OBJECTIVE: To assess sports participation in young adults with myelomeningocele and its association with personal, disease-related and psychosocial factors, physical activity and fitness.
DESIGN: Cross-sectional study.
SUBJECTS: Fifty-one persons (26 males) with myelomeningocele, mean age 21.1 (standard deviation 4.5) years.
METHODS: We assessed self-reported sports participation, ambulatory status, presence of hydrocephalus, functional independence, social support, perceived competence, exercise enjoyment, objective and self-reported physical activity, peak oxygen uptake, muscle strength and body fat. Associations were studied using regression analyses.
RESULTS: Thirty-five subjects (69%) participated in sports. Sports participation was not associated with disease-related characteristics, but was associated with social support from family, perceived athletic competence and physical appearance (p ≤ 0.05), and tended to be associated with global self-worth (p = 0.10). Sports participants had higher self-reported physical activity levels than non-participants (p ≤ 0.05); objective results did not support this. Furthermore, sports participants tended to be less likely to have subnormal muscle strength (odds ratio = 0.26; p = 0.08) and their peak oxygen uptake was 0.19 l/min higher, but not statistically significantly (p = 0.13).
CONCLUSION: Sports participation seems to be due to personal preferences rather than physical ability; it could benefit from improving social support and perceived competence, and is associated with higher self-reported physical activity.
Key words: spina bifida, sports participation, exercise behaviour, physical activity, physical fitness.
J Rehabil Med 2008; 40: 702–708
Correspondence address: Laurien Buffart, Rehabilitation Medicine, University Medical Centre Rotterdam, ‘s Gravendijkwal 230, NL-3015 CE, Rotterdam, The Netherlands. E-mail: l.buffart@erasmusmc.nl
Submitted February 1, 2008; accepted May 5, 2008
INTRODUCTION
In people with a disability, there is a shift from disability prevention to prevention of secondary conditions (1). This is emphasized in the report Healthy People 2010, which contains a separate chapter on improving health of persons with disabilities that includes specific goals and objectives for increasing physical activity and fitness (2). In the disabled population, optimizing physical activity may be even more important than in the general population, as disabilities commonly cause a cycle of deconditioning, in which physical functioning deteriorates, leading to further reduction in physical activity levels (3). Furthermore, regular physical activity, sports participation and active recreation are important for disease prevention and the maintenance of functional independence, aerobic capacity, participation, social integration, and life satisfaction (4).
Several barriers for engaging in sport activities have been recognized in people with a variety of disabilities, i.e. lack of transportation and accessible facilities, lack of equipment suited to their needs, lack of knowledge of where to obtain a programme, inability to perform physical activities, lack of time, money and social support, as well as poor self-efficacy and motivation (5–7). With the increased emphasis on healthy lifestyles, there is a strong need to understand physical activity of various subgroups of the disabled population. Furthermore, in the context of physical activity promotion, insight into modifiable determinants is warranted, since these can be targeted in interventions.
Myelomeningocele (MMC) is a common neural tube defect with an incidence of 1:1000 live births. MMC is often associated with paralysis and loss of sensation in the lower limbs, incontinence and hydrocephalus (8). Many persons with MMC now survive into adulthood, which raises the importance of a healthy lifestyle in this population. Previous research showed that adolescents and young adults with MMC have an inactive lifestyle compared with their able-bodied peers (9, 10). These studies have investigated daily physical activity by assessing total energy expenditure or total duration of dynamic activities (e.g. walking, cycling, wheelchair-driving, general non-cyclic movement); however, they did not specifically describe sports participation. Sports and exercise can be seen as a subcategory of physical activity, which is planned, structured and repetitive (11). Sports-related physical activities can easily be provided through rehabilitation services and could increase physical activity behaviour in persons with MMC. Furthermore, participating in sports may be important to improve their fitness, which was low in many (12).
Due to the lack of knowledge about sports participation in people with MMC, the present study aimed to investigate sports participation and its association with disease-related, personal and social factors in adolescents and young adults with MMC. Furthermore, this study focused on how sports participation might influence total physical activity behaviour and fitness.
METHODS
Study sample
Adolescents and young adults with MMC, aged between 16 and 30 years, were recruited from 4 university hospitals in the western part of the Netherlands (Rotterdam, Leiden, Utrecht and Amsterdam) and all rehabilitation centres in the southwest of the Netherlands. Exclusion criteria were: complete dependence on an electric wheelchair, presence of disorders other than MMC that affect daily physical activity (e.g. rheumatoid arthritis), and presence of disorders that contra-indicate a maximal exercise test (e.g. exercise-induced ischaemia or arrhythmias, uncontrolled hypertension and exercise limitation due to chronic obstructive pulmonary disease). We invited 171 persons, of whom 51 participated in the study (30%). The main reasons for non-participation were: no interest, lack of time, or duration of the measurements. We found no differences between participants and non-participants regarding age, gender, level of lesion and presence of hydrocephalus as assessed by independent t-test or χ2 test (10). All participants, and parents of adolescents aged less than 18 years, gave written informed consent before participating in the study. The medical ethics committee of the Erasmus MC Rotterdam and of all other participating institutes approved the study.
In total, 26 males and 25 females participated in the study. Information about the neurological level of lesions was obtained from the medical records; they were registered as sacral (n = 7), lumbosacral (n = 21), lumbar (n = 15), thoracolumbar (n = 7) and thoracic (n = 1).
Sports participation
The main outcome measure was self-reported current sports participation (yes/no). We also registered reasons for sports participation or non-participation, and among sports participants we assessed the kind of sport and average self-reported number of hours spent on each sport per week (13). Each sport was allocated to an intensity category using the physical activity compendium (14) using 4 intensity categories according to metabolic equivalents (METs: 1 MET = 4.184 kJ/kg body weight/h): < 3 METs, 3–6 METs, 6–9 METs and 9–12 METs. Activities in these categories were given intensity scores of 1.5, 4.5, 7.5 and 10.5 METs, respectively (13). From these intensity scores and from the average amount of time per week spent on each sport, we calculated a total sport score expressed in kJ/kg body weight/day for each sports participant.
Correlates of sports participation
Personal factors:
• Educational level: this was categorized as low (pre-vocational practical education or lower level, n = 17) or high (secondary theoretical educational and higher education, n = 34).
Disease-related factors:
• Ambulatory status: defined according to the classification of Hoffer (15). Participants were categorized as ambulatory (community ambulators, n = 15, or household ambulators, n = 8) or non-ambulatory (non- (functional) ambulators, n = 28).
• Hydrocephalus: the presence of hydrocephalus was obtained from medical records. Hydrocephalus was considered to be present when a shunt was placed (82%). For 2 participants, hydrocephalus was mentioned in the medical records at some time, but no shunt was placed. This was assumed to be only minor hydrocephalus and these participants were categorized as not having hydrocephalus (8).
• Functional independence: this assessed in a semi-structured interview based on the functional independence measure FIMTM and functional assessment measure (FAM) (16). In total, 30 items were assessed addressing 18 FIMTM items on functioning in basic physical and cognitive abilities and 12 FAM items on cognitive and psychosocial functioning. The items are divided into 7 subscales, i.e. self-care, sphincter control, transfers, locomotion, communication, psychosocial adjustment and cognitive functioning. Each item is scored on a 7-level scale from 1 (total dependence) to 7 (total independence). Total motor score is the sum of a person’s scores on the first 4 subscales and total cognitive score includes the last 3 subscales. We used these respective scores as indicator of motor and cognitive functioning. The FIMTM + FAM has shown to have high internal consistency, Cronbach’s alpha = 0.99, and good reliability (17, 18).
Psychosocial factors:
• Social support: the Dutch version of the scales for measuring Social Support for Diet and Exercise Behaviors by Sallis and co-workers (19) was used to measure social support from family and friends. The Dutch scale consists of 3 subscales: (i) the exercising together subscale from the Friend Support for Exercise Habits Scale (5 items), (ii) the participation and involvement subscale (10 items), and (iii) the rewards and punishment subscale (3 items). The latter 2 subscales are both from the Family Support for Exercise Habits scale (20). Items were rated on a 5-point scale (1 = “never” to 5 = “very often”) and possible sum scores ranged from 18 to 90. Respective Cronbach’s alpha values for the subscales were 0.69, 0.71 and 0.26, indicating sufficient internal consistency for the first 2 scales, but low internal consistency for the latter, which is most likely due to the small number of items (20).
• Perceived competence: the Dutch version of Harter’s Social Perception Profile for Adolescents scale (SPPA) was used to assess perceived competences and global self-worth (21, 22). The Dutch SPPA is a 35-item instrument covering 7 subscales (5 items per subscale), i.e. scholastic competence, social acceptance, athletic competence, physical appearance, behavioural conduct, close friendship and global self-worth. Since the subscales job competence and romantic appeal of the original SPPA were not applicable for Dutch adolescents, these were not included in the Dutch version (22). Items are scored on a 4-point scale, with a higher score corresponding to a more positive perception of a specific competence. Scale scores were calculated by summing the items (maximum score 20). The Dutch SPPA has shown good internal consistency, test-retest reliability and construct validity in able-bodied young adults (22).
• Enjoyment: enjoyment in exercise was measured with the Groningen Enjoyment Questionnaire (GEQ) (23). This consists of 10 statements with which subjects were asked to rate their agreement on a 7-point scale (1 = “absolutely disagree” to 7 = “absolutely agree”). Possible sum scores ranged from 10 to 70. Cronbach’s alpha for this scale was 0.88, indicating sufficient internal consistency (23).
Physical activity:
• Objective dynamic activity: the duration of dynamic activities (composite measure of the separately detected activities walking, including walking stairs and running, cycling, general movement and wheelchair-driving) was measured objectively during 2 randomly selected weekdays using an accelerometry-based activity monitor (AM, Temec Instruments, Kerkrade, The Netherlands). Participants were fitted with the AM at their homes and instructed to perform their usual daily activities, but not to swim, or take a shower or bath during activity monitoring. To avoid measurement bias, the principles of the AM were explained to the participants after the measurements. All participants agreed with this procedure. Detailed methods are described elsewhere (10). Since no differences existed between the first and the second measurement day, we used average results, expressed in min/day, for further analyses. The AM has shown to be a valid and reliable instrument to quantify mobility-related activities, including wheelchair driving (24, 25).
• Self-reported physical activity. Self-reported physical activity was assessed by interview using the Physical Activity Scale for Individuals with Physical Disabilities (PASIPD) to obtain insight into the composition of total physical activity behaviour (26). The Dutch version of the PASIPD is a 12-item, 7 day recall questionnaire, which consists of questions on leisure time, household and work-related physical activities (Cronbach’s alpha = 0.60), from which a total physical activity score in kJ/kg body weight/day was calculated. We also presented duration of total physical activity and of separate types of activities presented in min/day. A previous study reported acceptable test-retest reliability and criterion validity, which was comparable to other questionnaires (27).
Physical fitness:
• Aerobic capacity: this was measured during a progressive maximal exercise test, based on the McMaster All-Out Progressive Continuous Cycling and Arm test (28). Depending on whether the main mode of ambulation was walking or wheelchair driving, participants performed the test on an electronically braked cycle ergometer (Jaeger ER800) or an arm ergometer (Jaeger ER800SH; Jaeger Toennies, Breda, The Netherlands), respectively. Detailed descriptions of the test can be found elsewhere (12). We defined aerobic capacity as the mean oxygen uptake during the last 30 sec of exercise (peak VO2, in l/min).
• Body fat: thickness of skin-folds (biceps, triceps, subscapular, suprailiac) was measured twice on the right side of the body with a calliper (Harpenden, Burgess Hill, UK), and the average sum of the 4 skin-folds (in mm) was used as an indicator of body fat.
• Muscle strength: the strength of hip flexors and knee extensors was measured in persons whose main mode of ambulation was walking, and the strength of shoulder abductors and elbow extensors in persons whose main mode of ambulation was wheelchair driving, using the “break” testing method and a hand-held dynamometer (Microfet, Hoggan Health Industries, West Jordan UT, USA). The positions and performance of the measurements were according to van der Ploeg and co-workers (29). The average value of 3 repetitions of the dominant side was used for further analyses. Detailed descriptions of the testing method can be found elsewhere (12). To assess whether muscle strength was subnormal, values were normalized to Z-scores using reference values of healthy males and females (30, 31). A person’s lowest Z-score of upper or lower extremity was used as an indicator of muscle strength, dichotomizing it into normal (Z-score > –2) or subnormal (Z-score ≤ –2) muscle strength.
Statistical analyses
Data on sports participation were presented as mean (standard deviation (SD)) for the total group and for subgroups regarding gender and ambulatory status. Logistic regression analyses were performed to study correlates of sports participation, and linear regression analyses to study whether participating in sports was associated with higher levels of physical activity and physical fitness. Gender and ambulatory status were potential confounders adjusted for in all multivariable analyses. Due to high collinearity between type of ergometer and ambulatory status, ambulatory status was used as a proxy measure for type of ergometer (12). Odds ratios (OR) were presented for the logistic regressions and regression coefficients (RC) for the linear regressions, including 95% confidence intervals. p-values ≤ 0.05 were considered significant and p = 0.05–0.10 were mentioned as a trend.
RESULTS
Sports participation
Results for sports participation are presented in Table I. Thirty-five (69%) adolescents and young adults participated in sports, for an average of 30 (SD 24) min/day, which on average accounted for 3.3 (SD 2.5) kJ/kg/day. The top 5 sports were hand biking, (cardio) fitness, swimming, wheelchair basketball, and wheelchair tennis. The majority of the sports participants mentioned fun and improving fitness as main reasons for participating. Other reasons were to improve health, for social contacts or cosmetic reasons. Lack of time and lack of interest were the most frequently reported reasons for non-participation; others mentioned lack of energy, lack of transport, physical inability, not having a sports mate or fear of being criticized.
| Table I. Descriptive results for sports participation of adolescents and young adults with myelomeningocele |
| | Total group (n = 51) | Males (n = 26) | Females (n = 25) | Ambulators (n = 23) | Non-ambulators (n = 28) |
| Sport participation, n (%) | 35 (69) | 21 (81)* | 14 (56)* | 15 (65) | 20 (71) |
| Time spent on sports for doers†, min/day, mean (SD) | 30 (24) | 32 (27) | 27 (17) | 31 (29) | 29 (20) |
| Total sport score for doers†, kJ/kg/day, mean (SD) | 3.3 (2.5) | 3.5 (2.8) | 3.1 (2.0) | 3.2 (2.6) | 3.4 (2.4) |
| *Difference between males and females, p = 0.08. †Persons reporting participation in sports. SD: standard deviation |
Correlates of sports participation
Table II shows correlates of sports participation. Females tended to be less likely to participate in sports than males (OR = 0.30, p = 0.06). Ambulatory status, the presence of hydrocephalus, educational level, age, and motor and cognitive functioning were not related to sports participation.
| Table II. Association between sports participation and personal, disease-related, and psychosocial factors |
| Independent variable | Dependent variable | Logistic regression analyses |
| Sports (n = 35) | No sports (n = 16) | | p-value |
| Personal and disease-related factors | n (%) | n (%) | OR (95 % CI) | |
| Gender, male | 21 (60) | 5 (31) | 0.30 (0.09, 1.06) | 0.06 |
| Ambulators | 15 (43) | 8 (50) | 0.75 (0.23, 2.46) | 0.64 |
| Hydrocephalus | 26 (77) | 15 (94) | 0.16 (0.02, 1.54)1 | 0.11 |
| Educational level, low | 12 (34) | 5 (31) | 0.93 (0.24, 3.53)1 | 0.91 |
| | Mean (SD) | Mean (SD) | OR1 (95% CI) | |
| Age, years | 20.8 (4.8) | 21.8 (4.1) | 0.97 (0.86, 1.13) | 0.84 |
| Functional independence |
| Motor functioning | 6.03 (0.95) | 6.21 (0.49) | 0.81 (0.31, 2.09) | 0.66 |
| Cognitive functioning | 6.43 (0.70) | 6.58 (0.49) | 0.65 (0.19, 2.18) | 0.49 |
| Psychosocial factors |
| Social support |
| Friends | 11.7 (4.3) | 8.8 (4.5) | 1.17 (0.97, 1.40) | 0.09 |
| Family participation | 24.4 (7.0) | 19.4 (7.1) | 1.12 (1.00, 1.25) | 0.05 |
| Family rewarding | 13.2 (1.3) | 11.5 (2.9) | 2.12 (1.16, 3.86) | 0.01 |
| Perceived competence |
| Scholastic competence | 12.9 (3.0) | 11.7 (3.6) | 1.08 (0.88, 1.33) | 0.47 |
| Social acceptance | 15.2 (2.9) | 14.4 (3.2) | 1.05 (0.85, 1.31) | 0.66 |
| Athletic competence | 13.5 (3.4) | 8.4 (3.3) | 1.47 (1.17, 1.86) | 0.001 |
| Physical appearance | 13.5 (3.3) | 10.4 (4.3) | 1.24 (1.02, 1.50) | 0.03 |
| Behavioural conduct | 15.4 (2.9) | 15.2 (3.7) | 1.07 (0.87, 1.33) | 0.51 |
| Close friendships | 16.3 (3.6) | 15.6 (3.3) | 1.05 (0.88, 1.26) | 0.60 |
| Global self-worth | 16.0 (2.9) | 13.9 (3.9) | 1.20 (0.98, 1.48) | 0.10 |
| Enjoyment | 56.8 (10.9) | 49.4 (13.3) | 1.05 (0.99, 1.11) | 0.10 |
| 1Adjusted for gender and ambulatory status. OR: odds ratio; CI: confidence interval; SD: standard deviation. |
People who received more social support from family were more likely to participate in sports (OR = 1.12–2.12, p ≤ 0.05). In addition, those who received social support from friends (OR = 1.17, p = 0.09) and those who reported higher enjoyment of exercise (OR = 1.05, p = 0.10) tended to be more likely to participate in sports. Furthermore, sports participation was associated with athletic competence (OR = 1.47, p = 0.001) and physical appearance (OR = 1.24, p = 0.03), and appeared to have some association with global self-worth (OR = 1.20, p = 0.10).
Influence on physical activity behaviour and fitness
Table III presents results on physical activity and physical fitness and the association with sports participation. The 2-day objective measurements with the AM showed that participants spent on average 84 (SD 65) min on dynamic activities per day. According to the AM, after adjusting for gender and ambulatory status, sports participants spent 12 min longer on dynamic activities during the day than persons who did not participate in sports; however, this difference was not significant (p = 0.49).
| Table III. Association between sports participation and physical activity and physical fitness parameters |
| Dependent variable | Sports (n = 35) | No sports (n = 16) | Regression analyses |
| Mean (SD) | Mean (SD) | RC (95% CI)1 | p-value |
| Objective physical activity, AM |
| Dynamic activity, min/day | 84 (65) | 74 (57) | 12 (–23, 47) | 0.49 |
| Self-reported physical activity, PASIPD |
| Total score, kJ/kg/day | 58.6 (37.5) | 29.7 (23.6) | 29.6 (7.7, 51.6) | 0.009 |
| Total duration, min/day | 285 (191) | 179 (141) | 115 (0.6, 230) | 0.05 |
| Leisure activity, min/day |
| Non-exercise related walk/wheel | 122 (84) | 73 (83) | 56 (4, 109) | 0.04 |
| Light exercise | 16 (50) | 6 (19) | 4 (–23, 32) | 0.75 |
| Moderate + vigorous + strength exercise | 44 (45) | 3 (7) | 39 (14, 63) | 0.002 |
| Household activity, min/day | 41 (67) | 46 (59) | 5 (–36, 45) | 0.82 |
| Occupational activity, min/day | 61 (67) | 51 (96) | 11 (–51, 74) | 0.72 |
| Physical fitness | | | | |
| PeakVO2, l/min | 1.58 (0.53) | 1.27 (0.50) | 0.19 (–0.06, 0.44) | 0.13 |
| Sum 4 skin-folds, mm | 74.0 (38.6) | 75.5 (39.4) | 7.78 (–11.3, 26.9) | 0.42 |
| | % subnormal | % subnormal | OR (95% CI)1 | |
| Muscle strength, normal (0) vs subnormal (1) | 52 | 81 | 0.26 (0.06, 1.15) | 0.08 |
| 1Adjusted for gender and ambulatory status SD: standard deviation; RC: linear regression coefficient; OR: odds ratio; CI: confidence interval; AM: activity monitor; PASIPD: physical activity scale for individuals with physical disabilities. |
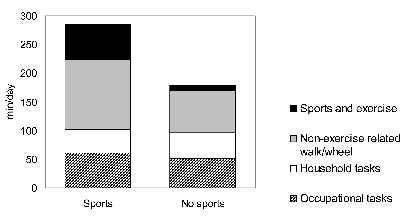
Self-reported physical activity recalled over the previous 7 days with the PASIPD, showed that sport participants spent on average 285 (191) min combined in leisure, household and occupational activities, corresponding with an average total score of 58.6 (37.5) kJ/kg/day. Results of the PASIPD showed that persons who engaged in sports were more physically active during the day, as indicated by total score (p = 0.009) and by total duration of physical activities expressed in min/day (p = 0.05). In addition, besides spending on average 39 min more on sports and exercise per day (p = 0.002), they also reported 56 min more on non-exercise-related walking or wheelchair driving (p = 0.04).
Fig. 1 shows the contribution of occupational tasks, household tasks, sports and exercise, and non-exercise related walking or wheelchair driving to total self-reported physical activity as measured with the PASIPD. In sports participants, the contribution of sports and exercise to total physical activity was 16%. Time spent on household and occupational activities did not differ between persons who participated in sports and those who did not (Fig. 1; Table III).
Fig. 1. Contribution of sports to total physical activity behaviour as measured with the Physical Activity Scale for Individuals with Physical Disabilities (PASIPD).
Average peak VO2 was 0.19 l/min higher in persons who participated in sports compared with those who did not; however this difference was not significant (p = 0.13). The percentage of participants with subnormal muscle strength tended to be lower in those who participated in sports (52%) compared with those who did not (81%; OR = 0.26, p = 0.08). Sports participation was not associated with body fat.
DISCUSSION
Sports and physical activity behaviour
The present study contributes to the understanding of sports participation behaviour in adolescents and young adults with MMC. Two-third of the study participants reported to be engaged in sports, which accounted for 30 min each day on average. Comparably, 6 out of 10 able-bodied persons aged 18–24 years participate in sports in The Netherlands (32). Of people with various physical disabilities (including persons after stroke, back disorders, neurological disorders, chronic pain and orthopaedic disorders), 53% participated in sports one year after rehabilitation (33). Although the proportion of adolescents and young adults with MMC participating in sports was not lower than in people with other physical disabilities, the estimated energy expended per day due to self-reported sports activities, as indicated by total sport score, was almost half as low; 3.3 kJ/kg/day in people with MMC vs 6.3 kJ/kg/day in people with other physical disabilities (33). It is unclear whether this difference is due to less time spent on sports or to lower intensity sports. In addition, self-reported levels of physical activity, as measured with the PASIPD, were considerably lower than those mentioned in persons with a variety of physical disabilities: average PASIPD scores reported by Washburn and co-workers (26) and by van der Ploeg and co-workers (33) – these were 84.5 kJ/kg/day and 63.7 kJ/kg/day, respectively, whereas the current study showed an average score of 58.6 kJ/kg/day in sport participants and 29.7 kJ/kg/day in non-participants. This is in line with results from previous studies reporting that persons with MMC have inactive lifestyles (9, 10).
Correlates of sports participation
Results showed that ambulatory status, the presence of hydrocephalus and functional independence were not related to sports participation. This is an important contribution to knowledge on physical activity behaviour in persons with MMC. In addition to lack of time and lack of interest being the most frequently mentioned barriers for sports participation, it supports the view that engaging in sports is a choice rather than an inability. Therefore, persons with MMC should be encouraged to become more physically active, and sports participation may be a way to accomplish this. Rehabilitation centres may provide a good setting to increase physical activity levels (13, 33).
A large proportion of persons with MMC show cognitive impairments of some sort (34), which may influence sports participation. In the present study, however, sports participation was not associated with educational level or cognitive functioning. Nevertheless, impairments in executive functioning rather than general intelligence might be associated with physical activity levels (35). Future studies are necessary to investigate the association between sports participation and cognitive impairments.
In the context of promoting physical activity behaviour, modifiable environmental and personal determinants are the most interesting targets in interventions. In able-bodied adults, the association between social support and physical activity behaviours is inconclusive (36). However, the present results support the view that social support is important for adolescents and young adults with MMC to participate in sports. This study did not include other environmental influences (7); however, in 113 adults with mobility impairments, Kinne and co-workers (5) found that exercise maintenance was not significantly associated with environmental barriers, whereas motivational barriers and self efficacy were. In contrast, other studies reported lack of transportation and accessibility facilities to be important barriers to exercise (6, 7). Future studies should provide insights into the role of such environmental barriers to sports participation and physical activity in general in persons with MMC. In line with the results of Kinne and co-workers (5), the present study showed that adolescents and young adults with MMC who perceived higher athletic competence were more likely to participate in sports than those who perceived lower athletic competence. In addition, sports participation was associated with perceived physical appearance and tended to be associated with global self-worth. Due to the cross-sectional study design, it is unclear whether persons with higher athletic competence, perceived physical appearance and global self-worth are more likely to participate in sports or whether participating in sports results in higher perceived competence for these aspects.
Furthermore, the present study showed that persons who perceived higher enjoyment during sports tended to be more likely to participate in sports. This is in line with previous results in persons with spinal cord injuries, that enjoyment was an important reason for participating in sports (37). Therefore, interventions aiming to increase physical activity levels should be tailored individually, ensuring that each person finds a type of physical activity that they enjoy.
Sports participation and physical activity
The present study found some evidence that persons who participated in sports had more active lifestyles than those who did not, regardless of gender and ambulatory status. Sports participation contributed to 16% of the total daily physical activity in persons who participated in sports. This is an important contribution to total physical activity behaviour because apparently, non-participants do not seem to compensate with other physical activities, such as household and occupational. In addition, those who participated in sports reported that they also spent more time on non-exercise-related walking or wheeling. Objective measurements of physical activity with the AM pointed in the same direction, i.e. persons who participated in sports spent on average 12 min more on dynamic activities, but it was not significantly different. In addition, there was a substantial difference in the total duration of physical activity measured with both instruments; the AM registered an average duration of 84 min/day, whereas the PASIPD reported 285 min/day. Both measures have limitations, which may have contributed to the discrepancy in results. Questionnaires are prone to overestimation of physical activity levels due to social desirability and recall difficulties (38). Furthermore, objective measurements with the AM covered 2 consecutive weekdays, whereas the self-reported PASIPD was a 7 day-recall, also including weekend-days. Although in this study the measurement days overlapped, the PASIPD covered a period more representative for usual physical activity patterns and probably recorded usual activities that may be missed by the AM, especially at the weekend. Moreover, both instruments measure somewhat different aspects of physical activity. The AM measures mobility-related activities, whereas the PASIPD includes several physical activity domains, i.e. leisure, household and occupational activities, of which not all are necessarily mobility-related and therefore not detected with the AM. We therefore consider both measures to be complementary using the PASIPD to describe the contribution of specific activity domains to total physical activity behaviour.
Sports participation and physical fitness
Although the present study failed to show significant correlations, data showed higher values of peak VO2 and higher muscle strength in sports participants. Fitness is known to be an independent risk factor for lifestyle-related diseases, but low values in persons with MMC are reported (12). Therefore, increasing sport participation may be important to increase and maintain health of persons with MMC. The correlation between sports participation and fitness has been found previously in persons with spinal cord injuries (39). Due to the relatively small sample sizes in the present study, correlations may have failed to show significances. There did not seem to be a correlation between sport participation and body fat levels.
Considering that the primary mode of ambulation elicits the highest values of peak VO2 we used different exercise modes to assess aerobic capacity for ambulatory and non-ambulatory persons. Arm and leg exercise are known to have different physiological responses. In the analyses, we adjusted for ambulatory status as a proxy measure for type of ergometer (12).
Study limitations
Some limitations should be taken into account when interpreting the results of the study. The response rate of the study was low, which may have led to selection bias with people who were more interested in physical activity being more likely to participate in the study. This may have resulted in the high proportion of sports participation. However, it is unlikely that this selection bias has influenced the relevant correlates of sports participation as well as its relation with fitness. Another limitation was the relatively small sample size and low statistical power, which might have led to overlooking some of the relevant relationships.
Furthermore, both the sport score and the PASIPD score were based on MET values derived from the general population. It is possible that MET values for the same activity differ between the general population and the persons with MMC. Consequently, the absolute values of the sport score and the PASIPD score might not be completely accurate, and comparability with the general population may be limited. However, during several daily activities, oxygen uptake did not differ between persons with MMC and aged-matched peers, although physical strain was higher in persons with MMC (40).
In conclusion, sports participation seems to be due to personal preferences rather than physical ability, it could benefit from social support (particularly from the patient’s family) and perceived competence, and is associated with higher self-reported physical activity. Conclusive evidence is needed on whether sports participation improves aerobic capacity. Improving physical activity behaviour and fitness in persons with MMC is important for health, and increasing sports participation may contribute.
AcknowledgEments
This study was supported by Johanna Children’s Fund (Arnhem, The Netherlands, grant numbers 20000005/20000158). The Trustfonds (Erasmus University Rotterdam) provided a grant to the first author (grant number 97030.16/07.0483) for a working visit to the Centre for Physical Activity and Health (University of Sydney, Australia). We thank all participating adolescents and young adults with MMC. The following members of the Transition Research Group South West Netherlands contributed to this study: Department of Rehabilitation Medicine, University Medical Center Rotterdam (J. van Meeteren, MD PhD, W. G. M. Janssen MD); Rijndam Rehabilitation Center (M. P. Bergen, MD PhD, D. Spijkerman, MD); Sophia Rehabilitation, The Hague and Delft (M. Rol, MD); Rijnlands Rehabilitation Center, Leiden (H. vd Heijden-Maessen, MD); Rehabilitation Center “De Waarden”, Dordrecht (H. J. R. Buijs, MD); Foundation of Rehabilitation Medicine Zeeland, Goes (Th. Voogt, MSc); Department of Rehabilitation Medicine, Leiden University Medical Center (J. H. Arendzen, MD PhD, M. S. van Wijlen-Hempel, MD, PhD). In addition, the University Medical Center Utrecht (M. W. Post, PhD) and VU University Medical Center (C. J. McDonald-ten Thij) collaborated in the study.
REFERENCES
1. Rimmer JH. Health promotion for people with disabilities: the emerging paradigm shift from disability prevention to prevention of secondary conditions. Phys Ther 1999; 79: 495–502.
2. United States Department of Health and Human Services. Healthy People 2010: Understanding and improving health. 2nd edn. Washington DC: US Government Printing Office; Nov 2000. Available from: http://www.health.gov/healthypeople
3. Cooper RA, Quatrano LA, Axelson PW, Harlan W, Stineman M, Franklin B, et al. Research on physical activity and health among people with disabilities: a consensus statement. J Rehabil Res Dev 1999; 36: 142–154.
4. Heath GW, Fentem PH. Physical activity among persons with disabilities – a public health perspective. Exerc Sport Sci Rev 1997; 25: 195–234.
5. Kinne S, Patrick DL, Maher EJ. Correlates of exercise maintenance among people with mobility impairments. Disabil Rehabil 1999; 21: 15–22.
6. Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med 2004; 26: 419–425.
7. Ellis R, Kosma M, Cardinal BJ, Bauer JJ, McCubbin JA. Physical activity beliefs and behaviour of adults with physical disabilities. Disabil Rehabil 2007; 29: 1221–1227.
8. Verhoef M, Barf HA, Post MW, van Asbeck FW, Gooskens RH, Prevo AJ. Secondary impairments in young adults with spina bifida. Dev Med Child Neurol 2004; 46: 420–427.
9. Bandini LG, Schoeller DA, Fukagawa NK, Wykes LJ, Dietz WH. Body composition and energy expenditure in adolescents with cerebral palsy or myelodysplasia. Pediatr Res 1991; 29: 70–77.
10. Buffart LM, Roebroeck ME, Rol M, Stam HJ, van den Berg-Emons RJ. Triad of physical activity, aerobic fitness and obesity in adolescents and young adults with myelomeningocele. J Rehabil Med 2008; 40: 70–75.
11. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985; 100: 126–131.
12. Buffart LM, van den Berg-Emons RJ, van Wijlen-Hempel MS, Stam HJ, Roebroeck ME. Health-related physical fitness of adolescents and young adults with myelomeningocele. Eur J Appl Physiol 2008; 103. 181–188.
13. van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten MM, van Harten WH, et al. Counselling increases physical activity behaviour nine weeks after rehabilitation. Br J Sports Med 2006; 40: 223–229.
14. Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32: S498–S504.
15. Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg Am 1973; 55: 137–148.
16. Hall KM, Hamilton BB, Gordon WA, Zasler ND. Characteristics and comparisons of functional assessment indices: Disability Rating Scale, Functional Independence Measure and Functional Assessment Measure. J Head Trauma Rehabil 1993; 8: 60–74.
17. McPherson KM, Pentland B, Cudmore SF, Prescott RJ. An inter-rater reliability study of the Functional Assessment Measure (FIM+FAM). Disabil Rehabil 1996; 18: 341–347.
18. Hawley CA, Taylor R, Hellawell DJ, Pentland B. Use of the functional assessment measure (FIM+FAM) in head injury rehabilitation: a psychometric analysis. J Neurol Neurosurg Psychiatry 1999; 67: 749–754.
19. Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987; 16: 825–836.
20. Stevens M, Bakker van Dijk A, de Greef MH, Lemmink KA, Rispens P. A Dutch version of the Social Support for Exercise Behaviors Scale. Percept Mot Skills 2000; 90: 771–774.
21. Harter S, editor. Manual for the Self-Perception Profile for Adolescents. Denver, CO: University of Denver; 1988.
22. Treffers PDA, Goedhart AW, van den Bergh BRH, Veerman JW, Ackaert L, de Rycke L, editors. Competentie Belevingsschaal voor Adolescenten [Dutch edition of the Self-perception Profile for Adolescents]. Lisse: Hartcourt Test Publishers; 2002 (in Dutch).
23. Stevens M, Moget P, de Greef MH, Lemmink KA, Rispens P. The Groningen Enjoyment Questionnaire: a measure of enjoyment in leisure-time physical activity. Percept Mot Skills 2000; 90: 601–604.
24. Bussmann JB, Martens WL, Tulen JH, Schasfoort FC, van den Berg-Emons HJ, Stam HJ. Measuring daily behavior using ambulatory accelerometry: the Activity Monitor. Behav Res Methods Instrum Comput 2001; 33: 349–356.
25. Postma K, van den Berg-Emons HJ, Bussmann JB, Sluis TA, Bergen MP, Stam HJ. Validity of the detection of wheelchair propulsion as measured with an Activity Monitor in patients with spinal cord injury. Spinal Cord 2005; 43: 550–557.
26. Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 2002; 83: 193–200.
27. van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten M, van Mechelen W. The Physical Activity Scale for Individuals with Physical Disabilities: test-retest reliability and comparison with an accelerometer. J Phys Act Health 2007; 4: 96–100.
28. Bar-Or O, editor. Pediatric sports medicine for the practitioner. From physiologic principles to clinical applications. New York: Springer Verlag; 1983.
29. van der Ploeg RJ, Fidler V, Oosterhuis HJ. Hand-held myometry: reference values. J Neurol Neurosurg Psychiatry 1991; 54: 244–247.
30. Bohannon RW. Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil 1997; 78: 26–32.
31. Phillips BA, Lo SK, Mastaglia FL. Muscle force measured using “break” testing with a hand-held myometer in normal subjects aged 20 to 69 years. Arch Phys Med Rehabil 2000; 81: 653–661.
32. Centraal Bureau voor de Statistiek. Jeugd 2003, cijfers en feiten [Youth 2003, numbers and facts]. Voorburg/Heerlen: Centraal Bureau voor de Statistiek; 2003 (in Dutch).
33. van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten MM, van Harten WH, et al. Successfully improving physical activity behavior after rehabilitation. Am J Health Promot 2007; 21: 153–159.
34. Barf HA, Verhoef M, Jennekens-Schinkel A, Post MW, Gooskens RH, Prevo AJ. Cognitive status of young adults with spina bifida. Dev Med Child Neurol 2003; 45: 813–820.
35. Roebroeck ME, Hempenius L, van Baalen B, Hendriksen JG, van den Berg-Emons HJ, Stam HJ. Cognitive functioning of adolescents and young adults with meningomyelocele and level of everyday physical activity. Disabil Rehabil 2006; 28: 1237–1242.
36. Prochaska JJ, Rodgers MW, Sallis JF. Association of parent and peer support with adolescent physical activity. Res Q Exerc Sport 2002; 73: 206–210.
37. Wu SK, Williams T. Factors influencing sport participation among athletes with spinal cord injury. Med Sci Sports Exerc 2001; 33: 177–182.
38. Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 2000; 71: S1–S14.
39. Dallmeijer AJ, Hopman MT, van As HH, van der Woude LH. Physical capacity and physical strain in persons with tetraplegia; the role of sport activity. Spinal Cord 1996; 3 : 729–735.
40. Bruinings AL, van den Berg-Emons HJ, Buffart LM, van der Heijden-Maessen HC, Roebroeck ME, Stam HJ. Energy cost and physical strain of daily activities in adolescents and young adults with myelomeningocele. Dev Med Child Neurol 2007; 49: 672–677.