OBJECTIVE: To evaluate the effectiveness of a night-time hand positioning splint in patients with rheumatoid arthritis.
DESIGN: Randomized controlled trial.
METHODS: Fifty patients with rheumatoid arthritis were divided randomly into 2 groups. The study group used a night-time splint starting at baseline, while the control group used the splint only during evaluations. All patients attended evaluations wearing their splints, so that the assessor remained blinded to patient allocation. The splints used in the control group were stored in a cabinet between assessments. Participants were evaluated at baseline, 45 and 90 days, using the visual analogue scale for pain; the Jamar dynamometer for grip strength; a pinch gauge for pinch strength; a Health Assessment Questionnaire for function; the Disability of the Arm, Shoulder and Hand (DASH) questionnaire for upper limb disability and symptoms; and a Likert scale for patient satisfaction with treatment.
RESULTS: The groups were homogenous for all parameters at baseline. Pain, Health Assessment Questionnaire score, DASH score, grip strength and pinch strength were significantly different between groups over time and satisfaction with the splint was reported as “better” and “much better” by most participants.
CONCLUSION: The use of a night-time hand positioning splint reduces pain, improves grip and pinch strength, upper limb function and functional status in patients with rheumatoid arthritis.
Key words: night-time splint, hand, rheumatoid arthritis, pain, function.
J Rehabil Med 2008; 40: 749–754
Correspondence address: Jamil Natour, Rheumatology Division, Rua Botucatu, 740, São Paulo, SP, 04023-900 Brazil. E-mail: jnatour@unifesp.br
Submitted January 23, 2008; accepted May 5, 2008
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, multisystemic disease of unknown aetiology, whose main characteristic is persistent inflammatory synovitis that affects the peripheral joints in a symmetric and additive manner (1, 2). The main signs and symptoms observed during the active phase of the disease are joint pain, oedema and morning stiffness (3, 4). Involvement of the wrist and fingers is observed in approximately 75% of cases, and these individuals usually feel the effects of the disease in the hands and upper limbs, with a marked impact on functional skills (5–7).
Splints are external devices applied to a body segment, whose aim is to offer support to joints, providing the best alignment possible (8, 9). Night-time splints maintain the hand in a resting position, promoting joint protection in patients with RA. These splints are frequently manufactured by occupational therapists and some authors recommend the use of a night-time splint to promote local rest, suggesting that this rest reduces inflammation and pain (10, 11). However, studies regarding the use of these splints, specifically in RA, are scarce (12, 13). A recent systematic review concluded that there are few quality publications regarding the use of splints in RA and that the evidence is insufficient to draw conclusions regarding the effectiveness of these devices in reducing pain or increasing functional capacity in patients with RA (14).
We found no studies in the literature confirming the effectiveness of these splints in patients with RA. In the present study, we evaluate the effectiveness of a night-time positioning hand splint in patients with RA in terms of pain, grip and pinch strength, upper limb function and patient satisfaction.
Methods
Subjects
Fifty patients diagnosed with RA were recruited sequentially from the outpatient clinics of the Rheumatology Division at the Federal University of São Paulo, SP, Brazil. Patients of both genders, ranging in age from 18 to 65 years, with RA classified according to the American College of Rheumatology (ACR) criteria (15) presenting the following characteristics were included in the study: use of the same remissive drugs (disease modification antirheumatic drugs) for at least 6 months prior to intervention and the same doses of corticosteroids and non-steroidal anti-inflammatory drugs for at least one month prior to the study; a score ≥ 3 and ≤ 7 on a visual analogue scale (VAS) for pain in the more affected hand. We excluded patients who presented deformities in the more affected hand that did not permit the fabrication of the splint; those using any other type of upper limb splint; those with surgery scheduled within 6 months following the study; those allergic to the splint material; and those who lived in inaccessible areas with difficult access to transportation. The study was approved by the ethics committee of the Federal University of São Paulo. Patients who fulfilled the criteria were randomized into 2 groups of 25 subjects each. Randomization was performed using opaque envelopes with concealed allocation.
Sample size
A minimum of 22 patients per group was necessary in order to achieve improvements in VAS pain of 3.0, with an alpha of 0.05 and a beta of 0.20. However, 25 patients were randomized as a previous compensation for a possible 20% loss during follow-up.
Outcome measures
The patients underwent 3 assessments: at baseline (T0), 45 days (T45) and 90 days (T90). All evaluations were performed by the same physiotherapist, who was trained in the tests used in the study and who was blind to patient allocation. In all assessments, patients were first seen by the occupational therapist responsible for the study, which examined splints on the patients in the study group (SG) and placed splints on the patients in the control group (CG). All patients were sent to the assessor with their splints to perform the evaluations. The splints used in the CG were stored in a cabinet between assessments. Patients were instructed not to comment on splint use to the assessor.
The primary outcome was:
• Pain: hand pain, as rated on a VAS ranging from 0 to 10 cm (16).
Secondary outcome measures included:
• Functional status: Health Assessment Questionnaire (HAQ), the final scores range from 0 to 3 and higher scores indicate more difficulty in performing activities of daily living. The HAQ was administered in interview form (17);
• Upper limb disability and symptoms: Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire, the final scores range from 0 to 100 and higher scores indicate more disabilities. Three modules of DASH scores were used: the optional modules for sports (Q1–4 questions), music or work (Q2–4 questions) and Disability/symptom score (Q3–30 questions). The DASH modules were administered in interview form (18–20);
• Pinch strength: both hands was evaluated with the patient seated and relaxed, with the elbow at 90º of flexion and a neutral position of the wrist (between prone and supine) using a Pinch gauge (A853-4, Smith & Nephew, Germantown, Tennessee, USA) (21). The 3 common types of pinch (tip, key and palmar) were evaluated and the mean of 3 measurements in kilogram force (kgf) was used for analysis. The assessor gave verbal instructions to the patient in order to stimulate and improve strength at every measurement.
• Grip strength: both hands was evaluated with patient seated and relaxed, with the elbow at 90º of flexion and a neutral position of the wrist (between prone and supine) using a Jamar dynamometer (PC 5030J1, Preston, Trenton, Ontario, Canada) (21). The Jamar handle was placed in the Number 2 position, according to the manufacturer's instructions. The mean of 3 measurements in kgf was used for analysis. The assessor gave verbal instructions to the patient in order to stimulate and improve strength at every measurement.
• Patient satisfaction in the study group was assessed using a Likert scale that consisted of 5 answers (much worse, worse, same, better and much better). For statistical analysis, values ranging from 0 (much worse) to 4 (much better) were used.
Intervention
For the participants in the 2 groups, a 3.2-mm thick night-time positioning splint was individually manufactured with thermoplast (Ezeform®, Smith & Nephew) and fixed with Velcro® (Velcro Industries BV, Montevideo, Uruguay); the self-adhesive hook (rougher strap) and loop (soft strap) parts had 2 different widths (2.5 and 5.0 cm). The night-time positioning splint was manufactured for the more affected hand by an occupational therapist specialized in rheumatology. The splints were designed to place the hand in a functional position, providing approximately 10° of wrist dorsiflexion, 25–30° of metacarpophalangeal joint flexion, 30° of proximal interphalangeal joint flexion and thumb abduction. The Velcro straps were positioned as follows: a wide strap at the height of the mid-forearm, another of the same width on the patient’s wrist and 2 narrower straps at the level of the metacarpophalangeal and proximal interphalangeal joints, with the self-adhesives placed on the palmar side of the splint for fixation.
Patients in the SG took the splint home after the first assessment and were instructed to use the appliance while sleeping. The patients received a table for recording the hours of daily use between assessments. The patients were also instructed regarding the correct position, placement, removal and cleaning of the splint. For the CG, splints were stored in a cabinet between assessments; patients in this group only took the splint home after the last assessment.
Statistical analysis
An intent-to-treat analysis was performed using the last-observation-carried-forward method. A level of significance of p < 0.05 was accepted for the trial. Pearson’s, χ2, Fisher’s Mann-Whitney U-test exact tests were used to determine homogeneity between groups. For normally distributed data, the dependent variables were analysed using a repeated-measures analysis of variance (ANOVA). The independent variables in all analyses were group (SG vs CG; inter-subject factors) and time (baseline, 45 days, and 90 days; intra-subject factors). When interaction time × group was significant, an ANOVA for repeated measures was used to detect intra-group changes and either the Mann-Whitney U or independent sample t-tests were used in the inter-group comparison of the changes in scores at midline and treatment completion. All tests were performed using SPSS version 10.0.1 (SPSS, Chicago, IL, USA).
Results
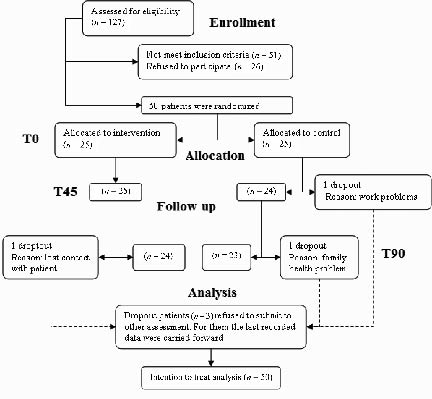
A total of 127 patients were screened, of whom 50 were included in the study after initial assessment. One participant in the SG and 2 in the CG dropped out during the intervention, leaving 49 participants at midline and 47 participants at the final assessment (Fig. 1). Patients who left treatment refused to undergo other evaluations; for these patients, any missing data were replaced with the last known value, even if this was the baseline value. Both groups were homogenous at baseline for all variables. Table I displays the population characteristics regarding age, duration of disease, gender, race, education level, profession, hand dominance, more affected hand, pain, HAQ, DASH, grip strength and pinch strength at baseline.
Fig. 1. Diagram showing the flow of participants through each stage of the trial. T0: baseline; T45: 45 days; T90: 90 days.
| Table I. Population characteristics at baseline |
| | Study group (n = 25) | Control group (n = 25) | p |
| Age, years (mean (SD)) | 51.16 (11.4) | 50.72 (10.51) | 0.992 |
| Duration of disease, years (mean (SD)) | 10.12 (7.39) | 9.02 (6.8) | 0.587 |
| Gender, female/male, n | 20/5 | 21/4 | 0.713 |
| Race, white/non-white, n | 8/17 | 11/14 | 0.382 |
| Educational level, n | | | |
| Incomplete high school | 4 | 1 | 0.057 |
| Incomplete primary school | 7 | 17 | |
| Complete primary school | 4 | 2 | |
| Incomplete secondary school | 4 | 0 | |
| Complete secondary school | 5 | 4 | |
| Illiterate | 1 | 1 | |
| Profession, n | | | |
| Home | 6 | 6 | 0.794 |
| Retired | 2 | 2 | |
| Student | 0 | 1 | |
| Others | 17 | 16 | |
| Hand dominance, right/left, n | 21/4 | 23/2 | 0.384 |
| More aching hand, right/left, n | 15/10 | 13/12 | 0.569 |
| Hand pain, VAS in cm (mean (SD)) | 6.33 (1.01) | 5.86 (1.40) | 0.196 |
| HAQ score (mean (SD)) | 1.48 (0.68) | 1.42 (0.50) | 0.747 |
| DASH Q2 (mean (SD)) | 39.77 (27.24) | 52.81 (18.52) | 0.111 |
| DASH Q3 (mean (SD)) | 39.41 (20.67) | 44.40 (15.61) | 0.340 |
| Key pinch strength, kgf (mean (SD)) | 3.10 (1.35) | 3.87 (1.48) | 0.481 |
| Grip strength, kgf (mean (SD)) | 8.9 (4.17) | 10 (6.56) | 0.061 |
| Palmar pinch strength, kgf (mean (SD)) | 2.30 (1.26) | 2.49 (1.04) | 0.573 |
| Tip pinch strength, kgf (mean (SD)) | 1.88 (1.14) | 2.11 (0.95) | 0.450 |
| SD: standard deviation; VAS: visual analogue scale; HAQ: Health Assessment Questionnaire; DASH: Disabilities of the Arm, Shoulder and Hand questionnaire; Q2: music and work score; Q3: disability/symptom score; kgf: kilogram force. |
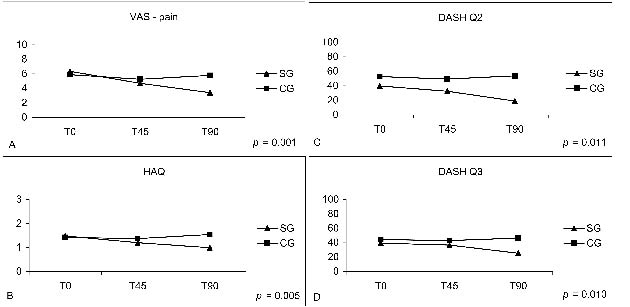
A decrease in pain in the more affected hand was observed in the SG, while pain in the CG remained constant, and a significant difference between groups over time was detected (p < 0.001). The comparison between groups at each time of evaluation revealed this difference at T90 (p = 0.001) (Fig. 2A, Table II). HAQ scores also decreased in the SG while remaining constant in the CG, showing a significant difference between groups over time (p < 0.005). The comparison between groups at each time of evaluation revealed this difference at T90 (p < 0.001) (Fig. 2B, Table II).
Fig. 2. Between-groups analysis over time for: (A) pain (VAS: visual analogue scale); (B) Health Assessment Questionnaire (HAQ); (C) Disabilities of the Arm, shoulder and Hand (DASH), work and music scores (Q2); and (D) disability/symptom score (Q3). SG: study group; CG: control group.
| Table II. Between-groups analysis of hand pain (VAS), HAQ score, DASH score, grip strength and pinch strength |
| | T0 | T45 | T90 | |
| SG | CG | SG | CG | SG | CG | p1 |
| Hand pain, VAS in cm (mean (SD)) | 6.33 (1.01) | 5.86 (1.40) | 4.7 (2.34) | 5.24 (5.16) | 3.4 (2.08) | 5.79 (2.14) | <0.001* |
| p2 | 0.196 | 0.425 | < 0.001* | |
| HAQ score (mean (SD)) | 1.48 (0.68) | 1.42 (0.50) | 1.20 (0.63) | 1.37 (0.38) | 0.99 (0.54) | 1.54 (0.43) | <0.005* |
| p2 | 0.747 | 0.250 | <0.001* | |
| DASH Q2 score (mean (SD)) | 39.77 (27.24) | 52.81 (18.52) | 32.38 (20.65) | 49.31 (22.05) | 19.03 (15.84) | 53.75 (18.73) | 0.011* |
| p2 | 0.111 | 0.015* | < 0.001 | |
| DASH Q3 score (mean (SD)) | 39.41 (20.67) | 44.40 (15.61) | 36.79 (19.42) | 42.90 (13.72) | 25.42 (17.73) | 46.49 (14.91) | 0.010* |
| p2 | 0.340 | 0.206 | <0.001* | |
| Grip strength, kgf (mean (SD)) | 8.9 (4.17) | 10 (6.56) | 10.74 (4.57) | 10.77 (4.99) | 12.04 (6.36) | 9.55 (5.41) | 0.04* |
| p2 | 0.481 | 0.982 | 0.144 | |
| Key pinch strength, kgf (mean (SD)) | 3.10 (1.35) | 3.87 (1.48) | 3.68 (1.38) | 3.69 (1.27) | 3.95 (1.79) | 3.71 (1.54) | 0.034* |
| p2 | 0.061 | 0.972 | 0.613 | |
| Palmar pinch strength, kgf (mean (SD)) | 2.30 (1.26) | 2.49 (1.04) | 2.82 (1.26) | 2.35 (0.88) | 3.17 (1.55) | 2.29 (1.04) | 0.002* |
| p2 | 0.573 | 0.133 | 0.023* | |
| Tip pinch strength, kgf (mean (SD)) | 1.88 (1.14) | 2.11 (0.95) | 2.15 (1.11) | 2.02 (0.93) | 2.77 (1.50) | 2.11 (0.97) | 0.004* |
| p2 | 0.450 | 0.669 | 0.072 | |
| Patient satisfaction, n (%) | | | | | | | |
| Much worse | | | 1 (4) | | 0 (0) | | 0.0179* |
| Worse | | | 2 (8) | | 1 (4) | | |
| Same | | | 4 (16) | | 2 (8) | | |
| Better | | | 13 (52) | | 11 (44) | | |
| Much better | | | 5 (20) | | 11 (44) | | |
| *Significant p-value. SD: standard deviation; SG: study group; CG: control group; T0: baseline; T45: after 45 days from baseline; T90: after 90 days from baseline; VAS: visual analogue scale; HAQ: Health Assessment Questionnaire; DASH: Disabilities of the Arm, Shoulder and Hand questionnaire; Q2: music and work score; Q3: disability/symptom score; kgf: kilogram force; p1: p-value between groups over time; p2: p-value between groups at each time. |
Only 2 DASH modules (DASH Q2 and DASH Q3, referring to work and general upper limb symptoms, respectively) were analysed in the present study. Questions regarding sports activities and playing musical instruments were excluded, as only one of the 50 patients practiced regular physical activity (swimming) and played the guitar. Regarding DASH Q2, the groups behaved differently over time, with a decrease in scores in the SG and constant scores in the CG and a significant difference was detected (p = 0.011). The comparison between groups at each time of evaluation revealed this difference at T45 and T90 (p = 0.015 and p < 0.001) (Fig. 2C, Table II). For DASH Q3, the groups behaved differently over time, the 2 groups remained unchanged until T45, after which the SG scores improved, while the CG scores remained constant and a significant difference between groups over time was detected (p < 0.010). The comparison between groups at each time of evaluation revealed this difference at T90 (p < 0.001) (Fig. 2D, Table II).
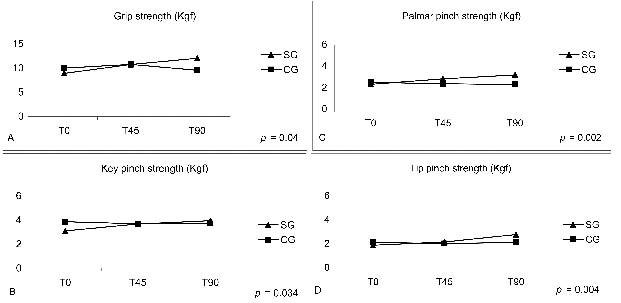
A significant difference between groups was observed for grip strength over the 3 months (p = 0.04). The SG increased in strength, while the CG decreased in strength. However, no statistically significant differences were found between groups at T0 (p = 0.481), T45 (p = 0.982) or T90 (p = 0.144). The intra-group comparison revealed the SG performed differently over time (p = 0.019), with differences between T0/T45 (p = 0.023) and T0/T90 (p = 0.009). The CG demonstrated no statistical differences over the 3 months of study (p = 0.365) (Fig. 3A, Table II).
Fig. 3. Between-groups analysis over time for: (A) grip strength; (B) key pinch strength; (C) palmar pinch strength; and (D) tip pinch strength. kgf: kilogram force.
There were significant differences in key pinch, palmar pinch and tip pinch strength over time (p = 0.034, p = 0.002 and p = 0.004, respectively) (Table II). There was no statistical difference between groups regarding key pinch at each evaluation; in the intra-group analysis, however, the SG demonstrated improved strength, which was statistically significant between T0/T45 (p = 0.020) and T0/T90 (p = 0.031), whereas the CG demonstrated no difference over time (p = 0.738) (Fig. 3B). In the palmar pinch analysis, there was a difference between groups at T90 (p = 0.023); in the intra-group analysis, the SG demonstrated improved strength, which was statistically significant between T0/T45 (p = 0.009) and T0/T90 (p = 0.009), whereas the CG demonstrated no difference over time (p = 0.558) (Fig. 3C). In the tip pinch analysis, there were no statistical differences at each evaluation (p = 0.450, p = 0.669 and p = 0.072, respectively); in the intra-group analysis, however, the SG demonstrated improved strength, which was statistically significant between T0/T45 (p = 0.035), T0/T90 (p = 0.002) and T45/T90 (p = 0.004), whereas the CG demonstrated no differences over time (p = 0.850) (Fig. 3D).
The analysis of satisfaction with treatment in the SG revealed a statistically significant difference over time (p = 0.0179), with differences between T0/T90 (p = 0.0124) and T45/T90 (p < 0.001). No significant difference was observed between T0/T45 (p = 0.677) (Table II). Mean time of splint use per night was 8 h (standard deviation 1.57; range 4.5–11 h) and showed no correlation with the other variables analysed.
Discussion
Maini & Zvaifler (22) reported a peak incidence of RA between 40 and 60 years of age, similar to the mean age of the patients in the present study, which were 51.16 years in the SG and 50.72 years in the CG. The gender (female/male) ratio of patients with RA was 4.5:1, a ratio slightly higher than those reported by Maini & Zvaifler (22) and Albani & Carson (23) (3:1 and 2:3, respectively). This ratio may be explained by the greater time availability of women for participation in the study, as most female patients were housewives or worked as daily cleaning women, thereby facilitating their presence at the evaluations. Moreover, data in the literature demonstrate that the frequency of seeking medical and rehabilitation services is higher among women.
Pain is the main factor responsible for disability and impaired manual ability in patients with RA. Together with physical deformities, pain leads to dependence regarding the activities of daily living. The participants reported difficulties in performing manual activities and attributed this fact to the pain in their hands, more specifically, in the wrist as well as distal and proximal interphalangeal joints. We believe the decrease in pain observed in the SG was due to a reduction in the inflammatory process, which allowed the patient to use his or her strength properly, consequently permitting a more satisfactory execution of daily activities. Similar findings were reported in a study by Nicholas et al. (10), in which patients had their hands immobilized by a splint and reduction in pain and inflammation was related to the time of splint use.
The functional capacity of the participants, as evaluated by the HAQ, also improved in the SG. O’Connor et al. (24) demonstrated the importance of the HAQ associated with pain scores and related these values to the functional capacity of individuals. Although the HAQ is the gold standard for the assessment of function in RA patients, the instrument is insufficient for the specific assessment of upper limb function. Therefore, the DASH was also used in the present study. According to Dubert et al. (25), the DASH is an objective instrument that provides specific scores for the comparison of different types of treatment. Regarding the DASH Q2, which evaluates work-related characteristics, significant improvement was observed in the SG at T45 and lasted until the end of the study, whereas no improvement was observed in the CG. Significant improvement was also observed regarding the DASH Q3 in the SG at T45 and T90, whereas CG tended to present poorer scores throughout the study, although this worsening did not reach statistical significance.
In the present study, the reduction in pain observed over the 3 months of intervention and monitored by the HAQ and DASH probably led to the improvement in upper limb function and symptoms, thus improving the performance of the participants in different daily activities. Since the positioning splint maintains the hand in a neutral resting position only at night, it does not impair the execution of daytime activities.
The improvement in the HAQ score was unexpected because this is a health-related questionnaire. We attempted to minimize bias by controlling other interventions, changes in medications and randomizing the patients immediately after the baseline assessment. We believe that the splint may account for the improved HAQ score, as hand function has a significant impact on a patient’s life. Therefore, improvements in hand pain enabled the patients to perform activities of daily life better.
A significant difference between groups was also observed in terms of hand grip strength, as measured by Jamar dynamometer. Key pinch, palmar pinch and tip pinch, measured with a pinch gauge, also differed significantly between groups. A number of uncontrolled studies on static wrist splints have shown a gain in grip strength (26–28) as observed in the present study. In contrast, dynamic hinged splints have been reported to reduce grip strength (29).
The patients in the 2 groups did not undergo any other type of upper limb therapy during the 3 months of intervention other than the use of the splints, suggesting that the maintenance of grip and pinch strength in the study group was due to a reduction in pain and the inflammatory process. This finding indicates that night-time positioning splints do not impair grip or pinch strength, but rather improve them by decreasing pain and the inflammatory process.
Patient satisfaction with the use of the splint in the SG was evaluated using a Likert scale at T45 and T90. Most patients reported feeling either better or much better with the use of the appliance. It is important to note that the night-time positioning splint was moulded to the individual patient’s hand, respecting its shape and range of motion, and that the material can be readjusted after fabrication if any pressure points cause discomfort.
One limitation of our study was the use of a control group with no intervention. However, our initial idea was to study whether the splint is better than no intervention. Further studies are necessary to compare the night-time splint with different forms of intervention. To minimize bias, the patients were randomized immediately following the baseline assessment; control subjects maintained their medication and did not undergo any physical intervention. Moreover, our study followed the patients for only 3 months. It is also very important to study the long-term benefits of the splint.
Nearly all patients in SG used the splint throughout the study. However, one patient admitted at the end of the 3 months that he had not used the splint correctly during the study period because he thought it would affect hand strength. A similar reluctance was reported by Pagnotta et al. (30), who found that the participants feared a reduction in strength, but used the appliance because pain relief was believed to be more important. This shows how important it is to offer clear information or education, which may improve patient adherence to the intervention.
In conclusion, this present study demonstrated that the use of a night-time hand positioning splint by patients with RA decreases hand pain and improves grip and pinch strength, upper limb function and functional status, as well as promoting patient satisfaction.
References
1. Skare TS, editor. Reumatologia: princípios e práticas [Rheumatology: Principles and practice]. Rio de Janeiro: Guanabara Koogan; 1999, p. 91–104 (in Spanish).
2. Hochberg MC, Chang RW, Dwosh I. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum 1992; 35: 498–502.
3. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid. Arthritis Rheum 1988; 31: 315–324.
4. Dieppe, P. Osteoarthritis – clinical features. In: Klippel JH, Stone JH, Crofford LJ, White P, editor. Primer on the rheumatic diseases. 13th edn. Atlanta: Arthritis Foundation; 2008, p. 224–228.
5. Vliet Vlieland TP, van der Wijk TP, Jolie IM, Zwinderman AH, Hazes JM. Determinants of hand function in patients with rheumatoid arthritis. J Rheum 1996; 23: 835–840.
6. Gordon DA, Hastings DE. Clinical features of early, progressive and late disease. In: Klippel JH, Dieppe PA. Rheumatology. 2nd edn. London: Mosby; 1998, p. 5.3.1–5.3.14.
7. Duruöz MT, Poiraudeau S, Fermanian J, Menkes CJ, Amor B, Dougados M, et al. Development and validation of a rheumatoid hand functional disability scale that assesses functional handicap. J Rheum 1996; 23: 1167–1172.
8. Katz PP. The impact of rheumatoid arthritis in life activities. Art Care Res 1995; 8: 272–278.
9. Melvin JL. Roles and functions of occupational therapy in hand rehabilitation. Am J Occup Ther 1985; 39: 795–798.
10. Nicholas JJ, Gruen H, Weiner G, Crawshaw C, Taylor F. Splinting in rheumatoid arthritis: factors affecting patient compliance. Arch Phys Med Rehabil 1982; 63: 92–94.
11. Trombly CA, editor. Terapia Ocupacional para a disfunção física [Occupational therapy in a patient with physical dysfunction]. 2nd edn. Sao Paulo: Livraria Santos; 1989, p. 265–287 (in Spanish).
12. Zoeckler AA, Nicholas JJ. Prenyl hand splint for rheumatoid arthritis. Phys Ther 1969: 49: 377–379.
13. Swigart CR, Eaton RG, Glickel SZ, Johnson C. Splinting in the treatment of arthritis of the first carpometacarpal joint. J Hand Surg 1999; 24: 86–91.
14. Egan M, Brosseau L, Farmer M, Quimet M, Rees S, Tugwell P, Wells G. Splints and orthosis for treating rheumatoid arthritis (Cochrane Review). Cochrane Database Syst Rev 2003; (1): CD004018.
15. Hochberg MC, Chang RW, Dwosh L. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Art Rheum 1992; 35: 498–502.
16. Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheum 1990; 17: 1022–1024.
17. Ferraz MB, Oliveira LM, Araujo PM, Atra E, Tugwell P. Cross-cultural reliability of physical ability dimension of the health assessment questionnaire. J Rheum 1990; 17: 813–817.
18. Case-Smith J. Outcomes in hand rehabilitation using occupational therapy services. Am J Occup Ther 2003; 57: 499–506.
19. Navsarikar A, Gladman DD, Husted JA, Cook RJ. Validity assessment of the disabilities of the arm shoulder and hand questionnaire (DASH) for patients with psoriatic arthritis. J Rheum 1999; 26: 2191–2194.
20. Orfale AG, Araújo PMP, Ferraz MB, Natour J. Translation into brazilian portuguese, cultural adaptation and evaluation of the reliability of the Disabilities of the arm, shoulder and hand questionnaire. Braz J Med Biol Res 2005; 38: 293–302.
21. Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg 1984; 9A: 222–226.
22. Maini RN, Zvaifler NJ. Rheumatoid arthritis. In: Dieppe PA, Klippel J, editor. Rheumatology. 2nd edn. London: Mosby; 1998, p. 2.1–2.6.
23. Albani S, Carson DA. Etiology and pathogenesis of rheumatoid arthritis. In: Koopman WJ, editor. Arthritis and allied conditions: textbook of Rheumatology. 13th edn. United states: Lippincott Williams & Wilkins; 1997, p. 979–992.
24. O’Connor D, Kortman B, Smith A, Ahern M, Smith M, Krishnan J. Correlation between objective and subjective measures of hand function in patients with rheumatoid arthritis. J Hand Ther 1999; 12: 323–329.
25. Dubert T, Voche P, Dumontier C, Dinh A. Le questionnaire DASH: adaptation française dun outil d’evaluation internationale. Chirurgie de la Main 2001; 20: 294–302.
26. Backman CL, Deitz JC. Static wrist splint: its effect on hand function in three women with rheumatoid arthritis. Art Care Res 1988; 1: 151–159.
27. Kjeken I, Moller G, Kvien TK. Use of commercially produced elastic wrist orthoses in chronic arthritis: a controlled study. Art Care Res 1995; 8: 108–113.
28. Nordenskiold U. Elastic wrist orthoses: reduction of pain and increase in grip force for women with rheumatoid arthritis. Art Care Res 1990; 3: 158–162.
29. Burtner PA, Anderson JB, Marcum ML, Poole JL, Qualls C, Picchiarini MS. A comparison of static and dynamic wrist splints using electromyography in individuals with rheumatoid arthritis. J Hand Ther 2003; 16: 320–325.
30. Pagnotta A, Baron M, Bitensky NK. The effect of a static wrist orthosis on hand function in individuals with rheumatoid arthritis. J Rheum 1992; 25: 879–885.