OBJECTIVE: To compare the effects of an interdisciplinary pain management programme with those of standard inpatient rehabilitation by comprehensive biopsychosocial self-assessment.
METHODS: In this naturalistic prospective controlled cohort study, 164 chronic pain patients who participated in the interdisciplinary pain programme and 143 who underwent standard rehabilitation were assessed using standardized instruments. Effect differences were compared bivariately and analysed by multivariate logistic regression to control for baseline differences in the outcome variables and confounders.
RESULTS: On entry into the clinic, the interdisciplinary pain programme patients were younger and showed significantly worse mental and psychosocial health than the standard rehabilitation patients. At discharge, the interdisciplinary pain programme patients reported greater improvement on pain (multivariate p = 0.034), social functioning (bivariate p = 0.009), and in trend in catastrophizing and ability to decrease pain. At the 6-month follow-up, the effects experienced by the standard rehabilitation group were higher on physical functioning, social functioning, anxiety, and life control (multivariate p = 0.013–0.050).
CONCLUSION: Intensive interdisciplinary rehabilitation with more behavioural therapies was accompanied by a greater improvement in patients who were severely affected by pain, compared with standard rehabilitation by the end of the stay, but not in the mid-term. Highly resource-consuming patients may benefit from subsequent, individually tailored outpatient care.
Key words: pain, assessment, interdisciplinary, rehabilitation, behavioural therapy, controlled study.
J Rehabil Med 2009; 41: 569–575
Correspondence address: Felix Angst, Schiedhaldenstrasse 1, CH-8700 Küsnacht, Switzerland. E-mail: fangst@vtxmail.ch
Submitted August 26, 2008; accepted March 10, 2009
Introduction
Chronic pain has multiple aetiologies, and results in a syndrome with common patterns (1). The high burden on somatic, psychological and psychosocial well-being, functionality and quality of life demands multi-dimensional and comprehensive management and comprehensive, but also sensitive, outcome assessment (2–6).
Interdisciplinary and intensive pain rehabilitation programmes are well established and have shown significant benefits with regard to clinical outcome and cost-effectiveness when compared with the health of waiting list patients or single treatment entities (3–5). However, to our knowledge, no published study has compared an interdisciplinary inpatient pain management programme with “regular”, standard inpatient rehabilitation as a control. After unsuccessful outpatient pain management, a decision on patient allocation has to be made. It is often difficult for primary care providers to justify their decision to allocate patients either to “ordinary”/standard inpatient rehabilitation or to a specific interdisciplinary inpatient pain management programme. For these reasons, this observational, i.e. “naturalistic” study design (concerning patient allocation to therapy) will provide results that are closer to clinical reality than those obtained by a randomized allocation design. Allocation to treatment in our study was decided by the referring physicians (primary care providers and rheumatologists) and the investigators did not intervene. The study design was, therefore, observational, “naturalistic”, and representative for daily clinical reality. In most studies, outcome focused mainly on pain intensity and physical function and less on psycho-functional and psychosocial interference with pain and pain coping (4, 5).
This study aimed to quantify the effects of a standardized interdisciplinary inpatient pain management programme and to compare them with standard inpatient rehabilitation by means of scores of standardized, well-tested, self-reported questionnaires with a special focus on pain, psychosocial, and coping aspects using an observational study design. We hypothesized that the interdisciplinary pain management programme would result in greater improvements than standard rehabilitation.
Methods
Patients
All subjects included in the study: (i) had either chronic non-specific back pain (i.e. lumbar, thoracic, cervical, or panvertebral pain syndrome), or fibromyalgia according to the definition of the American College of Rheumatology (ACR), or chronic widespread pain, i.e. generalized musculoskeletal pain syndrome that did not meet the definition criteria of fibromyalgia (7). Further inclusion criteria were: (ii) ability to complete self-assessment questionnaires, especially sufficient German language, and psycho-intellectual abilities; and (iii) written informed consent. The study’s protocol was approved by the local ethics committee (EK AG 2008/026).
Patients were consecutively referred by general practitioners, rheumatologists, psychiatrists, and hospitals (mainly departments of rheumatology), either to the interdisciplinary, inpatient pain management programme or to regular, standardized inpatient rehabilitation at the rehabilitation clinic “RehaClinic” Zurzach, Bad Zurzach, Switzerland. This allocation was left to the discretion of the health professionals and was not the result of randomization or any other mechanism. For the interdisciplinary pain management programme, each candidate was assessed by means of a standardized telephone interview regarding motivation, realistic aims, and cognitive abilities (in order to intellectually understand the contents of cognitive behavioural therapy) by the head of the programme (RB). This procedure ensured standardized and valid criteria for inclusion into the programme and patients’ potential of rehabilitation. Additionally, for each participant, special permission for the costs had to be obtained from the relevant health insurance company. The patients in the interdisciplinary, inpatient pain management programme, whose data were published in our previous report (65 patients with fibromyalgia and 60 with chronic back pain), also participated in this study (6).
Interventions
The “Zurzach Interdisciplinary Pain (German: Schmerz) Programme (ZISP)” is a comprehensive, standardized, interdisciplinary, inpatient pain management programme and consists mainly of 3 management entities, which gives rise to “the 3 column principle”: (i) medical care including adapted drug therapy; (ii) graded activity exercises; and (iii) psychotherapy, mainly cognitive and operant behavioural therapy (6). The programme is intensive (in total over 100 h of therapy). Over the course of treatment patients received on average 6 daily sessions of the following treatments: physiotherapy, aerobic endurance training, Qigong/tai chi exercises, individual psychotherapy including cognitive behavioural therapy, participation in a pain coping group, relaxation therapy, humour therapy, information and education about pathophysiology of pain mechanisms and management of chronic disabling pain, nursery care, and regular medical consultations, including drug therapy. Individual treatment strategies were identified and discussed during the interdisciplinary meetings of the pain management team (2 h per week for 6 patients). A comparison of the interdisciplinary, inpatient pain management programme (Intervention) with standard, inpatient rehabilitation (Control) in the same clinic is shown in Table I. For both the intervention and control groups, subsequent ambulatory care was organized for the time after discharge from the clinic.
| Table I. Comparison of treatment modalities between interdisciplinary (intervention) and standard (control) rehabilitation |
| Duration | Interdisciplinary programme | Standard rehabilitation |
| Inpatient stay, weeks | 4 | 3 |
| Nursing care, h/day | 24 | 24 |
| Physician: Eexamination in first week, h Examination in last week, h | 1 0.5 | 0.5 0.5 |
| Physician, visit, h/week | 0.75 | 0.75 |
| Information about pain (group), h/week | 0.75 | 0.75 |
| Physiotherapy: individual (mainly active), h/week | 2.5 | 2.0 |
| Physiotherapy: cardiovascular training group, h/week | 2 | 2 |
| Strength and endurance training (non supervised) | Optional | Optional |
| Aquatic exercise group, h/week | Optional | 2 |
| Physiotherapy: relaxation therapy, h/week | 2 | 2 |
| Occupational therapy (group), h/week | 1 | – |
| Tai chi/Qigong, h/week | 3 | 3 |
| Psychology: pain coping group, h/week | 3 | – |
| Psychology: CBT individual, h/week | Optional, max. 3 | Optional, max. 3 |
| Psychology: humour therapy (group), h/week | 1.5 | – |
| Movement analysis, Cary Rick method (group), h/week | 3 | – |
| Interdisciplinary meetings, h/week | 2 for 6 patients | 0.5 for approx. 20 patients |
| CBT: cognitive behavioural therapy. |
Measures
The Short Form 36 (SF-36) comprehensively measures physical, mental, and psychosocial health and quality of life through 36 items (questions) composing 8 scales: bodily pain, physical functioning, role physical, general health, vitality, social functioning, role emotional, mental health (8, 9). The SF-36 has been implemented in numerous studies in over 50 languages worldwide and its clinimetric quality has been proven in various settings. Normative data stratified by sex, age and comorbidity are available from a population survey (n = 6948) in Germany (10).
The West Haven-Yale Multidimensional Pain Inventory (WHYMPI, abbreviated to MPI) assesses pain and pain-specific consequences on the basis of 51 items that make up 9 scales: pain severity, interference with pain, negative mood, (social) support, life control, negative responses, solicitous responses, distracting responses, activity (11,12). The MPI has been tested in numerous studies and has been used widely for various pain conditions, especially in chronic pain.
The Coping Strategies Questionnaire (CSQ) assesses cognitive and behavioural strategies to tolerate, manage and compensate for pain and their consequences by 48 items, resulting in 8 scales plus 2 additional control items: diverting attention, reinterpreting pain, self-statements, ignoring pain, praying and hoping, catastrophizing, activity level, pain behaviours, ability to control pain, ability to decrease pain (13–15). The German CSQ has been tested and applied in several studies (e.g. 6, 15).
The Hospital Anxiety and Depression Scale (HADS) is a short self-rating of anxiety and depression (each 7 items), these being 2 of the most important affective health dimensions for people with chronic musculoskeletal pain (16, 17). It has been developed for non-psychiatric conditions, has a long history of application in psychology and medicine, and is well-tested in large populations and patient surveys. We used the sex- and age-specific norms from a German population survey (n = 2037) (18).
All instruments are self-reported, standardized, widely used, and recently tested for responsiveness in chronic pain patients (19). For reasons of special interest (pain, function, psychosocial abilities and coping) based on the corresponding constructs of the instrument scales, to avoid redundancy, and to make use of the most responsive scores, the following scales were chosen (6, 19): pain severity on the MPI to assess pain, the SF-36 physical functioning to assess physical function (in general, mainly ambulation), the SF-36 social functioning to assess the ability to participate socially, both HADS depression and anxiety scales to assess affective health specifically and comprehensively, the MPI life control to assess a salutogenic attitude, the CSQ catastrophizing and ability to decrease pain to assess 2 of the most important predictors for successful coping with pain. The main outcome was pain (MPI pain severity) and the other 7 scales were regarded as secondary outcomes.
In addition, socio-demographic data were recorded in a standardized way (20). Medical records of the physicians in charge of our clinic (reports of the inpatient rehabilitation sent to the admitting physicians) were reviewed for data on further medical history, e.g. comorbidities and medication at entry and discharge.
Analysis
Assessments were performed on entry to the clinic (baseline), at discharge (1 month follow-up), and at 6 months after baseline (at home, by post). The scores were determined following the “missing rules” of the instruments (6), i.e. 50% answered items were necessary to determine the scales of the SF-36, 6/7 answered items for those of the HADS, and 2/3 for those of the MPI and the CSQ (6, 8, 19). The score ranges were transformed into 0 = maximal pain / no function / worst coping / worst health to 100 = no pain / full function / best coping / best health for all instruments’ scores as originally described for the SF-36 to ease comparison between all scales and instruments (6, 8, 9). This means that, for example, the HADS scales were transformed from the original scaling of 0 = no depression/anxiety to 21 = maximal depression/anxiety into 0 = maximal depression/anxiety to 100 = no depression/anxiety (16, 17).
Absolute effects, i.e. score differences between follow-up and baseline, were stratified and listed for the intervention and control groups and then compared by application of the non-parametric, frequency distribution independent Wilcoxon test for bivariate comparison of effects (21). Effect sizes (ES) according to Kazis were computed to quantify the effects in a standardized way (22). The ES = [mean score at follow-up minus mean score at baseline] / [standard deviation of the scores at baseline]. Positive values reflect standardized, i.e. unit-free improvements in the number of standard deviations of the baseline scores. An ES ≥ 0.80 is considered as large, 0.50–0.79 as moderate, 0.20–0.49 as small, and 0.00–0.19 as very small (22). ES of the difference ("delta"), ES∆, are a standardized, unit-free measure for the difference of the score changes (baseline to follow-up) between the intervention and the control group and reflect the difference of 2 ES (ES intervention minus ES control) as described above (23). They are equal to the difference of the mean scores changes (baseline to follow-up) between the intervention and the control group divided by the "pooled" baseline scores standard deviation (23). Positive values reflect higher improvements in the intervention group than the control group and negative values higher effects of the control group when compared with those of the intervention group. An ES∆ is proportional to the t-value of the t-test and allows determination of the minimal necessary ES∆ to show significance between the effects of the intervention compared with the control group given the sample sizes (24).
Bivariate comparison of effects, as described above, would be valid if there were no cofactors that are of different level or differently distributed between the intervention and the control group. Covariates, for example, age, depression, use of analgetics etc., may affect the outcome of pain if different between the 2 groups at baseline. In other words, they may confound the outcome at follow-up and the ES. Multivariate regression can solve this problem.
This analysis provides a test for each outcome variable as to whether, by controlling for the effects of the covariates, the score differences (baseline to follow-up) are significant predictors of whether a subject is an intervention or a control patient. In other words, multivariate analysis tests statistically whether the effects were different between intervention and control when all confounders had equal values for the 2 groups (partial significance testing).
The non-randomized study design generally provides baseline data that are not equally or even statistically significantly different when comparing the intervention with the control group. These baseline differences were tested by χ2 test and Wilcoxon test and showed significant differences in many comparisons (see Tables II–IV). Therefore, it was interesting and necessary to test the effect differences (intervention vs control) adjusting for all potential confounders to determine whether there would have been significant differences when all confounders had equal values for the 2 groups.
| Table II. Descriptive socio-demographic and disease-related data at baseline |
| | Intervention n = 164 % | Control n = 143 % | p |
| Sex, female | 78.7 | 78.3 | 0.943 |
| Education Basic school (8–9 years) Vocational training College/high school/university | 29.3 53.0 17.7 | 24.5 55.9 19.6 | 0.890 |
| Living with partner/spouse | 78.0 | 75.5 | 0.601 |
| Smoking, yes | 38.4 | 32.9 | 0.312 |
| Sport > 2 h/week > 0–2 h/week None | 11.0 40.2 48.8 | 23.1 37.7 39.2 | 0.006 |
| No working capacity | 45.7 | 34.3 | 0.041 |
| Diagnosis Back pain Fibromyalgia Widespread pain | 49.4 32.3 18.3 | 72.7 14.7 12.6 | < 0.001 |
| Comorbidities, n None 1 2 3 or more | 9.1 26.8 34.8 29.3 | 5.6 16.1 29.4 48.9 | 0.020 |
| Paracetamol | 29.3 | 33.6 | 0.418 |
| Opioids | 28.7 | 25.9 | 0.585 |
| Opiates | 7.3 | 7.0 | 0.913 |
| NSAIDs | 39.6 | 45.5 | 0.303 |
| Tricyclics & SNRIs | 26.2 | 11.9 | 0.002 |
| SSRIs | 11.6 | 8.4 | 0.354 |
| Tranquillizers | 11.0 | 11.2 | 0.953 |
| Other drugs | 33.5 | 44.8 | 0.044 |
| Age, years, mean (SD) Min–max | 45.3 (10.6) 19.7–72.7 | 53.4 (12.4) 29.4–88.0 | < 0.001 |
| BMI (kg/m2), mean (SD) Min–max | 25.9 (5.1) 16.1–49.5 | 26.3 (4.9) 15.0–40.0 | 0.233 |
| Duration of pain, months, mean (SD) Min–max | 72.0 (42.1) 6–156 | 79.3 (76.2) 3–564 | 0.731 |
| NSAIDs; non-steroidal anti-inflammatory drugs, SNRIs: selective serotonin, noradrenaline reuptake inhibitors, SSRIs: selective serotonin reuptake inhibitors, BMI: body mass index; SD: standard deviation. |
Logistic regression was used with the group (intervention vs control) as the binary dependent variable (to predict) and all possible factors (predictors) as independent covariables that might have an effect on each of the 8 outcome scores. Such confounders were widely accepted epidemiological cofactors, or by various studies reported risk factors for outcome in chronic pain (25–28). They are listed in Table I: sex, age, diagnosis, number of comorbidities, education, living alone/with partner, working capacity (at each time-point), body mass index (BMI), sports (at each time-point), smoking, duration of the pain disease, medication (at each time-point: paracetamol, opioids, opiates, non-steroidal anti-inflammatory drugs (NSAID), analgesic antidepressants (tricyclics and selective serotonin, noradrenaline reuptake inhibitors (SNRI)), selective serotonin reuptake inhibitors (SSRI), tranquilizers, other drugs, and all baseline values of the 8 outcome variables (pain, physical function, social function, depression, anxiety, life control, catastrophizing, decreased pain).
First, all these covariates were included in the logistic model together with the raw score difference (entry to discharge) of the main outcome MPI pain severity. Not "significant" covariates with p ≥ 0.200 were then excluded backwards step by step and the new model was compared with the previous model using the change of the explained variance, which did not have to be significantly changed (data not shown in detail), as proposed by Hosmer & Lemeshow (29). The significantly differently distributed parameters in the bivariate tests at baseline (see Table I) were added to the final significant covariates. The final model contained all those variables and the score difference (entry to discharge) for each of the 8 outcome variables, i.e. one specific logistic model per outcome variable and per follow-up. The model should not contain more than (number of) covariates = number of patients/10 to be finite and result in valid data (29).
All analyses were performed using the statistical software package SPSS 16.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
Patients and baseline characteristics
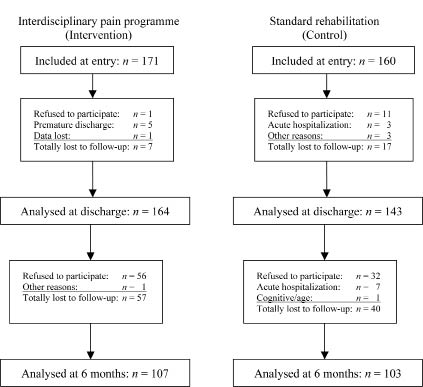
The cohort consisted of 331 chronic pain patients who were included between 2002 and 2007. The allocation procedure, assessments and the content of the interventions did not change over this time period. The flow chart of the patients and the patients’ characteristics at baseline are listed in Fig. 1 and Table II. Complete baseline socio-demographic and disease-relevant confounder and outcome data at entry and discharge were obtained for n = 164 interdisciplinary pain management programme (intervention) and n = 143 standard rehabilitation (control) patients. The drop-out rates at discharge were 4.1% for the intervention group vs 10.6% for the control group and 34.7% vs 28.0% at the 6 month follow-up (Fig. 1).
Fig. 1. Patients in the study.
Compared with the standard rehabilitation subjects at entry, the interdisciplinary pain management programme patients were significantly younger, less sporty, more frequently unable to work, more frequently affected by fibromyalgia and widespread pain (i.e. by soft tissue pain), affected by fewer comorbid conditions, and consumed more tricyclics, SNRIs and less other drugs (e.g. against hypertension, cholesterol, etc.) (Table II: p < 0.050). In addition, they experienced significantly more pain, lower physical and social function, more depression and anxiety, less life control, and more catastrophizing. This is reflected by the lower baseline scores of the intervention group in Tables III and IV – the baseline scores tested between intervention and control group, see column “1p”: p ≤ 0.001 in many comparisons.
| Table III. Comparison of interdisciplinary (intervention, n = 164) with standard (control, n = 143) rehabilitation, from entry to discharge |
| | Entry (baseline) | | | Change at discharge (follow-up) | Effect comparison |
| Intervention Mean (SD) | Control Mean (SD) | p1 | Intervention | | Control | | Bivar.3 p | Multivar.4 p | ES∆5 |
| Mean (SD) | ES2 | Mean (SD) | ES2 |
| MPI Pain severity | 23.1 (14.3) | 29.8 (15.6) | 0.000 | 10.8 (17.5) | 0.76 | 9.4 (16.1) | 0.61 | 0.750 | 0.034 | 0.09 |
| SF-36 Physical functioning | 39.0 (20.9) | 44.7 (19.9) | 0.016 | 9.0 (18.9) | 0.43 | 7.8 (13.5) | 0.39 | 0.206 | 0.361 | 0.06 |
| SF-36 Social functioning | 40.8 (24.3) | 51.8 (24.1) | 0.000 | 12.5 (26.0) | 0.52 | 4.9 (25.1) | 0.20 | 0.009 | 0.076 | 0.32 |
| HADS Depression | 54.0 (21.2) | 64.5 (18.2) | 0.000 | 8.1 (15.4) | 0.38 | 6.1 (12.8) | 0.33 | 0.313 | 0.730 | 0.10 |
| HADS Anxiety | 50.3 (21.6) | 59.8 (21.4) | 0.000 | 5.6 (16.6) | 0.26 | 5.9 (12.8) | 0.28 | 0.769 | 0.229 | –0.01 |
| MPI Life control | 48.7 (19.6) | 58.0 (17.4) | 0.000 | 10.1 (20.9) | 0.52 | 6.8 (17.9) | 0.39 | 0.225 | 0.559 | 0.18 |
| CSQ Catastrophizing | 46.1 (19.2) | 54.0 (20.2) | 0.001 | 6.1 (14.2) | 0.32 | 4.7 (13.0) | 0.23 | 0.270 | 0.169 | 0.07 |
| CSQ Decrease pain | 37.2 (20.9) | 40.3 (19.0) | 0.144 | 7.8 (22.1) | 0.38 | 5.3 (21.7) | 0.28 | 0.220 | 0.148 | 0.13 |
| p: p-values (type I error) of the significance tests: 1Comparison of baseline scores (intervention-control, Wilcoxon test), 2ES: effect size (mean change divided by the standard deviation (SD) at baseline each for intervention and control, 3Bivariate comparison of the changes (raw score differences baseline to follow-up between intervention and control) by the Wilcoxon test, 4Multivariate comparison of the changes by logistic regression including confounders (see text), 5ES∆: effect size of the differences (baseline to follow-up), equals (mean change intervention group minus mean change control group) divided by the pooled standard deviation of the baseline scores (see text). MPI: Multidimensional Pain Inventory, SF-36: Short Form 36, HADS: Hospital Anxiety and Depression Scale, CSQ: Coping Strategies Questionnaire. |
| Table IV. Comparison of interdisciplinary (intervention, n = 107) with standard (control, n = 103) rehabilitation, from entry to 6 months follow-up |
| | Entry (Baseline) | | | Change at 6 month follow-up | Effect comparison |
| Intervention Mean (SD) | Control Mean (SD) | p1 | Intervention Mean (SD) | ES2 | Control Mean (SD) | ES2 | Bivar.3 p | Multivar.4 p | ES∆5 |
| MPI Pain severity | 23.6 (14.5) | 31.2 (16.5) | 0.001 | 6.3 (20.2) | 0.44 | 6.0 (21.3) | 0.36 | 0.761 | 0.208 | 0.02 |
| SF-36 Physical functioning | 41.0 (21.4) | 43.9 (20.1) | 0.308 | 6.9 (20.5) | 0.32 | 9.6 (18.5) | 0.48 | 0.304 | 0.050 | –0.13 |
| SF-36 Social functioning | 42.9 (25.5) | 51.2 (24.2) | 0.021 | 3.1 (27.5) | 0.12 | 7.9 (30.1) | 0.33 | 0.173 | 0.016 | –0.19 |
| HADS Depression | 55.1 (21.8) | 64.8 (17.6) | 0.001 | 1.1 (17.9) | 0.05 | 1.0 (17.5) | 0.06 | 0.723 | 0.119 | 0.00 |
| HADS Anxiety | 50.7 (22.3) | 60.4 (20.7) | 0.002 | 3.6 (19.1) | 0.16 | 5.4 (17.2) | 0.26 | 0.244 | 0.013 | –0.08 |
| MPI Life control | 49.5 (20.2) | 58.4 (16.9) | 0.000 | 3.0 (22.9) | 0.15 | 3.7 (23.6) | 0.22 | 0.680 | 0.039 | –0.04 |
| CSQ Catastrophizing | 47.0 (19.8) | 53.9 (19.9) | 0.013 | 5.1 (17.4) | 0.26 | 4.7 (19.1) | 0.24 | 0.765 | 0.225 | 0.02 |
| CSQ Decrease pain | 38.2 (20.3) | 40.8 (18.0) | 0.291 | 3.6 (24.8) | 0.18 | 2.1 (22.4) | 0.12 | 0.609 | 0.481 | 0.08 |
| p: p-values (type I error) of the significance tests: 1Comparison of baseline scores (intervention-control, Wilcoxon test), 2ES: Effect size (mean change divided by the standard deviation (SD) at baseline each for intervention and control, 3Bivariate comparison of the changes (raw score differences baseline to follow-up between intervention and control) by the Wilcoxon test, 4Multivariate comparison of the changes by logistic regression including confounders (see text), 5ES∆: effect size of the differences (baseline to follow-up), equals (mean change intervention group minus mean change control group) divided by the pooled standard deviation of the baseline scores (see text). MPI: Multidimensional Pain Inventory, SF-36: Short Form 36, HADS: Hospital Anxiety and Depression Scale, CSQ: Coping Strategies Questionnaire. |
Effect comparison between baseline and discharge
At discharge (Table III), all mean raw score differences were positive, showing improvement in all 8 outcome scales. The improvements were, on average, higher for the interdisciplinary pain management programme participants (n = 164) on 7 scales (positive ES∆) except for HADS anxiety when compared with those of the standard rehabilitation subjects (n = 143). However, these differences were small, and significant (p < 0.050) only for SF-36 social functioning (12.5 vs 4.9 score points, bivariate Wilcoxon’s p = 0.009). This is in accordance with the ES∆ of 0.32 exceeding the minimal necessary value of 0.23 for significance by the t-test.
Backward stepwise logistic regression with the improvement (entry to discharge) of the main outcome MPI pain severity, revealed the following 9 "significant" (according to the rules for including variables into logistic regression: p < 0.200) co-factors: age, number of comorbidities, amount of sports, smoking, diagnosis, use of NSAIDs, SSRIs, tricyclics/ SNRIs, and other drugs. Sex and BMI were included for reasons of broadly accepted clinical importance. Together with the baseline scores of all 8 outcomes, the final model was comprised of 21 confounders combined with the score differences of one of each of the outcome variables. These multivariate logistic regression models showed greater improvements for the intervention group for all 8 outcomes at discharge (positive regression coefficients for the outcome effects, coefficient data not shown). However, significance was attained only for the main outcome, the pain severity on the MPI (p = 0.034). A trend was detected for SF-36 social functioning (p = 0.076), CSQ catastrophizing (p = 0.169), and CSQ decreased pain (p = 0.148).
Effect comparison between baseline and 6 month follow-up
At the 6 month follow-up (Table IV), the mean effects of all 8 outcome variables were again positive, showing overall improvement. The participants in the interdisciplinary rehabilitation programme (n = 107) reported slightly greater improvements in SF-36 physical functioning and SF-36 social functioning (negative ES∆). The effect differences of the other scores were close to zero (ES∆ close to zero). None of these or any other effect differences favouring the control group (n = 103) were found to be significant in the bivariate testing (necessary for significance: ES∆ > 0.28).
In contrast, logistic regression resulted in negative coefficients (data not shown in detail) for all 8 outcome effects (entry to 6 month follow-up) which means that the effects of the standard rehabilitation were higher than those of the interdisciplinary pain management programme in the multivariate comparison. These differences reached significance in SF-36 physical functioning (almost, p = 0.050), SF-36 social functioning (p = 0.016), HADS anxiety (p = 0.013), and MPI life control (p = 0.039).
DISCUSSION
We assessed 2 cohorts of chronic pain patients admitted either to our interdisciplinary, inpatient pain management programme or to standard inpatient rehabilitation at the same clinic. Bivariate and multivariate comparisons of the effects favoured the interdisciplinary intervention at discharge from the clinic, especially for the main outcome pain (MPI pain severity) and, to a lesser extent also, coping with pain. At home (6 month follow-up), these effects disappeared, which corresponds to a greater loss of improvements in the interdisciplinary pain management programme group compared with the standard rehabilitation group, especially with regard to the functional and affective outcomes.
This change over time in the relationship of the different effects between the 2 groups may be explained by faster loss of the attained improvements in the more psychosocially affected interdisciplinary pain management programme patients. On the other hand, the “healthier” (based on the 8 outcomes) standard rehabilitation participants may be better able to preserve and further develop over time their improvements achieved during the inpatient stay. This finding was irrespective of the fact that the standard rehabilitation participants were, on average, older and more severely affected by somatic disorders (i.e. were psychosocially less affected than the patients in the interdisciplinary pain management programme). The standard rehabilitation subjects reported fewer psychiatric disorders and psychosocial limitations and consumed less anti-depressive medications. We hypothesize that for chronic pain patients it is obviously more difficult to individually manage psychiatric and psychosocial dysfunctions over time (e.g. anxiety, depression, catastrophizing), as compared with predominantly somatic disorders (e.g. osteoarthritis, hypertension, diabetes). However, during their stay in the clinic, the interdisciplinary pain management programme patients showed a high potential for rehabilitation and, subsequently, may profit from more individually tailored outpatient care.
A tentative interpretation is that the partially different and overall higher numbers of treatment modalities, as well as the higher costs of the interdisciplinary pain management programme, are worthwhile to achieve successful treatment of the greater burden of mental disorders and psychosocial problems found in the interdisciplinary pain management programme patients compared with the standard rehabilitation patients. Reviews of comprehensive pain management programmes have found them to be most efficacious and cost-effective in chronic pain (3). The higher effects of the interdisciplinary pain management programme patients may stem from the more intensive therapy programme. The differences between the 2 programmes in this study were small and the interdisciplinary pain management programme mainly consisted of a one week longer stay, participation in psychological group therapies focused on cognitive and operant behavioural therapies (in total additional 7.5 h/week), and frequent interdisciplinary meetings of all therapists for less patients when compared with the standard rehabilitation programme. These positive effects may be reinforced by the fact that the pain management programme is performed with fixed patient groups so that the patients have a better chance of building new social relationships during their stay at the clinic and experience an intense peer group effect.
Consistent with our results, 7 reviewed studies showed medium short-term pain relief but no improvement in functional or behavioural outcomes when compared with behavioural treatment for chronic low back pain with waiting list controls (30). Those outcomes showed large variation, as was also observed for our data. However, mid- and long-term effects were not assessed. The positive effects on pain and function of exercise have been empirically well demonstrated (31). In fibromyalgia, multidisciplinary treatment programmes showed positive effects on pain, function, and self-efficacy when compared with single treatment or no treatment (4). An older review of multidisciplinary rehabilitation of fibromyalgia and musculoskeletal pain showed no significant effects, but cited the low quality of the studies included (32). In summary, although many studies with large therapy differences showed no effect differences and the 2 intervention programmes differed little in our study, interdisciplinary and behavioural therapies revealed higher short-term improvements, on average, than standard rehabilitation.
The observational, naturalistic study design led to heterogenic baseline characteristics of the 2 compared groups. The results of the regression model provided comparison results as if the 2 groups had the same baseline characteristics (e.g. proportion of females, age, comorbidity, baseline pain, etc.), as would be the case in a randomized controlled trial. Given the results of this study and the possible implications for external validity (i.e. whether the results can be reasonably applied to a definable group of patients in a particular clinical setting in routine practice), this “naturalistic” allocation process might be more evidence-based than allocation by randomization. This study might help ease the decisions of the referring medical doctors about whether to allocate their chronic pain patients to an inpatient interdisciplinary pain management programme or to standard inpatient rehabilitation in future.
Further strengths of the study are the large sample sizes of the intervention and the control groups, the use of well-tested, standardized assessment tools, the high proportion of complete data, and high comparability of the interventions that were used in both groups (intervention and control) by the same providers at the same clinic. Multivariate logistic regression allowed us to control for most of the known disease relevant factors and their interactions, as reported in the literature and experienced in clinical practice (25–28, 33).
As limitations of this study, the allocation to therapy was not randomized, which led to group differences in outcome relevant parameters at baseline. However, for baseline, differences between intervention and control were controlled by multivariate logistic regression analysis. A second limitation arises from the fact that all main outcome parameters were obtained from self-report questionnaires, e.g. SF-36 physical functioning screening for perceived disability, and not from examiner-rated physical function. Finally, the relatively high proportions of patients who were lost to follow-up may lead to bias. In future studies, we plan to run so-called booster sessions (by telephone) at 3 and 7 weeks after discharge from the clinic.
In conclusion, patients who are severely affected by chronic pain may benefit from interdisciplinary inpatient pain management programmes focusing on operant and cognitive behavioural therapies when compared with standard rehabilitation. They may benefit still further from subsequent, individually tailored outpatient care.
ACKNOWLEDGEMENTS
This study was supported by the Zurzach Rehabilitation Foundation SPA, Bad Zurzach, Switzerland. We are grateful to all patients for their participation in the study, and to Joy Buchanan for her English editing.
Conflict of interest: The authors declare no conflicts of interest.
REFERENCES