OBJECTIVE: To evaluate the effects of pool exercise in patients with fibromyalgia and chronic widespread pain and to determine characteristics influencing the effects of treatment.
METHODS: A total of 134 women with fibromyalgia and 32 with chronic widespread pain were randomized to a 20-session pool exercise and a 6-session education programme or to a control group undertaking the same education programme. The primary outcomes were the Fibromyalgia Impact Questionnaire (FIQ) total score and the 6-minute walk test (6MWT). FIQ Pain and other health variables were included.
RESULTS: The FIQ total (p = 0.04) improved in the intervention group, with an effect size of 0.32. Patients who had participated in at least 60% of the exercise sessions improved in the FIQ total (effect size 0.44), the 6MWT (effect size 0.43) and FIQ Pain (effect size 0.69) compared with controls (p < 0.05). Long-term follow-up revealed lasting, but small, improvement (effect size < 0.29) in the 6MWT among the active participants (p < 0.05). Analyses within the subgroups showed that patients with milder stress, pain or depression improved most by treatment on the FIQ total (effect size > 0.50, p < 0.05) compared with controls.
CONCLUSION: The exercise-education programme showed significant, but small, improvement in health status in patients with fibromyalgia and chronic widespread pain, compared with education only. Patients with milder symptoms improved most with this treatment.
Key words: pain measurement, fibromyalgia, exercise therapy, stress, psychological, outcome assessment (health care).
J Rehabil Med 2009; 41: 751–760
Correspondence address: Kaisa Mannerkorpi, University of Gothenburg, Sahlgrenska Academy, Department of Rheumatology, Guldhedsgatan 10, SE-413 46 Göteborg, Sweden. E-mail: kaisa.mannerkorpi@rheuma.gu.se
Submitted September 9, 2008; accepted April 28, 2009
INTRODUCTION
Fibromyalgia (FM) is characterized by long-lasting, widespread pain and generalized allodynia, often accompanied by fatigue, stiffness, non-restorative sleep, distress (1), activity limitations (2) and impaired body functions (3). Aberrations in physiological pain-processing mechanisms (4), together with psychological and environmental factors, are thought to interact in the development and maintenance of FM (4). Criteria for FM include a history of long-lasting widespread pain and pain at 11 of a total of 18 tender points examined by manual palpation (1), while patients with widespread pain who do not fulfil the tender-point criteria are classified as having chronic widespread pain (CWP) (1). The prevalence of FM in the general population ranges from 1% to 3%, while that of CWP is approximately 10% (5, 6), and it has been suggested that CWP and FM represent overlapping disorders rather than discrete diseases (7).
The biopsychosocial model of health acknowledges that the individual’s own beliefs and actions can influence health. Educational programmes have been developed to enhance self-efficacy for the management of FM (8, 9), and when combined with exercise, positive effects have also been found in physical function and symptoms (8–13).
More knowledge is needed about the effects of education and physical exercise, respectively, to develop guidelines for treatments of patients with FM or CWP. Two earlier studies reported improved self-efficacy in patients participating in education or education-exercise programmes (8, 9), while patients in the combined treatments improved most (8). A recent study showed that patients participating in an education plus exercise programme improved more than those randomized to an education programme (13).
It has been found previously that patients with more severe pain and physical impairments obtain the best effects from operant- and cognitive-behavioural treatment programmes (14), while, to the best of our knowledge, there are no studies reporting which patients with FM or chronic pain benefit most from physical exercise. Exercise is troublesome for some patients due to the activity-induced pain, while others appear to manage it (15, 16). A high level of distress or stress may also impact on the ability to exercise (17).
The aim of the present study was therefore to investigate the effects of supervised physical exercise on health status and body functions in patients with FM or CWP, and to analyse whether the level of pain, distress, stress and activity limitations might influence the outcomes. As pool exercise has been found to be suitable also for patients with FM, presenting severe impairments (18) it was chosen as a mode of exercise for this study. The intervention group was compared with an active control group, participating in the same education programme as the patients in the intervention group.
METHODS
Study design
A randomized controlled trial (RCT) aiming to compare the effects of a 20-session exercise programme combined with a standardized 6-session education programme based on self-efficacy principles with an active control group, which undertook the same education programme. The primary outcome measures were health status using the Fibromyalgia Impact Questionnaire (FIQ) total score and body functions using the 6-minute walk test (6MWT). The secondary outcomes included pain (the FIQ Pain), fatigue (the FIQ Fatigue), depression (the Hospital Anxiety and Depression Scale (HADS-D)), health-related quality of life (the 36-item Short Form Health Survey (SF36)) and amount of leisure time physical activity (the Leisure Time Physical Activity Instrument (LTPAI)). The exploratory outcomes included clinical manifestations of stress (the Stress ans Crisis Inventory (SCI)), multiple dimensions of fatigue (the Multidimensional Fatigue Inventory (MFI-20)) and experience of physical activity. Outcomes were evaluated using both an intention-to-treat (ITT) and a per-protocol (PP) design, which was defined as attendance at least 60% of the sessions. Per-protocol analyses were conducted to study changes in patients who completed most of the protocol they were randomized to, as several studies have reported poor compliance with exercise protocols in FM (19). The outcomes were assessed at the study start and after 20 weeks. Follow-up was conducted 11–12 months after the baseline. The subgroups were created using rating scales assessing aspects of health that were hypothesized to influence the primary outcomes. The following variables were selected for subgroup analyses: pain (the FIQ Pain), distress (the HADS-D), stress (the SCI) and activity limitations (the SF36 Physical Function). To study clinical relevance of treatment effects, effect sizes were calculated.
Recruitment
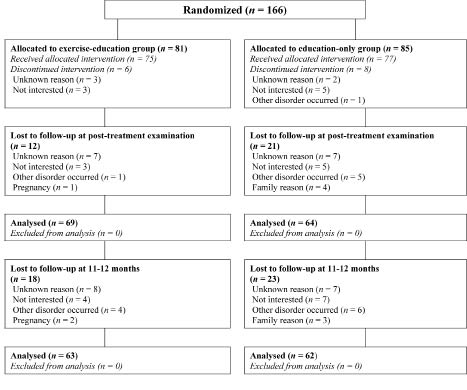
A total of 166 patients were recruited. This number enabled a subgroup analysis. The patients were recruited from primary healthcare centres in western Sweden by searching patient journals for the diagnoses of FM and CWP (between 1995 and 2004) and by consecutive recruitment (in 2004 and 2005). A systematic search of patient journals, found 818 subjects who were potentially eligible, but when the journals were scrutinized, 520 individuals did not fulfil the inclusion criteria for FM or CWP, or they fulfilled exclusion criteria. The remaining 298 individuals were contacted by post (n = 55) or telephone (n = 243) for further screening. Forty-eight persons could not be contacted, 35 did not meet inclusion criteria, and 61 declined to participate in the study, while 154 agreed to participate in an examination. Twenty-two of them did not meet inclusion criteria, and 12 were excluded due to treatment in progress (n = 3) or severe disorders (n = 9) and 18 declined to participate. A final total of 102 patients was referred to the intervention study, but one was excluded for not fulfilling the inclusion criteria, leaving a total of 101 patients. At the same time, 93 individuals were consecutively recruited to the study. Sixty-five of them fulfilled the criteria and agreed to participate in the study. The study population therefore comprised 166 patients, 134 of whom fulfilled the criteria for FM and 32 for CWP (see flow-chart in Fig. 1).
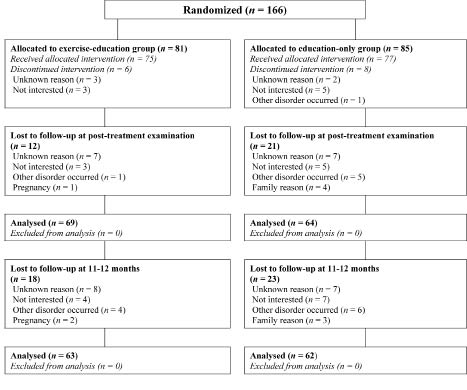
Fig. 1. Flow-chart for the study population.
The inclusion criteria were: women with FM or CWP, in the age range 18–60 years. Patients who had a history of widespread pain for at least 3 months and pain at manual palpation at 11 out of a total of 18 examined tender-point localizations were classified as FM (1). Widespread pain was defined as pain above and below the waist, on the right and left side and at the axial localization (1). Patients with widespread pain for at least 3 months who did not fulfil the tender-point criteria were classified as CWP.
The exclusion criteria were: other severe somatic or psychiatric disorders, such as stroke or schizophrenia, inability to understand Swedish, allergy to chlorine, ongoing exercise therapy supervised by a physical therapist, or plans to start such therapy during the study period.
Randomization
The patients were allocated to one of the 2 treatment programmes using stratified randomization for the disorder, FM or CWP (20). Sealed envelopes were prepared by the statistician, who created the allocation sequence. When the patient examination had been conducted, the numbered envelope was opened by a person who was not involved in the examination, and who also informed the patient about the treatment group to which she had been randomized.
Ethics
The study was approved by the ethics committee at Göteborg University. Written and oral information was given to all the patients and written consent was obtained from all the patients.
Background data
The trained examiners were blinded to the patients’ group assignments. Demographic data, and data on employment and pharmacological treatment, were gathered using a standardized interview (see Table I). Pain localizations (0–18) were recorded by the patient on a self-administered sheet (6). Tender points were examined by manual palpation (1). Muscle tenderness was examined using a Somedic algometer (Somedic Production AB, Sollentuna, Sweden) (21) (Table I).
|
Table I. Demographic data of the patients randomized to the Exercise-Education and Education programmes, n = 166. p-values for the differences between the 2 groups are given
|
|
|
Exercise-Education
n = 81
|
Education
n = 85
|
p-value
|
|
Mean (SD)
|
Mean (SD)
|
|
Age, years
|
44.6 (9.26)
|
46.5 (8.30)
|
0.235
|
|
Symptom duration, years
|
10.3 (6.85)
|
10.6 (7.46)
|
0.925
|
|
Tender points, n
|
13.4 (3.68)
|
13.6 (3.41)
|
0.796
|
|
Algometer, kPa/sec
|
180 (72.94)
|
187 (75.17)
|
0.702
|
|
Pain localization, 0–18
|
12.5 (3.42)
|
13.3 (3.42)
|
0.105
|
|
|
n (%)
|
n (%)
|
|
|
Living with an adult
|
59 (73)
|
64 (75)
|
0.854
|
|
Born outside Sweden
|
9 (11)
|
18 (21)
|
0.120
|
|
Education
|
|
≤ 9 years
|
18 (22)
|
20 (24)
|
|
|
10–12 years
|
44 (54)
|
45 (53)
|
|
|
> 12 years
|
19 (24)
|
19 (22)
|
0.819
|
|
Employment
|
|
Not working
|
45 (55)
|
53 (62)
|
|
|
Working part-time
|
28 (35)
|
23 (27)
|
|
|
Working full-time
|
8 (10)
|
9 (11)
|
0.562
|
|
Sick leave
|
|
0%
|
61 (75)
|
68 (80)
|
|
|
25–75%
|
7 (9)
|
9 (11)
|
|
|
100%
|
13 (16)
|
8 (9 )
|
0.294
|
|
Sick pension of limited duration
|
|
0%
|
61 (75)
|
61 (72)
|
|
|
25–75%
|
10 (13)
|
9 (11)
|
|
|
100%
|
10 (12)
|
15 (18)
|
0.501
|
|
Disability pension
|
|
0%
|
51 (63)
|
49 (58)
|
|
|
25–75%
|
14 (17)
|
15 (18)
|
|
|
100%
|
16 (20)
|
21 (25)
|
0.433
|
|
Pharmacological treatment
|
|
Analgesics
|
57 (70)
|
61 (72)
|
0.978
|
|
Psychotropic drugs1
|
36 (44)
|
38 (45)
|
0.110
|
|
1Antidepressants, sedatives.
SD: standard deviation.
|
Self-administered questionnaires
Fibromyalgia Impact Questionnaire (FIQ). This is a self-administered questionnaire, comprising 10 subscales of disabilities and symptoms, ranging from 0 to 100, and validated for a Swedish FM population (22). A higher score indicates lower health status. The total score, being the mean of the 10 subscales, and the subscales for Pain and Fatigue were applied in the study.
Short-Form 36 (SF36). This is a generic instrument assessing health-related quality of life, comprising 8 subscales ranging from 0 to 100. The subscales building 2 composite scores, the Physical Component (PCS) and the Mental Component (MCS) (23), were included in the study, together with the subscales building the PCS. A higher score indicates better quality of life.
Hospital Anxiety and Depression Scale (HADS). This contains 14 statements, ranging from 0 to 3, in which a higher score indicates a higher degree of distress. The scores build 2 subscales: HADS-A for anxiety (0–21) and HADS-D (0–21) for depression. The cut-off score of 8 is suggested to indicate possible anxiety and depression (24).
Leisure Time Physical Activity Instrument (LTPAI). This instrument assesses the amount of physical activity during a typical week, divided into light and moderate exercise. The total score is the sum of the activities (25).
Stress and Crisis Inventory (SCI). The SCI comprises 35 items (0–4), assessing clinical manifestations of stress on a scale ranging from 0 “not at all” to 4 “very much”. The questions include physical and mental sensations. The total score ranges from 0 to 140 and a higher score indicates more stress (26). The SCI has been used in a previous study of chronic pain (27).
Multidimensional Fatigue Inventory (MFI-20).The MFI-20 contains 20 statements that build 5 subscales. Each subscale ranges from 4 to 20 and a higher score indicates a higher degree of fatigue (28, 29).
Experience of physical activity. This scale comprises 22 items ranging from 0 to 7 and assessing the following aspects related to physical activity: Activity-related Physical relaxation (AR), Activity-related Well-being (AW), Activity beliefs (AB), Activity-related symptoms (AS) and Activity habits (AH). A higher score indicates more dissatisfaction (30).
Physical test of body function
Six-minute walk test (6MWT). The patient was instructed to walk as quickly as she could without running. The test has shown satisfactory test-retest reliability in a Swedish FM population (31).
Procedure
Examinations. The trained examiners were blinded to the patients’ group assignments. The examination for the American College of Rheumatology criteria for FM and CWP included a pain localization sheet (6), a standardized interview and an examination of tender points (1). The patients completed a battery of questionnaires and performed the 6MWT. The FIQ, the SF36, the HADS, the LTPAI and the SCI were completed at baseline, post-test and follow-up. The MFI-20 and the Experience of activity scale were completed at baseline and post-test. The patients were instructed to continue their baseline medical treatment with no change throughout the 20-week study period, and their medical treatment was monitored at post-test.
Intervention. The education programme, which was designed to introduce strategies to cope with the FM symptoms, consisted of 6 1-h sessions, conducted once a week for 6 weeks. The programme was led by a physiotherapist. The pedagogical approach was based on the active participation of the patients through discussions and practical exercises. The topics were theories for long-lasting pain, pain alleviation, physical activity, stress, relaxation and modifications of lifestyle to enhance health. At each session, the patients drew up a plan (a contract) for physical activity for the next week and performed a short relaxation exercise. The control group received the same education programme. Details of the programme are shown in Appendix I.
The exercise programme comprised 20 sessions of 45-min pool exercise once a week for 20 weeks in temperate (33°C) water, supervised by a physiotherapist. The exercise was planned to permit individual progress, aiming to improve overall function and to motivate regular physical activity. The median value for exertion (6–20), measured by the Borg scale for rating perceived exertion (BRPE) (32), ranged from 9 (“very light”) to 11 (“light”) during flexibility, co-ordination and stretching exercises, while it was 13 (“somewhat hard”) during aerobic exercise. Heart rate (HR) was monitored with a Polar S610i HR monitor (Kempele, Finland) and expressed in values for age-adjusted maximum HR, 220 minus age (HRmax). The mean value for HR during the programme ranged from 48% to 65% HRmax, which corresponds with light to moderate intensity (33). Details of the programme are shown in Appendix II.
Statistics
Descriptive data are presented as the mean and standard deviation (SD) or the number and percentage. For comparisons between 2 groups, Mann-Whitney U test was used for continuous variables, Fisher’s exact test for dichotomous variables and Mantel-Haenszel χ2 test for trend in contingency tables for ordinal categorical variables. For comparisons within groups, Wilcoxon’s signed-rank test was used for continuous variables, while McNemar’s test was used for dichotomous variables.
Effect size was calculated for variables showing a significant change. Effect size for between-group analyses was calculated by dividing the mean difference between the post-test score and baseline score in the intervention group and in the control group by the pooled SD. Effect size for the 11–12 months follow-up was calculated as the mean difference between the follow-up score and baseline score divided by the SD at baseline. Effect sizes from 0.20 to < 0.50 were regarded as small, while effect sizes from 0.50 to < 0.80 were regarded as moderate (19). To control possible Type I errors, the upper limit of expected number of false significances for the secondary and exploratory variables was calculated by the following formula: α/1– α × number of tests – number of significant tests), where α is the significance level.
Pre-specified subgroups were created by dichotomized values for the SCI, the FIQ Pain, the HADS-D and the SF36 PF. The SCI, the FIQ Pain and the SF36 PF were dichotomized by the median value, as there are no known cut-off points for these variables indicating more or less pathology in a pain population, while the HADS-D was dichotomized by a score of 8, which indicates possible depression (24). The heterogeneity, an interaction between the independent variable, group membership and the change score for the primary outcome measure (the FIQ total and the 6MWT), was analysed using a generalized linear model for subgroup analyses. A significant heterogeneity implies different effects of the intervention for 2 subgroups. Differences in the change scores were analysed by Fisher’s non-parametric permutation test, and mean differences with 95% confidence intervals within each subgroup are presented in the graph. All significance tests were 2-tailed and values of p < 0.05 were concidered significant.
RESULTS
Study population
No significant baseline differences in demographic data were found between the patients (n = 166) randomized to either the intervention group (n = 81) or the control group (n = 85) (see Table I). Baseline pharmacological treatment is shown in Table I.
Use of analgesics at post-test was reported by 67% of the patients in the exercise-education group and by 65% in the control group. Use of antidepressants and/or sedatives was reported by 45% of the patients in the exercise-education group and by 44% in the control group. No significant change in pharmacological treatment over time was found for either of the 2 groups.
Intention-to-treat analyses (Table II)
Primary outcomes. Significantly higher improvement (p = 0.040, z = –2.049) was found for change in the FIQ Total in the exercise-education programme (–4.8, SD 13.2) compared with change in the control programme (–0.7, SD 12.2) after the 20-week study period. The effect size of the FIQ total for the intervention group compared with the control group was 0.32.
Change in the 6MWT in the exercise-education programme (7.5, SD 53.5) was not statistically significant (p = 0.067, z = –1.830) compared with change in the control group (–2.0, SD 63.2) after the 20-week study period.
Secondary outcomes. Significant improvement (p = 0.018, z = –2.370) was found for change in the FIQ Pain in the exercise-education group (–7.8, SD 22.6) compared with change in the control group (1.7, SD 19.5) after the 20-week treatment. The effect size of the FIQ Pain was 0.45 for the intervention group compared with the control group.
Exploratory outcomes. Change in the MFI-20 Reduced Motivation in the exercise-education group (–0.8, SD 3.3) was significantly improved (0.046, z = –1.994) compared with change in the control group (0.3, SD 3.2). Change in the Activity-related Relaxation in the exercise-education group (–0.4, SD 1.2) was also significantly improved (p = 0.017, z = –2.396) compared with change in the control group (0.2, SD 1.4). The effect size of the MFI-20 Reduced Motivation was 0.34, while the effect size of the Activity-related Relaxation was 0.45 for the intervention group compared with the control group.
Type I error. The secondary and exploratory between-group analyses comprised a total of 23 statistical analyses, and the upper level of number of false significances was 1.05, which indicates that one of the significances found might be false.
Per-protocol analysis (Table III)
Forty-seven of 81 patients (58%) randomized to the exercise-education programme and 56 (66%) of 85 patients randomized to education were defined as active participants.
Primary outcomes. Significant improvement (p = 0.013, z = –2.486) was found for change in the FIQ total in the exercise-education programme (–6.3, SD 14.4) compared with change in the control programme (–0.6, SD 12.5) at the 20-week post-test. The effect size of the FIQ total for the intervention group compared with the control group was 0.44.
Significant improvement (p = 0.013, z = –2.497) was found for change in the 6MWT in the exercise-education programme (14.5, SD 35.8) compared with change in the control programme (–6.4, SD 58.3) after 20 weeks. The effect size of the 6MWT for the intervention group compared with the control group was 0.43.
Secondary outcomes. Significant improvement (p = 0.002, z = –3.073) was found for change in the FIQ Pain (–10.0, SD 18.8) in the exercise-education programme compared with change in the control programme (3.0, SD 18.9). The effect size of the FIQ Pain for the intervention group compared with the control group was 0.69.
Change in the LTPAI Total activity (1.0, SD 3.7) was significantly increased (p = 0.026, z = –2.220) in the exercise-education group compared with change in the control group (–0.1, SD 5.06). Most part of the increase was at a moderate level, shown by significant (p = 0.048, z = –1.976) change in the LTPAI Moderate activity (1.3, SD 2.7), among the exercisers compared with change among the controls (0.2, SD 2.9). The effect size of the LTPAI total activity was 0.25, while the effect size of the LTPAI Moderate activity was 0.39 in the intervention group compared with the control group.
Exploratory outcomes. Significant improvement (p = 0.005, z = –2.789) was found for change in the MFI Reduced Motivation among the exercisers (–1.1, SD 3.1), compared with the controls (–0.7, SD 3.0), effect size being 0.13. Significant improvement (p = 0.002, z = –3.027) was also found for change in the Activity-related Physical relaxation among the exercisers (–0.6, SD 1.2), compared with the controls (0.4, SD 1.5), as well as for the Activity-related Well-being (p = 0.021, z = –2.312) in the exercise group (–0.7, SD 1.4) compared with the controls (–0.1, SD 1.4). The effect size of Activity-related relaxation was 0.72, while the effect size of Activity-related Well-being was 0.43 when the intervention group was compared with the controls.
Type I error. A total of 23 between-group analyses were conducted, and the upper level of number of false significances was 0.89, which indicates that one of the significances found might be false.
11–12-month follow-up in the intention-to-treat population (Table II)
A total of 125 patients (75%) randomized to the study completed the follow-up at the 11–12-month examination. Within the exercise-education group, significant improvement was found for change in the 6MWT (14.1, SD 57.6, p = 0.013, z = –2.472), as well as for change in the SF36 Physical Component (2.86, SD 8.6, p = 0.006, z = –2.731), the SF36 Role Physical (12.1, SD 40.7, p = 0.035, z = –2.108) and the SCI (–3.9, SD 13.2, p = 0.011, z = –2.552). The effect size of the 6MWT was 0.18. The effect size of the SF36 Physical Component was 0.35 and of the SF36 Role Physical 0.38. The effect size of the SCI was 0.17.
Within the control group, change in the FIQ Total (–4.5, SD 14.3) significantly improved (p = 0.024, z = –2.254) over time, effect size being 0.29. The change scores for the control group have been omitted from Table II.
Type I error. A total of 15 analyses were conducted, and the upper level of number of false significances was calculated to 0.78, which indicates that one of the significances found might be false.
11–12- month follow-up in the pre-protocol population (Table III)
The follow-up outcomes were analysed separately for the PP population. Significant improvements over time were found for the 6MWT (21.5, SD 48.2; p = 0.007, z = –2.707), the FIQ Pain (–9.1, SD 20.9; p = 0.019, z = –2.336); the SF36 Physical Component (3.0, SD 6.7; p = 0.002, z = –3.057); the SF36 Physical function (4.2, SD11.1; p = 0.024, z = –2.250); the SF36 Bodily Pain (8.3, SD 32.5; p = 0.014, z = –2.454); the LTPAI Moderate Activity (0.8, SD 2.7; p = 0.045, z = –2.009); and the SCI (4.5, SD 10.2; p = 0.010, z = –2.569). The effect size was 0.29 for the 6MWT; 0.54 for the FIQ Pain; 0.35 for the SF36 Physical Component; 0.43 for SF36 Bodily Pain; 0.12 for SF36 Vitality; 0.41 for the LTPAI moderate activity, and 0.18 for the SCI.
No significant improvements over time were found within the control group, and the change scores have been omitted from Table III.
Type I error. A total of 15 analyses were conducted, and the upper level of number of false significances was 0.42, which indicates that 0–1 significances found might be false.
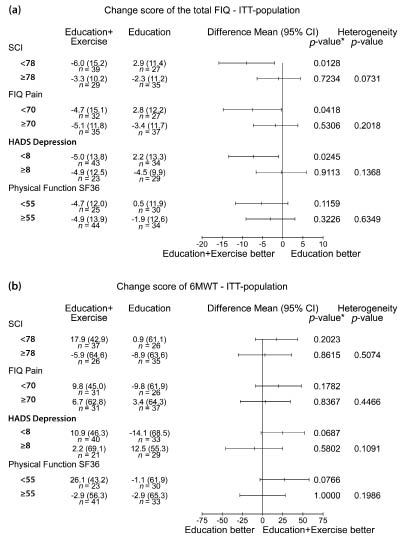
Subgroup analysis (Fig. 2)
Fig. 2. Subgroup influences on change in the primary outcomes. (a) Fibromyalgia Impact Questionnaire (FIQ) total. (b) Six-minute walk test (6MWT). The subgroups were created by dichotomized values of the stress and crisis inventory (SCI), the FIQ Pain, the Hospital Anxiety and Depression Scale (HADS), and the 36-item Short-Form Health Survey (SF36) Physical Function. Mean differences for the change score and 95% confidence intervals (CI) are presented in the graphs, followed by p-value, separately for each subgroup. p-value for heterogeneity (interaction between the randomized group and the change score of the primary outcome) is given in the right-hand column. ITT: intention to treat.*Fisher’s Non-Parametic Parmulation test.
FIQ Total. No significant heterogeneity was found for the subgroups created by level of pain, distress, stress and activity limitations, implying that these aspects did not have any significant influence on change in the FIQ total score. However, a non-significant tendency towards heterogeneity (p = 0.073) was found for the subgroup created by the SCI (< 78/≥ 78), implying that the improvement in the FIQ total tended to be influenced by stress, in favour of those with lower stress scores.
Analysis within the subgroup characterized by lower degree of the stress (< 78 on the SCI) relieved a significant (p = 0.013) improvement in the FIQ Total in the exercise-education group (–6.0, SD 15.2) compared with change in the control group (2.9, SD 11.4), effect size for the intervention group compared with the control group being 0.64. A significant improvement (p = 0.042) was also found for change in the FIQ total (–4.7, SD 15.1) in the exercise-education group characterized by lower ratings on the FIQ Pain (< 70), compared with change in the control group (2.8, SD 12.2), effect size for the intervention group compared with the control group being 0.54. Significant improvement (p = 0.025) was also found for change in the FIQ total (–5.0, SD 13.8) in the patients in the exercise-education group reporting lower level of distress (< 8 on the HADS-D), compared with change in the control group (2.2, SD 13.3), effect size for the intervention group compared with the control group being 0.53. No significant change in the FIQ total was found in the patients reporting more severe scores on the SCI (p = 0.723), the FIQ Pain (p = 0.530) or HADS-D (p = 0.911) (see Fig. 2).
6MWT. No significant heterogeneity was found for the subgroups created by the level of pain, distress, stress and activity limitations implying their influence on the change score of the 6MWT.
DISCUSSION
The present RCT showed that a 20-week supervised exercise-education programme improved health status (the FIQ total score) in patients with FM and CWP, which is in line with previous studies of exercise and education (8–13). The intervention group was compared with a control group that undertook the same 6-week education programme, including planning weekly exercise in their own environment. The effect size of the FIQ total was small (0.31) in the intervention group compared with the controls in the ITT-population, but it increased to 0.45 in the active participants in the intervention group compared with the controls (the PP-population). These results are comparable to the effect sizes found in pharmacological and non-pharmacological studies of patients with FM in primary healthcare (34).
The 6MWT, the primary outcome at the level of body function, did not significantly improve in the between-group analysis of the ITT population. In the active participants (PP-population), the 6MWT improved in the intervention group, compared with the controls, but the change was smaller than expected. A contributory reason for this poor improvement might be the fairly good baseline walking capacity in the patients (> 500 m, SD > 70 m), which possibly resulted in ceiling effects for several patients. It is probable that patients today are more physically active than in previous years, as the mean baseline walking distance in the present study appears to be higher than in our previous study (467 m) published in 2002 (12). Increased public knowledge of the benefits of exercise may have contributed to a higher activity level.
Improvement in the FIQ total in the intervention group was supported by improvement in several components related to health. The FIQ Pain showed significant improvement in the intervention group compared with the control group. Effect size of the FIQ Pain score was 0.45 in the ITT-population, increasing to 0.69 in the active participants in the exercise-education group compared with the controls. Significantly enhanced activity-related relaxation among the exercisers, being in line with previous studies (35–37), might also have contributed to the improved health status. No significant changes were found for pharmacological treatment during the study period, indicating that a reduction in pain intensity cannot be explained by pharmacology.
MFI-20 Reduced motivation significantly improved in the intervention group compared with the control group. Other fatigue dimensions showed conflicting results, as some of them improved within the control group, while others improved within the intervention group. Improvement in fatigue within the education group is supposedly related to the programme, designed to introduce strategies to cope with the symptoms.
Symptoms in the study population ranged from mild to very severe. The median value of the FIQ Pain was 70 on the 0–100 scale, which indicates severe pain. Distress was also common in the study population, as shown by the HADS scores. The median SCI score in the patient population was 78, which indicates a high level of stress, but it corresponds with the findings in a previous Swedish study of stress in FM, where the SCI score was 75 (26).
The second aim of the present study was to investigate the influence of stress, pain, distress and activity limitations on changes in the primary outcomes. No significant heterogeneity was found, but stress tended (p = 0.07) to influence change in the FIQ total. This implies that exercisers presenting with lower scores for stress might improve more in their health status as a consequence of the treatment than those with higher scores. A slight tendency towards heterogeneity (p = 0.137) was also found in the HADS-D.
Separate within-group analyses of patients presenting with lower ratings for stress, pain and distress revealed a significant improvement in the FIQ total (p < 0.05) among the exercisers, compared with the control group (effect size > 0.50).
No significant heterogeneity was found for change in the 6MWT, which may be related to the small improvement in the intervention group discussed earlier. However, the HADS-D showed a slight tendency (p = 0.109) towards heterogeneity, in favour of exercisers not perceiving distress (< 8). This result was supported by a non-significant (p = 0.069) improvement in the 6MWT (10.9, SD 46.3) among the exercisers with low HADS-D scores, compared with change among the controls (–14.1, SD 68.5). A non-significant improvement (p = 0.077) in the 6MWT (26.1, SD 43.2) was also found among the exercisers characterized by better SF36 Physical Function compared with the control group (–1.1, SD 61.9).
Subgroups based on symptom severity and physical impairments among patients with FM have been described previously (14, 38, 39). To the best of our knowledge, this is the first study to demonstrate subgroup differences in outcomes of exercise in patients with FM, suggesting that patients with milder symptoms gain the best effects from exercise.
The long-term follow-up, conducted 11–12 months after the baseline, revealed lasting, but small, improvement in the 6MWT in the exercise-education group, in both the ITT and PP populations. The FIQ Pain and the SF36 Bodily Pain revealed significant long-term improvements in the active participants, indicating that regular exercise may contribute to control of pain in FM. An alternative explanation might be the significantly shorter symptom duration (9.7, SD 7.19) in the PP-population compared with the non-active participants (11.7, SD 6.95). Also, a previous study has suggested that shorter symptom duration is associated with higher improvement in FM (34). No significant baseline differences for age, education, work status or main outcomes were found between the active and non-active participants.
The pool exercise programme provided an opportunity for individual adjustments of exercise to perceived pain and fatigue. Perceived exertion (BRPE) ranged from “very light” to “somewhat hard” (32), reflecting the content of the programme that included exercises with and without resistance. The patients exercised in the pool only once a week, which is a limitation of the exercise protocol studied. Increased frequency might have improved the effects of exercise.
Another limitation of the present study was the choice of the control group. Education is regarded as a treatment modality; therefore the control group was not totally without intervention, which would have been the ideal situation. Comparison between 2 treatment protocols may have minimized the differences indicating improvement in the intervention programme. Significant improvements within the education group were, however, few in number. One reason might be the long symptom duration of the patients, as many of them reported that they had already participated in education to help them manage their symptoms.
Several outcomes were included in the study, as we were interested in different aspects of health. The 2 primary outcomes were analysed first and the FIQ Pain was regarded as the most important secondary outcome. Due to multiple comparisons, the significance levels found should be interpreted with caution, and the upper limit of expected number of false significances is presented after each analysis.
The recruitment process began with a systematic search of patient journals with codes associated with myalgia. A total of 818 journals were found and scrutinized. Most of these did not meet the inclusion criteria for CWP. A total of 109 patients could not be assessed for eligibility, while 30 patients who fulfilled the criteria declined to participate or were excluded from the study. Thus, all together, 17% of the total number of potentially eligible patients was not included in the study; this proportion is, however, not regarded as a threat to the external validity of the study.
Twenty percent of the patients (n = 33) included in the study did not complete the post-test, despite attempts to motivate them to participate. Half of these patients (n = 17) did not start the treatment programme, mainly due to time limitations associated with changes in work schedules or family commitments or concomitant disorders. Other reasons for dropping out were dissatisfaction with the group to which they had been randomized, increase in pain and other reasons not reported. Drop-out rates of approximately 20% are not rare in exercise studies enrolling patients with FM, as highlighted in several reviews (40).
In conclusion, an exercise-education programme improved health status in FM and CWP. No significant heterogeneity was found for the subgroups created by level of pain, distress, stress and activity limitations, but patients with milder stress, pain or depression improved most by treatment, gaining moderate improvements in their health status,
ACKNOWLEDGEMENTS
The GAU Study Group: Mona Lind, Eva Melin, Anne Fredrikson, Marianne Hjerpe and Åsa Holmestrand in Primary Health Care, Alingsås;
Mattias Hjelm and Elisabeth Enhörning in Primary Health Care, Uddevalla; Ann-Kristine Neuman in Primary Health Care in Göteborg. The statistical adviser was Nils-Gunnar Pehrsson.
Financial support was provided by The Swedish Research Council, The Health and Medical Care Executive Board of Västra Götaland Region, The Swedish Rheumatism Association, The Länsförsäkringsbolagens Research Foundation, The Rheumatic Pain Society in Göteborg/RiG, The Göteborg Region Foundation for Rheumatology Research/GSFR and ALF at Sahlgrenska University Hospital.
REFERENCES