OBJECTIVE: To evaluate the effects of hand exercise in patients with rheumatoid arthritis, and to compare the results with healthy controls.
METHODS: Forty women (20 patients with rheumatoid arthritis and 20 healthy controls) performed a hand exercise programme. The results were evaluated after 6 and 12 weeks with hand force measurements (with a finger extension force measurement device (EX-it) and finger flexion force measurement with Grippit). Hand function was evaluated with the Grip Ability Test (GAT) and with patient relevant questionnaires (Disability of the Arm, Shoulder, and Hand (DASH) and Short Form-36). Ultrasound measurements were performed on m. extensor digitorum communis for analysis of the muscle response to the exercise programme.
RESULTS: The extension and flexion force improved in both groups after 6 weeks (p < 0.01). Hand function (GAT) also improved in both groups (p < 0.01). The rheumatoid arthritis group showed improvement in the results of the DASH questionnaire (p < 0.05). The cross-sectional area of the extensor digitorum communis increased significantly in both groups measured with ultrasound.
CONCLUSION: A significant improvement in hand force and hand function in patients with rheumatoid arthritis was seen after 6 weeks of hand training; the improvement was even more pronounced after 12 weeks. Hand exercise is thus an effective intervention for rheumatoid arthritis patients, leading to better strength and function.
Key words: hand exercise therapy, rheumatoid arthritis, extension force, muscle architecture, ultrasound, hand strength, DASH, SF-36.
J Rehabil Med 2009; 41: 338–342
Correspondence address: Sofia Brorsson, Halmstad University, School of Business and Engineering, PO Box 823, SE-301 18 Halmstad, Sweden. E-mail: sofia.brorsson@hh.se
Submitted June 27, 2008; accepted November 14, 2008
INTRODUCTION
Exercise has become an important part of the rehabilitation of patients with rheumatoid arthritis (RA) during recent years, and the benefits of both aerobics and hand-strengthening exercises have been reported (1, 2).
Although there is general agreement regarding the necessity for rest during an acute flare, there is a wide variation in the activities recommended for the non-acute rheumatoid hand. This wide variation in hand exercise may be due to the few objective studies regarding the effect of hand exercise on the rheumatoid hand. Studies have shown that daily hand exercise is effective in increasing grip strength (3, 4). Despite these positive trends, other studies have presented radiographic evidence of aggravation of the disease in physically active patients and in the dominant hand (5, 6).
It is widely accepted that measurement of grip force (flexion force) provides an objective measure of hand function, and this is commonly used in the clinical setting (7). An important, but sometimes neglected, ability in good hand function is the extension capacity of the wrist and fingers. Most hand grips require opening of the hand and adjustment of finger position. In addition, the extensor muscles are important for stabilization during flexion force production, and active in developing a controlled grip force (8).
Previously, we developed a finger extension force measurement device (EX-it) and evaluated its accuracy, usability and test-retest reliability (9). We have also shown that high-resolution ultrasound technology is a valuable tool for studying muscle architecture. The results of these two methods, ultrasound and finger extension force measurements, have been shown to be suitable for studying healthy and rheumatoid muscles (10).
The objective of this study was to evaluate the effect of hand exercise in patients with RA and compare the outcome with healthy subjects. Furthermore, we wanted to determine the usefulness of finger extension force measurements and ultrasound as methods for analysing the results of exercise.
SUBJECTS AND METHODS
Subjects
Female patients with RA who visited the outpatient clinic at Spenshult Rheumatic Hospital during a period of one month were asked to participate in this study. The inclusion criteria were: disease duration of at least one year and the subjects should be able to fully extend their fingers. Twenty patients with RA, (diagnosis based on 1987 American College of Rheumatology (ACR) criteria (11)), median disease duration 16 years (range 2–40 years), median age 59 years (range 33–70 years), were included in the study. A control group was selected to match the RA group for sex and age. The control group consisted of 20 healthy women, with a median age of 59 years (range 36–73 years). The exclusion criteria for the controls were: inflammatory or muscle disease, or previous hand or arm injuries. Four subjects, 2 controls and 2 patients with RA, withdrew from the study for reasons unrelated to the study; 36 subjects thus completed the study. The study was approved by the ethics committee at Lund University. All procedures complied with the Declaration of Helsinki.
Study design
The study period was 18 weeks, during which the subjects were examined at 6-week intervals. Before the exercise started, 2 examinations (occasions I and II) baseline values were determined, which are presented in the text as Week 0. Data collected on occasion III are presented as 6-week data and on occasion IV as 12-week data.
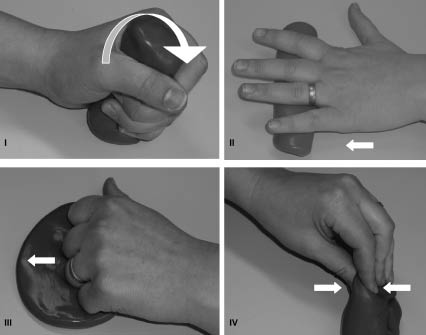
The exercise programme started after occasion II and was performed for 12 weeks. The exercise programme was designed according to Flat (12), and performed 5 times a week, each task was repeated 10 times and the position of maximal effort was held for 3–5 sec with a 20-sec rest between repetitions (Fig. 1). The exercise sessions were separated by at least one day. The exercise programme took 10 min to complete and the participants used therapeutic putty (85 g) for finger resistance. The participants were free to choose soft, medium or firm putty. The participants kept diaries during this training period in which all hand exercise occasions were declared.
Fig. 1. Arrows illustrate the directions of movement. (I) The hand was squeezing the putty. (II) The putty was moved between the wrist proper and the finger tips. (III) The wrist proper was placed in the putty, and then the fingers were stretched (movement in the metacarpophalangeal joint) in the putty. (IV) The thumb and index finger (middle-, ring- and little finger) shaped the putty. The fingertips were bent during the motion.
Evaluation methods
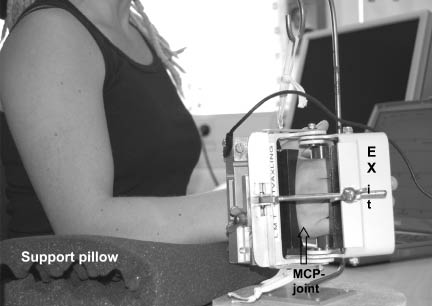
Force measurements. Two devices were used to measure muscle force, the EX-it, for measuring finger extension force (9), and the Grippit (Detektor AB, Göteborg, Sweden) for measuring finger flexion force (13). The procedure for the measurements was standardized in terms of sitting position, instructions and encouragement (7, 14). The subjects were seated in an upright position on a chair in front of the instrument (Fig. 2) (9). Before and after the measurements, the subjects were asked to report the level of pain on a visual analogue scale (VAS), ranging from 0 to 10 (0 = no pain, 10 = highest pain tolerance limit) (15).
Fig. 2. Subjects were seated in an upright position, the forearm resting on a pillow and the hand was placed in the extension measurement device. The position of the metacarpophalangeal (MCP) joint during the measurements is illustrated by an arrow.
Grip ability test. Hand function was evaluated with the grip ability test (GAT), which measures the degree of limitation of activities of daily living (ADL) and is designed for patients with RA (16).
Questionnaires. Two patient-reported questionnaires were used in their Swedish version, the Disabilities of Arm, Shoulder and Hand (DASH) questionnaire (extremity specific) and the SF-36, Short-Form health survey containing 36 questions (generic) (17, 18).
Ultrasound measurements. Ultrasound examination of the extensor digitorum communis (EDC) muscle was performed with a Siemens Acuson, Aspen system (Wrightwood Medical, Inc., Chicago, IL, USA) using a 7.5 MHz linear transducer (38 mm width). The measurements were performed according to a previously published protocol (10) and produced data on muscle cross-sectional area (CSA), muscle thickness, pennation angle and contraction pattern (change in shape of the muscle and time from start to maximal contraction (MCT)). Ultrasound recordings were obtained during a change from a neutral relaxed position to maximal static contraction of the extensor muscles, maintaining a neutrally positioned wrist.
Statistics
In the statistical analysis, SPSS version 11.5 for Windows XP was used. For comparisons between groups, the Mann-Whitney U test was used, and for comparisons within groups, the Wilcoxon test was used. Descriptive data included either median or quartiles or means (and standard deviation (SD)) values. A p-value of less than 0.05 (2-tailed test) was considered to be significant. The mean value of the baseline measurement was used in the analyses.
RESULTS
Force measurements and hand function
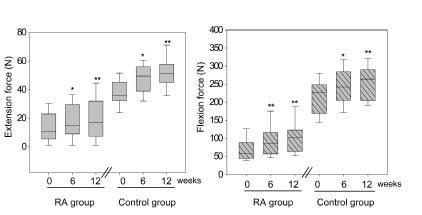
Both extension force and flexion force increased significantly in both groups after 6 weeks of hand exercise. Hand force increased further after 12 weeks of hand exercise (Fig. 3). Both the RA group and the control group showed significant improvement of the GAT score after hand exercise. The exercise programme caused no significant change in the pain level (Table I). The information in the diary supported that all participants performed the exercise programme at a regular basis in their homes.
| Table I. Hand function evaluations before and after hand exercise in patients with rheumatoid arthritis (RA) and controls. Median values of hand function tests before (week 0) and after 6 and 12 weeks of hand exercise. Median and range are given for the grip ability test (GAT), Disability, of Arm Shoulder and Hand questionnaire (DASH) and reported pain level (visual analogue scale, VAS) |
| | Week | RA group | Control group |
| Median | Range | Median | Range |
| GAT | 0 | 19.8 | 16.5–51.6 | 13.4 | 8.9–16.9 |
| | 6 | 16.8 | 14.4–40.0** | 11.5 | 6.9–15.8** |
| | 12 | 16.1 | 12.1–30.2** | 10.3 | 7.7–14.5** |
| DASH | 0 | 37.3 | 8.8–62.5 | 2.5 | 0.0–16.3 |
| | 6 | 37.5 | 5.8–75.0 | 2.1 | 0.0–17.5 |
| | 12 | 39.2 | 6.7–47.5* | 5.0 | 0.0–15.0 |
| VAS | 0 | 1.5 | 0.0–6.0 | 0.0 | 0.0–2.0 |
| | 6 | 2.5 | 0.0–7.0 | 0.0 | 0.0–2.0 |
| | 12 | 2.0 | 0.0–7.0 | 0.0 | 0.0–2.0 |
| *p < 0.05, **p < 0.01. |
Fig. 3. Finger extension force (left) and flexion force (right) in the 2 groups of participants after 6 and 12 weeks of hand exercise. *p < 0.05 **p < 0.01
Patient-reported questionnaires
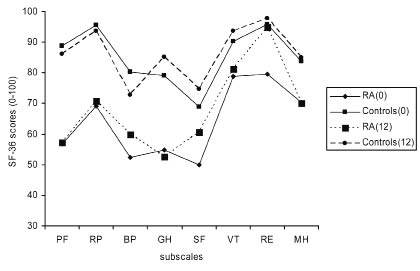
After 12 weeks of hand exercise the RA group showed a significant improvement in the DASH score, while there was no improvement in the control group (Table I). Neither of the 2 groups showed any significant improvement in the SF-36 score (Fig. 4).
Fig. 4. Results of the Short form-36 (SF-36) questionnaire, before (0) and after 12 weeks (12), of hand exercises. The scale is 0–100, from worst to best. The questionnaire is designed to measure the generic health in the general population, but also for different patient groups. SF-36 are divided into 8 health profiles scales; physical function (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). All dimensions are independent of each other.
Ultrasound measurements
After 6 weeks of hand exercise therapy, the CSA of the EDC muscle in the RA group increased, while no improvement was observed in the control group. However, after 12 weeks of hand exercise the CSA increased significantly in both groups. The pennation angles did not increase after hand exercise therapy. No improvement was seen in muscle thickness in the RA group. However, the muscle thickness in the control group increased significantly after 6 weeks. After 12 weeks of hand exercise the MCT and the muscle shape increased significantly in both groups (Table II). The CSA of the EDC muscle showed a significant difference between the 2 groups before the period of hand exercise (p < 0.05), but after 6 weeks no significant difference was observed between the groups (p = 0.4).
| Table II. Muscle architecture evaluated with ultrasound before and after hand exercise in patients with rheumatoid arthritis (RA) and controls. Values of architecture parameters are given before training (0 weeks) and after 6 and 12 weeks of training. The median and range for extensor digitorum communis muscle cross-sectional area (CSA), pennation angle, muscle thickness, time from start to maximal contraction (MCT) and shape change |
| Muscle parameter | Week | RA group | Control group |
| Median | Range | Median | Range |
| CSA, cm2 | 0 | 1.7 | 0.9–2.5 | 1.8 | 1.4–2.6 |
| | 6 | 1.9 | 1.0–2.5** | 2.0 | 1.4–2.4 |
| | 12 | 1.9 | 0.9–2.5** | 2.1 | 1.8–2.4** |
| Pennation angle,° | 0 | 5.8 | 3.8–6.5 | 5.4 | 4.0–8.5 |
| | 6 | 5.6 | 3.5–7.5 | 7.0 | 4.0–9.0 |
| | 12 | 5.5 | 3.5–8.0 | 6.3 | 4.0–9.0 |
| Thickness, cm | 0 | 0.8 | 0.5–1.2 | 1.0 | 0.7–1.2 |
| | 6 | 0.9 | 0.5–1.1 | 1.1 | 0.8–1.3* |
| | 12 | 0.9 | 0.6–1.1 | 1.1 | 0.8–1.3** |
| MCT, sec | 0 | 1.6 | 1.2–2.3 | 1.2 | 0.7–1.7 |
| | 6 | 1.6 | 1.1–2.0 | 1.0 | 0.6–1.5** |
| | 12 | 1.4 | 1.0–2.3* | 1.1 | 0.6–1.5* |
| Shape change | 0 | 0.3 | 0.3–0.5 | 0.4 | 0.3–0.5 |
| | 6 | 0.4 | 0.3–0.5* | 0.5 | 0.4–0.6** |
| | 12 | 0.4 | 0.3–0.6** | 0.5 | 0.3–0.6* |
| *p < 0.05, **p < 0.01. |
DISCUSSION
The study demonstrates the usefulness of short-term hand exercise for patients with RA and that a home exercise programme can enhance hand function. The RA group and the control group showed significantly improved hand force (both flexion and extension force) and hand function after only 6 weeks of hand exercise. The finger extension force improved by 36% in the RA group and by 25% in the control group. The flexion force was improved by 40% in the RA group and by 14% in the control group. Previous studies on flexion force support our results on the hand force of RA patients (19, 20). Although hand force improved in the RA group, there is still a significant difference in muscle force between patients with RA and healthy controls (p < 0.01). Hand function improved in both groups (p < 0.01), which is in agreement with Dellhag et al. (21) who reported improved hand function after 4 weeks of hand exercise.
After 12 weeks of hand exercise, hand force further increased in both groups. The extension force in the RA group increased by 52% and the flexion force by 56%, compared with the baseline values, while in the control group, the extension force improved by 35% and the flexion force by 19%. The reason why the RA group responded so positively could be that the RA patients had been reluctant to use their hands because of fear of pain and/or fatigue, but once they started the training programme they experienced encouraging results.
Ultrasound measurements showed a significant difference between muscle CSA in the 2 groups before the exercise period, but after 6 weeks no significant difference was observed between the groups. One explanation of the greater response in the RA group could be that the intensity of the training programme and the resistance of the therapeutic putty were adequate for this group. Stenström & Minor (19) reported in their study that the load for strength exercises for RA patients should be 50–80% of a maximal voluntary contraction, and should be performed 2–3 times per week. Our study showed significant improvements in both groups concerning change in muscle shape, and the MCT increased significantly in the control group. In previous studies it has been suggested that an early increase in force is accompanied by an increase in muscle contractility; this could be one explanation for the results in this study concerning MCT and change in muscle shape (22). After 12 weeks of hand exercise muscle parameters such as CSA and muscle shape change improved further in the RA group and after the exercise period there was no significant difference between the 2 groups concerning these 2 muscle parameters. One explanation for this could be muscle hypertrophy and adaptive changes in the neuromuscular system (23). The MCT in the RA group increased significantly after 12 weeks, while it increased after only 6 weeks in the control group. This could be explained by the fact that muscles in patients with RA are weaker at baseline and the muscle function is reduced, which can present itself as loss of functional balance and co-ordination (24).
Hand function improved significantly in the RA group after 12 weeks of exercises, as measured with the DASH questionnaire. These results indicate that impaired hand force influences hand function to a significant degree.
Methodological issues and limitations
The finger extension force measuring device, EX-it, has previously been found to be reliable in healthy individuals through test-retest procedures (9). However, the reliability of this device has not been evaluated in the rheumatoid hand. Test-retest measurements have been carried out on patients with RA with the Grippit device, showing a coefficent variation (CV) of 27% (25). However, the significant improvement of 36–40% in hand force after 12 weeks of exercise can be regarded as reliable. The use of ultrasound to assess in vivo muscle architecture has previously been shown to be reliable both in healthy subjects and patients with RA (9, 10). Reliable measures imply that standard methodologies were used, including measurement sites for the ultrasound transducer and a standardized procedure with the metacarpophalangeal joint in a fixed position during the extension force measurements. Finger extension control is one of the most difficult motions to regain after disease/injury and is also very important for prehensile activities (26). Since both EX-it and ultrasund in the present study has proved to be sensitive for evaluating hand exercise, it can be expected that these methods can be used to evaluate other interventions, such as surgical procedures, physiotherapy and/or pharmacological treatment. With these new methods, arthroplastic interventions in the metacarpophalangeal joints of the fingers can be evaluated objectively. In a longer perspective it may be possible to establish a more efficient rehabilitation programmes for patients with RA.
In order to generalize the results of the present study, a larger group of RA patients should be investigated. However, the size of the study groups is comparable to those in previous studies involving hand exercise in patients with RA (27). The effects of medication and other concomitant treatment on the study results are unknown. Detailed information about the hand deformities in the RA patients was not measured, but all patients in the study were able to extend their fingers. The range of disease duration in the RA group was wide (2–40 years) and may also have influenced the results. Häkkinen et al. (23) reported that the loss of muscle strength and functional capacity in patients with RA may be prevented by performing physical exercise with sufficient intensity on a regular basis.
Previous studies on RA patients have identified the index finger, middle finger and the metacarpophalangeal joints as the most important contributors to functional ADL tasks (28). With the new EX-it device, it is possible objectively to evaluate the single finger extension force before and after hand exercise. Furthermore, this study supports the clinical usefulness of hand exercise in patients with RA to improve hand force and function. It is possible that RA patients need continuous exercise to prevent loss of muscle force and to improve the performance of activities of daily living (27, 29).
We found no negative effects of the exercise programme on reported pain level in the RA group. Stenström et al. (29) reported that home exercises involving the whole body decreased the perceived pain level during the exercise period. Our results suggest that the benefits of exercise outweigh its possible drawbacks.
In conclusion, this study shows that regular hand exercise increases the hand function and hand force in patients with RA. None of the subjects experienced more pain in their hands during the exercise period. Hand exercise deserves consideration for routine inclusion in the treatment of patients with RA.
ACKNOWLEDGEMENTS
We would like to thank the patients at Spenshults Hospital and the healthy subjects who participated in the study. This study was supported by The Crafoordska Foundation, Camp Scandinavia AB, Siemens AB and Halmstad University.
REFERENCES
1. Masiero S, Boniolo A, Wassermann L, Machiedo H, Volante D, Punzi L. Effects of an educational-behavioral joint protection program on people with moderate to severe rheumatoid arthritis: a randomized controlled trial. Clin Rheumatol 2007; 26: 2043–2050.
2. Stenström CH. Therapeutic exercise in rheumatoid arthritis. Arthritis Care Res 1994; 7: 190–197.
3. Brighton SW, Lubbe JE, van der Merwe CA. The effect of a long-term exercise programme on the rheumatoid hand. Br J Rheumatol 1993; 32: 392–395.
4. Hoenig H, Groff G, Pratt K, Goldberg E, Franck W. A randomized controlled trial of home exercise on the rheumatoid hand. J Rheumatol 1993; 20: 785–789.
5. Glick EN. Influence of mechanical factors on the rheumatoid wrist. Proc R Soc Med 1966; 59: 555–558.
6. Castillo BA, el Sallab RA, Scott JT. Physical activity, cystic erosions, and osteoporosis in rheumatoid arthritis. Ann Rheum Dis 1965; 24: 522–527.
7. Innes E. Handgrip strength testing: a review of the literature. Austral Occup Ther J 1999; 46: 120–140.
8. Richards LG, Olson B, Palmiter-Thomas P. How forearm position affects grip strength. Am J Occup Ther 1996; 50: 133–138.
9. Brorsson S, Nilsdotter A, Sollerman C, Hilliges M. A new force measurement device for evaluating finger extension function in the healthy and rheumatoid arthritic hand. Technol Health Care 2008; 16: 283–292.
10. Brorsson S, Nilsdotter A, Hilliges M, Sollerman C, Aurell Y. Ultrasound evaluation in combination with finger extension force measurements of the forearm musculus extensor digitorum communis in healthy subjects. BMC Med Imaging 2008; 8: 6.
11. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988; 31: 315–324.
12. Flatt AE. Letter: shoulder-hand syndrome. Lancet 1974; 1: 1107–1108.
13. Nordenskiöld UM, Grimby G. Grip force in patients with rheumatoid arthritis and fibromyalgia and in healthy subjects. A study with the Grippit instrument. Scand J Rheumatol 1993; 22: 14–19.
14. Fess E. Grip strength. American Society of Hand Therapists Clinical Assessment Recommendations 1992; 2: 41–45.
15. Berntson L, Svensson E. Pain assessment in children with juvenile chronic arthritis: a matter of scaling and rater. Acta Paediatr 2001; 90: 1131–1136.
16. Dellhag B, Bjelle A. A Grip Ability Test for use in rheumatology practice. J Rheumatol 1995; 22: 1559–1565.
17. Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand 2000; 71: 613–618.
18. Sullivan M, Karlsson J, Ware JE Jr. The Swedish SF-36 Health Survey – I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995; 41: 1349–1358.
19. Stenström CH, Minor MA. Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Rheum 2003; 49: 428–434.
20. Buljina AI, Taljanovic MS, Avdic DM, Hunter TB. Physical and exercise therapy for treatment of the rheumatoid hand. Arthritis Rheum 2001; 45: 392–397.
21. Dellhag B, Wollersjo I, Bjelle A. Effect of active hand exercise and wax bath treatment in rheumatoid arthritis patients. Arthritis Care Res 1992; 5: 87–92.
22. Blazevich AJ, Gill ND, Deans N, Zhou S. Lack of human muscle architectural adaptation after short-term strength training. Muscle Nerve 2007; 35: 78–86.
23. Häkkinen A, Mälkiä E, Häkkinen K, Jäppinen I, Laitinen L, Hannonen P. Effects of detraining subsequent to strength training on neuromuscular function in patients with inflammatory arthritis. Br J Rheumatol 1997; 36: 1075–1081.
24. Ekdahl C, Andersson SI. Standing balance in rheumatoid arthritis. A comparative study with healthy subjects. Scand J Rheumatol 1989; 18: 33–42.
25. Hammer A, Lindmark B. Test-retest intra-rater reliability of grip force in patients with stroke. J Rehabil Med 2003; 35: 189–194.
26. Cauraugh J, Light K, Kim S, Thigpen M, Behrman A. Chronic motor dysfunction after stroke: recovering wrist and finger extension by electromyography-triggered neuromuscular stimulation. Stroke 2000; 31: 1360–1364.
27. O’Brien AV, Jones P, Mullis R, Mulherin D, Dziedzic K. Conservative hand therapy treatments in rheumatoid arthritis – a randomized controlled trial. Rheumatology (Oxford) 2006; 45: 577–583.
28. Goossens PH, Heemskerk B, van Tongeren J, Zwinderman AH, Vlieland TP, Huizinga TW. Reliability and sensitivity to change of various measures of hand function in relation to treatment of synovitis of the metacarpophalangeal joint in rheumatoid arthritis. Rheumatology (Oxford) 2000; 39: 909–913.
29. Stenström CH. Home exercise in rheumatoid arthritis functional class II: goal setting versus pain attention. J Rheumatol 1994; 21: 627–634.