OBJECTIVE: The aims of this study were: (i) to classify subgroups according to the degree of pain intensity, depression, and catastrophizing, and investigate distribution in a group of patients with chronic whiplash-associated disorders; and (ii) to investigate how these subgroups were distributed and inter-related multivariately with respect to consequences such as health and quality of life outcome measures.
DESIGN: Descriptive cross-sectional study.
Patients: A total of 275 consecutive chronic pain patients with whiplash-associated disorders who were referred to a university hospital.
METHODS: The following data were obtained by means of self-report questionnaires: pain intensity in neck and shoulders, background history, Beck Depression Inventory, the catastrophizing scale of Coping Strategy Questionnaire, Life Satisfaction Checklist, the SF-36 Health Survey, and the EuroQol.
RESULTS: Principal component analysis was used to recognize subgroups according to the degree of pain intensity, depression, and catastrophizing. These subgroups have specific characteristics according to perceived health and quality of life, and the degree of depression appears to be the most important influencing factor.
CONCLUSION: From a clinical point of view, these findings indicate that it is important to assess patients for intensity of pain, depression, and catastrophizing when planning a rehabilitation programme. Such an evaluation will help individualize therapy and intervention techniques so as to optimize the efficiency of the programme.
Key words: neck, whiplash, pain, depression, catastrophizing, health, quality of life.
J Rehabil Med 2008; 40: 562–569
Correspondence address: Björn Börsbo, Department of Rehabilitation Medicine, Faculty of Health Sciences, SE-581 85 Linköping, Sweden. E-mail: bjorn.borsbo@inr.liu.se
Submitted March 7, 2007; accepted February 26, 2008
Introduction
Chronic pain, including chronic whiplash-associated disorder (WAD), has a negative impact on quality of life (1, 2) and negative consequences for perceived health (3–5). The bio-psycho-social framework of chronic pain (6) proposes an interaction between several factors that influence the development and maintenance of chronic pain and its consequences.
Pain intensity is an important factor that contributes to various forms of disability, which in turn is related to the chronicity dimension of pain. Acute pain levels can predict functional outcome following whiplash injury (7, 8). However, in terms of the impact on perceived quality of life, pain intensity has not been found to be the most prominent contributor (9).
Catastrophizing has been broadly defined as an exaggerated negative orientation toward pain stimuli and pain experience (10). Studies identify connections between catastrophizing and psychological distress (11), physical functioning and disability (12), ratings of pain intensity (13), interference with life activities (14), psychosocial dysfunction (15) and quality of life (16). Knowledge about whether catastrophizing is a cause or a consequence of chronic pain is still lacking (17); there are studies that can be interpreted either way (10, 18–21).
Depression is not simply a co-morbid condition, but interacts with chronic pain to increase morbidity and mortality. High frequencies of depressive symptoms have been found in patients with chronic pain as well in the chronic WAD subgroup (22, 23). Depressed patients with chronic pain report greater pain intensity, greater interference from pain, more pain behaviours, less life control, and greater use of passive/avoidance coping strategies than non-depressed patients with chronic pain (24, 25). The temporal relationship between chronic pain and depression is under debate. Fishbain et al. (26) found strong support for the consequence hypothesis: depression is a consequence that follows the development of pain. To describe the relationship between chronic pain and depression, Banks & Kerns (22) developed a diathesis-stress-model where the diathesis is conceptualized as pre-existing, semi-dormant characteristics of the individual before the onset of chronic pain. These characteristics are activated by the stress of the chronic condition and may lead to depression. Qualitative differences between depression as a result of chronic pain and depression as a primary psychiatric disorder have been reported (26, 27). Pincus & Morley (28) suggest that “affective distress”, which incorporates wider emotions such as anger, frustration, fear, and sadness, is a better term than “depression”.
The framework of the bio-psycho-social model emphasizes an integrated relationship between depression, pain intensity and catastrophizing. Fear and avoidance beliefs and strategies are influenced by catastrophizing and depression in patients with chronic pain. Distinct profiles of psychological functioning could be identified and meaningfully related to future disability (29). For chronic WAD patients, a combination of symptoms (pain and depression) and catastrophizing may explain their health-related quality of life issues (9).
Based on the above literature it is reasonable to expect that patients with high pain intensity, depression and catastrophizing will perceive their health and quality of life as considerably worse than those patients who rate their situations better with respect to these 3 factors. Using, for example, certain regression techniques, the mean influences of these 3 factors on health and quality of life can theoretically be determined separately at group level for each outcome variable. However, the clinical question might be more complex; for example, are the effects of high catastrophizing with respect to health and quality of life similar when pain intensity is high and low? Or, from a treatment or rehabilitation perspective, is it important to intervene against high catastrophizing regardless of pain intensity in patients with WAD? These questions are complex and require a large number of subjects in order to achieve valid regression models for the whole range of the 3 symptoms (i.e. pain intensity, depression and catastrophizing). An alternative approach is to divide into subgroups based on dichotomizing of the 3 symptoms separately and then investigate how the different combinations of dichotomized symptoms will differ with respect to health and quality of life. In a second step based on these results, but also requiring a substantial sample size, cluster analysis can be performed in order to confirm the results obtained.
Aims
The aims of this study were: (i) to classify subgroups according to the degree of pain intensity, depression, and catastrophizing and to investigate the distribution in a group of patients with chronic WAD; and (ii) to investigate how these subgroups are distributed and interrelated multivariately with respect to consequences such as health and quality of life outcome measures.
PATIENTS and Methods
Patients
All patients were recruited from the consecutive flow of patients during 3 years seeking care at the Pain and Rehabilitation Centre of the University Hospital, Linköping, Sweden. This cross-sectional study is based on 275 patients fulfilling the criteria of WAD grades II or III (see (9) for details).
Methods
Each patient received a questionnaire, to be completed at home, shortly before the examination at the centre. The questionnaire contained the following items and instruments (for references concerning the instruments presented below including psychometric aspects see (9)):
• Age, gender, and anthropometric data.
• Number of visits to a physician in the previous 6 months, number of days sick-leave during the previous 12 months, number of months out of work. The degree of sick-leave/disability pension is assessed in terms of 4 percentage levels, ranging from 0% to 100% according to the Swedish social security system.
• Pain intensity ratings using a visual analogue scale (VAS) at 11 predefined anatomical regions in the previous 7 days (30); in the present study only the mean value of the neck and shoulders was used.
• The Beck Depression Inventory (BDI) combines 21 symptoms of depression in a scale ranging from 0 to 63.
• The coping strategy catastrophizing (CSQ-cat) of the Coping Strategy Questionnaire (CSQ) was used to measure catastrophizing.
• The instrument Life Satisfaction Questionnaire, LiSat-11, consisted of estimations of life satisfaction in general (LSQgen) as well as 10 specific domains to be estimated: satisfaction with vocational situation (LSQwork), financial situation (LSQecon), leisure situation (LSQleis), contact with friends and acquaintance (LSQsoc), sexual life (LSQsex), activities of daily living (ADL) (LSQadl), family life (LSQfam), and partnership (LSQmarr), physical (LSQphysH) and psychological health (LSQpsycH).
• SF-36 Health Survey (Swedish version) is an instrument that intends to represent multi-dimensional health concepts and measurements of the full range of health states, including levels of well-being and personal evaluations of health. The instrument has 8 dimensions (reported using a standardized scale from 0 to 100): physical functioning (SF 36pf), role limitations due to physical functioning (SF 36rp), bodily pain (SF 36bp), general health (SF 36gh), vitality (SF 36vit), social functioning (SF 36sf), role limitations due to emotional problems (SF 36re), and mental health (SF 36mh).
• The European Quality of Life instrument (EuroQol) captures a patient's perceived state of health and 5 dimensions (EQ-5D) are defined in the first part of the instrument: mobility (Eqmob), self-care (Eqhyg), usual activities (Eqact), pain/discomfort (Eqpain), and anxiety/ depression (Eqanx). A second part concerns a self-estimation of today's health according to a 100-point scale, a "thermometer" (EQ-VAS) with defined end-points (high values indicate good health and low values indicate bad health).
Statistics
All statistical evaluations were made using the statistical packages SPSS (version 12.0) for traditional statistics and SIMCA-P+ (version 11.1) for multivariate statistics. Results in the text and tables are generally given as mean values and 1 standard deviation (SD). For univariate comparisons between groups, analysis of variance (ANOVA) was used for all variables except gender, for which the χ2-test square was used.
Each subject was classified on the basis of catastrophizing (CSQ-cat), depression (BDI), and pain intensity in the neck/shoulder (VAS). Subjects were classified as “high” if their value for the variable was higher than or the same as the median value for the whole group and as “low” if it was lower. Hence the following combinations exist: high pain (HP), low pain (LP), high depression (HD), low depression (LD), high catastrophizing (HC), and low catastrophizing (LC). These can be combined into 8 possible combinations or subgroups (SG): SG1: HP/HD/HC; SG2: HP/HD/LC; SG3: HP/LD/HC; SG4: HP/LD/LC; SG5: LP/HD/HC; SG6: LP/HD/LC; SG7: LP/LD/HC; and SG8: LP/LD/LC.
For each of the 8 subgroups, the mean values of LISAT-11, EuroQol, and SF-36 were used in a Principal Component Analysis (PCA) using SIMCA-P+. PCA can be viewed as a multivariate correlation analysis and was used to investigate how the 8 subgroups are multivariately interrelated with respect to the health and quality of life variables (i.e. LISAT-11, EuroQol, and SF-36). A cross-validation method, which keeps part of the data out of the model development, is used to assess the predictive power of the model. A component consists of a vector of numerical values between –1 and 1, referred to as loadings (p) and obtained significant components are uncorrelated. Variables that have high loadings (with positive or negative sign) on the same component are inter-correlated. Items with high loadings (ignoring the sign) are considered to be of large or moderate importance for the component under consideration. When obtaining more than one component, the vectors are orthogonally projected to each other and thus uncorrelated. Two plots are generated from the PCA analysis: the loading plot describes correlations between variables; while the score plot (scores are denoted as t) describes correlations between the subjects (the sub-groups in the present study). Two concepts are further used to describe the results: R2 and Q2. R2 describes the goodness of fit – the fraction of sum of squares of all the variables explained by a principal component. Q2 describes the goodness of prediction – the fraction of the total variation of the variables that can be predicted by a principal component using cross-validation methods. Outliers were identified using the 2 methods available in SIMCA-P+: score plots in combination with Hotelling’s T2 and distance to model in X-space (DModX). For all statistical analyses, p ≤ 0.05 was regarded as significant.
Results
Distributions and characteristics of the 8 subgroups
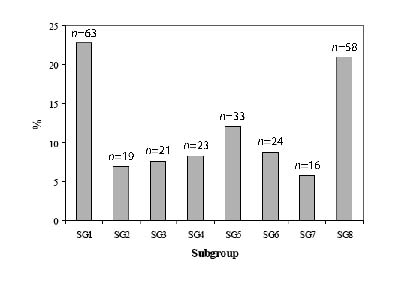
The results of the classification procedure – based on pain intensity, BDI, and CSQ-cat – showed that 24.7% of the patients with WAD belonged to SG1 and 22.6% to SG8 (Fig. 1). SG1 (i.e. HP/HD/HC) scored high on all scales used in the classification procedure, while SG8 scored low according to the 3 classification variables (i.e. LP/LD/LC). The remaining half (approximately 52%) of the patients with WAD were relatively equally distributed among the intermediary subgroups (Fig. 1).
Fig. 1. Distribution of the different subgroups (SG) based on high or low values of pain intensity, depression, and catastrophizing. SG1 had high values on these 3 dichotomized variables, SG8 low levels and SG2–7 intermediary values.
According to the statistical analyses (ANOVA) of the background variables, no significant differences were found with respect to age, gender, or items related to sick-leave and disability pension. The only exception was the “number of visits to physician”, which had highest values in SG1 (4.5 (SD) 3.0 visits) and SG6 (4.5 (SD) 2.5 visits) and lowest in SG3 (2.6 (SD) 2.4 visits) (p = 0.048).
In sharp contrast, there were significant differences in almost all variables concerning aspects of quality of life and perceived health (Table I); i.e. SF-36, LiSAT-11 and EuroQol. As expected, the SG1 with high figures on the 3 classification variables (i.e. pain intensity, BDI, and CSQ-cat) perceived the situation as worst.
| Table I. Mean values (1 standard deviation (SD)) of SF36, LiSAT-11, and EuroQol in the 8 subgroups (SG). The right-hand column shows the result of the univariate statistical evaluation |
| Variables | All Mean (SD) | SG 1 Mean (SD) | SG 2 Mean (SD) | SG 3 Mean (SD) | SG 4 Mean (SD) | SG 5 Mean (SD) | SG 6 Mean (SD) | SG 7 Mean (SD) | SG 8 Mean (SD) | ANOVA p-value |
| Scales of SF-36 |
| Physical functioning | 58.0 (24.5) | 45.2 (22.1) | 50.8 (23.0) | 54.4 (20.8) | 60.0 (20.9) | 65.6 (40.7) | 63.6 (17.0) | 65.5 (10.7) | 66.3 (16.1) | < 0.001 |
| Role physical | 11.5 (26.9) | 6.3 (20.9) | 6.9 (14.4) | 11.9 (26.9) | 16.3 (29.8) | 16.1 (42.6) | 5.7 (17.1) | 9.3 (18.0) | 16.7 (28.1) | ns |
| Bodily pain | 24.2 (14.7) | 13.9 (11.0) | 16.3 (11.5) | 22.9 (15.2) | 26.0 (16.1) | 26.0 (14.8) | 29.6 (11.8) | 24.2 (1.3) | 34.4 (12.0) | < 0.001 |
| General health | 44.0 (20.8) | 34.3 (19.7) | 35.4 (19.7) | 46.9 (18.8) | 53.8 (21.8) | 32.8 (11.9) | 42.4 (14.5) | 47.1 (15.8) | 58.2 (20.4) | < 0.001 |
| Vitality | 29.4 (19.8) | 18.6 (15.9) | 16.8 (13.8) | 35.4 (21.1) | 43.7 (19.0) | 24.8 (15.1) | 25.6 (16.2) | 29.0 (15.8) | 41.9 (19.2) | < 0.001 |
| Social functioning | 56.0 (28.5) | 39.6 (27.0) | 38.8 (22.8) | 67.9 (29.7) | 75.5 (25.7) | 44.9 (21.7) | 60.4 (26.0) | 46.9 (21.7) | 74.1 (20.8) | < 0.001 |
| Role emotional | 51.6 (45.6) | 28.8 (41.7) | 45.1 (48.5) | 56.7 (46.0) | 95.7 (15.2) | 23.7 (37.7) | 50.0 (40.8) | 48.9 (46.9) | 73.6 (38.9) | < 0.001 |
| Mental health | 61.0 (21.4) | 46.3 (21.1) | 57.1 (18.6) | 70.1 (15.2) | 78.4 (12.3) | 46.9 (17.3) | 60.7 (16.3) | 57.5 (14.8) | 77.1 (14.5) | < 0.001 |
| Scales of LiSat-11 |
| Life as a whole | 3.7 (1.4) | 2.9 (1.3) | 2.8 (1.3) | 4.5 (1.1) | 4.1 (1.7) | 3.3 (0.9) | 3.7 (1.3) | 4.0 (1.82) | 4.7 (1.0) | < 0.001 |
| Vocational situation | 3.0 (1.7) | 2.5 (1.8) | 1.5 (0.8) | 3.3 (1.5) | 3.0 (1.6) | 2.2 (1.5) | 3.0 (1.7) | 3.2 (1.5) | 4.1 (1.3) | < 0.001 |
| Financial situation | 3.6 (1.4) | 2.7 (1.5) | 2.8 (1.7) | 3.8 (1.3) | 3.9 (1.1) | 3.3 (1.2) | 3.2 (1.5) | 4.3 (1.0) | 4.5 (0.9) | < 0.001 |
| Leisure | 3.2 (1.5) | 2.6 (1.3) | 1.9 (0.9) | 3.5 (1.5) | 4.0 (1.2) | 2.6 (1.2) | 3.5 (1.4) | 3.6 (2.0) | 4.3 (1.2) | < 0.001 |
| Contacts with friends | 4.1 (1.5) | 3.4 (1.6) | 3.5 (1.3) | 4.8 (1.2) | 4.6 (1.2) | 3.4 (1.3) | 4.0 (1.3) | 4.3 (1.7) | 5.0 (1.0) | < 0.001 |
| Sexual life | 3.6 (1.6) | 2.9 (1.6) | 3.0 (2.1) | 4.4 (1.0) | 5.0 (0.9) | 3.0 (1.5) | 3.0 (1.6) | 3.9 (1.4) | 4.3 (1.4) | < 0.001 |
| ADL | 4.8 (1.3) | 4.2 (1.5) | 4.2 (1.7) | 4.6 (1.3) | 4.6 (1.4) | 4.6 (1.1) | 5.3 (0.9) | 5.4 (0.6) | 5.4 (1.0) | < 0.001 |
| Family life | 4.8 (1.2) | 4.1 (1.5) | 4.7 (1.2) | 5.2 (0.8) | 5.3 (0.8) | 4.2 (1.1) | 4.7 (1.1) | 5.2 (0.7) | 5.3 (0.9) | < 0.001 |
| Partnership relations | 4.4 (1.6) | 3.6 (1.8) | 4.3 (1.7) | 5.1 (1.0) | 5.4 (0.8) | 3.9 (1.4) | 4.2 (1.7) | 4.5 (1.7) | 5.0 (1.2) | < 0.001 |
| Physical health | 2.6 (1.4) | 2.2 (1.4) | 1.7 (1.0) | 3.0 (1.3) | 2.3 (1.1) | 2.3 (1.1) | 2.4 (1.5) | 2.9 (1.5) | 3.3 (1.3) | < 0.001 |
| Psychological health | 3.8 (1.3) | 3.0 (1.3) | 3.5 (1.0) | 4.7 (0.9) | 4.5 (1.0) | 2.8 (1.1) | 3.3 (1.2) | 3.9 (1.4) | 4.7 (0.8) | < 0.001 |
| Scales of EuroQol |
| Mobility | 1.4 (0.5) | 1.6 (0.6) | 1.5 (0.5) | 1.5 (0.5) | 1.4 (0.5) | 1.4 (0.5) | 1.1 (0.3) | 1.1 (0.3) | 1.2 (0.4) | < 0.001 |
| Self-care | 1.2 (0.4) | 1.3 (0.5) | 1.2 (0.4) | 1.2 (0.4) | 1.2 (0.4) | 1.2 (0.4) | 1.2 (0.4) | 1.0 (0.0) | 1.1 (0.3) | 0.022 |
| Usual activities | 2.2 (0.6) | 2.2 (0.6) | 2.4 (0.7) | 2.1 (0.6) | 2.2 (0.7) | 2.2 (0.6) | 2.2 (0.6) | 2.3 (0.6) | 2.1 (0.6) | ns |
| Pain/discomfort | 2.6 (0.5) | 2.8 (0.4) | 3.0 (0.0) | 2.7 (0.5) | 2.6 (0.5) | 2.6 (0.5) | 2.3 (0.5) | 2.8 (0.4) | 2.4 (0.5) | < 0.001 |
| Anxiety/depression | 1.8 (0.6) | 2.2 (0.6) | 1.8 (0.5) | 1.6 (0.5) | 1.3 (0.5) | 2.3 (0.5) | 2.0 (0.5) | 1.9 (0.6) | 1.4 (0.5) | < 0.001 |
| EQ-5D | 0.3 (0.3) | 0.1 (0.3) | 0.1 (0.1) | 0.3 (0.3) | 0.4 (0.3) | 0.2 (0.3) | 0.4 (0.3) | 0.2 (0.2) | 0.5 (0.3) | < 0.001 |
| EQ-VAS | 40.7 (20.2) | 25.5 (13.0) | 31.4 (19.7) | 42.6 (21.1) | 48.1 (17.8) | 36.6 (12.6) | 44.7 (16.6) | 42.0 (18.2) | 55.8 (17.8) | < 0.001 |
| SG: subgroup; EuroQol: European Quality of Life instrument; ADL: activities of daily living; SD: standard deviation; LiSat-11: Life Satisfaction Questionnaire; ANOVA: analysis of variance; EQ-5D: European Quality of Life instrument – five dimensions; EQ-VAS: European Quality of Life instrument – 100 point health scale; SF-36: Short form 36 health survey; ns: not significant. |
Multivariate correlation analysis among the subgroups
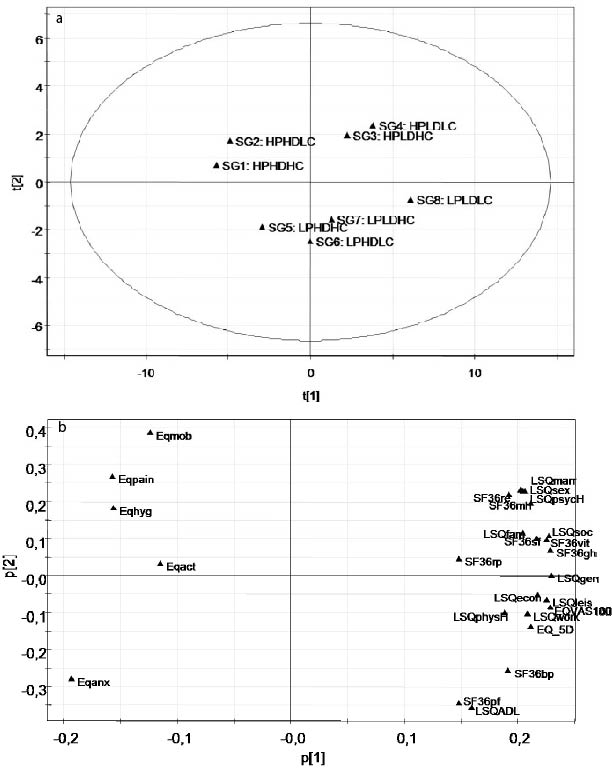
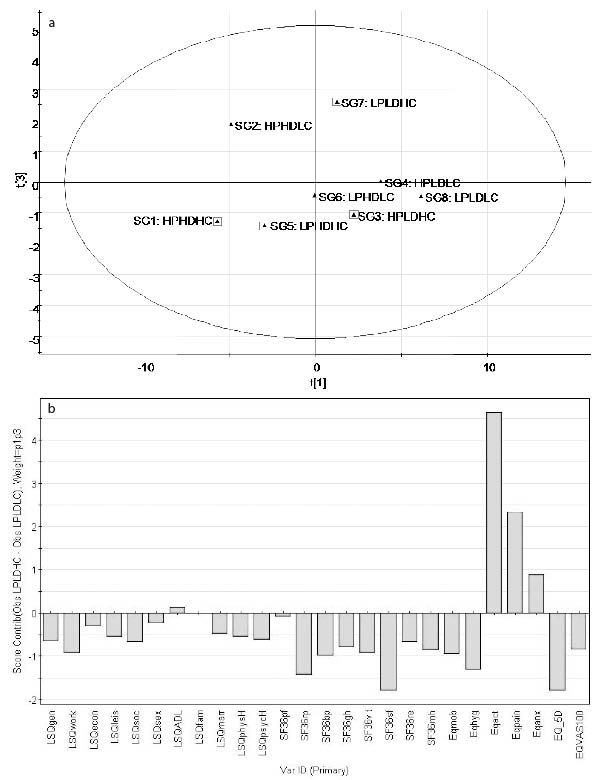
For each of the 8 subgroups (SG1–8), the mean values of LiSAT-11, EuroQol, and SF-36 were used in a PCA analysis (Fig. 2). The calculated PCA model (R2cummulated = 90%) is based on 3 principal components (component 1: R2 = 0.68, Eigen value = 5.4; component 2: R2 = 0.14, Eigen value = 1.1; component 3: R2 = 0.08, Eigen value = 0.7); only the first component was significant. Fig. 2 multivariately and graphically summarizes Table I at group level; the score plot shows the interrelations between the subgroups (Fig. 2a) and the loading plot (Fig. 2b) shows the relationships between the items of LiSAT-11, EuroQol and SF36. Subgroups clustered together share similar characteristics, whereas the characteristics of subgroups far from each other differ (Fig. 2a); e.g. SG2 (i.e. HP/HD/LC) differed little from SG1 (HP/HD/HC) with respect to LiSAT-11, EuroQol, and SF-36. According to the loading plot (Fig. 2b), it is obvious that high loadings on the first component are associated with a positive situation with respect to life satisfaction and health and negative values with a negative situation. Since the 2 plots are complementary, e.g. subgroups located far to the right horizontally in the score plot (Fig. 2a) have high values on the variables far to the right in the loading plot (Fig. 2b). As expected from Table I, SG1 (i.e. HP/HD/HC) has low (negative) values with respect to life satisfaction and is located to the left in Fig. 2a, whereas SG8 (i.e. LP/LD/LC) with a good situation is located mostly to the right. The following multivariate ranking order (from low to high health and life satisfaction) can be revealed from Fig. 2a and 2b: SG1, SG2, SG5, SG6, SG7, SG3, SG4, and SG8.
Fig. 2. (a) The principal component analysis score plot illustrates the relationships between the subgroups according to the scores of first component ([t1]) vs the scores of second component ([t2]). The complementary loading plot (b) shows the relationships between the items of LISAT-11, EuroQol and SF36. For detailed interpretation see Results. For an explanation of abbreviations, see text.
Multivariate differences between the subgroups
The analysis can be refined further, including the second and third components. The results below show that different patterns of variables are discerned according to the different constellations of pain, depression, and catastrophizing.
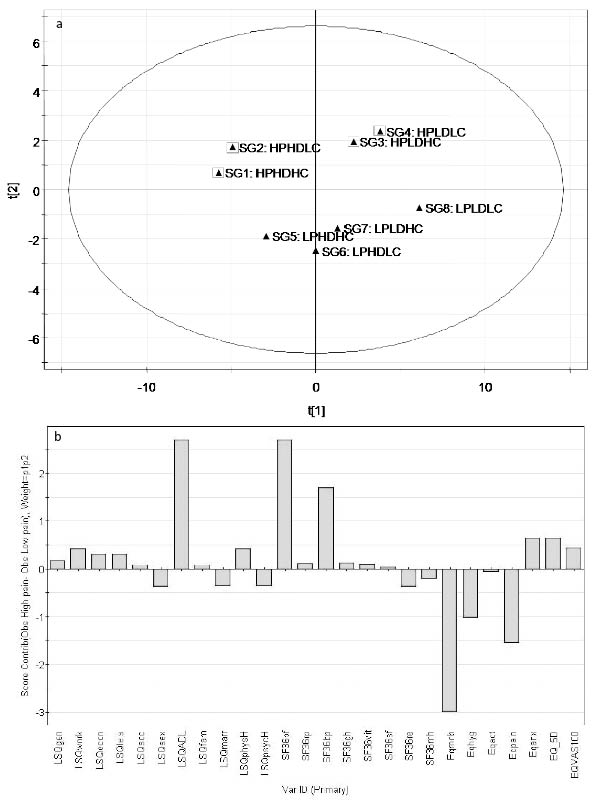
High vs low pain intensity. The clustering of all groups reporting high pain (marked with squares in Fig. 3a) was compared with all groups reporting low pain. The separating variable pattern is presented in Fig. 3b. Thus subgroups with high pain vs subgroups with low pain differed mainly in functional variables relating to aspects such as ADL, physical functioning, and mobility (i.e. high positive or negative bars in Fig. 3b).
Fig. 3. (a) Marked principal component analysis plots highlighting common features (scores of first ([t1]) vs scores of second component ([t2])). In this plot, subgroups with high pain (denoted with square symbols) vs low pain are shown. The complementary loading plot (Fig. 2b) shows the relationships between the items of LISAT-11, EuroQol and SF36. (b) Corresponding contribution plot. High absolute bars indicate prominent differences between subgroups with high pain vs subgroups with low pain. For detailed interpretation see Results. For explanation of abbreviations, see text.
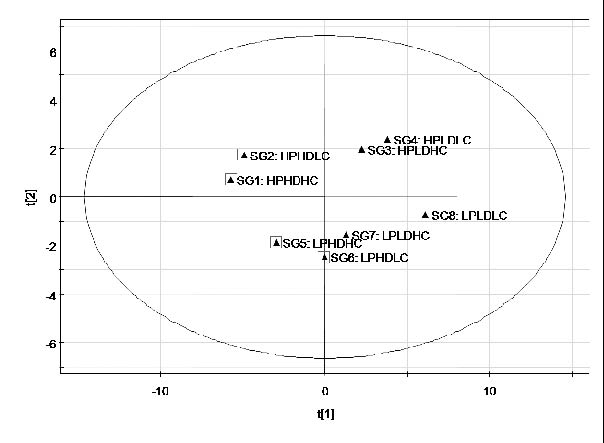
High vs low depression. When separating all groups scoring high on depression scales (marked with squares in Fig. 4) vs all groups scoring low, subgroups with high depression are all located farthest to the left, indicating the worst perceived health and quality of life. The contribution plot indicated that items concerning psychological, well-being, vitality, emotional, and participation aspects were all important and differed between subgroups with high and low depression (data not shown).
Fig. 4. Marked principal component analysis plots highlighting common features (scores of first component ([t1]) vs scores of second component ([t2])). In this plot, subgroups with high depression (denoted with square symbols) vs low depression are shown. The complementary loading plot (Fig. 2b) shows the relationships between the items of LISAT-11, EuroQol and SF36. For detailed interpretation see Results. For explanation of abbreviations, see text.
High vs low catastrophizing. Finally, when comparing subgroups scoring high (marked with squares in Fig. 5a) or low on catastrophizing, a more subtle variable profile appeared (data not shown). The third component captured parts of a new informative structured variance (Fig. 5a). This third component separated the LP/LD/HC subgroup from all other subgroups, but particularly the remaining subgroups with high catastrophizing. The impact of catastrophizing appears to be most important when both pain and depression are low. If either pain or depression is high, the catastrophizing parameters seem to have a minor impact on perceived health and well-being. When comparing the subgroups LP/LD/LC and LP/LD/HC, the resulting variable pattern indicates that 2 items, activity and pain, were most important (Fig. 5b).
Fig. 5. (a) Marked principal component analysis plots highlighting common features (scores of first ([t1]) vs scores of third component ([t3])). In this plot, subgroups with high catastrophizing (denoted with square symbols) vs low catastrophizing are shown. (b) Separating variable profile (contribution plot) between LP/LD/LC and LP/LD/HC. High absolute bars indicate prominent differences between LP/LD/LC and LP/LD/HC. For detailed interpretation see Results. For explanation of abbreviations, see text.
Discussion
Major findings
The 8 subgroups – based on dichotomizing pain, depression, and catastrophizing – showed multivariate differences with respect to health and quality of life. The results indicate that, in a clinical setting, it is important to assess every patient individually in detail with respect to pain intensity, degree of depressive symptoms, and catastrophizing in order to determine specific treatment or rehabilitation strategies.
Distribution of the 8 subgroups
The distribution of subgroups is interesting; 50% of the patients belonged to the extreme groups LP/LD/LC (SG8) and HP/HD/HC (SG1). Additionally, relatively large intermediate groups were found with separate characteristics and, furthermore, it was possible to investigate the multivariate relationships and discriminate between them. Our study group is a selected group of chronic pain patients with WAD who were referred to a university hospital, i.e. patients who have had severe pain problems for a long time. Time, and interaction between the 3 factors pain, depression, and catastrophizing, may explain the large subgroup HP/HD/HC (i.e. SG1); however, the group of patients with chronic WAD might be heterogeneous and some patients could have been referred earlier in the process of pain chronification according to local and national recommendations. Previous studies have shown that duration is an important aspect of the relationship between psychological components and function in chronic pain (31, 32). Furthermore, in a prospective study a strong interrelation was found between negative affect, expectations, and beliefs (33). The relatively large subgroup LP/LD/LC (i.e. SG8) consists of patients scoring low according to the 3 symptoms, which we believe indicates a less developed sensitivity towards a worsened situation. As this is a cross-sectional study it was not possible to study changes over time, and we do not have valid information about the duration of pain for each patient.
Interrelationships and characteristics of the 8 subgroups
Depression (24, 25), catastrophizing (16), and possibly high pain (9) per se and their interactions contribute to low quality of life and low levels of perceived health. Therefore, these factors low (i.e. LP/LD/LC (i.e. SG8)) should, as in the present study, indicate a better situation than all factors high (HP/HD/HC; i.e. SG1) (Fig. 2a and b).
Out of the factors pain, depression, and catastrophizing, depression seems to be the most important with respect to poor outcome for quality of life and health measures; i.e. the subgroups with high depression (i.e. SG1, SG2, and to some extent SG5 and SG6) are located farthest to the left in Fig. 2a and show the worst situation relatively independent of the scores on pain intensity and catastrophizing (Fig. 2 b). To our knowledge, there are no previous studies that address the relative importance of depression vs pain and catastrophizing with respect to health and quality of life in chronic pain patients. The subgroups with high depression differ from subgroups with low depression mostly according to items of health and quality of life concerning psychological, well-being, vitality, and emotional, as well as participation, aspects. Sinikallio et al. (34), in a study of patients with lumbar spinal stenosis and pain, showed that depression correlated with restrictions of daily living, a finding that contradicts our results. Our results, however, agree with Pincus et al.’s (35) finding that depression corresponds to a more general reduced activity and social withdrawal.
Subgroups with high pain intensity differ from those with low pain intensity mainly in quality of life variables referring to physical functioning (ADL, mobility, and physical functioning) (Fig. 3b). The processes leading to impaired physical functioning in patients experiencing high pain are widely discussed. It is not possible from the present study to cast any further light on this issue. However, from a clinical point of view, it might open up a possibility to enhance the quality of life for patients with high pain by trying to increase the patient’s physical activity level.
In this study, the catastrophizing factor does not show a clear impact on quality of life and health, in contrast to the results of other studies (13, 16). Our results indicate that adding high catastrophizing to low pain and low depression worsens the situation considerably; thus the greatest impact occurs when comparing the subgroups LP/LD/LC (SG8) and LP/LD/HC (SG7), and the important separating items with respect to health and quality of life were activity and pain (Fig. 5b). This might support the catastrophizing/fear avoidance model (36), which perceives catastrophizing as a prerequisite and elemental factor in the acquisition of avoidance behaviour. However, this model has been questioned and other models are proposed (35). In a study of the outcome of treatment for low back pain, it was shown that treatment elements not deliberately targeting cognitive factors can reduce catastrophizing and mediate improvement of functioning (21). Thus, enhancing physical activity might reduce pain catastrophizing and, according to our study, put the patient in a much better situation with respect to perceived health and quality of life.
According to the diathesis-stress model (22) and the work of Pincus & Morley (28), it is better to characterize depression in chronic pain as “affective distress” incorporating wider emotions such as anger, frustration, fear and sadness. The diathesis is conceptualized as pre-existing characteristics of the individual before the onset of pain, which are activated by the stress of the chronic condition and lead to depression. In a prospective study of patients with rheumatoid arthritis it was found that patients with high pain catastrophizing at baseline showed increases in depression 6 months later (37). Our results indicate that catastrophizing may be looked upon as a diathesis because its presence in patients with low pain and low depression indicates much lower quality of life and, if there is a temporal correlation in our subgroups, it may lead to depression.
Clinical implications
The present and recent results (9) indicate that, from a therapeutic point of view, it is of great importance to assess the degree of and interrelationships between pain, depression, and catastrophizing before planning treatment and rehabilitation. Our results suggest that treating existing depression can be an important way to achieve better perceived quality of life and health. Furthermore, it would be more efficient, with respect to quality of life and health, to influence catastrophizing in patients with lower pain and depression than in patients with higher pain and depression. Similar conclusions were drawn by Sullivan et al. (38) in a study of depression and cognitive-behavioural interventions for work disability. They suggested that intervention techniques designed to reduce catastrophic thinking and modify individual’s appraisals of their level of disability might be important components of the successful treatment of mildly depressed pain patients. Overall, their study pointed to the important role of depressive symptoms in the rehabilitation and that individuals with more severe depressive symptoms might require treatment for longer periods than in typical rehabilitation programmes. Alternatively, they suggested initiating treatment for depression before enrolling in such a programme. Furthermore, the combination of antidepressant medication and cognitive behavioural therapy is more efficient than cognitive behavioural therapy alone among individuals who score relatively highly in depressive symptoms (39).
Methodological considerations
The cross-sectional study design reduces the possibility of making any statement about temporal processes and causality. Therefore, there is a need for prospective studies. In addition, this group had been referred to a university hospital, which means that the patients had severe pain problems for a long time. Hence, future studies ought to investigate patients at an earlier stage and/or within primary healthcare.
The median split is a common method, for instance when using dummy variables in regressions. Our method, of creating the subgroups using dichotomizing based on medians, has disadvantages, for instance for subjects near the median. It would have been preferable to use clinically motivated cut-offs, but these do not exist for pain intensity and catastrophizing. We suggest that our results are confirmed using e.g. cluster analysis. However, then a substantially larger sample of patients is needed in order to achieve sufficiently large subgroups. The optimal number of subgroups to determine in the cluster analysis is another aspect that must be taken into careful consideration (i.e. chosen by the researcher).
Some considerations about the statistical significance of the PCA analysis are necessary. The first component is indeed the most important, as it explains a large amount of the variance; the first component explains 68% of the variation, while corresponding figures for the second and third components were 14% and 8%, respectively. The second and third components are not significant in a statistical/mathematical sense according to the algorithm used in SIMCA-P+. However, these components still have noteworthy Eigen values (1.1 and 0.7). In the SPSS package, Eigen values above 1.0 are considered significant rather than non-trivial. Therefore, it could be argued that these components still describe important structures in the variations, although caution should be used when drawing conclusions about these findings. Instead they could be used as an indication or a trend, pointing to areas or relationships that need to be studied further.
CONCLUSION
Based on dichotomizing of 3 factors: the degree of pain intensity, depression, and catastrophizing, we identified subgroups with specific characteristics according to perceived health and quality of life. The degree of depression appears to be the most important influencing factor. From a clinical point of view, our findings indicate the importance of assessing each individual in detail with respect to intensities of pain, depression, and catastrophizing when planning treatment and rehabilitation.
References
1. Schlenk EA, Erlen JA, Dunbar-Jacob J, McDowell J, Engberg S, Sereika SM, et al. Health-related quality of life in chronic disorders: a comparison across studies using the MOS SF-36. Qual Life Res 1998; 7: 57–65.
2. Lame IE, Peters ML, Vlaeyen JW, Kleef M, Patijn J. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. Eur J Pain 2005; 9: 15–24.
3. Becker N, Bondegaard Thomsen A, Olsen AK, Sjogren P, Bech P, Eriksen J. Pain epidemiology and health related quality of life in chronic non-malignant pain patients referred to a Danish multidisciplinary pain center. Pain 1997; 73: 393–400.
4. Soderlund A, Lindberg P. Long-term functional and psychological problems in whiplash associated disorders. Review. Int J Rehabil Res 1999; 22: 77–84.
5. Sterner Y, Bränholm I-B, Nyberg V, Elert J, Gerdle B. Aspects of impairments, disabilities and life satisfaction in patients with chronic whiplash associated disorders. J Whiplash & Related Disorders 2002; 1: 39–62.
6. Adams N, Poole H, Richardson C. Psychological approaches to chronic pain management: part 1. J Clin Nurs 2006; 15: 290–300.
7. Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Physical and psychological factors predict outcome following whiplash injury. Pain 2005; 114: 141–148.
8. Berglund A, Bodin L, Jensen I, Wiklund A, Alfredsson L. The influence of prognostic factors on neck pain intensity, disability, anxiety and depression over a 2-year period in subjects with acute whiplash injury. Pain 2006; 125: 244–256.
9. Peolsson M, Gerdle B. Coping in patients with chronic whiplash-associated disorders: a descriptive study. J Rehabil Med 2004; 36: 28–35.
10. Sullivan MJL, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995; 7: 524–532.
11. Geisser ME, Robinson ME, Keefe FJ, Weiner ML. Catastrophizing, depression and the sensory, affective and evaluative aspects of chronic pain. Pain 1994; 59: 79–83
12. Martin MY, Bradley LA, Alexander RW, Alarcon GS, Triana-Alexander M, Aaron LA, et al. Coping strategies predict disability in patients with primary fibromyalgia. Pain 1996; 68: 45–53.
13. Lefebvre JC, Lester N, Keefe FJ. Pain in young adults. II: the use and perceived effectiveness of pain-coping strategies. Clin J Pain 1995; 11: 36–44.
14. Geisser ME, Robinson ME, Henson CD. The Coping Strategies Questionnaire and chronic pain adjustment: a conceptual and empirical reanalysis. Clin J Pain 1994; 10: 98–106.
15. Hill A, Niven CA, Knussen C. The role of coping in adjustment to phantom limb pain. Pain 1995; 62: 79–86.
16. Lame IE, Peters ML, Vlaeyen JW, Kleef M, Patijn J. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. Eur J Pain 2005; 9: 15–24.
17. Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001; 17: 52–64.
18. Tripp DA, Stanish WD, Reardon G, Coady C, Sullivan MJ. Comparing postoperative pain experiences of the adolescent and adult athlete after anterior cruciate ligament surgery. J Athl Train 2003; 38: 154–157.
19. Edwards RR, Haythornthwaite JA, Sullivan MJ, Fillingim RB. Catastrophizing as a mediator of sex differences in pain: differential effects for daily pain versus laboratory-induced pain. Pain 2004; 111: 335–341.
20. Jensen MP, Turner JA, Romano JM. Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J Consult Clin Psychol 2001; 69: 655–662.
21. Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain 2006; 7: 261–271.
22. Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: a diathesis-stress framework. Psychol Bull 1996; 119: 95–100.
23. Carroll LJ, Cassidy JD, Cote P. Frequency, timing, and course of depressive symptomatology after whiplash. Spine 2006; 31: E551–E556.
24. Haythornthwaite JA, Sieber WJ, Kerns RD. Depression and the chronic pain experience. Pain 1991; 46: 177–184.
25. Weickgenant AL, Slater MA, Patterson TL, Atkinson JH, Grant I, Garfin SR. Coping activities in chronic low back pain: relationship with depression. Pain 1993; 53: 95–103.
26. Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain 1997; 13: 116–137.
27. Pincus T, Pearce S, McClelland A, Isenberg D. Endorsement and memory bias of self-referential pain stimuli in depressed pain patients. Br J Clin Psychol 1995; 34: 267–277.
28. Pincus T, Morley S. Cognitive-processing bias in chronic pain: a review and integration. Review. Psychol Bull 2001; 127: 599–617.
29. Boersma K, Linton SJ. Psychological processes underlying the development of a chronic pain problem: a prospective study of the relationship between profiles of psychological variables in the fear-avoidance model and disability. Clin J Pain 2006; 22: 160–166.
30. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987; 18: 233–237.
31. Boersma K, Linton SJ. How does persistent pain develop? An analysis of the relationship between psychological variables, pain and function across stages of chronicity. Behav Res Ther 2005; 43: 1495–1507.
32. Sullivan MJL, Sullivan ME, Adams HM. Stage of chronicity and cognitive correlates of pain-related disability. Cogn Behav Ther 2002; 31: 111–118.
33. Boersma K, Linton SJ. Expectancy, fear and pain in the prediction of chronic pain and disability: a prospective analysis. Eur J Pain 2006; 10: 551–557.
34. Sinikallio S, Aalto T, Airaksinen O, Herno A, Kroger H, Savolainen S, et al. Depression and associated factors in patients with lumbar spinal stenosis. Disabil Rehabil 2006; 28: 415–422.
35. Pincus T, Vogel S, Burton AK, Santos R, Field AP. Fear avoidance and prognosis in back pain: A systematic review and synthesis of current evidence. Arthritis Rheum 2006; 54: 3999–4010.
36. Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007; 30: 77-94.
37. Keefe FJ, Brown GK, Wallston KA, Caldwell DS. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain 1989; 37: 52–56.
38. Sullivan MJ, Adams H, Thibault P, Corbiere M, Stanish WD. Initial depression severity and the trajectory of recovery following cognitive-behavioral intervention for work disability. J Occup Rehabil 2006; 16: 63–74.
39. Thase ME, Greenhouse JB, Frank E, Reynolds CF 3rd, Pilkonis PA, Hurley K, et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry 1997; 54: 1009–1015.