The aim of this review is to describe aspects of vocational rehabilitation relevant for a physician aiming to become a specialist in physical and rehabilitation medicine (PRM). The review discusses the epidemiology of incapacity for work, the major patient groups in vocational rehabilitation (musculoskeletal and psychiatric diagnoses comprise approximately 50–70% of the patients), the influence of different kinds of environmental and individual risk factors on work resumption (such as the legal framework, application of the law, resources for rehabilitation and its effectiveness, the degree of co-operation between vocational rehabilitation agencies, economic factors/labour market situation, medical and personal factors). The review describes different models of vocational rehabilitation, the effectiveness of various vocational rehabilitation programmes on work resumption or sick leave (where strong evidence is reported for multimodal rehabilitation programmes for patients with long-lasting musculoskeletal pain). Finally, there are sections about the PRM physician’s history-taking in vocational rehabilitation (using the International Classification of Functioning, Disability and Health (ICF)), and report writing with a structure where ICF body functions and activity limitations are reported separately.
Key words: vocational rehabilitation, educational review, return-to-work, sick leave, working capacity, risk factors, effectiveness, functional assessment, ICF.
J Rehabil Med 2009; 41: 856–869
Correspondence address: Jan Ekholm, Section of Rehabilitation Medicine, Karolinska Institutet Department of Clinical Sciences, Building 39, 3rd Floor, Danderyd Hospital, SE-182 88 Stockholm, Sweden. E-mail: Jan.Ekholm@ki.se
Submitted June 3, 2009; accepted August 25, 2009
INTRODUCTION
A person’s ability to work can be profoundly affected by their disease, disability and a range of contextual factors. Rehabilitation medicine is integral to the process leading back to working life after illness or injury, but other rehabilitation disciplines are also essential. It is important to be clear about what rehabilitation physicians, or trainees in rehabilitation medicine, need to know about vocational rehabilitation (VR). The aim of the present review is to describe those aspects of VR that the authors believe are relevant for a physician aiming at becoming a specialist in physical and rehabilitation medicine (PRM). This review discusses the background to the problem, the evidence for the effectiveness of VR, general factors involved in the VR process, and the roles of the rehabilitation physician and others.
DEFINITIONS IN VOCATIONAL REHABILITATION
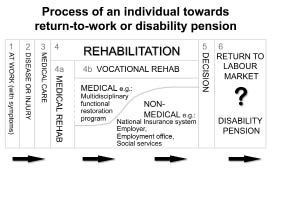
VR is a process whereby those disadvantaged by illness or disability can be enabled to access, maintain or return to employment, or other useful occupation (1). This applies to those with temporary and permanent impairments (for alternative definitions see (2, 3)). The journey towards return-to-work or a disability pension is illustrated in Fig. 1. Rehabilitation clinicians are involved in parallel during the process. A decision is taken, usually in the context of an insurance settlement, as to whether the individual will return to the labour force or be granted a disability pension or long-term incapacity benefit. VR deals mainly with rehabilitation at the International Classification of Functioning, Disability and Health (ICF)-level of “participation” (3, 4).
Fig. 1. The rehabilitation process towards a return to the labour market or to a disability pension (Source: modified after Ekholm J, et al., Report to Ministry of Social Welfare, Mid Sweden University, Östersund, CSF Reports No 2003:1).
Work instability
Work instability is a state in which the consequences of a mismatch between an individual’s functional activities and the demands of the work can threaten employment if not resolved (5, 6). Measures for work instability exist for rheumatoid arthritis (RA) (available in 13 languages), ankylosing spondylitis, traumatic brain injury, epilepsy and multiple sclerosis. A work instability screen also exists for nursing staff (7).
Work disability
Work disability has been defined by Allaire et al. (8) in relation to RA as work cessation irrespective of its cause, e.g. being granted a sickness pension or early retirement, whether attributed to RA or not. This allows comparison with other studies (9, 10). Using this definition includes those who ceased working for reasons that superficially may not be related to their RA, but on further inspection, have a complex relationship with the condition. In RA, approximately 30% of people have ceased work at 10 years. This is in agreement with findings from studies in other conditions, including multiple sclerosis (11).
MAJOR COMPONENTS
VR comprises assessment and interventions, as follows.
Assessment
Assessment begins with evaluating the person’s impairments, functional abilities (physical, psychological and cognitive) including fitness for work, followed by an assessment of their work and workplace. One must also examine the interface between the person and their work and the potential for the person to return to this work. Assessment maps onto the ICF (4), which is the model that will be used in this review.
There is a hierarchy of outcomes: the most desirable is when the person returns to their own work, which may need to be modified (some of the tasks may be delegated or the hours may be reduced). If this is not possible, they may be able to return to the same workplace in a different capacity. Finally, they may need to apply for different work when their current skills and abilities do not match the requirements of their previous role.
Assessment culminates in an individualized goal-directed rehabilitation plan, which is agreed with the worker. This will probably lead to several coordinated interventions.
Interventions
Interventions focus on diminishing the limitations and restrictions identified during the assessment, e.g. increasing fitness, work conditioning, ameliorating anxiety or depression, building confidence and training in the management of stress. The workplace may require modification, including the acquisition of specific equipment.
Case management and networking across many agencies will be necessary when the worker’s needs are particularly complex. The role of the case manager is: “to coordinate and oversee the early stages of recovery from illness or injury the overall programmes of rehabilitation and return-to-work activities planned for each client” (1). Counselling, job coaching, workplace supervision or support in the workplace should also be available.
HOW, WHEN AND WHERE IS VOCATIONAL REHABILITATION PRACTISED?
VR is frequently practised as a bolt-on to medical rehabilitation: the physician or surgeon conducting a clinic or advising an operation forgets that the person in front of them is a worker, and that a much greater part of that person’s life is lived at work rather than as a patient (12).
The use of a standard history that includes details of the person’s work and education will focus the clinician’s mind on these roles. Even at this early point some people will be at risk of losing their work, and in these cases quantification of the risk by a work instability measure will be helpful (5). This is good preventive medicine.
The status of the person as a worker and their work situation needs to be noted in the acute phase of a medical condition and this knowledge should be used in planning return-to-work by the specialist and the general practitioner.
Where rehabilitation is part of this pathway, medical and vocational rehabilitation need to overlap. For many people with musculoskeletal conditions, the pathway consists of pain relief, management of mood, maintenance and return of fitness and function, and a staged return-to-work. For more complex situations and diagnoses the pathway will be more complicated and has to be rapidly accessible and properly structured (2).
VR may take place in the community, in the specialist hospital department, including the therapy departments, at the workplace and in other locations, either owned by insurers or the Department of Social Insurance (in the UK, the Department of Work and Pensions). Good results are often achieved when VR is performed in close proximity to the workplace (13, 14), but in many countries most small and medium sized employers have little access to these facilities.
In straightforward conditions, interventions may be simple and take place in any of these departments, but where the person has a complex or long-term condition, or has been out of work for a long time, a multidisciplinary approach will be necessary. Any type of rehabilitation may have an effect at an early stage of decreased work ability, but may be ineffective later on if applied as the only mode of rehabilitation (13). Where chronic disability is already present, multimodal medical rehabilitation needs to be combined with VR in order to reduce sick leave and progression towards disability pension.
Where there are numerous risk factors for unemployment a multiprofessional, multi-agency approach with shared responsibility (15, 16) will be necessary.
EPIDEMIOLOGY OF INCAPACITY FOR WORK/LONG-TERM DISABILITY
There are 44.6 million disabled people of working age in the European Union (EU): 7% are aged 16–25 years. Currently, 42.2% of disabled people are in employment, compared with 64.5% of non-disabled people (2); 44% of unemployed disabled people feel that they would be able to work if given the appropriate assistance.
In the UK, the economic cost of incapacity is estimated to be in excess of €115 billion (17). This is greater than the annual budget for the UK National Health Service (NHS) and is equivalent to the Gross Domestic Product (GDP) of Portugal. Self-reported disability increases with age: from 10% at 16–24 years to 34% of those aged from 50 years to state pension age (18).
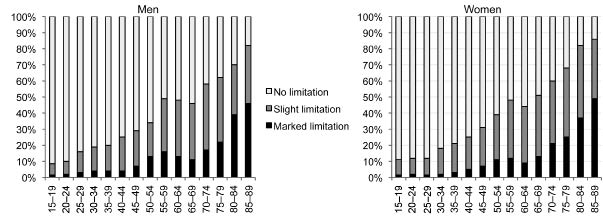
Fig. 2 shows the proportion of people in Austria with self-reported limitations in activities of daily living (ADL) across age groups (19). Between the ages of 55 and 59 years, 15% of men and 10% of women perceived their ADL to be limited.
Table I shows the percentage of population outside the labour market in the Nordic countries granted disability pension and unemployment benefit. Benefits from different branches of social security can sometimes have unintended consequences. For example, if disability pensions are restricted, individuals who are not granted a pension may continue to be job seekers, thus contributing to unemployment. The figures for Finland, with a relatively low percentage of disability pensions (8%) and relatively high unemployment (7%), may be explained in that way.
Fig. 2. Proportion of persons in Austria with self-reported limitations in activities of daily living (ADL) as a percentage of age classes. Source: (19).
| Table I. Percentage of population outside labour market in the Nordic countries due to granted disability pension (dp%) and unemployment (unemp%), respectively. Age group 20–64 years (2006) |
| Country | dp% | unemp% | Total % |
| Denmark | 7 | 3.5 | 10.5 |
| Finland | 8 | 7 | 15 |
| Iceland | 7 | 2.1 | 9.1 |
| Norway | 11.5 | 3 | 14.5 |
| Sweden | 10.5 | 6.1 | 16.5 |
WHO NEEDS VOCATIONAL REHABILITATION?
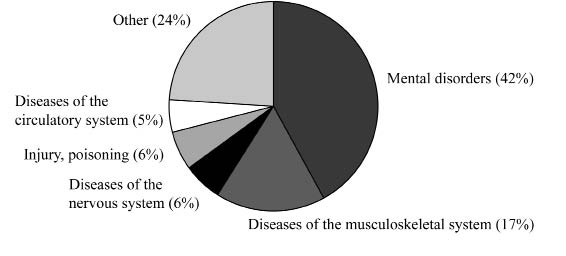
Fig. 3 shows the diagnoses of those on long-term incapacity benefit in the UK. Mental health conditions are rarely major diagnoses such as psychoses, but include anxiety, depression, and stress-related medical conditions, sometimes without a formal diagnosis. A few years ago the majority of benefit recipients had musculoskeletal problems, again not of a very severe nature.
Fig. 3. Diagnoses of those on long-term incapacity benefit in the UK (2008). The largest group of people have mental health problems (42%) and the second largest have (specified) diseases of the musculoskeletal system (17%).
General practitioners need to be aware that the person’s best chance to return to work is by early intervention through prompt rehabilitation, whether in primary care or obtained through rehabilitation services.
A significant number of people have respiratory diagnoses where early rehabilitation has proven effective. A small, but important, group have complex disabilities such as traumatic brain injury which require co-ordinated, specialist and multidisciplinary management. SUVA, the Swiss insurance company, recognizes that these constitute 5% of the claims but consume approximately 80% of the resources and require a sophisticated response to enable clients to return to work (20).
To plan VR effectively it is necessary to discriminate between static disabilities (in which the individual may be healthy and have predictable difficulties in the workplace) and progressive, fluctuant, long-term conditions where the response may have to be more flexible and allow for variation from day-to-day.
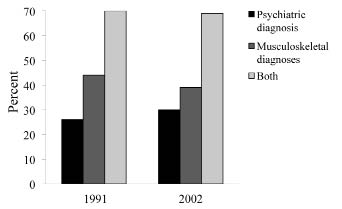
Seventy percent of those granted disability pension in Sweden had either musculoskeletal (39–44%) or psychiatric conditions (26–30%) (Fig. 4). Very little change occurred between 1991 and 2002 (21).
Fig. 4. Proportion of psychiatric and musculoskeletal diagnoses of those who have been granted disablement/disability pension by the Swedish National Insurance Agency and the sum of the 2 proportions. The small difference between 1991 and 2002 is illustrated. Source: (21).
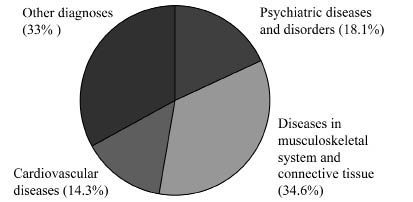
Fig. 5 shows the diagnostic groups of recipients of invalidity pensions in Austria.
Fig. 5. Diagnoses of those granted disablement/disability pension in Austria. The largest group of people had diseases of the musculoskeletal system (34.6%) and the second largest had psychiatric diseases and disorders (18.1%). 14.3% had cardiovascular diseases.
INDIVIDUAL AND ENVIRONMENTAL RISK FACTORS FOR BEING OFF WORK
Hindrances or facilitators to work resumption
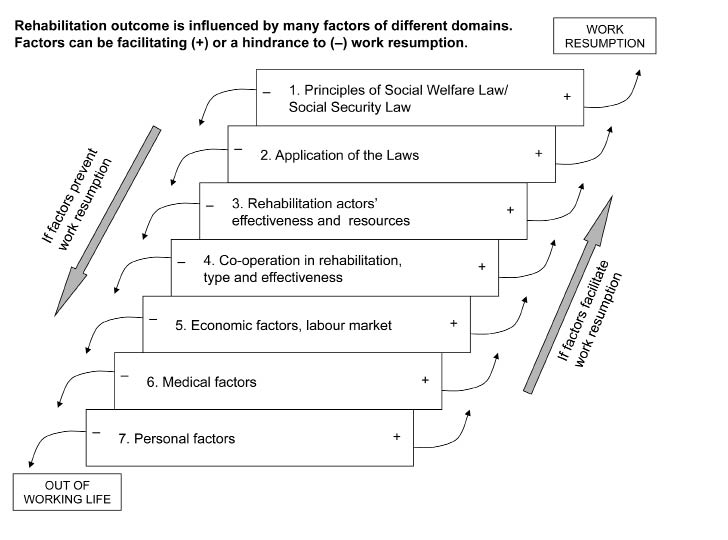
There are various factors influencing return-to-work. If an individual is exposed to many negative influences the chance of work resumption is lower than if there are many positive factors. Some factors are personal and medical and some are external influences, which are categorized in the ICF Environmental factors (4). There are differences between these factors’ relative importance across countries. Fig. 6 emphasizes that an individual’s chance of returning to work is influenced by many factors, in addition to medical ones.
Fig. 6. The rehabilitation outcome – either work resumption or removal from working life by means of sickness pension – is influenced by several different domains of factors, both environmental and individual. The factors can be facilitating (+) or a hindrance (–) to work resumption. If an individual is exposed to many negative influences the chance of work resumption is lower than if he/she is exposed to many positive factors. Adapted from Vahlne Westerhäll L, et al. Lärobok i Rehabiliteringsvetenskap. [Textbook of rehabilitation science]. Studentlitteratur: Lund; 2006.
Relevant legislation
VR operates within the United Nations (UN) Convention on the Rights of Persons with Disabilities, which came into force on 3 May 2008. The Convention has 8 guiding principles including non-discrimination, full and effective participation and inclusion in society, and equality of opportunity. These encompass the right to work and to full access to employment (22).
The EU supports social inclusion, with a non-discrimination directive (23), which includes key challenges: (i) to make labour markets truly inclusive; (ii) to overcome discrimination and increase the integration of disabled people, ethnic minorities and immigrants.
Individual countries have anti-discrimination legislation of varying effectiveness. The Disability Discrimination Act in the UK is strong and is regularly tested in the courts, so that an increasing body of case law exists. Governmental policy supports VR, e.g. in the Netherlands, Denmark, UK, Sweden, Austria and Germany. Policy is often linked to benefit payments, and in the last few years several countries have greatly changed the field of benefits and VR.
There are important differences between countries in relation to legislation relevant to VR, e.g. Social Welfare Law / Social Security Law, General Insurance Act, Occupational Safety Act and Employment Law. Legislation is recognized under the domain of the ICF Contextual Factor “external influences on functioning and disability” (see Legal services, systems and policies: e550 (4)).
In Scandinavian countries the principles that underpin VR include early action and priority for work resumption with a comprehensive view of the client’s problem. Legislation emphasizes the importance of co-operation between organizations.
Priority for work resumption implies that the first priority of the State is to assist a person in improving functioning and finding work. It is not good practice to merely grant allowances before assisting the person to find work, and before being assessed as incapable of work. Long-term benefits should only be awarded after this point.
Application of legislation
Rehabilitation services have to interpret and apply the relevant legislation within each jurisdiction in the EU. Great variations occur within this domain. Rehabilitation services need to be aware of how the laws are interpreted by the health and social insurance systems (ICF domain e570 Social, services, systems and policies). They also need to bear in mind the employers’ responsibilities and the patients’ rights to access rehabilitation services (see Table II), where these exist, subject to the Convention.
| Table II. Roles and responsibilities of each of the main actors that will ensure the success of vocational rehabilitation programmes |
| Employee’s role Keep in contact with employer Openness with occupational health Discuss which parts of job can be done | Employer’s role Keep in contact with employee Ensure understanding of sickness absence policy ergonomics Check line managers’ understanding Facilitate phased return-to-work (RTW) Accommodate rehabilitation process |
| Responsibilities of social insurance system Advise on eligibility benefits Assessment to work Work experience Job introductions Provide retraining Support employers Support employees | Responsibilities of health system Adjust environment/provide equipment Advise on RTW Encourage liaison with employers Teach coping strategies Provide rehabilitation Support after RTW |
Health and social insurance systems are often managed by government authorities, so these systems will be subject to political aims, targets and national agendas. They are also subject to fluctuations in the general economic situation in a country. When the costs for public insurance are considered to be too high, restrictions are placed on social insurance systems, in general, and benefits in particular.
Examples of failures of the system to respond adequately to peoples’ needs: (i) too few participate in rehabilitation: in Sweden only approximately 20% of those who have been assessed as needing VR to be able to resume work participate in VR (25–27); (ii) many participate in rehabilitation too late (25–27); (iii) many of those who participate receive inadequate rehabilitation input (25, 26, 28). The evidence would suggest these factors diminish the likelihood of return-to-work (28).
Resources required for rehabilitation
The effectiveness, quality and quantity of the resources involved in VR are, of course, important for success in work resumption. Individuals may seek VR from a number of sources: (i) medical rehabilitation, e.g. primary care, occupational health, private PRM units or hospital-based departments of specialized rehabilitation medicine (ICF e580); (ii) the employment office (ICF e590, e585); (iii) public insurance offices or private insurance companies (ICF e 570); (iv) employers, if they have rehabilitation responsibilities in the workplace (ICF e 590); and (v) social services (ICF e570).
The resources available for VR vary. The association between use of VR resources and work resumption for patients with neck, shoulder or back problems has been reviewed (28). Studies of VR show greater chance of return-to-work when multidisciplinary treatment was given compared with unidisciplinary (unimodal) treatment (e.g. 29). VR programmes should include education, as results have been shown to be better than when education is not included (30).
Early rehabilitation produces better results than delayed rehabilitation even when it is used for a longer time (31, 32, 34). Better results are produced when participants influence their own rehabilitation goals (34). Participants are more likely to return to work if they are offered modified work and a structured return to the workplace. They are less likely to report sick again if their work tasks have been modified and if the workplace is a good environment (35–37). Return-to-work coordinators also have a positive impact (38).
Coordination, cooperation and collaboration in vocational rehabilitation
The agencies that deliver VR may have defined responsibilities with no overlap with the responsibilities of other agencies delivering part of the return-to-work pathway. For maximum effectiveness there needs to be cooperation and collaboration between agencies, which can be at several levels: at the top of the organization; routinely within the structures or; between individuals practising in each of the organizations. Such cooperation may comprise: (i) multi-agency cooperation between different authorities with responsibility for VR – “Cross-sector rehabilitation”; (ii) cooperation between different medical specialities, e.g. PRM, orthopaedic surgery, neurology, psychiatry; (iii) multidisciplinary collaboration between different professionals within PRM teams.
When multi-professional cross-sector teams hold systematic rehabilitation group meetings, the results in terms of work resumption are better than when such cross-sector meetings do not take place (15, 16).
Economic factors and labour market
Economic factors within each country influence the success of VR at all levels – individual, organizational and societal. For instance, in a recession, it is more difficult for disabled people to return-to-work and the number of disabled people granted pensions increases.
A review of VR for neck, shoulder and back pain reported that there was a greater chance of work resumption when (28): (i) partial sickness benefit was provided prior to the start of VR compared with full benefit (30, 39); (ii) the person lived in a region with a low level of unemployment (40); (iii) low national unemployment rates prevailed (41). People are less likely to return to work: (i) following a long period of sickness absence before VR (30); and (ii) when disability compensation is higher (42–45).
Medical factors
Medical factors that influence the likelihood of work resumption include the type and extent of impairments, complications, co-morbidity, medical rehabilitation resources, relations between primary care rehabilitation and PRM specialists, waiting times in the healthcare sector and physicians’ willingness to issue sickness certificates.
In the review of risk factors quoted above (28), people were less likely to return to work if they had: (i) intense pain compared with moderate pain (46); (ii) nerve root symptoms in addition to back problems compared with no neurological symptoms (47); (iii) more treatment before VR compared with less (48); (iv) limitations in ADL (49); (v) depression as co-morbidity (50). There was greater chance of return-to-work when: (i) reduction of pain had been achieved (51); (ii) the injury was a first one rather than when there was a history of repeated injury (52); (iii) the person had received less rather than more back surgery (51).
Personal factors
Personal factors, such as educational background, self-efficacy, immigration status, sex and age are important and can influence the odds of resuming work after illness or injury.
A person’s psychological factors that promote return-to-work include (28): they (i) had already considered a change of occupation; (ii) had greater life satisfaction; (iii) were highly cooperative; (iv) had greater self-esteem (see also 53); (v) strongly believed they would return-to-work. Return-to-work was less likely when the patient had: (i) reduced internal locus of control; (ii) less motivation for work resumption.
MODELS OF VOCATIONAL REHABILITATION
In most countries, the general practitioner issues sickness certificates. Many will have little training in VR or even in rehabilitation. Increasingly, rehabilitation medicine or occupational medicine provide training and this raises awareness of the need to consider VR for those at risk of long-term work loss (e.g. Sweden, UK).
New legislation in the UK will require that before people obtain Employment Support Allowance, they are assessed for their ability to work and offered rehabilitation or training. This will mainly be provided outside the health service by private companies who will assess capacity to work and provide input to address the deficiencies (54).
In Germany, the onus is on the employer to draw up a plan for Disability Management. This has to be done when the employee is absent from work for more than 6 weeks, otherwise the employee will not be eligible for benefits (55). In the Netherlands, the new Work and Income according to Labour Capacity Act requires that the person is assessed before benefits are given (56).
In Sweden, employers are responsible for part of VR, such as testing working capacity, work training, transfer to another post, changes in work tasks or working hours. The employer’s responsibility for financing VR is restricted to measures that can be performed within or in direct connection with the employer’s own enterprise or business. The Social Insurance Office makes up the VR plan. Social security usually has no direct responsibility for VR in Sweden, but gives economic support when a family cannot support itself. Social security has an interest in successful VR in order to reduce its costs (57).
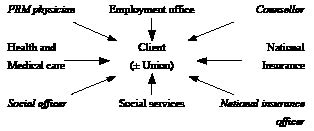
Many people require the full multidisciplinary team of rehabilitation physician, psychologist, physiotherapist, occupational therapist, social worker and ergonomist. The wider VR team will include the professionals outlined in Fig. 7.
Fig. 7. Interactions of some of the players in return-to-work. Many patients require the full multidisciplinary rehabilitation team, and some of those patients/clients need, in addition, support from a counsellor of the Employment office, a National Insurance officer and perhaps a social officer from the Social services. PRM: physical and rehabilitation medicine.
There are many models of VR. Most require cooperation between those in different parts of a single service, such as social security, and between agencies; their effectiveness will depend on the extent of cooperation and collaboration.
Models may be defined according to whether all parts of the assessment, interventions and follow-up are delivered by staff within the system (“closed”) or, as is more usual, the system is “open”. Two examples of a closed system worth noting are: (i) In the UK, since the Second World War, the armed services have run their own highly intensive rehabilitation service. Participants continue to draw their pay and are subject to service discipline. They participate in intensive rehabilitation tailored to their needs in individual and group work, and over 90% return to work (58); and (ii) In Switzerland, SUVA (serving two-thirds of all Swiss workers), the insurance company providing prevention, rehabilitation and reintegration for those who have accidents and occupational conditions, has 3 types of service; standard for those whose needs are satisfied by compensation; normal for those who can return rapidly to the workplace and; complex for the 5% whose service consists of situational analysis, procedural planning, case management and closure (20).
SUVA uses a networked, multidisciplinary approach using in-house and external expertise as necessary. Their response is rapid and flexible and the client is involved throughout. The result is that clients are satisfied, and that there was a 26% reduction in disability pensions within 4 years of commencing this system. The costs of disability pensions has dropped by one-third without compromising practice (59).
All Scandinavian countries (which do not use an insurance-based system) are based on the principle of universal coverage of services, which utilizes the back-to-work model. Everyone who can do so is supposed to support him or herself by work. Society takes active measures to help individuals to earn their living through work rather than exist passively on benefits. This requires the patient’s active participation in VR. Although there is a common model, welfare policies have developed differently in each Scandinavian country and there are varying solutions for how to improve efficiency in VR. Sickness absence for employees in Sweden and Norway is higher than in Denmark, Finland and Iceland, resulting in excessively high costs at present (60, 61).
In Austria, personal insurance is compulsory and is provided by government insurance institutions. Within each institution 3 main branches of insurance are defined: health insurance, accident insurance and retirement insurance/pension fund. Groups of employers offer their employees different combinations of finance for the 3 branches of insurance (62).
The examples used in this educational review come from the author’s countries of practice. However, these are representative of the health, social insurance and employment systems across Europe. Descriptions of other models of VR can be found for Belgium (63), France (64), Greece (65), Italy (66), Ireland (67) and Spain (68).
OUTCOME MEASURES
The most tangible outcomes in VR are return-to-work and the numbers of days on sick leave. Outcomes should not merely be recorded as “fully fit” or returned to work, but recorded explicitly as returned to full-time, part-time, or sheltered or voluntary work. When assessing work incapacity, a person’s activity limitations need to be related to the particular job that exists or is the planned goal after VR. A judgement has to be made as to whether a return-to-work that is less demanding or commands less pay is as successful as when the person returns to their previous work.
EFFECTIVENESS OF VOCATIONAL REHABILITATION
There are many randomized controlled trials (RCT) demonstrating the impact of VR on long-term pain conditions (2). However, only a proportion report work resumption or sick leave as outcome measures, which are the most important for the evaluation of the effect of a VR programme. Even if there are associations between work resumption and reduced level of pain intensity/improvement in relevant activities after VR, the effect of VR on these parameters do not necessarily imply work resumption or reduced sick leave.
The term multimodal rehabilitation means rehabilitation using several ”modalities” instead of only one or two, and implies a broad, coordinated, comprehensive rehabilitation programme usually with a combination of medical and psychological measures, such as cognitive behavioural therapy (CBT), with physical activities, training or physiotherapy. Since such programmes involve different rehabilitation professionals they sometimes have the designation multiprofessional. Some RCTs involving multimodal rehabilitation have included work resumption or days on sick leave as outcome measures. One example is that of the Finnish studies (69, 70) of multimodal rehabilitation of patients with persistent or recurrent back pain showing, at 30 months, significantly less sick leave overall and fewer days due to musculoskeletal problems than ”treatment as usual”, but no significant difference in progression onto disability pension. Another example of rehabilitation for patients with long-lasting back pain (71) showed less sick leave and fewer disability pensions for women at 18 months following a 4-week behavioural physiotherapy programme and a 4-week combination of that programme with CBT compared with controls.
A 3-year study of multidisciplinary behavioural programme has also been reported (72). A team-based outpatient multimodal programme for back pain patients demonstrated less sick leave for men than ”treatment as usual” at 26 months (73). A programme for patients with long-term back pain treated by graded activity combined with problem solving therapy (a variety of CBT) resulted in fewer sick leave days than graded activity combined with group tuition (74). Less sick leave was reported for patients with back pain 2-years after a programme of functional restoration combined with psychological treatment (75).
A systematic review of the efficacy of VR for patients on sick leave due to low back pain presented evidence of clinically relevant effects on work resumption compared with conservative treatment (76). The effect was better for patients with less than 3 months sick leave before the intervention than for those with more than 3 months.
A functional restoration programme for patients with work-related long-term musculoskeletal injuries reduced the number of pensions granted compared with ”treatment as usual” (77). A 12-week multimodal programme twice a week for prolonged neck pain gave better ”subjective working capacity” than ”treatment as usual” (78).
Several systematic reviews of multimodal rehabilitation for chronic back pain with data on work resumption and days on sick leave are presented (29, 79, 80) and some on chronic pain in general (81, 82). The conclusions of the reviews regarding protracted pain conditions demonstrate that pain is reduced, more people resume work, and sick leave periods become shorter if a multimodal rehabilitation programme is followed compared with controls, and compared with less comprehensive programmes comprising, for example, unimodal input (82).
There is less evidence to support VR in other conditions. One study, which recruited participants with a variety of diagnoses, demonstrated that 52% had attained full working capacity directly after completing VR, with 37% still at full working capacity 2 years later (33). The risk of work disability can be temporarily reduced for up to 4 years by means of vocationally-oriented multidisciplinary interventions (83). Return-to-work following multidisciplinary VR for patients with musculoskeletal and psychiatric diagnoses was 80% compared with 66% in the control group at 4 months (84). Studies have shown improvements in work resumption when CBT was offered and fitness and health problems were addressed in patients with mental health conditions (24). Return-to-work rates range from 12% to 70% after VR for traumatic brain injury patients (85). Recommendations for enhancing return-to-work for stroke survivors have been presented (86).
Arising from this evidence we need to consider which kind of rehabilitation programme gives the best long-term effects on work resumption or reduced absence due to illness. The evidence appears to be incomplete, but the consensus is that the core team should be multidisciplinary and should include all the professionals most commonly needed for assessment and intervention. The wider VR team should include those who can deliver education and those who represent the other authorities that need to be involved to facilitate return to work.
Economic effectiveness
The costs to an individual of not working include the increased cost of the disability itself, of staying at home and of attending medical services. There are also the costs to the person’s family. A variable amount of these costs may be reversible with early and intensive VR interventions.
Multidisciplinary VR programmes are expensive and the question is frequently asked whether this is justified: comparing the cost of the intervention with the time in work required to pay back this expenditure can provide evidence in its favour.
In an official Swedish report (27) on VR it was calculated that 1 SEK invested in VR would give 10 SEK back to society. Patients with very long sick leave and complex impairments often need comprehensive rehabilitation and input from a full rehabilitation team, which increases the cost. An example of this is a study of the economic consequences of an 8-week multiprofessional programme for patients with persistent pain (87). The programme reduced production losses due to sick leave. When this benefit was compared with the actual cost of the programme, the total cost was recovered when the successfully rehabilitated patients had worked for 9–17 months. Additional work yielded net economic benefits to society. Assuming patients remain in work at 3 years and have done so for the full 3 years, the economic benefits are more than 3.5 times the running cost.
More developed forms of cooperation between teams lead to economic gains for society due to improved production caused by fewer sick leave days. In this example this was systematic cooperation between employer, occupational health service and social insurance office with regular cross-sector team meetings (15). No extra investment was needed for the changed working model; it was merely another way of management. Those who received more coordinated VR had fewer sick leave days than those who received the control service (5.7 days per month per person over 6 years). This translates as an estimated average economic benefit for society of €36,600 per person over a 6-year period (15). Cost-effectiveness and cost-benefit studies of various VR programmes have been reported, showing positive results (73, 88–93).
HISTORY-TAKING USING ICF
A complete medical history and full physical examination is an essential first step. The history must include educational and vocational details, previous injuries, possible problems on the job and recovery periods, and interests and leisure activities, as this may open the possibility of alternative employment. Self-reported participation and activity limitations may be helpful (94).
The history is the first step when preparing a rehabilitation plan, and also the first step when assessing work capacity. Gobelet et al. (95) and Chamberlain & Frank (96) have stated that medical assessment should start early in the rehabilitation programme.
The ICF is a useful tool to describe human functioning and the consequences of health problems on activities and participation (4). Return-to-work can depend on numerous factors: impairments in body functions and structures (e.g. pain, reduced range of motion, muscle weakness), activity limitation (e.g. in lifting, walking, ADL), participation restriction (e.g. job, social events, leisure), environmental factors (e.g. physical environment, such as transport, attitudes and support from the home, workplace, family and friends,) as well as personal factors (e.g. age, sex, coping strategies) influence each other in varying extents.
An ICF core set for disability evaluation in social security has been developed to evaluate rights to long-term benefits (97) (Table III). This core set is generic, including 20 ICF categories. Compared with other core sets this is a small number, which is a useful advantage.
| Table III. Core set for disability evaluation in social security |
| Code | Chapter | Title | 1st vote (n = 20) | 2nd vote (n = 9) |
| b164 | Mental functions | Higher-level cognitive functions | 19 | |
| b280 | Sensory functions and pain | Sensation of pain | 13 | 5 |
| b455 | Functions of the cardiovascular, haematological, immunological and respiratory systems | Exercise tolerance functions | 9 | 5 |
| b710 | Neuromusculoskeletal and movement-related functions | Mobility of joint functions | 12 | 5 |
| b730 | Neuromusculoskeletal and movement-related functions | Muscle power functions | 13 | 6 |
| d110 | Learning and applying knowledge | Watching | 16 | |
| d115 | Learning and applying knowledge | Listening | 16 | |
| d155 | Learning and applying knowledge | Acquiring skills | 14 | 5 |
| d177 | Learning and applying knowledge | Making decisions | 12 | 5 |
| d220 | General tasks and demands | Undertaking multiple tasks | 20 | |
| d240 | General tasks and demands | Handling stress and other psychological demands | 20 | |
| d399 | Communication | Communication, unspecified | 17 | |
| d410 | Mobility | Changing basic body position | 17 | |
| d415 | Mobility | Maintaining a body position | 20 | |
| d430 | Mobility | Lifting and carrying objects | 19 | |
| d440 | Mobility | Fine hand use | 19 | |
| d445 | Mobility | Hand and arm use | 19 | |
| d450 | Mobility | Walking | 14 | 7 |
| d470 | Mobility | Using transportation | 20 | |
| d720 | Interpersonal interactions and relationship | Complex interpersonal interactions | 16 | |
| From Brage et al. (97), printed with permission from Informa Healthcare. |
A practical framework for the ICF in job placement has been described and body functions, activity and participation, environmental and personal factors, are dealt with systematically in this framework (98). The agreement of ICF core sets for back pain/widespread pain and the instruments used for work capacity assessment at a University Rehabilitation Medicine clinic has been described (99). In addition, the agreement between clinical assessment and back-to-work predictors were analysed. The tables describe the relevant ICF codes and the clinical method used to assess the item.
What ICF categories insurance physicians (IPs) take into account in assessing short- and long-term work ability has been analysed (100). It was found that IPs predominantly consider “functions and structures” and “participation” to be important. The components “environmental factors” and “personal factors” were rarely mentioned.
Who should do the history-taking and examination? The answer differs from country to country and the circumstances of the person. It is usually done by the general practitioner or a specialist in PRM, or a doctor working with a social government organization. It is important that the PRM doctor takes a full history, but the responsibility for this in terms of occupational health may lie with the occupational health physician. It is also incumbent on the medical practitioner who certifies fitness to work that he or she has taken a full history and done a complete examination.
There may be a conflict of interest for the general practitioner who regards his or her first duty as the support of the patient, but who is asked by the government or insurer to provide evidence for ability to work. It may therefore be better for specialized physicians not directly responsible for the patient’s care to be involved in this certification (95). This has to be balanced by the general practitioner’s knowledge of the patient and family over many years which may provide useful insights into their return to work.
Factors that may negatively influence return-to-work have to be recognized (28, 95, 101). These include older age, sex, health status, ethnicity, low social status and poor educational attainment. In some countries (e.g. Sweden) only health status and its functional consequences are taken into account when assessing work ability for the national insurance office. Extended sick leave and expectation concerning likelihood of return to work also have an influence (8).
ASSESSMENT OF WORK CAPACITY
The evaluation of various functional capacity tests has been discussed (95, 102). The assessment tests most frequently used in the EU are the progressive isoinertial lifting evaluation (PILE Test) (103), Isernhagen’s functional capacity evaluation (104) and the ERGOS work simulator (105). Work observation has proven to be very useful. Bicycle spiroergometry for the evaluation of work capacity has been described (106).
The compatibility of assessments with the ICF has been analysed (107, 108). There are 2 approaches to integrate assessment tools into the ICF: one based on the aim of an assessment tool (“goal-oriented”) and another by allocating several items or assessment domains to ICF categories by means of linking (109, 110). Many elements of the tests mentioned above have been linked to different ICF items. With regard to generic instruments, the use of the ICF seems possible, although one has to check whether all the relevant ICF domains are considered. The use of some of the specific instruments seems more difficult if they are mainly based on the ICD-10.
Whether the assessments were related to goal-oriented rehabilitation and the ICF-concept has been studied (108), and it is suggested that the following tests map onto the ICF and are useful measures for vocational assessment: (i) activity: ERGOS, Isernhagen, ARCON (Applied Rehabilitation Concepts; lumbar range of motion), Blankenship (detecting submaximal efforts), PACT-Test (Performance Assessment Capacity Test), IMBA (Integration von Menschen mit Behinderungen in die Arbeitswelt); (ii) body function: Neutral-0-method, Isokintetics, bicycle ergometer; (iii) personal factors: AVEM (Arbeitsbezogenes Verhaltens- und Erlebensmuster); (iv) multiple components: e.g. 36-item Short Form Health Survey, Oswestry, Lysholm and Gillquist Score (108).
Studies are ongoing to find solutions on how to select tests, measurements and instruments to assess functioning and work capacity in clinical situations. The present review does not cover these studies. A general rule is to select tests that are as relevant as possible for the patient’s job or planned new job.
REPORT WRITING
The physician’s role concerning report writing is important for the patient’s possibility of work resumption. The report usually forms the basis of decisions taken at the insurance level regarding disability pension or return-to-work. In some countries, these reports have to be given a particular format. It may be necessary to use the ICF when describing functioning and disabilities.
Essential elements in reports are:
• Patient’s profession and employer, or if unemployed, since when
• Description of the onset (date) of the work-limiting disease/injury and its course, and medical care received (where and when)
• Relevant findings of physical examination and investigations regarding physical and cognitive impairments, including functional impairments (ICF body functions). (If applicable, a description of whether criteria for the suggested diagnoses are fulfilled). If available and appropriate, investigations made by other professionals of the rehabilitation team can preferably be quoted (and if so, with an indication that it is a quotation from another rehabilitation professional’s report)
• Diagnoses (and ICD numbers) with, if relevant, an indication of which diagnosis is the main one for the work incapacity
• Summary of the medical condition with a focus on how it influences physical and mental activity limitations (according to ICF categories) (also, including a summary of possible other rehabilitation professionals’ reports). A clear statement about physical or cognitive barriers to the performance of particular work tasks. An assessment of working capacity may be given relating to: (i) current work; (ii) adapted work at the present employer; (iii) any normal job in the whole labour market; and (iv) sheltered job in some form
• Assessment of whether improvement of the impairments and activity limitations is expected: will the disabilities be fully reversible? Which measures would be needed to improve functioning? (What measures are already planned? Referrals? To which agencies and when?) Is there a need for a more comprehensive assessment of working capacity at specialist level?
• Assessment of how long the present impairments and activity limitations will last.
GLOSSARY
• Gainful employment: a relatively permanent job, providing income, compared with housework/ domestic work or other non-profit work and/or work not providing any income.
• Wage earner: someone who is paid a wage (or salary) for working for the employer. This term also includes when the employer gets some kind of subsidy for those wages from the social insurance system.
• Remunerative employment: (ICF d850) engagement in all aspects of work, as an occupation, trade or profession for payment, as an employee or self-employed. The employment can be part-time (ICF d8501) or full-time (d8502).
• Self-employment: (ICF d8500) remunerative work generated by the individual without a formal employment, e.g. as a craftsperson.
• Sheltered employment: this aims at giving people with disabilities and partial work capacity some employment, often with rehabilitative elements, usually run by the public sector or a not-for-profit organization. The jobs may be integrated in the public sector or in the form of particular enterprises based on sheltered employment. The person is remunerated at a normal rate, which may be subsidised.
• Employment with subsidy: a subsidy is given to a private or public employer for wages paid to disabled employees with reduced work capacity. The subsidy is usually time-limited and diminishes by gradual stages. The ICF system has, at present, no category for this.
• Adapted work: a job – usually at the original employer – where adjustments have been performed to adapt the work tasks to the needs of the former patient/worker.
• Work-like occupations: assessments of work capacity must often be done in situations that are as similar as possible to the person’s work and workplace to determine whether a patient needs formal vocational training (ICF d825). It is usually an adapted situation for the patients with perhaps reduced work hours and self-selected tempo etc – factors that need to be taken into account when assessing the “work” capacity – or functioning capacity.
A similar situation occurs when the assessment deals with whether the patient is able to begin seeking employment (ICF d8450). The process of seeking and preparing for employment is time-consuming and should begin as early as possible.
Seeking employment: when the health insurance benefit runs out because functioning has improved and the patient no longer has an employer, the person is in a job-seeking phase (ICF d8450) and usually moves from health insurance benefit to jobseeker’s allowance. The person is in that sense ready for work but as yet has no work.
• Non-remunerative employment: engagement in work without payment, such as voluntary work, charity work, working for a community, sports club or religious group (ICF d855).
• Supported work: where a participant receives help and guidance from a job coach before returning to an independent work role.
REFERENCES