Winnie W. Y. Hung, MSc1,2 and Marco Y. C. Pang, PhD2
From the 1Physiotherapy Department, Kowloon Hospital, and 2Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Hong Kong, China
Winnie W. Y. Hung, MSc1,2 and Marco Y. C. Pang, PhD2
From the 1Physiotherapy Department, Kowloon Hospital, and 2Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Hong Kong, China
OBJECTIVE: To compare the effects of group-based and individual-based motor skill training on motor performance in children with developmental coordination disorder.
DESIGN: Randomized controlled pilot intervention study.
SUBJECTS/PATIENTS: Twenty-three children (4 girls) with develop- mental coordination disorder (mean age (standard deviation (SD)) 8 years (1 year and 2 months)).
METHODS: Twelve children were randomly assigned to undergo a motor training programme once a week for 8 consecutive weeks in a group setting, and 11 children received the same training on an individual basis during the same period. Each child was also instructed to perform home exercises on a daily basis. The Movement Assessment Battery for Children (MABC) was used to assess motor ability. Home exercise compliance and parental satisfaction with the programmes were also evaluated.
RESULTS: A significant reduction in the MABC total impairment score was found following both group-based (mean –4.4 (SD 5.0), p = 0.003) and individual-based training (mean –5.2 (SD 5.1), p = 0.016). However, the change in total impairment score did not differ significantly between the 2 groups (p = 0.379). There was similarly no significant between-group difference in home exercise compliance (p = 0.288) and parental satisfaction (p = 0.379).
CONCLUSION: Group-based training produced similar gains in motor performance to individual-based training. Group-based training may be the preferred treatment option due to the associated cost savings.
Key words: exercise; balance; motor; developmental coordination disorder; rehabilitation.
J Rehabil Med 2010; 42: 122–128
Correspondence address: Marco Y. C. Pang, Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Hong Kong. E-mail: rsmpang@inet.polyu.edu.hk
Submitted March 19, 2009; accepted October 19, 2009
INTRODUCTION
Approximately 6% of all school-aged children are affected by developmental coordination disorder (DCD) (1). The deficits in motor skills associated with this condition not only lead to unsatisfactory performance in daily activities, but may also have a negative impact on psychosocial domains (2–4). Without proper intervention, the problems that arise from DCD may persist into adolescence and adulthood (5, 6). Early intervention to enhance motor performance is thus important for children with the disorder.
Exercise training may be a viable way of improving motor skills in children with DCD (7–11). A frequently used approach is individual-based training, in which children with DCD receive 1-on-1 training from a therapist (7, 10, 11). An alternative approach is group-based training, in which several children are grouped together and participate in similar motor activities (8, 9). With the increasingly limited fiscal resources in the public health sector, group-based training may be an appealing approach if it can be proved to produce similar, if not better, outcomes.
A meta-analysis by Pless & Carlsson (12) showed that group-based therapy (effect size = 0.96) may be more effective than individual-based therapy (effect size = 0.45) in improving motor skills in children with DCD. However, the comparison between the 2 treatment delivery modes was based on separate studies with vastly different subject selection criteria, study designs, treatment approaches, and training protocols. To date, no study has directly compared the effects of group-based and individual-based motor skill training in school-aged children with DCD.
In this randomized controlled study, we aimed to compare the effects of group-based and individual-based motor skill training on motor performance in children with DCD. The motor skill training employed was a multi-dimensional exercise programme designed to target the various motor impairments commonly found in children with DCD (e.g. balance impairment, poor coordination of movement, poor core stability). As this was a pilot study, other issues such as compliance with the home exercises and parental satisfaction with the programmes were also explored. Such information should prove useful in the further development and implementation of motor skill training programmes for the DCD population.
METHODS
Study design
A randomized controlled pilot intervention trial was undertaken to compare the effects of group-based and individual-based motor skill training on motor performance in school-aged children with DCD. The outcome assessors were blinded to the group allocation, making this a single-blinded study.
Subjects
Children with DCD who were referred by the Child Assessment Centre to receive physiotherapy intervention at the Kowloon Hospital between May 2007 and December 2007 were recruited to participate in the study. The Child Assessment Centre is a government institution that provides assessment services for children in Hong Kong. To be included in the study, a child had to be aged between 6 and 10 years with a diagnosis of DCD. The diagnosis was determined following an assessment performed by an interdisciplinary team (comprising a paediatrician, a paediatric neurologist, a physiotherapist, an occupational therapist, and a clinical psychologist) at the Child Assessment Centre according to the criteria stated in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (1). These are: (i) motor coordination substantially below that expected for their age, with a gross motor composite score of < 42 as measured by the Bruininks-Oseretsky Test of Motor Proficiency (13); (ii) motor difficulties that significantly interfere with academic performance or activities of daily living; (iii) motor difficulties that cannot be explained by any medical or neurological disorders (e.g. cerebral palsy); and (iv) an intelligence level within the normal range. Children were excluded if they: (i) had received or were undergoing physical therapy or occupational therapy; (ii) had any profound visual or hearing deficiencies that could not be corrected by external devices; and (iii) demonstrated excessive disruptive behaviour. Each child referred to the Kowloon Hospital by the Child Assessment Centre was further screened by our research personnel using the Motor Assessment Battery for Children (MABC) (14). Children with an MABC total impairment score of greater than the 15th percentile (i.e. those that fell into the no motor difficulty category) were excluded.
A total of 29 children with DCD were referred to undergo physiotherapy intervention at the Kowloon Hospital by the Child Assessment Centre during the study period. Three refused to participate in the study. Three other children attained an MABC total impairment score of greater than the 15th percentile (i.e. no motor difficulty category) upon assessment (14), and were thus excluded from the study. As a result, 23 children with DCD enrolled in the study.
The study was explained to the potential subjects by our research personnel. If the parents and children agreed to participate in the study, they were asked to give their written informed consent. Ethics approval was obtained from the ethics committees of the Hong Kong Polytechnic University and the Kowloon Central Cluster of the Hospital Authority. All of the procedures were conducted in accordance with the Declaration of Helsinki.
Randomization
To ensure that the number of subjects in each group was approximately equal, the subjects were randomized by the drawing of a sealed opaque envelope containing a group code in blocks of 10. The randomization procedure was performed by a research therapist who was not involved in the assessment of the children. Twelve (2 girls) and 11 children (2 girls) were randomly assigned to the group-based and individual-based training programmes, respectively (Fig. 1).
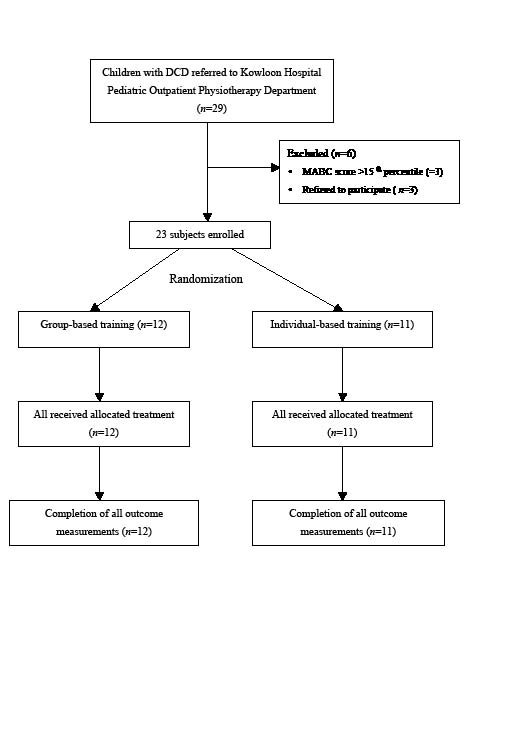
Fig. 1. CONSORT flowchart. DCD: developmental coordination disorder; MABC: Movement Assessment Battery for Children.
Intervention
The subjects underwent a weekly 45-min session of motor skill training held at the Pediatric Physiotherapy Outpatient Department of Kowloon Hospital for 8 consecutive weeks. The activities involved in the individual training and group training were essentially the same, and are outlined in Appendix I. A variety of functional tasks and exercises was designed to address common motor difficulties faced by children with DCD, such as agility, balance, core stability, and movement coordination. The same exercises listed in Appendix I were applied to both groups in each treatment session. As the training progressed, the motor tasks were adapted to ensure successful execution of the tasks while providing an adequate challenge to the child’s motor abilities. Such successful experiences induce feelings of joy and confidence, which may further motivate children to participate in the training (15). The child to therapist ratio was 4–6:1 for the group-based training and 1:1 for individual-based training. To maintain the consistency of the treatment approach, both the group-based and individual-based training were conducted by the same physiotherapist, who had many years of experience in paediatric rehabilitation.
Each subject was given home exercises to reinforce what had been learned at each session and to increase the exercise frequency. The home exercises were selected from among those used in face-to-face training sessions, and were intended to address the specific areas of motor difficulty experienced by each child. The children were instructed to perform these exercises on a daily basis within the study period. The parents were provided with clear written instructions, and were asked to coach or assist their children in performing the home exercises. The exercise programme was designed to take approximately 20 min to complete.
Outcome measures
Motor performance. Motor performance was evaluated using the MABC (14) within one week of the initiation of the intervention and again within one week of the termination of the 8-week training programme. Both assessments were performed by the same independent assessors, who were experienced paediatric physiotherapists and were blinded to the group assignment. The children and their parents were instructed not to inform the assessors of the group allocation or the type of treatment that they had received during the sessions. The outcome assessors were also instructed not to ask questions that might lead to the disclosure of the group assignment.
The MABC is a reliable and valid tool for evaluating motor performance in children aged between 4 and 12 years, and consists of 4 age-related batteries (14, 16, 17). Each battery has 8 motor tasks that measure 3 cluster areas of motor performance: manual dexterity (3 items), ball skills (2 items), and static/dynamic balance (3 items). The point scores for individual items were added to form 3 cluster scores. The sum of these cluster scores yielded the total impairment score, which ranged from 0 to 40, with a lower total impairment score indicating a higher motor competence level. The total impairment score was used to measure the treatment effectiveness, as it has been shown to have adequate sensitivity to detect change in motor ability level among children with DCD (16). To further ensure the reliability of our measurements, the intra-rater reliability and inter-rater reliability of the assessors were also investigated before the data collection. The intra-rater reliability was determined by asking the same 3 raters to assess the videotaped performances of 5 children with DCD twice over a 1–2-week interval. The inter-rater reliability was estimated by asking the same 3 independent raters to assess another 5 children with DCD simultaneously. The reliability coefficients obtained were all greater than 0.95, indicating excellent intra-rater and inter-rater reliability.
Home exercise compliance. A logbook was provided to parents for them to record on a daily basis (except for the days on which the face-to-face training sessions took place) whether their child had carried out the home exercise programme over the 8-week study period. The home exercise compliance rate (% days) was calculated using the following formula: (number of days of home exercise participation) × 100%/(total number of days).
Parental satisfaction. A parental satisfaction questionnaire was used to gather information on the perceived benefits of the motor skill training programmes (Table I). The questionnaire consisted of 2 parts, with part I (5 questions) and part II (8 questions) addressing the perceived benefits of the programme for the parents themselves and for the children, respectively. The parents were given the questionnaire at the end of the final training session and asked to indicate their level of satisfaction by rating each item on a 5-point Likert scale (5 = strongly agree; 3 = neither agree nor disagree; 1 = strongly disagree). The scores for the individual items were then summed and averaged to yield an overall satisfaction score, which was expressed as a percentage (%), with a higher percentage score representing a higher level of satisfaction. The therapist who conducted the training session was not present when the parents were completing the questionnaire. Upon completion, the questionnaires were collected by independent assessors.
Statistical analysis
Non-parametric statistic analysis was used due to the relatively small sample size. To ensure that the baseline parameters were comparable between the 2 groups, the Mann-Whitney U test (for age and total impairment score) and the χ2 test (for the proportion of boys and girls) were used.
To assess the effect of each type of intervention on motor performance (the within-group effect), Wilcoxon-signed rank tests were used to compare the MABC total impairment score and the subtest scores before and after the intervention for each group. The Mann-Whitney U tests were then used to compare the change in total impairment score and subtest scores (the post-test score minus the pre-test score) between the 2 groups (the between-group effect). As a higher total impairment score indicates more severe motor impairment, a more negative change in total impairment score represents a greater improvement in motor abilities. The Mann-Whitney U test was also used to compare the home exercise compliance rate and parental satisfaction scores of the 2 groups. The Spearman’s rho correlation coefficient was used to explore whether the change in total impairment score was associated with the baseline total impairment score or home exercise compliance rate. All of the statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) software program version 16.0. The level of significance was set at 0.05 (2-tailed). In addition, post-hoc power analysis was performed using the G*Power statistical software (Faul & Erdfelder, Bonn University, Germany, 1992).
RESULTS
There were no statistically significant differences between the 2 groups in age (group-based training group: mean 8 years and 4 months, SD 1 year and 2 months; individual-based training group: mean 7 years and 8 months, SD 1 year and 2 months) (p = 0.134), the proportion of boys and girls (p = 1.000), or the baseline MABC total impairment score (p = 0.608). All of the children in both groups completed the training programme with 100% attendance, and there were no drop-outs. No adverse events were reported during the study period.
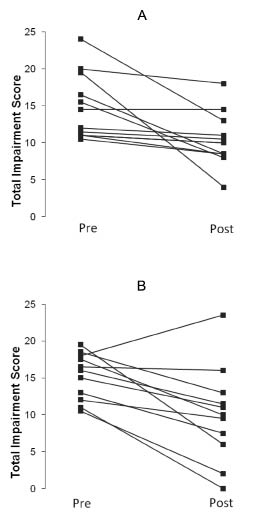
In the pooled data, a significant decrease in the total impairment score was found in both the group-based training group (mean –4.4 (SD 5.0), p = 0.003) and the individual-based training group following the intervention (mean –5.2 (SD#5.1), p = 0.016), indicating an improvement in motor performance (Table II). The change in total impairment score was not significantly different between the 2 groups (p = 0.379). Six of the children in each group attained a MABC score of greater than the 15th percentile (denoting no motor difficulty) post-intervention. The change in the motor proficiency of each child is shown in Fig. 2. Although the MABC total impairment score decreased for most of the children following individual-based training, it seems that in the group-based training group, those who had a higher initial total impairment score (more severe impairment) tended to experience a greater improvement than those who had milder motor impairment (Fig. 2). Indeed, the association between the MABC total impairment score at baseline and the change in total MABC score was not significant for the individual-based training group (p = –0.082, p = 0.811), but was marginally significant for the group-based training group (p = 0.542, p = 0.069).
Fig. 2. Motor performance before and after intervention (individual data). Change in total impairment score for (A) subjects who received group-based motor skill training and (B) subjects who received individual-based motor skill training. Each filled square represents the data of a single subject.
In examining the 3 cluster scores of the MABC (manual dexterity, ball skills, static/dynamic balance), it was found that both treatment groups showed significant improvement in manual dexterity (p < 0.05). In addition, the children in the individual-based training group showed a significant improvement in static/dynamic balance over time (p = 0.040). However, there was no significant between-group difference in the change in scores for the 3 subtests, indicating that the improvement in these 3 clusters was similar following the individual-based and group-based training.
Home exercise compliance was similar between the 2 groups (individual-based: mean 62.2% (SD 29.3%); group-based: mean 50.1% (SD 23.7%), p = 0.288). There was also no significant correlation between the home exercise compliance rate and the change in total impairment score following either group-based (p = –0.429, p = 0.164) or individual-based training (p = –0.037, p = 0.915). In terms of parental satisfaction (Table I), there was no significant between-group difference in the satisfaction score for each individual item (p > 0.200) or in the overall satisfaction score (p = 0.379).
Post-hoc power analysis
The standardized effect sizes based on the difference in change in motor proficiency between the 2 treatment approaches were 0.2, 0.1, 0.5 and 0.2 for the MABC manual dexterity, ball skills, and static/dynamic balance subtest scores and the total impairment score, respectively. These values represent a small-to-medium effect size. With an alpha value of 0.05 and a sample size of 12 and 11 children in each group, the magnitude of the corresponding statistical power was calculated to range from 0.1 to 0.2.
DISCUSSION
Group-based vs individual-based training
Our results show that the motor training programme administered in a group setting was as effective as that administered individually, based on both the objective measurement of motor performance and the subjective perception of the children’s parents. One explanation for the similar outcomes is that each treatment approach has its own unique merits that induce positive effects on motor proficiency. Although individual-based motor skill training is presumed to provide the maximum opportunity to practice motor skills with minimal waiting time and distractions from other children, group-based motor skill training may have its own advantages. First, the group setting provides opportunities for social interaction. Secondly, children are competitive, and this motivates them to perform better. Furthermore, a stronger sense of competence may be developed if a child can successfully demonstrate the acquired motor skills in front of his or her peers in the group. This perceived competence may further encourage the children’s participation in the training and in other physical activities affecting their motor competence (15, 18, 19). Comparable results for group-based and individual-based therapy have also been reported in research on other childhood diseases (20, 21). For example, children with cerebral palsy who underwent sensory-perceptual-motor training in an individual-based or group-based format had significantly better motor outcomes than controls (20). Group therapy has also been shown to be as effective as individual therapy in the management of childhood obesity (21). Although these studies show that both individual therapy and group therapy produce comparable results, some have found that the group setting may provide additional social benefits, as group interaction facilitates a child’s motivation to succeed and achieve the treatment goals (19, 20).
Another explanation for the similar treatment effect obtained in both groups in this study is the supplementing of the weekly face-to-face sessions with a daily home-based exercise programme regardless of group assignment. Given the satisfactory compliance rate, it is likely that a great part of the gain in motor skills was due to the home exercise programme itself, which was similar in both groups, and may thus account for the similarities in outcomes.
It is interesting that almost all of the children in the individual-based therapy group improved in motor proficiency, whereas in the group-based therapy group children with a higher initial total impairment score (i.e. more severe impairment) tended to show greater improvement. The reason for this result is unknown. It is possible that children who have poorer motor performance may have more room for improvement or a lower training threshold, and would respond well to any motor training regardless of whether it is delivered in an individual-based or a group-based format. However, group-based training may not be ideal if the children in the group have very different motor abilities. In the group setting, certain activities involve taking turns. Children with more severe impairment may take longer to complete the task. Thus, those with less severe impairment, who may need more intensive training before improvement can be achieved, may not have an adequate opportunity to practice the task. Future studies should consider the homogeneity of motor impairment level within groups when assigning the children to group-based therapy.
It is interesting that the children also improved in manual dexterity, despite the fact that the exercise protocol mainly involved gross motor skills. We cannot rule out that the improvement observed was due to changes related to normal development (e.g. a maturation effect), as a non-treatment control group was not employed. It is also possible that the improvement in motor performance was indirectly caused by the psychological benefits of training, such as increased perceived competence and motivation to perform better during the testing sessions. However, there may also be a relationship between proximal stability and fine motor skills (22). Improvement in postural control may have allowed the children to perform fine motor tasks more efficiently.
Comparison with previous studies
Few randomized controlled studies have examined the effect of group-based motor training in children with DCD. In a recent study, Peens et al. (9) found that children (aged 7–9 years) who had undergone a motor-based intervention programme (2 sessions per week for 8 weeks) that was a combination of task-specific and sensory integration treatment methods showed significantly greater gains in motor performance as measured by the MABC compared with children in the control or psychological intervention groups. In an intervention study on 5- to 6-year-old children with DCD, Pless et al. (8) showed that their group-based functional training programme (1 session per week for 10 weeks) was beneficial for those with mild motor deficits, but not for those with severe motor problems. This is in contrast to our finding that children with more severe motor impairments tended to benefit more from group therapy than those with milder motor problems. The discrepancy in the results is probably partly due to differences in the exercises used and the higher child to therapist ratio (6–10:1) in the study of Pless et al. (8) than in our study (4–6:1). Perhaps a lower child to therapist ratio is more desirable for those with more severe motor problems. A recent study by Green et al. (23) showed that children with more profound and complex sensorimotor problems benefit from motor skill training, although residual motor difficulties may persist after training. Taken together, these findings indicate that, despite the difference in training methods, group motor skill training seems to be a promising treatment option for many children with DCD.
It is difficult to compare the effectiveness of our training programme with the various treatment approaches used in other studies, such as sensory integration therapy, task-specific training, and the cognitive-motor approach (7–12). This is partly due to differences in treatment frequency and duration. Another reason is the different subject selection criteria. A major issue with the sample in previous studies, as pointed out by Missiuna et al. (24), is that children were often identified as meeting the criteria for DCD without undergoing a comprehensive diagnostic process. In their recent report, Missiuna et al. showed that only 77% of children diagnosed with DCD by their physicians were confirmed as having the disorder by an interdisciplinary team assessment (20). It is thus likely that a substantial proportion of included subjects may not, in fact, have had DCD if a comprehensive, interdisciplinary diagnostic procedure was in place for subject selection. This may account for the difference in treatment outcomes in different studies. In our study, all of the subjects underwent an interdisciplinary assessment at the Child Assessment Centre before a diagnosis of DCD was made.
Home exercise compliance
Our face-to-face training sessions were held only once a week for 8 weeks. We cannot rule out the possibility that better results might have been produced had we used a higher training frequency or duration. However, we believe that our protocol is more practical and feasible in clinical settings considering the busy schedule of children and parents and the many issues faced by physiotherapists today, such as a large number of clients, limited staffing, and budgetary cuts. The implementation of a home programme was a means of increasing the exercise frequency without cost to the healthcare system. Indeed, it has been shown that provided adequate guidelines are given, most parents are highly capable of providing effective intervention for children with DCD (25, 26). Using a home exercise programme may also help children to develop a sense of responsibility for their own physical well-being. The home exercise compliance rate was 50–60% in both groups, which was satisfactory given the demanding workload of the children in terms of school classes and homework. It is thus interesting that the home exercise compliance rate was not significantly correlated with the change in total impairment score. There is some evidence that the severity of emotional and behavioural characteristics may influence treatment success in children with DCD (7). Other factors, such as motivation and participation in physical activity, may also influence treatment outcomes. Future studies should monitor these factors more closely.
Parental satisfaction
According to the results of our parental satisfaction questionnaire, the parents perceived the training programmes to be beneficial, not only for the children but also for themselves. The parents felt that the programmes provided them with psychological support. They also felt more motivated to play an active role in the physiotherapy management of their children, which is a critical factor in the success of home exercise programmes. The high parental satisfaction level may also partly explain the perfect attendance rate in both groups (100%).
Limitations
The study has several limitations. First, the sample size was relatively small, as this was a pilot study. The results should thus be interpreted with caution, as the post-hoc power analysis showed that the study was underpowered to detect a significant difference between the 2 groups if a real difference existed. Secondly, we did not measure how the change in motor impairment affected activity and participation (according to the International Classification of Functioning, Disability and Health) (27). Thirdly, we did not include a non-treatment control group. Thus, although we are able to conclude that group-based intervention was as effective as individual-based intervention, whether the improved performance in both groups was a result of treatment or the consequence of normal development during the treatment period is uncertain. Finally, we did not assess the long-term effect of the training.
Future research directions
In light of the encouraging findings of this study, a multi-centred randomized controlled study is planned to further assess the effects of individual-based motor skills training and group-based motor skills training. Based on the experiences gained in this study, the future trial will incorporate measures of activity and participation, as it is common for children with DCD to experience limitations in these areas (3, 28, 29). A non-treatment control group will also be included to account for the effects of developmental change. A follow-up assessment will be conducted to explore whether the motor gain is retained after a period of non-intervention. Moreover, the children’s social and emotional behaviour will be recorded and monitored more closely, as there is evidence that these characteristics may affect the response to motor skill training (7).
In conclusion, this study demonstrated that group-based and individual-based motor skill training programmes are equally effective in improving the motor proficiency of children with DCD. Considering the increasing fiscal restraints faced by public healthcare systems and the problem of long waiting lists, group-based training may be a more economical and efficient option for delivering treatment to children with DCD.
ACKNOWLEDGEMENT
The funding for this study was provided by the Hong Kong Polytechnic University.
REFERENCES
