmes under the supervision of residents (26, 28, 31, 32). A few programmes are restricted to single lectures or a one-day teaching programme (29). As far as these programmes have been evaluated, an increase in knowledge within the field, and an improvement in awareness and change of attitudes towards people with disabilities could be shown (23, 27–30). However, none of these concepts takes a systematic approach to implementing PRM or rehabilitation in all phases of the undergraduate medical curriculum.
The concept described here is therefore the first to take a systematic approach throughout the entire medical curriculum and set up a “learning spiral”, from introducing the basics of rehabilitation at the very beginning of studies (10), via mentioning rehabilitation issues throughout the curriculum, to a systematic two-week teaching of PRM and practical training, in a similar way as has been done in other fields for a long time. For this reason it seems to be justified to call the concept the “Hannover model for the implementation of rehabilitation in the undergraduate medical training”.
However, despite obvious progress compared with former concepts, it still has some relevant limitations and needs further improvement. One of these limitations is the lack of introduction of new types of learning, such as problem-based learning, and modern methods of examination (27). This is due to the fact that the Hannover model curriculum was implemented without extending the teaching capacities of Hannover Medical School, and that the model curriculum is applied to all students and not only subgroups of students. For these reasons many lectures and even patient-interviews are performed in a class teaching manner with a large number of students. However, experience shows, that, especially in the first weeks and months of the course of studies, the students’ awareness even in such a setting is very high.
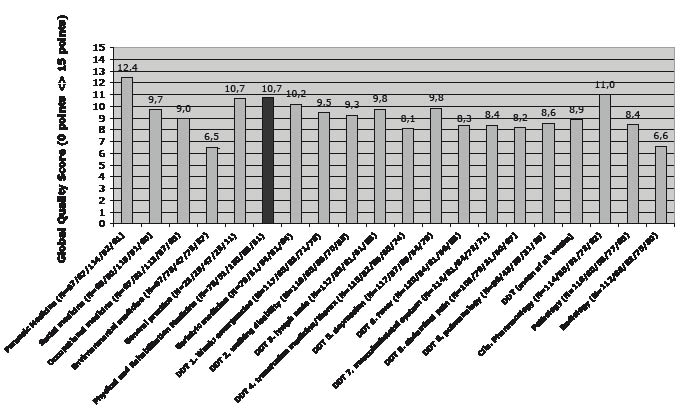
Systematic evaluation is crucial for all teaching activities and education programmes. In Hannover Medical School a standardized method has been established covering all courses and modules. The method is scientifically proven (20) and makes a benchmark possible, at least within the faculty. The results of the evaluation of 2 of the core courses show good to very good acceptance. The comparison of the evaluation results of all modules of the fifth academic year shows that PRM is rated high (rank 3 from 20) (Fig. 3). However, some negative ratings still have to be taken into account. The free-text answers give at least some insight into the students’ criticism, which is mostly about problems in course organization (e.g. late access to information, no organized transport to external rehabilitation centres) and, in a few cases, negative votes on the lecturers’ didactic skills. In order to implement improvements, the students’ comments are circulated to all lecturers and course organizers. In addition, a programme with didactic courses is now established at Hannover Medical School. Taking these remarks and reported experiences into account, changes were made to the courses that improved the students’ ratings.
Fig. 3. Comparison of the evaluation results of all modules in the fifth academic year. Score from 0 (“worse”) to 15 (“best”). Mean of five consecutive courses (academic year 2007–2009). DDT: differential diagnostics and differential therapy.
However, there are some limitations in this type of evaluation of courses and lectures. Students’ ratings may be influenced by factors other than the quality of teaching. Examples are: the kind of topic or field; external conditions; and the composition of the group of students. Further comparisons with other fields, and perhaps a benchmark with other faculties, should be carried out in future. In addition, it is clear, that evaluation of the quality of courses is not naturally correlated with good outcomes in terms of knowledge and professional skills of the graduates. An evaluation of parameters representing knowledge and professional skills should therefore be performed in the future.
In conclusion, the Hannover model to implement rehabilitation teaching in undergraduate medical education appears to be a successful concept and a great improvement over former curricula. It fulfils the requirements of a recent white paper on chronic care education in medical school (10). However, further attempts to improve these concepts are required, and a more comparative and comprehensive evaluation should be carried out.
REFERENCES