Thomas H. M. Heung, MSc1 and Shamay S. M. Ng, PhD2
From the 1Physiotherapy Department, Tuen Mun Hospital and 2Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
Thomas H. M. Heung, MSc1 and Shamay S. M. Ng, PhD2
From the 1Physiotherapy Department, Tuen Mun Hospital and 2Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
OBJECTIVE: To identify the effect of chair seat height and turning direction on the Timed Up and Go scores of patients after stroke.
DESIGN: A cross-sectional study.
SETTING: A geriatric day hospital in Hong Kong.
SUBJECTS: Twenty-five patients with sub-acute stroke.
METHODS: The time taken to complete the Timed Up and Go test with various chair seat heights (65%, 90% and 115% of each subject’s leg length – distance from lateral knee joint line to ground in sitting) and turning directions (toward the affected and unaffected side) was recorded using a stopwatch with randomized test order.
RESULTS: There were significant differences in Timed Up and Go scores between the 3 levels of chair seat height (p < 0.001), with the lowest Timed Up and Go scores recorded when the seat height was 115% of the subject’s leg length and the highest at a seat height of 65% of the subject’s leg length. Turning toward the affected side was found to be significantly quicker than turning toward the unaffected side (p < 0.001).
CONCLUSION: Chair seat height and turning direction significantly influence the Timed Up and Go scores of patients after sub-acute stroke. Optimizing chair seat height with reference to subject’s leg length and turning direction is essential when using the Timed Up and Go test as an outcome measure in stroke rehabilitation.
Key words: outcome assessment (health care), stroke, rehabilitation.
J Rehabil Med 2009; 41: 719–722
Correspondence address: Shamay S. M. Ng, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China. E-mail: shamay.ng@inet.polyu.edu.hk
Submitted January 23, 2009; accepted May 7, 2009
INTRODUCTION
The Timed Up and Go (TUG) test (1) was modified from the Get-up and go test (2) by Podsiadlo & Richardson in 1991. It is a basic functional mobility test that has shown good construct validity and reliability in assessing the basic functional mobility of stroke survivors (3, 4), frail elderly people (1), patients with idiopathic Parkinson’s disease (5), and those with unilateral lower limb amputation (6). It can be used to measure intervention outcomes (7), to screen people for risk of falling (8), to predict declining ability in the activities of daily living (9), and for nursing home placement (10).
Different chair seat height, ranging between 40 and 50 cm, has been used in previous studies (4, 11–14). As seat height affects patients’ ability to stand up after stroke (15), optimizing the seat height used in TUG assessments is important. In addition, no study has yet investigated the effect of turning direction on stroke survivors’ TUG scores.
The objectives of this study were to investigate: (i) the effect of chair seat height, and (ii) the effect of turning direction on TUG scores in patients after stroke.
METHODS
Participants
Twenty-five subjects, mean age 66.1 years (standard deviation (SD) 6.2) and mean 87.8 days after a single stroke (SD 40.4), were recruited at a local rehabilitation day hospital. The subjects recruited all had Mini-Mental State Examination (16) scores over 23; had no or mild plantar-flexor spasticity (the Composite Spasticity Scale (17) score of the plantar-flexor of the affected side ankle was ≤ 9); and could walk 6 m unassisted, though perhaps with a walking aid. Subjects were excluded if they had a medical co-morbidity or disability other than stroke, such as visual impairment, or if they had co-existing medical disorders that might have hindered a proper assessment.
According to Eekhof’s study (18), differences of 5 sec in TUG scores were required to represent significant differences in the results for different chair heights and directions. A sample size of 25 subjects would be needed if the threshold for statistical significance was set at 5% (alpha level = 0.05) and the power at 80% (beta level = 0.2).
The study was approved by the local ethics committee. The study procedure was clearly explained to all participants beforehand, and informed, written consent forms were signed before the assessments.
Measurements
Timed Up and Go test. The subjects were instructed to begin in a starting position of sitting upright with back leaning against the “chair back” with their hands resting on their thighs and feet placed directly under their knees. Timing began when the examiner said “Go”. They were required to stand up from the chair, walk 3 m at a comfortable speed, cross a line on the floor, turn around in the direction as instructed in advance, walk back, turn in the prescribed direction again and then sit down without falling onto the chair. Timing stopped when their backs touched the “chair back”. The time taken to complete the task was measured in seconds with a stopwatch. The same investigator performed all the testing.
Procedure
Each participant performed the TUG test under 6 experimental conditions in random sequence by drawing lots to analyse the effect of “chair seat height” and “turning direction” on TUG scores. The 6 conditions were:
• turning to the affected side, with a chair seat height of 115% of the subject’s leg length;
• turning to the unaffected side, with a chair seat height of 115% of the subject’s leg length;
• turning to the affected side, with a chair seat height of 90% of the subject’s leg length;
• turning to the unaffected side, with a chair seat height of 90% of the subject’s leg length;
• turning to the affected side, with a chair seat height of 65% of the subject’s leg length;
• turning to the unaffected side, with a chair seat height of 65% of the subject’s leg length.
The subject’s leg length was measured from the lateral knee joint line of the unaffected leg to the ground with the knee flexed at 90 degrees and wearing the subject’s usual footwear.
Each subject performed 2 familiarization trials with the seat height at 65%. They then performed 3 trials in each test condition with v1 min rests between trials. The average time in the 3 trials was used in the analyses.
Statistical analysis
Descriptive statistics described the demographic characteristics of the subjects. Significant main effects and any interaction of chair seat height and turning direction were sought using two-way analyses of variance (ANOVA) with repeated measures, followed by Bonferroni’s post-hoc multiple comparison test. The analysis employed Statistical Package for the Social Sciences software (Version 11.0, SPSS Inc., USA).
RESULTS
The demographic characteristics of subjects are shown in Table I. The TUG scores and their SD in each testing condition are summarized in Table II, and the mean chair seat height corresponding to 65%, 90% and 115% of our subjects’ leg length are shown in Table III.
| Table I. Descriptive characteristics of the subjects (n = 25) | |
| Variable | n (%) |
| Gender, male/female | 20 (80)/5 (20) |
| Type of stroke, haemorrhage/infarction | 2 (8)/23 (92) |
| Side of hemiplegia, left/right | 11 (44)/14 (56) |
| Walking aids Quadripod Stick Unaided | 16 (64) 6 (24) 3 (12) |
| Anti-footdrop device Need orthosis No orthosis | 7 (28) 18 (72) |
| Mean (SD) [range] | |
| Age, years | 66.12 (6.15) [55–75] |
| Body weight, kg | 59.14 (9.60) [44.90–84.3] |
| Height, m | 1.62 (0.08) [1.46–1.74] |
| Body mass index (kg/m2) | 22.42 (2.59) [18.22–27.84] |
| Score on the Cantonese version of the Mini-mental State Examination | 26.56 (2.31) [24–30] |
| Leg length, cm | 43.04 (2.3) [40–47] |
| Composite spasticity scale score | 6.84 (1.28) [5–9] |
| Days since first stroke | 87.84 (40.41) [24–175] |
| Functional reach, cm | 22.48 (4.99) [12–31] |
| Elderly mobility scale score | 17.28 (2.35) [13–20] |
| SD: standard deviation. | |
| Table II. Summary of Timed Up and Go (TUG) test results | ||
| Chair seat height, % of leg length | Mean TUG score, sec (SD) | |
| Turn affected side | Turn unaffected side | |
| 115 | 27.45 (12.02) | 28.97 (12.63) |
| 90 | 28.89 (12.55) | 30.60 (13.69) |
| 65 | 32.25 (14.87) | 34.49 (16.31) |
| SD: standard deviation. | ||
| Table III. Mean chair seat height corresponding to 65%, 90% and 115% of our subjects’ leg length | ||
| Chair seat height, % of leg length | Mean seat height, cm (SD) | Range, cm |
| 115 | 49.49 (2.65) | 46–54.05 |
| 90 | 38.74 (2.07) | 36–42.30 |
| 65 | 29.98 (1.50) | 26–30.55 |
| SD: standard deviation. | ||
Two-way repeated measure ANOVA showed no significant interaction between “chair seat height” and “turning direction” in terms of the TUG scores (p = 0.073; F = 2.772). The main effects of seat height and turning direction could thus be interpreted directly. The mean TUG scores with 65%, 90% and 115% heights were significantly different (p < 0.001; F = 24.787). Post-hoc multiple comparison test (Bonferroni) showed that there were significant differences on TUG scores between 65% and 90% height (p < 0.001), as well as between 90% and 115% height (p < 0.001) (Fig. 1). In addition, there was a significant difference in TUG scores between turning to the affected side (mean: 29.53 sec, SD 13.05) and the unaffected side (mean: 31.36 sec, SD 14.09) (p < 0.001; F = 41.590) (Fig. 2).
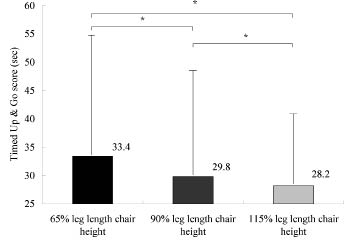
Fig. 1. Timed Up and Go scores with 3 seat heights (*p < 0.001).
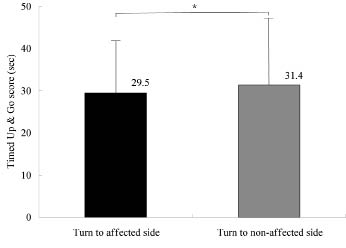
Fig. 2. Average Timed Up and Go scores turning to the affected and unaffected side (*p < 0.001).
DISCUSSION
This study with stroke subjects shows that TUG scores are significantly influenced by chair seat height. These results are consistent with a previous study of patients after elective hip- or knee-replacement surgery or spinal fusion with a seat height difference of 4 cm (19), but not with a study by Eekhof et al. with a seat height difference of 2 cm (18). The smaller seat height difference and different types of chairs used (an armchair, a high-backed chair, and an easy chair) in Eekhof’s study (18) might account for the negative findings.
It is not surprising that TUG times are longer when a lower chair is used. First, the total distance travelled by the subject’s centre of mass from a low chair to fully erect standing is necessarily greater (20). Secondly, a different sit-to-stand movement strategy is usually adopted to generate sufficient forward momentum to bring the centre of mass over the new base support in the flexion-momentum phase (21). There are also greater maximum hip and knee extension moments involved in the momentum-transfer phase (22–24). In our study, each subject’s leg length was used to normalize the seat heights in order to minimize any influence of a subject’s leg length on their TUG test performance, as a previous study found that loading on a subject’s leg and the strategies adopted during the sit-to-stand transition were affected by the subject’s leg length when the length was greater than 44 cm and the seat was 40 cm high (25).
It is interesting that the stroke subjects completed the TUG test more quickly when turning to the affected side. This finding contrasts with those of Chow (26), who found TUG times to be shorter when turning to the unaffected side with patients with hip and lower limb fractures. Differences in motor impairment, pain, muscle tone abnormality, the distribution of muscle weakness and skill in using a walking aid between the stroke and fracture patients may account for the different findings between these studies.
Thigpen’s group (27) investigated 55 subjects over 64 years of age, and found that those with balance dysfunction took more steps during turning, turned more slowly, and had longer TUG scores compared with those without balance difficulties. The investigators concluded that an increase in the number of steps during turning was one characteristic of turning difficulty in elderly people (27). It is plausible that the number of steps used in turning could determine the time taken in turning and thus determine TUG scores. In the present study, although the number of steps during turning was not formally recorded, the stroke survivors were observed to take more steps when turning to the unaffected side. This increased number of steps contributed to the longer TUG test times when turning to the unaffected side.
It is important to note that these conclusions can be applied only to subjects similar to those recruited in this study: patient after acute to sub-acute stroke (mean 87.8 days after a single stroke, SD 40.4). Moreover, one should note that the assessor of this study was not blind to research question. Note also that the interaction between “chair seat height” and “turning direction” had a p-value of 0.073. Some interaction between these 2 factors might have been revealed had the sample size been greater. Further research with a larger sample might be fruitful.
The design of the chair (the height of the armrests, the seat depth and the inclination angle of the back support) might also influence the TUG scores. Further exploration of these factors might profitably complement with three-dimensional motion analysis of gait patterns during turning using stroke survivors and healthy subjects. Lastly, we suggest that a commercial piano stool can be a useful chair for the TUG test in clinical setting, as it is not expensive and is convenient and rapid for adjusting the seat height, especially for seat heights at 90% of the subject’s leg length.
In conclusion, the most important findings of this study are that “chair seat height” and “turning direction” both significantly influence the TUG scores of stroke survivors. Optimization of the turning direction and the height of the seat with respect to the subject’s leg length are essential when using the TUG test to monitor the progress of functional mobility or using the TUG score as a screening tool after stroke.
REFERENCES
