Ivan Bautmans, PhD1, 2, Judith Van Arken, MSc1, Mike Van Mackelenberg, MSc1 and Tony Mets, PhD1, 2
From the 1Frailty in Ageing (FRIA) Research Department, Vrije Universiteit Brussel and 2Geriatrics, Universitair Ziekenhuis Brussel, Brussels, Belgium
Ivan Bautmans, PhD1, 2, Judith Van Arken, MSc1, Mike Van Mackelenberg, MSc1 and Tony Mets, PhD1, 2
From the 1Frailty in Ageing (FRIA) Research Department, Vrije Universiteit Brussel and 2Geriatrics, Universitair Ziekenhuis Brussel, Brussels, Belgium
OBJECTIVE: To explore the feasibility and effects of rehabilitation using manual mobilization of the thoracic spine in elderly female patients with osteoporosis.
METHODS: Forty-eight postmenopausal patients with osteoporosis (age 76 ± 7 years) were randomly assigned to 3 months rehabilitation (18 sessions including manual mobilization, taping and exercises, n = 29) or control (wait-list, n = 19). The primary outcome was thoracic kyphosis degree (Spinal-Mouse). Secondary outcomes were back pain (visual analogue scale) and quality of life (Qualeffo-41). Explanatory outcomes were compliance with rehabilitation, complications, and patients’ and therapists’ perceptions regarding the rehabilitation programme.
RESULTS: Thoracic kyphosis improved significantly following rehabilitation compared with controls (intention-to-treat analysis, p = 0.017); and in patients who were compliant with rehabilitation (n = 15) compared with those who were non-compliant (p = 0.002) and controls (p = 0.001). Mental health worsened slightly in the rehabilitation group (p = 0.029), but not significantly compared with controls. Neither patients nor physical therapists reported serious adverse effects.
CONCLUSION: Three months of rehabilitation with manual mobilization can attenuate thoracic kyphosis in elderly patients with osteoporosis. Its impact on back pain and quality of life remains unclear and needs further investigation.
Key words: osteoporosis; frailty; thoracic kyphosis; musculoskeletal manipulations; rehabilitation; posture.
J Rehabil Med 2010; 42: 129–135
Correspondence address: Tony Mets, Gerontology & Geriatrics, Vrije Universiteit Brussel, Laarbeeklaan 103, BE-1090 Brussels, Belgium. E-mail: tony.mets@vub.ac.be
Submitted March 23, 2009, accepted October 8, 2009
INTRODUCTION
Postural changes are a well-known phenomenon of ageing. Most common is an increased thoracic kyphosis associated with a loss of lumbar lordosis, especially over the age of 60 years (1). The presence of a hyperkyphotic posture in older ages is related to a higher risk of occurrence of physical disability (2), falls (3, 4) and mortality (5). Hyperkyphosis can develop without the presence of vertebral fractures (6, 7) and is considered as one of the characteristics of senescence both in rodents and humans (2, 8, 9). However, the presence of anterior vertebral wedging is closely related to the degree of thoracic kyphosis (10), and elderly patients presenting hyperkyphosis show a significantly increased risk of future vertebral fractures (11). Therefore, given the burden of vertebral deformities in elderly patients with osteoporosis, the prevention and treatment of thoracic hyperkyphosis in these subjects is highly important (12, 13).
Recent reports have shown that back-extensor muscle strength is significantly related to spinal range of motion (14) and thoracic kyphosis in elderly women (15). Moreover, back-muscle strengthening exercises and proprioceptive training can reduce the extent of thoracic hyperkyphosis in elderly women (16, 17). As well as by exercise therapy, restrictions in spinal range of movement can be approached by manual mobilization performed by a physiotherapist. Sran & Khan (18) report positive effects of a rehabilitation programme including manual mobilization of the thoracic spine in a the case of a woman with severe osteoporosis. Although physical therapists report being concerned about complications (91% in a Canadian sample), approximately 50% apply manual therapy in patients with osteoporosis (19). Currently, evidence for the efficacy and safety of rehabilitation programmes comprising manual mobilization in the management of thoracic hyperkyphosis in elderly patients is lacking.
The aim of this randomized controlled trial was to investigate the effects of thoracic spine rehabilitation (manual mobilization, taping and exercises for postural correction) on the severity of thoracic kyphosis, back pain and quality of life in frail, elderly postmenopausal patients with osteoporosis, and to explore its feasibility in a clinical rehabilitation setting.
METHODS
Participants
Elderly female patients scheduled in the period January to February 2006 for a 3-monthly intravenous (IV) pamidronate treatment for postmenopausal osteoporosis at the geriatric day hospital of the Universitair Ziekenhuis Brussel, Belgium, were eligible to participate in the study. Exclusion criteria were: Paget’s disease, rheumatoid arthritis, ankylosing spondylitis, cancer, and cognitive or physical inability to understand and/or participate in the test procedures. For all eligible patients, recent (< 3 months) plain X-ray images of the thoracic and lumbar spine were available in the medical records. Given the burden of vertebral fractures in elderly postmenopausal patients with osteoporosis with hyperkyphosis, antecedents of low-impact vertebral fractures was not an exclusion criterion per se. However, recent (< 3 months) and/or symptomatic vertebral fractures were considered as a contra-indication for intervention and these patients were not eligible. A total of 77 patients matching the inclusion/exclusion criteria were invited to participate in the study, of whom 48 (mean age 76 ± 7 years) agreed to participate (Fig. 1). All subjects had a documented diagnosis of osteoporosis based on dual X-ray absorptiometry (DEXA) according to World Health Organization criteria (T-score < –2.5). The study protocol was approved by the local ethics committee and all volunteers provided written informed consent.
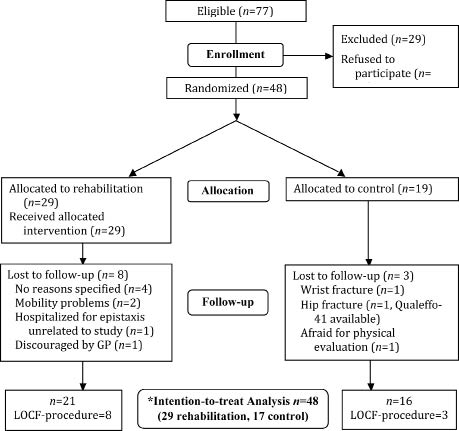
Fig. 1. Flow of participants. *Data were analysed following the intention-to-treat principle and missing data were managed using the last observation carried forward (LOCF) technique.
Randomization
Participants were sequentially included in the study and assigned randomly to an intervention or control group by an independent investigator. Stratification was applied according to age (< 80 or ≥ 80 years) and the antecedents of vertebral fractures because we considered these characteristics to be potential prognostic factors for outcome. Briefly, the randomization procedure was as follows: 4 envelopes were created based on the stratification criteria: (i) age < 80 years without antecedents of vertebral fractures; (ii) age < 80 years with antecedents of vertebral fractures; (iii) age > 80 years without antecedents of vertebral fractures; and (iv) age > 80 years with antecedents of vertebral fractures. Within each stratum, patients were randomized to rehabilitation or control. Since a higher drop-out rate was predicted in the intervention group, we aimed to obtain a larger number of participants in the intervention group by enclosing twice as many intervention as control assignment cards in the envelopes (6 cards for intervention and 3 for control). At the inclusion of each participant, an assignment card (intervention or control) was taken from the corresponding envelope (according to the stratum) by an independent investigator who was unaware of the proportion and the total number of assignment cards in the envelopes. When an envelope was empty, it was refilled with a new set of assignment cards. Finally, 29 subjects were assigned to intervention and 19 to control (not all assignment cards in the envelopes were used when the inclusion period was closed).
Intervention
Participants in the intervention group were prescribed 18 sessions (which is the usual number of sessions prescribed in Belgium) of spinal rehabilitation with a physical therapist of their choice. The rehabilitation protocol (Fig. 2) aimed to correct the posture of the thoracic spine and consisted of the procedures described below.
Fig. 2. The thoracic spine rehabilitation. (A, B) Manual mobilizations. (C, D) Taping. (E–H) Exercises for postural correction. (See methods section for detailed descriptions).
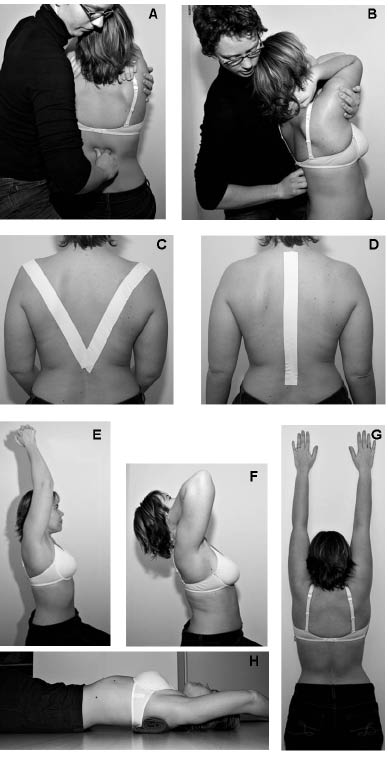
Gentle spinal mobilization of the thoracic spine using manual techniques. The patient was seated, with both hands on the neck or crossed on the shoulders. In this position, the patient’s upper arms were resting on the therapist’s arm, with which the therapist applied the mobilizing manoeuvre. The therapist’s other hand was applied on the lumbo-thoracic junction in order to provide gentle fixation. Gentle regional (whole thoracic spine), angular mobilizations were performed towards thoracic extension, and combined extension with lateral flexion and/or rotation. Each mobilization consisted of 10–15 free passive angular movements of the thoracic spine without active participation of the patients and without supplementary traction or other components. All mobilizations were performed within the available range of movement, without eliciting muscular defence or complaints from the patients. If possible, end-range positions were maintained for up to 5 sec without applying any supplementary force or thrust.
Taping. Free sets of elastic Cure-Tape® (FysioTape BV, Enschede, The Netherlands) were provided to the therapists. The tape was applied once per week and worn by the patient during 3 consecutive days. In order to avoid skin irritation, alternation of 2 methods of taping was used: V-shape taping (the patient is seated as straight as possible, and a strip of tape is applied bilaterally from the acromion to the spinal process of the twelfth thoracic vertebra) and longitudinal taping (the patient is seated as straight as possible, and a strip of tape is applied on the spinal processes from the first thoracic vertebra to the deepest point of the lumbar lordosis). The tape was highly extensible and caused gentle traction on the skin of the thoracic spine when the patient adopted a forward flexed posture.
Exercises for postural correction. The exercise programme comprised 5 basic exercises aimed at improving postural awareness, strengthening the back extensors and improving extension mobility of the thoracic spine. The exercises were performed under the supervision of the physical therapist, who provided guidelines (verbal and/or written) to the patients so that they could also perform the exercises alone (at home). The exercise programme comprised a daily session of 15–20 min (under the supervision of the therapist or alone at home). Briefly, the exercises comprised: (i) seated, lifting both hands together above the head (3 series of 10–15 movements, using a dumbbell if necessary); (ii) seated or standing with the back against a wall, straightening the back as far as possible (3 series of 10–15 repetitions, maintaining the upright position for 3–10 sec); (iii) seated on a chair with both hands on the neck or crossed over the thorax on the shoulders, lifting the arms and extending the upper back without compensation in the hips or lumbar spine (3 series of 10–15 repetitions, maintaining the upright position for 3–10 sec); (iv) standing in front of a wall, scrolling with both hands as high as possible over the wall (3 series of 10–15 repetitions, maintaining the upright position for 3–10 sec); (v) lying on the back, knees and hips flexed and feet resting on the ground, a small rolled-up towel under the 5th to 7th thoracic vertebrae (perpendicular to the spinal processes), stretching the thoracic spine for 30–180 sec (depending on the patient’s capacities, without compensation of the lumbar spine or eliciting back pain).
The physical therapists received a set of Cure-Tape® and written guidelines for the rehabilitation protocol, in which they were advised to spread the 18 rehabilitation sessions over a period of 12 weeks with decreasing frequency (first 2 weeks 3 sessions/week, second 2 weeks 2 sessions/week and remaining weeks 1 session/week). During the rehabilitation, therapists were contacted by telephone in order to control compliance with the guidelines and to provide supplementary specifications when needed.
Subjects in the control group were assigned to a waiting list for physical therapy. In fact, the physical therapy was delivered to these subjects at the end of the study (after 3 months).
Measurements
The primary outcome measure was change in thoracic kyphosis. Secondary outcomes were changes in back pain and quality of life. Explanatory outcomes were compliance with the prescribed therapy, complications due to the therapy, and patients’ and therapists’ perceptions regarding the rehabilitation programme.
Thoracic kyphosis, back pain and quality of life were assessed at baseline and after 3 months by 2 different researchers who were blinded for group assignment and baseline values. At baseline, height, weight, waist and hip circumferences, cognitive functioning (Mini Mental State Examination, MMSE (20)), and basic activities of daily living (bADL) (21) and instrumental ADL (iADL) (22) were measured in all participants. In addition, the presence of vertebral low-impact fractures and medication use was noted from the medical records of each participant.
Participants’ compliance with the prescribed physical therapy was assessed by 3-weekly telephone interviews, during which the subjects were asked whether they followed the prescribed physical therapy, how they perceived the rehabilitation and if there were any complications. After 3 months the physical therapists who treated the study patients were interviewed by telephone regarding their adherence to the rehabilitation protocol, how the rehabilitation programme was perceived, whether they were concerned about complications related to the spinal rehabilitation, and whether they observed any complications.
Thoracic kyphosis. The degree of thoracic kyphosis was assessed using a Spinal Mouse® device (Idiag, Fehraltorf, Switzerland), comprising a hand-held inclinometer connected wirelessly to a computer. Briefly, the spinal mouse was rolled paravertebrally along the spine from the 7th cervical to the third sacral vertebra while the patient was seated on an armless chair first in an upright position, then maximally flexed and, finally, maximally extended. The spinal mouse software provides a table with inclination angles at each vertebral segment. Each position was measured 3 times consecutively and the mean inclination at each vertebral segment was calculated. For this study, only the mean inclination of the thoracic spine in the upright position (sum of segments from cervical 7 to thoracic 12) was taken into account, which has been shown to be a reliable measure for thoracic kyphosis (interclass correlation coefficient (ICC) = 0.73–0.88 for intra-observer reliability and ICC = 0.83–0.87 for inter-observer reliability) (23).
Back pain and quality of life. Back pain perceived during the past week was scored by the participants on a visual analogue scale (VAS) ranging from 0 to 100 mm.
Quality of life was evaluated using the Qualeffo-41, a questionnaire specifically developed for patients with osteoporosis (24, 25). The Qualeffo-41 provides scores on 5 domains: Pain, Physical Function (further subdivided into Activities of daily living, Jobs around the house and Mobility), Social Function and General Health Perception, Mental Function, and a total score (all scores converted to a 0–100 scale, with higher scores indicating worse quality of life).
Statistical analysis
Statistical analysis was performed using SPSS for Windows (release 15.0.1). Average values are given ± their standard error (SEM). Data were analysed following the intention-to-treat principle and missing data were managed using the last observation carried forward (LOCF) technique. Unpaired t-tests (Mann-Whitney U test for the ordinal distributed scales bADL and iADL) were performed to assess differences between groups. Differences between groups in changes over time were computed with repeated measures analysis of variance (ANOVA), and paired t-tests were used to assess within-group changes over time. Significance level was set at two-sided p < 0.05. Data collected during interviews with participating patients and therapists were managed using a qualitative approach.
RESULTS
At baseline, the rehabilitation and control groups were similar for all outcome measures (Table I). A total of 38 participants completed the study, of whom 21 were in the rehabilitation group and 16 were in the control group (Fig. 1). Eight participants from the rehabilitation group could not be re-assessed: 4 participants withdrew from the study without specifying the reason; 2 reported inability to attend the hospital for re-evaluation due to mobility problems (of whom one completed the Qualeffo-questionnaire by post); one anxious subject reported having been discouraged by her general practitioner from participating further; one participant was hospitalized following epistaxis (due to known hypertension). Three participants from the control group were unavailable for follow-up: 2 declined further participation: one broke her wrist due to an unrelated fall and another became afraid of the physical evaluation; a third participant had an unrelated hip fracture (she completed the Qualeffo-questionnaire). Compared with those who completed the study, patients unavailable for follow-up were significantly slimmer (weight 55.7 ± 2.2 vs 66.4 ± 2.3 kg, p = 0.002 and body mass index (BMI) 23.1 ± 2.7 vs 27.0 ± 5.8 kg/m2, p = 0.005) and showed significantly better scores on the domains Pain (20.0 ± 4.9 vs 38.3 ± 5.1, p = 0.014), ADL (11.1 ± 2.8 vs 21.9 ± 3.2, p = 0.016) and General health perception (30.0 ± 3.8 vs 58.3 ± 2.9, p < 0.001) of the Qualeffo-41. No significant differences were found for the thoracic kyphosis or other remaining outcome measures.
| Table I. Participants’ characteristics at baseline, given as mean values ± standard error, unless otherwise stated | ||
| Parameter | Rehabilitation n = 29 | Control n = 19 |
| Age, years | 75.2 ± 1.3 | 77.6 ± 1.6 |
| Weight, kg | 63.6 ± 2.4 | 65.1 ± 3.4 |
| Height, m | 1.58 ± 1.0 | 1.55 ± 1.4 |
| BMI, kg/m2 | 25.5 ± 0.9 | 27.2 ± 1.5 |
| Hip-waist ratio, index | 0.84 ± 0.02 | 0.90 ± 0.03 |
| MMSE, score/30 | 27.4 ± 0.9 | 25.9 ± 1.1 |
| Antecedents of vertebral fractures, n (%) | 16 (52) | 8 (42) |
| bADL, score/24 | 8.6 ± 0.2 | 8.8 ± 0.5 |
| iADL, score/27 | 24.1 ± 0.5 | 22.4 ± 1.0 |
| Medication use, n | 5.7 ± 0.5 | 5.7 ± 0.6 |
| BMI: body mass index; bADL: basic activities of daily living; iADL: instrumental activities of daily living; MMSE: Mini Mental State Examination. | ||
Compliance
Participants were considered as compliant when they received at least 9 of the 18 prescribed physical therapy sessions (50%) and/or if they exercised independently at home at least once a week. Fifteen participants from those allocated to rehabilitation were compliant with the prescribed therapy (14 from those available for follow-up). Reasons for non-compliance with rehabilitation were different among individuals, and illustrate the beliefs and motivations of elderly patients with osteoporosis and their caregivers regarding physical therapy. One subject reported that she did not like physical therapy and found rehabilitation to be unnecessary; one had not enough time; 3 reported problems with mobility and/or financial reasons; another considered herself too old for rehabilitation at 78 years of age; one did not consider the rehabilitation useful since she suffered from back pain, considered herself not sporty enough for physical therapy and, moreover, reported being discouraged by her general practitioner from starting rehabilitation. Participants who were compliant with rehabilitation presented significantly higher BMI (27.5 ± 1.1 vs 23.5 ± 1.2 kg/m2, p = 0.022) and a worse general health perception, as measured by the Qualeffo-41 at the limit of statistical significance (61.1 ± 5.1 vs 44.0 ± 6.7, p = 0.052) compared with those who were non-compliant. No significant differences were found regarding thoracic kyphosis or other remaining outcome measures.
Thoracic kyphosis
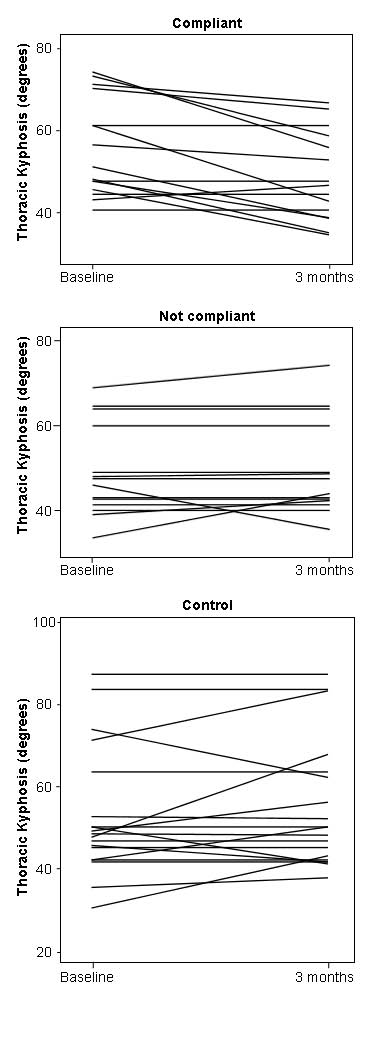
As can be seen in Table II, 3 months rehabilitation significantly reduced the degree of thoracic kyphosis (p = 0.017) compared with controls (no change, difference in evolution between both groups, p = 0.017). The per-protocol analysis plotted in Fig. 3, shows that subjects assigned to rehabilitation who were compliant with treatment improved significantly compared with those who were non-compliant (repeated measures ANOVA p = 0.002) and controls (repeated measures ANOVA p = 0.001). In fact, thoracic kyphosis improved by 7.1 ± 1.9 degrees (p = 0.002), whereas kyphosis in non-compliant and control subjects did not change significantly (–0.7 ± 1.2 and –1.9 ± 1.7 degrees, respectively).
| Table II. Change in spine-related dysfunction and complaints given as mean values ± standard error | |||||||
| Parameter | Rehabilitation | Control | p* | ||||
| Baseline | 3 months | p† | Baseline | 3 months | p† | ||
| Thoracic kyphosis (degrees) | 52.5 ± 2.2 | 49.1 ± 2.0 | 0.017 | 52.8 ± 3.6 | 54.8 ± 3.6 | 0.272 | 0.017 |
| VAS-pain (score/100) | 33.6 ± 5.2 | 33.9 ± 5.2 | 0.947 | 29.5 ± 6.4 | 31.3 ± 6.8 | 0.871 | 0.920 |
| Quality of life (Qualeffo-41) | |||||||
| Pain (score/100) | 37.4 ± 5.7 | 38.1 ± 4.9 | 0.836 | 30.0 ± 6.4 | 29.7 ± 5.7 | 0.936 | 0.891 |
| Activities of daily living (score/100) | 22.2 ± 3.2 | 21.5 ± 3.9 | 0.751 | 15.8 ± 4.5 | 18.1 ± 4.0 | 0.407 | 0.606 |
| Jobs around the house (score/100) | 35.1 ± 5.0 | 33.7 ± 5.4 | 0.612 | 41.3 ± 6.7 | 37.2 ± 6.2 | 0.300 | 0.364 |
| Mobility (score/100) | 31.1 ± 4.8 | 29.6 ± 4.4 | 0.500 | 30.1 ± 5.0 | 32.2 ± 5.5 | 0.479 | 0.679 |
| Physical function (score/100) | 30.3 ± 4.3 | 28.9 ± 4.3 | 0.417 | 30.0 ± 5.0 | 30.5 ± 5.1 | 0.859 | 0.976 |
| Social function (score/100) | 51.0 ± 3.5 | 49.7 ± 5.0 | 0.686 | 53.7 ± 4.0 | 55.7 ± 4.7 | 0.511 | 0.520 |
| General health perception (score/100) | 52.9 ± 4.4 | 52.3 ± 4.4 | 0.841 | 51.8 ± 3.3 | 50.0 ± 3.1 | 0.649 | 0.982 |
| Mental function (score/100) | 37.9 ± 3.7 | 40.8 ± 3.8 | 0.029 | 36.6 ± 2.9 | 35.2 ± 3.8 | 0.725 | 0.345 |
| Total score (score/100) | 37.8 ± 3.6 | 38.0 ± 3.7 | 0.860 | 34.4 ± 3.8 | 36.6 ± 3.5 | 0.473 | 0.560 |
| Intention-to-treat analysis: n = 48 (rehabilitation n = 29 and control n = 19). *p-value of the difference in evolution between rehabilitation and control groups assessed with repeated measures ANOVA. †p-value of the changes over time within rehabilitation and control groups assessed by paired t-tests. VAS: visual analogue scale. | |||||||
Fig. 3. Per-protocol analysis of the effects of rehabilitation on the degree of thoracic kyphosis. Subjects assigned to rehabilitation and who were compliant with treatment (n = 15) improved significantly compared with those who were non-compliant (n = 14, repeated measures analysis of variance (ANOVA) p = 0.002) and controls (n = 19, repeated measures ANOVA p = 0.001).
Back pain and quality of life
Mental health perception worsened slightly but significantly (p = 0.029) in the rehabilitation group (Table II). No significant difference in evolution between groups was observed for any of the other outcome measures, either in the intention-to-treat or in the per-protocol analysis.
Patients’ and therapists’ perceptions
Overall, patients reported consistently positive experiences regarding the rehabilitation programme. Some patients reported that after rehabilitation they experienced less pain, less fatigue in the back, being able to walk longer or being more flexible. Also, positive remarks regarding the relationship with the therapist were reported. Despite a positive overall experience, some patients indicated that certain exercises were sometimes difficult to perform, especially when lifting the arms above shoulder level. When questioned about perceived adverse effects during the rehabilitation, some patients reported none, while others experienced a mild skin irritation due to the tape, pain during the mobilizations, difficulties in lifting the arms above the head during the exercises, or shoulder pain during exercises with the arms. All therapists mentioned a positive experience regarding the rehabilitation programme. When questioned about fear of complications while treating elderly patients with osteoporosis with spinal mobilization and exercises, therapists responded either as having no particular fear of adverse effects, or else as being concerned about the occurrence of vertebral fractures, fractures during the exercises or increased pain. Other items reported by the therapists during the interviews included: not being used to mobilizing the spine; having started exercises for other elderly patients with osteoporosis since their participation in the study; sometimes finding spinal mobilizations heavy or difficult to perform; a proposition to extend the programme to the lumbar spine; observing that patients needed a lot of guidance during the exercises or were difficult to motivate to exercise at home.
DISCUSSION
This is one of the first studies exploring the feasibility and effects of a spinal rehabilitation programme using manual mobilization of the thoracic spine in elderly postmenopausal patients with osteoporosis. The results demonstrate that 3 months spinal rehabilitation reduces modestly, but significantly, the degree of thoracic kyphosis compared with controls (intention-to-treat analysis p = 0.017). In a per-protocol analysis, we found that those patients who were compliant with therapy had a clearly better improvement (mean improvement 7.1 ± 1.9 degrees, p = 0.002) compared with non-compliant patients (p = 0.002) and controls (p = 0.001) whose kyphosis did not change significantly. These results support the assumption that postural changes, i.e. thoracic kyphosis, are at least partly reversible in elderly patients with osteoporosis by means of conservative treatment. The amount of improvement in thoracic kyphosis in our study is comparable with the 6 ± 3 degrees reduction in kyphosis after 3 months exercise therapy found by Katzman et al. (16) in a single-group study involving 21 community-dwelling elderly women. It is unclear whether a longer period of rehabilitation can further improve posture in elderly patients, but it can be assumed that continuation of the rehabilitation might be necessary in order to maintain the obtained improvements. From the results of our study it remains unclear by which mechanisms the improvement in thoracic kyphosis occurred following rehabilitation. Greig et al. (26) demonstrated a significant decrease (from 58 ± 3 to 55 ± 13 degrees) in thoracic kyphosis immediately following the application of postural taping on the thoracic spine, which was not obtained using “sham” taping (without postural correction). However, in contrast to the results of the study of Greig et al., the participants in our study were assessed without wearing the postural tape, and it can be assumed that the attenuation of the severity of kyphosis was the result of the combination of both passive (manual mobilization and postural tape) and active (exercises) components of the rehabilitation programme.
Since hyperkyphosis is related to lower lung volume (27) and worse quality of life (28) in osteoporotic women, we hypothesized that the attenuation of the severity of kyphosis would improve the quality of life in our participants. Contrary to our expectations, the patients allocated to rehabilitation did not improve with respect to quality of life or back pain, as measured with the Qualeffo-41 questionnaire and the VAS. Instead, a slight worsening on the domain of mental function (from 37.9 ± 3.7 to 40.8 ± 3.8, p = 0.029) was found within the rehabilitation group. It cannot be excluded that the rehabilitation programme increased their awareness regarding their posture, explaining higher reported disability in mental function. However, this worsening was not significantly different from the changes in the control group, thus challenging its clinical relevance. Our findings are in contrast with those of Chien et al. (17) and Hongo et al. (29), who found a significant improvement in quality of life in elderly postmenopausal women following, respectively, 12 weeks and 4 months back-strengthening exercises. However, Chien et al. (17) did not perform an intention-to-treat analysis, and in the study of Hongo et al. (29) the assessors were not blinded for allocation and outcome testing. Also, their participants were in better health and much younger (mean age 61 ± 9 and 67 ± 5 years for intervention and 58 ± 9 and 67 ± 7 years for controls, respectively, in the study of Chien et al. (17) and Hongo et al. (29)) compared with the participants in our study. Although the Qualeffo-41 was specifically developed to measure quality of life in patients with osteoporosis who have spinal complaints (24), its responsiveness might be too low to demonstrate early changes after rehabilitation (18). On the other hand, the primary goal of the rehabilitation programme was to reduce the severity of kyphosis. The addition of supplementary modalities for pain reduction might have led to larger improvements in quality of life and back pain.
In accordance with recently published guidelines for designing randomized controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons (30), we limited as much as possible the exclusion criteria for participation in our study. Given the frail profile of our participants, illustrated by high age, prevalence of vertebral fracture antecedents and polypharmacy, we anticipated a higher drop-out-rate in the rehabilitation group by doubling the chance for allocation to rehabilitation compared with control in our randomization system. Finally, 11 patients were unavailable for follow-up (8 in the rehabilitation and 3 in the control group). This drop-out rate is similar to that reported in other studies involving elderly patients with osteoporosis (16, 17). Analysis of the characteristics of the patients who dropped out revealed that they were significantly slimmer, less obese (lower BMI) and presented better scores on the domains pain, ADL and general health perception of the Qualeffo-41 compared with those who completed the study. Also, several reasons for drop-out suggest a lack of motivation of the participant and her peers to be reassessed. Therefore, we can accept that the most vulnerable group of patients remained in our study and that our results are representative for frail elderly patients with osteoporosis.
In this study, we aimed to optimize compliance with the prescribed rehabilitation programme by referring the patients to a physical therapist of their choice, who could provide rehabilitation at the patient’s home if necessary. Also, patients allocated to rehabilitation were contacted by telephone every 3 weeks regarding their compliance. Despite these incentives, only 52% of all patients allocated to rehabilitation were compliant with therapy (67% of those available for follow-up). A relatively low compliance rate is a well-known issue in studies targeting frail elderly patients. Compliance with rehabilitation in our study is similar to that reported by van Heuvelen et al. (31), who studied determinants for attendance of elderly persons at psychological and physical training sessions. In our study, non-compliant patients showed significantly lower BMI and tended to present a better general health perception, similar to those who dropped out. It cannot be excluded that those patients who perceived being in better general health were less motivated to continue rehabilitation. On the other hand, patients who were less obese might have been more likely to fear manual mobilization of the thoracic spine. These assumptions are partly supported by the reasons for non-compliance with rehabilitation that were collected in our study.
Overall, consistently positive experiences were reported by our participants regarding the rehabilitation programme. Also, the reported subjective improvements in somatic symptoms and well-being are to be considered as important results in studies with frail elderly patients (30). However, we did not collect these data in a quantitative way (e.g. by using Likert scales of perceived improvement) and therefore we managed the information in a qualitative analysis strategy. The interviews also revealed that exercise during which the arms must be lifted above shoulder level in frail elderly patients with osteoporosis can be experienced as difficult. Except for incidental skin irritation due to the taping, no major adverse effects of the rehabilitation programme have been reported. From these results it is justified to assume that the manual mobilizations in our rehabilitation programme were safe and did not produce any adverse effects. However, some of the therapists who provided the rehabilitation reported being concerned about complications during the rehabilitation of elderly patients with osteoporosis. In our opinion, special attention should be paid to rehabilitation strategies in frail elderly patients with osteoporosis, and specific skills-training should be included in the education of physical therapists.
Remarkably, 2 patients (one drop-out and one non-compliant) reported being discouraged by their general practitioner from continuing with rehabilitation. Therefore, physicians must be aware of the important role they can play in the social support of elderly patients with osteoporosis to adhere to rehabilitation.
The strengths of this study are its randomized controlled trial design, the rehabilitation programme aimed at improving thoracic kyphosis, the setting reflecting the real clinical rehabilitation environment, and the included population representing frail geriatric elderly patients with postmenopausal osteoporosis. The weakness of this trial is the relatively poor compliance in the intervention group, which reduces the feasibility of the studied rehabilitation programme in this frail and vulnerable geriatric population. On the other hand, the qualitative data concerning the therapists’ and patients’ perceptions provide insights into the potential underlying causes of resistance to therapy, which may assist researchers and clinicians to improve the compliance of frail osteoporotic patients with rehabilitation interventions.
In conclusion, a 3-month rehabilitation programme including manual mobilization of the thoracic spine can significantly reduce thoracic kyphosis in elderly female patients with osteoporosis. The impact of this rehabilitation on quality of life and back pain requires further investigation. Elderly patients with osteoporosis should be given particular support in order to optimize their adherence to the prescribed rehabilitation.
ACKNOWLEDGEMENT
The authors thank FysioTape B.V. (Enschede, The Netherlands) for providing the free samples of Cure-tape for this study.
REFERENCES
