Andrew J. Haig, MD, Jonathan Im, Deji Adewole, MD, Virginia Nelson, MD and Brian Krabak, MD, MBA
From the International Rehabilitation Forum, Ann Arbor, MI, USA
Andrew J. Haig, MD, Jonathan Im, Deji Adewole, MD, Virginia Nelson, MD and Brian Krabak, MD, MBA
From the International Rehabilitation Forum, Ann Arbor, MI, USA
Introduction: The medical specialty of physical and rehabilitation medicine has had a proven impact on people with disabilities and on healthcare systems. Documents such as the White Book on Physical and Rehabilitation Medicine in Europe have been important in defining the scope of practice within various regions. However, in some regions the practice has not been well defined.
OBJECTIVE: To explore the practice of physical and rehabilitation medicine in Sub-Saharan Africa and Antarctica.
METHODS: Medline searches, membership data searches, fax survey of medical schools, internet searches, and interviews with experts.
RESULTS: The continents are dissimilar in terms of climate and government. However, both Antarctica and Sub-Saharan Africa have no physical and rehabilitation medicine training programs, no professional organizations, no specialty board requirements, and no practising physicians in the field. Since there are no known disabled children on Antarctica and adults are air-lifted to world-class healthcare, the consequences of this deficit are minimal there. However, the 788,000,000 permanent residents of Sub-Saharan Africa, including approximately 78 million people with disabilities, are left unserved.
CONCLUSION: Antarctica is doing fine, but Africa is in a crisis. Local medical schools, hospitals doctors, and people with disabilities, along with foreign volunteers, aid groups, and policymakers can have an impact on the crisis. However, governments, specifically national ministries of health, are ultimately responsible for the health and well-being of their citizens.
Key words: physical and rehabilitation medicine, physiatry, rehabilitation, Africa, Antarctica, healthcare policy, government policy.
J Rehabil Med 2009; 41: 401–405
Correspondence address: Andrew J. Haig, Physical Medicine and Rehabilitation, The University of Michigan, 325 E. Eisenhower, Ann Arbor, MI 48108, USA. E-mail andyhaig@umich.edu
Submitted December 5, 2008; accepted March 10, 2009
*Simultaneous publication in: European Journal of Physical and Rehabilitation Medicine, Journal of Rehabilitation Medicine, Disability and Rehabilitation, PM&R. In review: Chinese Journal of Physical Medicine and Rehabilitation.
INTRODUCTION
The World Health Organization (WHO) estimates that one in 10 people in the world have a significant disability (1). There is an extensive literature showing the effectiveness and cost-effectiveness of medical rehabilitation in returning people with disabilities to independence and to productive lives (2). Over the last half century this literature, along with the intuitive observation of those who have been exposed to rehabilitation, has led to the rapid growth of the physician specialty that drives the medical rehabilitation process, physical and rehabilitation medicine (PRM).
In Europe, the Americas, Asia and Australia, tens of thousands of physician specialists in the field of PRM practise their trade of caring for people with strokes, brain injuries, spinal cord injuries, arthritis, back pain, developmental disabilities and numerous other medical disorders in settings ranging from private offices to large comprehensive medical rehabilitation hospitals. As this valuable “field that owns no organ system” has matured, regional organizations in America, Europe, and Asia have codified the specialty and quantified the reach of the field (3–5).
Perhaps the most influential and detailed of these publications in PRM is the White Book on Physical and Rehabilitation Medicine in Europe (4, 6). The result of collaboration between 3 different continent-wide specialty organizations, the White Book was published simultaneously in 2 major journals. Its 46 pages document the problem of disability, the relevance of rehabilitation to people with disabilities and to society, and the principles of PRM. It defines the specialty as it is practised in Europe, outlines standards for clinical training and practice, and provides a framework for future research in the field. Appendices quantify the number of practitioners and trainees, as well as various aspects of practice. This document has evoked a number of commentaries and contrasts with the field as practised elsewhere (7–9).
Two continents are notably absent from this type of documentation; Sub-Saharan Africa and Antarctica. Sub-Saharan Africa is a continent of 788,000,000 people, many of whom live in poverty, and many of whom are affected by war or infectious diseases (10). Antarctica is populated by approximately 4000 wealthy scientists, most of whom go home for the winter, and a large number of penguins (11). The International Rehabilitation Forum (IRF, www.rehabforum.org) is an organization supported by a consortium of major academic PRM departments, with a goal of uniting them to develop medical rehabilitation throughout the world. Since no other organization appears to represent the specialty in these 2 regions, the IRF set out to document the specialty as practised in these regions.
METHODS
A commission was established to find the leaders of all African and Antarctic professional specialty societies in PRM. Having found none, the IRF determined to include leading physicians practising the specialty in Africa and Antarctica. Again, having found none, the IRF then sought out the most expert people they could find: a Ghanaian general practitioner who had been awarded the Globus Fellowship from the International Society for the Study of the Lumbar Spine to study spine rehabilitation in the USA, an American PRM specialist who has volunteered for many years in East Africa, another American PRM specialist who has consulted on program-building with universities and governments in West Africa, and an undergraduate student who was adept at internet searches. To represent Antarctica, the IRF included a PRM specialist who had visited the continent as medical director for an ultra-endurance running race.
The team performed a Medline literature search on the terms “physiatry” or “physical medicine” and the various continents, covering dates from 1950 to October 2008. The membership list of the International Society for Physical and Rehabilitation Medicine (ISPRM) was searched for members from African countries. A Boolean search of internet resources including Google, Google Scholar, PubMed articles, National Library of Medicine, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane, and Medline Plus for PRM, physical medicine and rehabilitation, or physiatry, and Africa (including various nations) or Antarctica was performed, and the highest ranked “hits” were traced to determine whether they contained any evidence for the practice of PRM on the continents.
No medical schools were found in Antarctica. All Sub-Saharan medical schools listed on websites for the Institute for International Medical Education and its directory (IMED) online search (www.faimer.org/resources/imed) were sought. These included schools in: Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Republic of Cape Verde, Central African Republic, Chad, Comoros, Democratic Republic of Congo, Republic of Congo, Côte d’Ivoire, Djibouti, Equatorial Guinea, Eritrea, Ethiopia, Gabon, The Republic of the Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Sao Tome and Principe, Senegal, Seychelles, Sierra Leone, Somalia, South Africa, Swaziland, Tanzania, United Republic of Togo, Uganda, Zambia, and Zimbabwe.
Websites of these schools, if available, were searched for any evidence of PRM specialists. A survey was sent via fax or e-mail to those schools for which fax or e-mail addresses were available.
The commission contacted the West African College of Physicians and the South African College of Physicians asking for information on any PRM specialists in Africa. Throughout the process the commission asked visitors to Africa, African expatriates, African medical personnel, and international leaders in the specialty about the practice of PRM in Africa.
RESULTS
The data is best summarized by Fig. 1, which illustrates the number of physiatrists (PRM physicians) per 10 million people living in Antarctica and Sub-Saharan Africa. Detailed analysis was performed for each continent separately, as noted below.
Antarctica
A Google search of the term “Antarctica physiatry” found that Brian Krabak, MD, MBA, of the University of Washington, USA, had acted as competition physician for an ultra-endurance running race in Antarctica (12). Dr Krabak was invited to join the commission. At the time of this research he knew of no other physiatrist (PRM physician) in Antarctica.
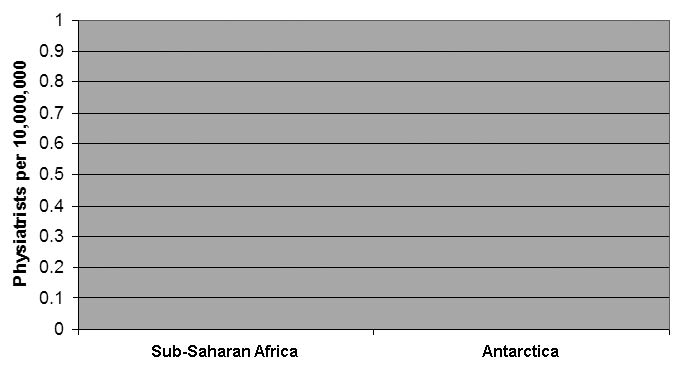
Fig. 1. Number of PRM physicians per 10 million people in Sub-Saharan Africa and Antarctica.
Sub-Saharan Africa
The search found no PRM specialty organizations or specialty journals in Sub-Saharan Africa. There are no known training programs in Sub-Saharan Africa, and requirements for the field are not specified by any Sub-Saharan African regulatory body. No medical school website was found to mention the specialty. There are no Sub-Saharan Africa members of the International Society for Physical and Rehabilitation Medicine. Only 2 surveys were returned. One respondent suggested that there was a group of physicians in South Africa who may have had formal training in the field. Contact with the South African Medical Association revealed that there were indeed 6 physicians in the country who specialized in PRM1. After extensive discussion with colleagues and numerous trips to the region, the West and East African consulting physicians were quite confident that there were no PRM specialists in those regions.
1Myburgh, Marilyn, Head Operations/Database, South African Medical Association, personal communication, 6 November 2008.
The Medline search for dates from 1950 to October 2008 found 16,132 articles on “physiatry” or “physical medicine” (Table I). For “Africa below the Sahara” there were 135,373 citations. Combining these, only 60 joint citations were found. A detailed analysis of these 60 showed that almost all were related to allied health professionals or were irrelevant. None could be traced to a practising African PRM physician. Apart from recent publications by the IRF, only 2 articles addressing the specialty in Africa were found, both of which were written more than 40 years ago by the same author (13, 14).
| Table I. Medline search for articles (n) with English titles from 1950 to 2008 that matched the terms “physical medicine” or “physiatry” and various continents | |
| America | 2858 |
| Europe | 2492 |
| Asia | 290 |
| Africa | 60 |
| Africa (pertinent)* | 2 |
| Antarctica | 0 |
| *Africa (pertinent) refers to articles that actually dealt with the medical specialty of Physical and Rehabilitation Medicine. | |
DISCUSSION
The results of this research suggest that the chance of a person with a disability in Sub-Saharan Africa meeting a physician who specializes in appropriate care is zero. The tragedy and absurdity of this finding is not communicated well through simple statistics. Therefore, a comparison with Antarctica is made in this paper and illustrated graphically in Fig. 2. While this comparison may at first appear absurd, the research findings are serious; the implications are both deadly to Africans and devastating to Sub-Saharan African economies.

Fig. 2. Top: Pygoscelis adeliae or Adélie penguins in Antarctica. Bottom: A disabled football team in Africa. Both groups have a statistically similar chance of interacting with a physical and rehabilitation medicine physician. Note that the penguins all have legs. (Penguin photograph courtesy of Katie M. Dugger, PhD, Oregon State University, USA, and the football team is photographed by the first author (AJH)).
The investigation has strengths and weaknesses. The thousands of articles relating to PRM on other continents were not searched in detail for relevance or for authorship by native PRM physicians. However, they are clearly evident of an active and vibrant field everywhere else in the world. Web searches used in this article typically turned up thousands of “hits”, most of which are completely irrelevant. Due to the volume of hits we were not able to prove exhaustively that there is no web citation on PRM in Sub-Saharan Africa. The response rate to the faxed survey was extremely low. Whether that is because faxes were misdirected, arrived at offices that had no authority, or because authorities chose not to respond, the survey results may be challenged. However, the search for individuals or organizations in Africa was fairly robust. The authors have met with African government and health leaders on a number of occasions; posed the question at numerous international specialty meetings, and sought information from leaders in the field. We conclude that, apart from the small number of specialists in South Africa, who are not members of the ISPRM, there are no PRM doctors residing in Sub-Saharan Africa.
Currently there are more than 10,280 PRM specialists in Europe, more than 7000 in the USA, and perhaps 10,000 in China. Self-evidently from these numbers, and supported by a strong scientific literature, we know that multidisciplinary, physician-led rehabilitation is both effective and cost-effective in returning people with disabilities to the community. Currently, 80% of the world’s disabled population lives in low-income countries, such as those of Sub-Saharan Africa. The WHO reports that rehabilitative services, even basic physical therapy, reach only 1–2% of people with disabilities (15). It is fruitful to explore potential reasons for this mismatch in Africa.
Some might suggest that there is no PRM because Africa is a desperate place; with people dying every day, the continent cannot afford to improve the quality of life of the living. It is a poor region, but not exclusively so; in South Africa last year 32,144 people purchased new Mercedes passenger vehicles (16). In the USA there is one PRM specialist for every 30,000 urban dwellers (3). There are enough rich and middle-income Africans to support the specialty of PRM. Despite this, when an African Mercedes is involved in a road traffic accident, no amount of money will bring a PRM physician to consult in the intensive care unit. However, the fallacy in the theory of Sub-Saharan Africa being in constant crisis is not just about the rich affording the luxury of rehabilitation. Society and the economy depend on a positive ratio of consumption to contribution. People with disabilities in this region are also consumers, but they are untreated, so they and their families contribute less to the economy than they might otherwise do. The WHO’s estimate of 10% of the population having major disabilities means this is a huge drain on the economy of the region. Rehabilitation is a good social investment even in poorer regions; and therefore countries need to invest.
Global policies to date are a failure, some would say. What policy? The WHO and many other bodies have promoted a strategy of community-based rehabilitation (CBR) (17) in which people with disabilities and their families are taught to care for themselves. At face value this may seem to be empowering and democratic, and the process is supported strongly by many disabled people’s organizations. It may have some value in social reintegration of people with disabilities; however, it has clearly failed in Africa. Why is this? The initial phase of rehabilitation is intensely medical, and the nursing acuity of modern rehabilitation hospitals is often compared to that of an intensive care unit. However, in Sub-Saharan Africa people who survive their initial injury often languish until they die, or face complex and irreversible complications ranging from contractures to pressure sores to spasticity to hopelessness. They go home to families who are not trained in their care and prognosis. In other parts of world they go to medical rehabilitation wards run by PRM physicians.
Relegating the medical part of rehabilitation to the community is akin to developing a community-based neurosurgery program. In fact it is worse than this, because in Africa people with disabilities are the least educated, most impoverished, and most ostracized members of the community. CBR is a politically expedient way to allocate the least amount of funds possible to the problem. After all, uneducated villagers do try to take control over their own lives. They are cheaper than doctors, and they do not have the depth of medical knowledge to know what they are missing. With no experts who understand the medical aspects of rehabilitation to advise or to advocate, and with the approval of the WHO, governments often give complete responsibility for rehabilitation to ministries of social welfare, education, employment or agriculture. CBR is insufficient. The WHO and other policymakers need to recognize that, in every country with reasonable rehabilitation services, the medical programs are led by physicians who dedicate their careers to this cause.
The local healthcare systems have some responsibility. With no PRM physician role models in the entire region, medical school deans, department chairs, practising physicians, and hospital administrators have no idea of what is missing. They look to orthopedic surgeons (who are typically very busy in the operating room and with little formal training in rehabilitation) and others to perform the services. They often view PRM as equivalent to physical therapy, perhaps with a nod towards orthotics and prosthetics. Yet the literature on rehabilitation is clear; disability is multifactorial. A multidisciplinary team led by a physician expert always outperforms individual therapists. In fact, patient outcomes directly relate to the quality of team interaction (18). Programs on all other continents (except Antarctica) succeed because of PRM physician coordination of teams including occupational and physical therapists, speech-language pathologists, rehabilitation nurses, rehabilitation psychologists, rehabilitation social workers, vocational rehabilitation counselors, rehabilitation engineers and others. The medical expertise, leadership, and specific skills of PRM physicians as portrayed in documents such as the European White Book are simply not understood. Local healthcare systems must build rehabilitation programs that look like the programs elsewhere in the world.
Deans of medical schools and the leadership of regional Colleges of Physicians might get the process started. The need for expert physicians is compelling. However, apart from the absence of specialty training programs in PRM, other serious questions reflect the unmet educational need across the medical education system in Sub-Saharan Africa. For example, do medical students realize that a baby with cerebral palsy might be more intelligent than them? Do general practitioners know how to manage contracture, autonomic hyper-reflexia, neurogenic bladder and decubitus ulcers with physical means? Which medical school professor can tell the government of the functional impairment and societal cost of AIDS survival? Which of their hospital quality initiatives looks beyond the date of discharge to employment, social integration and even sexual relationships? Leadership in these areas will not occur until these entities name chairs in physical and rehabilitation medicine, develop programs for trainees, and hire PRM medical directors.
African communities frequently rely on help from outside of Africa. Foreign governments typically provide exactly the aid that the African politicians request, rather than the aid that they need. So, for instance, the US Agency for International Development spends billions of dollars to support Africa, but, apart from the small Leahy War Victims Fund, has made almost no investment in rehabilitation. Major non-governmental organizations are often more focused on acute disasters than on the large-scale chronic disaster of living with a disability. Doctors Without Borders, the Red Cross/Red Crescent, and others have no PRM representation among their leadership. As a result they are largely not prepared for the medical acuity of disability management after crises. Their missions and their operational policies mean that they have less invested in the long-term goal of saving function once lives have been saved. Still, numerous small and large private aid groups know the value of rehabilitation, and strive to build sustainable rehabilitation programs in Africa. Free wheelchairs make great photo-opportunities, but this kind of equipment supply without rehabilitation will never be sufficient and is not a locally sustainable intervention. Caring and thoughtful non-governmental organizations should look at policies that grow locally-trained expert physicians and allied health professionals who will make a living carrying out rehabilitation and teach others to do the same.
During the course of this investigation we encountered dozens of PRM physicians who volunteer their time and then return home. They know that rehabilitation is longitudinal, multidisciplinary, and exceedingly culturally dependent. They would readily admit that they are no substitute for locally-trained permanently-employed specialists. They often petition their home country professional organizations for help, but without much luck. Understandably national and regional organizations exist to serve their members. However, small investments in international development can rally the membership around a cause greater than their day-to-day practice. Students are drawn to a field in which there is a great need and a great compassion. It may be easier to define the scope of practice in the home country by showing how the specialists build programs elsewhere. We would argue that non-African professional organizations in PRM have self-serving reasons to reach out to developing countries.
In the final analysis, the responsibility lies with the Africans. Governments are responsible for the well-being of their people. As much as they care and as much as they may advocate, neither the people with disabilities, nor the specialty outside of Africa, nor the agencies that provide external funding are responsible. While organizations such as the universities who have come together under the IRF can bring together the expertise, the responsibility rests squarely on the shoulders of each country’s governing bodies. Ministries of Health are charged with execution of health policy. Under the Ministries, colleges of physicians are responsible for deciding on specialty training programs. Under the Ministries, medical schools are responsible for training the physicians who will care for their country. These organizations must bear ultimate responsibility for failure or success, and the Ministries of Health must lead them responsibly.
Ministries are government, and governing bodies run on political power. Where does the political power come from? One observation about disability in Africa is that it does not spare the rich or the powerful or the intelligent members of society who can make changes happen. It is statistically likely that every parliament, every industry consortium, and every medical school in Africa has members who secretly identify themselves or a close family member as disabled. However, the stigma against people with disabilities is so strong in many African cultures that disability is often hidden from view. The situation is reminiscent of US president Roosevelt who, in the 1940s, hid his polio from a society that readily went along with the deception (19). More than half a century later in America, television advertisers find that healthy wheelchair users draw positive attention to their message. This hidden power is a critical force for change, but must be unleashed by pride, shame, or commitment to do what is right.
In summary, as Fig. 2 illustrates, the likelihood that a disabled child in Sub-Saharan Africa receives the quality of care that children all over the rest of the world receive is similar to the likelihood that an Antarctic penguin is fed a mackerel by a PRM physician. The difference, however, is important: African governments are elected by the child’s family and friends.
ACKNOWLEDGEMENTS
There are no appropriate African rehabilitation journals; therefore this paper is published simultaneously in prestigious journals that represent the best in rehabilitation as it exists in all continents except Africa. The IRF wishes to thank the editors of these journals for their courage in representing this unrepresented region of the world. The publication of this report reaffirms their commitment to the core mission of academic publication: to better human health by presenting and debating the facts.
REFERENCES
