OBJECTIVE: Interest in exploring the positive emotional health of adults has increased. The current study investigated the positive emotion of adults with stroke at discharge from in-patient medical rehabilitation and 3 months post-discharge.
DESIGN: A longitudinal study in which information was collected during in-patient medical rehabilitation stay and 3 months post-discharge.
SUBJECTS: The study included 856 persons with stroke aged 55 years or older.
RESULTS: Mean age for the sample was 72.5 years, 78.7% of subjects were non-Hispanic white and 51.9% were women. Mean length of hospital stay was 20.2 days. More than one-third of patients reported higher positive emotion over the 3-month follow-up, while 29.7% reported lower positive emotion. In addition to discharge positive emotion, 4 factors, including depression, level of education and motor and cognition functional status score, significantly predicted lower depression at 3-month follow-up.
CONCLUSION: A large percentage of adults reported high positive emotion in the initial months following a stroke. This finding adds to work on stroke recovery and indicates the emotional resilience of adults when faced with a health challenge. Understanding the role of positive emotion in persons living with stroke may provide insight into long-term recovery.
Key words: positive emotion, ethnic groups, cerebrovascular accident, recovery of function.
J Rehabil Med 2008; 40: 477–481
Correspondence address: Glenn V. Ostir, UTMB, 301 University Blvd., Galveston, TX 77555-0460, USA. E-mail: gostir@utmb.edu
Submitted September 27, 2007; accepted January 29, 2008
INTRODUCTION
Compelling evidence points to the importance of positive emotion in the face of a health challenge (1–3). Individual reports of positive emotion have been reported under the most difficult and stressful of circumstances and may, in part, be necessary for recovery and survival (4–6). In a 15-year prospective study of women with breast cancer (stages I and II), Greer et al. (7), found those with a fighting spirit reported the best outcomes compared with those who viewed the situation as hopeless. Among patients with hip fracture, those who reported good emotional health were 3 times more likely than depressed patients to achieve independence in walking, 9 times more likely to return to pre-fracture levels of physical functioning, and 9 times more likely to reach the highest quartile of overall physical function (8). Patients with HIV with high positive emotion have demonstrated slower immune decline, later symptom onset, and longer survival times (9, 10). Fredrickson & Levenson (11) have also shown positive emotion to reduce reports of depression following a stressful event.
A goal of the current investigation was to assess the positive emotion of adults aged 55 years or older following a stroke at 2 time-points, including discharge from in-patient medical rehabilitation and approximately 3 months later. Annually, an estimated 10 million individuals worldwide survive a stroke (12), yet little is known about the positive emotional experiences of these individuals. A second goal of the investigation was to explore sociodemographic characteristics and measures of health and functional status associated with positive emotion. An association between these factors and positive emotion would add to studies of recovery and resilience and may open new directions for clinical and rehabilitation care delivery and research. Such new directions are of importance for stroke survivors who hope to reacquire functional abilities and independence.
Methods
Source of data
Data came from the Stroke Recovery in Undeserved Populations (SRUP) database, an ongoing observational follow-up study of persons with stroke who received in-patient medical rehabilitation services in 2005–06. A total of 20 facilities were invited to participate and were sent information describing the goals of the study. Of these, 16 agreed to participate in the study. Five facilities located in the Gulf coast region and affected by hurricanes (2005) were subsequently removed from the study. The 11 remaining facilities were located across diverse regions of the country, including: California, Florida, Iowa, Illinois, Kentucky, New Jersey, New York (2), Texas (2) and Washington DC. Number of operating beds ranged from 12 to 155 (median bed size = 78); all 11 facilities were accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO); and all but one facility was accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF).
Data collection
Sociodemographic characteristics and clinical measures of health and functional status were collected at 2 time-points: within 72 h of discharge from in-patient medical rehabilitation facility, and approximately 3 months post-discharge (mean 93 days, standard deviation (SD) 20.7). In-hospital interviews were performed by nursing staff at the in-patient medical rehabilitation facility. Follow-up information was collected by trained nurse researchers by telephone interview among persons living at home at the 3-month follow-up interview. In-hospital and follow-up interviews were conducted in Spanish or English.
Study population
Individuals eligible for inclusion into the SRUP study had to be admitted to an in-patient medical rehabilitation facility with a diagnosis of stroke (ICD-9 codes 436–439) and aged 55 years or older of either gender. Patients were screened for cognitive appropriateness by nursing staff at the rehabilitation facility, on their ability to respond to basic questions about orientation to person, place and time. A total of 1006, non-proxy and cognitively appropriate patients (798 non-Hispanic whites, 150 African Americans, and 58 Hispanics) were interviewed within 72 h of discharge from in-patient medical rehabilitation facility.
The current study included 856 patients with stroke who had complete information on positive emotion at discharge and 3-month follow-up interview. Of the original 1006 patients, 29 died, 42 refused follow-up interview, and 28 could not be contacted. An additional 51 patients were removed from the analysis because of missing sociodemographic and health-related measures. To evaluate the potential bias of those lost to follow-up, we tested for significant differences across various sociodemographic and health-related measures. After reviewing these measures we did not identify any potential confounders with known or suspected associations with positive emotion. Central and local ethics committee approval was sought and obtained. Consent was obtained in-person at the time of the discharge interview.
Outcome measure
Positive emotion. A 4-item positive emotion summary score was created from a 20-item Center for Epidemiologic Studies – Depression (CES-D) scale (13, 14). The 4 positive items included: “I felt that I was just as good as other people”, “I felt hopeful about the future”, “I was happy”, and “I enjoyed life” (14). Responses were scored on a 4-point scale and ranged from 0 (rarely or none of the time) to 3 (most of the time). Summing the responses from the 4-items created a positive emotion summary score at 2 time points including discharge and 3-month follow-up. A positive emotion change score was computed as the difference between 3-month follow-up and discharge, where higher scores indicate higher positive emotion. The 4 positive emotion items have shown high internal consistency (alpha = 0.80), and a weak correlation (r = –0.26) with the 16 negative items on the CES-D (15).
Covariates
Sociodemographic, health-related and functional status measures were included as covariates in the statistical models described below. Sociodemographic measures included age (≥ 55 years), gender, marital status (married vs unmarried), ethnicity (non-Hispanic white, non-Hispanic black and Hispanic) and years of schooling completed.
Health-related measures included co-morbidities (heart attack, diabetes, arthritis, kidney disease and cancer), length of hospital stay, stroke type (ischemic, hemorrhagic or other), body involvement (right or left, bilateral or no paresis) and depressive symptoms. Length of stay was calculated in days from in-patient admission to discharge. Depressive symptoms were calculated by summing the 16 remaining items from the CES-D scale (range 0–48), where higher scores indicated higher depressive symptoms.
Functional status was assessed by the Inpatient Rehabilitation Facilities-Patient Assessment Instrument (IRF-PAI). The IRF-PAI is a 54-item instrument used to assign medical rehabilitation inpatients to a case-mix group. The case-mix group determines prospective reimbursement for medical rehabilitation by the Centers for Medicare and Medicaid Services (16–18). The functional status items in the IRF-PAI are from the Functional Independence Measure (FIMTM), a standardized measure including 18 items covering 6 domains: self-care, sphincter control, transfer, locomotion, communication, and social cognition. All 18 items are scored into 1 of 7 levels of function, ranging from complete dependence (level 1) to complete independence (level 7). Total FIM ratings have a potential range of 18 to 126, where higher scores indicate greater functional independence. Total FIM ratings can be grouped into Motor and Cognition ratings. Motor ratings contain self-care, sphincter control, mobility, and locomotion items, and Cognition ratings contain communication and social cognition items. Ratings for the Motor subscale ranges from 9 to 91, and for the Cognition subscale from 5 to 35. The reliability, validity, and responsiveness of the FIM instrument have been widely investigated (19–20). The reliability (intraclass correlation coefficient) of the total FIM and of its domains has consistently been found to be > 0.85 (19–21).
Statistical analysis
Descriptive statistics were reported as means (and SD) for continuous measures and as percentages for categorical measures. To compare associations for discharge sociodemographic, health-related and functional status measures on follow-up positive emotion, 3 generalized linear regression models were computed. The first model included sociodemographic measures (age, sex, marital status, and years of education) as predictor variables. The second model added health-related measures (type of stroke, main area of body involvement, length of hospital stay (LOS), co-morbidities and depressive symptoms) and Motor FIM score. The third model included sociodemographic and health-related measures and Cognition FIM score.
A fourth model examined associations between positive emotion change score (from discharge to 3-month follow-up) and discharge sociodemographic and health-related measures and Motor and Cognition FIM scores. For all models, testing was 2-sided using an alpha of 0.05. Model assumptions for the 4 regression models were tested and met. All analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, NC, USA).
Results
A total of 856 patients with complete information at discharge and 3-month follow-up interview were included in the study. The most prevalent type of stroke was ischemic (75.2%), followed by hemorrhagic (15.3%) and other stroke (9.5%). A high percentage of patients had left (42.2%) or right body involvement (39.6%). A small percentage had bilateral body involvement (3.3%) and 14.9% had no paresis. Most patients were admitted from home (97.3%) and discharged to home (74.8%). Of those not discharged directly to home (n = 195), the majority (91.2%) were placed in a skilled nursing facility, an acute unit at another facility or in a subacute setting. The average LOS was 20.2 (SD 10.1) days and did not significantly differ by age, gender or ethnicity.
Table I shows sociodemographic, health-related and functional status characteristics of the sample at discharge from in-patient medical rehabilitation facility. A majority of the patients were women (51.9%), non-Hispanic white (78.7%) and aged 55–74 years (52.8%). Most had a high school education or more (78.5%) and more than half were currently married (53.3%). Most had one or more co-morbidities (76.2%) and about a third reported high depressive symptoms (32.5%). Average Motor and Cognition FIM scores were 56.4 (SD 18.1) and 24.8 (SD 7.4), respectively.
| Table I. Sociodemographic and health-related characteristics of patients with stroke at discharge from in-patient medical rehabilitation facility (n = 856) |
| Patient characteristic | Total sample, % |
| Age (years) 55–64 65–74 75–84 ≥ 85 | 23.1 29.7 35.6 11.6 |
| Gender Men Women | 48.1 51.9 |
| Ethnicity Non-Hispanic white Non-Hispanic black Hispanic | 78.7 15.7 5.6 |
| Marital status Unmarried Married | 46.7 53.3 |
| Education (years) < 12 ≥ 12 | 21.5 78.5 |
| Co-morbidities 0 1 ≥ 2 | 23.8 44.2 32.0 |
| Depressive symptoms < 16 ≥ 16 | 30.7 69.3 |
| Motor FIM (mean, SD) | 56.4 (18.1) |
| Cognition FIM (mean, SD) | 24.8 (7.4) |
| FIM: Functional Independence Measure; SD: standard deviation. |
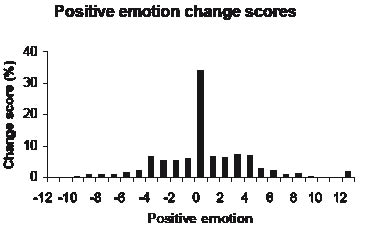
Scores on the positive emotion summary scale improved marginally from discharge (median = 10, interquartile range 7–12) to 3-month follow-up (median = 11.0, interquartile range 8–12) interview. No significant differences on positive emotion score were found for gender, age and ethnic group, or type of stroke. Fig. 1 shows positive emotion change scores from discharge to 3-month follow-up for the overall sample. Approximately one-third of patients (34.7%) reported no change in their positive emotion score, with 35.6% reporting higher scores and 29.7% reporting lower scores over the 3-month follow-up. Of those who reported no change (n = 297), 79.1% recorded the highest positive emotion score of 12 at discharge and 3-month follow-up.
Fig. 1. Positive emotion change scores from discharge to 3-month follow-up.
To examine independent associations between discharge sociodemographic, health-related and functional status measures and follow-up positive emotion, 3 generalized linear regression models were tested (Table II). For each model unstandardized parameter estimates (b) and standard error (SE) were presented, p < 0.05 was considered significant. Model 1 included sociodemographic measures and showed that higher level of education (b = 0.10, SE 0.03) and discharge positive emotion (b = 0.45, SE 0.03) were significantly associated with higher positive emotion at follow-up. Model 2 added health-related measures and Motor FIM score to the analysis. Significant associations with follow-up positive emotion included Motor FIM score (b = 0.03, SE 0.006) and depressive symptoms (b = –0.07, SE 0.01). Higher education (b = 0.08, SE 0.03) and discharge positive emotion (b = 0.29, SE.04) also remained significant predictors of follow-up positive emotion. LOS, type of stroke, body involvement and number of co-morbidities was not significantly associated with follow-up positive emotion. Model 3, included Cognition FIM score, in addition to sociodemographic and health-related measures. The findings showed that higher Cognition FIM score (b = 0.04, SE 0.01) at discharge was significantly associated with higher follow-up positive emotion.
| Table II. Sociodemographic and health-related characteristics at discharge associated with positive emotion at 3-month follow-up for patients with stroke (n = 856) |
| Discharge characteristic | Model 1 | Model 2 | Model 3 |
| b | SE | p | b | SE | p | b | SE | p |
| Age (continuous) | –0.06 | (0.10) | 0.54 | –0.01 | (0.10) | 0.95 | –0.06 | (0.10) | 0.53 |
| Men (vs women) | 0.06 | (0.20) | 0.75 | –0.01 | (0.20) | 0.94 | 0.04 | (0.25) | 0.86 |
| Non-Hispanic black (vs non-Hispanic white) | –0.12 | (0.27) | 0.65 | –0.18 | (0.26) | 0.49 | –0.26 | (0.26) | 0.31 |
| Hispanic (vs non-Hispanic white) | –0.62 | (0.44) | 0.16 | –0.65 | (0.42) | 0.12 | –0.75 | (0.42) | 0.07 |
| Married (vs unmarried) | 0.03 | (0.20) | 0.87 | 0.15 | (0.20) | 0.46 | 0.12 | (0.20) | 0.54 |
| Education (continuous) | 0.10 | (0.03) | 0.003 | 0.08 | (0.03) | 0.008 | 0.08 | (0.03) | 0.008 |
| Stroke type | | | | 0.10 | (0.19) | 0.61 | 0.11 | (0.20) | 0.95 |
| Body involvement | | | | 0.13 | (0.09) | 0.29 | 0.16 | (0.10) | 0.10 |
| LOS (continuous) | | | | 0.01 | (0.01) | 0.11 | 0.01 | (0.01) | 0.84 |
| Motor FIM (continuous) | | | | 0.03 | (0.006) | 0.0001 | | | |
| Cognition FIM (continuous) | | | | | | | 0.04 | (0.01) | 0.002 |
| Depression (continuous) | | | | –0.07 | (0.01) | 0.0001 | –0.08 | (0.01) | 0.0001 |
| Co-morbidities (0–5)* | | | | –0.02 | (0.11) | 0.83 | –0.06 | (0.11) | 0.57 |
| Positive emotion (continuous) | 0.45 | (0.03) | 0.0001 | 0.29 | (0.04) | 0.0001 | 0.30 | (0.04) | 0.0001 |
| R2 | 0.21 | | | 0.28 | | | 0.26 | | |
| *Summary comorbidity index that included: heart attack, diabetes, arthritis, kidney disease and cancer. b: unstandardized parameter estimates; SE: standard error; FIM: Functional Independence Measure; LOS: length of hospital stay. |
In a fourth model, predictors of positive emotion change score were examined. These predictors included discharge sociodemographic and health-related measures and Motor and Cognition FIM score. The findings showed higher education (b = 0.08, SE 0.03, p = 0.006), depressive symptoms (b = –0.07, SE 0.01, p = 0.0001), Motor FIM score (b = 0.04, SE 0.01, p = 0.0001), and discharge positive emotion (b = 0.71, SE 0.04, p = 0.0001) were significantly associated with higher positive emotion change score.
Discussion
The current study examined the positive emotional health of patients following stroke, a previously unexplored area of research. Overall, we found that patients can experience positive emotion in the initial months following their stroke event and that the level of positive emotion does not significantly differ by age, gender or ethnicity. We further observed that positive emotion is a dynamic process. More than one-third of our sample reported higher positive emotion change scores between discharge and at 3-month follow-up interview, just under one-third reported lower change scores and about one-third reported no change. Of those who reported no change, 79.1% recorded the highest positive emotion score of 12 at both the discharge and at the follow-up interview. This suggests a ceiling effect, and may underestimate the actual percentage of those with lower depression change score.
We further showed 3 discharge measures, depressive symptoms, education, and motor and cognitive functional status, were significantly linked to positive emotion at follow-up. It should be noted that discharge positive emotion was also significantly associated with follow-up positive emotion, independent of depression, so was not simply the opposite or absence of this negative measure. This finding adds further support to the independence hypothesis between positive and negative emotions (3, 5, 15, 22).
Assessing the role of positive emotion in the onset, progression and treatment of disease has gained in importance during the last decade. In epidemiologic studies, high positive emotion has been significantly associated with a reduced risk of new onset disease, disability and mobility limitations in adults (15). Clinical data have also shown a link between positive emotion and biological markers. In a sample of middle-aged adults, Steptoe et al. (3) demonstrated an association between higher positive emotion and lower neuroendocrine, inflammatory and cardiovascular activity. Epel et al. (23) showed that individuals who were able to find positive meaning after a traumatic event had more adaptive hormonal responses to subsequent stressors. Although exact mechanisms are not well-known at this point, these studies indicate that positive emotion may play an important role in keeping the body in balance via chemical and neural responses,(1, 24, 25), which may be of added importance among the less healthy.
A number of researchers have hypothesized that, under stressful conditions, when negative emotions such as depression dominate, positive emotions may provide relief and help support coping efforts (4, 26, 27). Although not formally tested in the current study, this idea has potential implications in stroke recovery programs and warrants investigation. That is, understanding the role of positive emotion in limiting the negative effects of depression, for example, may subsequently result in a better understanding of how patients with stroke cope and adapt. The CARF (28) suggests that programs that can demonstrate improved emotional health for their patients after discharge will have a clear advantage in the healthcare marketplace.
As previously mentioned, we identified 2 key measures, functional status and education, in addition to depression, that influence positive emotion. Functional status is an important indicator of recovery and provides clinicians with an objective means to track patient progress during hospital stay and post-discharge. In persons with stroke, Granger et al. (29) observed an inverse gradient of association, where each 1-point increase in FIMTM score decreased the need of assistance by another person to complete basic activities of daily living by about 2.2 min. In persons recovering from an acute medical event, it is likely that functional ability and positive emotion act as a positive feedback loop, where an increase in one measure likely contributes to an increase in the other (30).
The link between education, a component of socioeconomic status, and positive emotion is less clear, but may be mediated by greater psychosocial resources, which include better coping styles, personal control and greater social support (31–33). Using data from 3 national samples, Lachman & Weaver (34) found significant interactions between personal control and education in relation to health and well-being. A challenge for researchers is not only to control for socioeconomic status variables in statistical models, but to combine them in meaningful ways with clinically relevant data, to potentially identify at risk individuals. In the current study we included one component of socioeconomic status, education; however, other unmeasured components at the individual (income, wealth, occupation) and neighborhood level need to be examined, as these may have different meanings in different social groups (e.g. ethnicity or gender) which may affect the conclusions drawn.
Our analysis has some limitations. First, as in all longitudinal studies, biases might have been introduced by missing data or unbalanced representation of the population. A large majority of our sample reported 12 or more years of schooling and most (89.5%) were retired. Second, although our data was collected across diverse geographic regions in the USA, the study participants were not randomly selected and may not be representative of all persons with stroke. Third, because there exists inter-hospital variability in the type and quality of care delivered by in-patient medical rehabilitation facilities in the USA, selected facilities in this study may not adequately reflect the rehabilitation experience at other facilities. Nevertheless, the study did include JACHO- and CARF-accredited facilities, which set guidelines and standards for rehabilitation facilities. Strengths of the investigation include the large representative sample of persons with stroke and diagnosis of stroke using Centers for Medicare and Medicaid Services codes.
In summary, good long-term recovery for persons with stroke requires a healthy mind and body. The importance of collecting information on positive emotion is that it not only assesses what the patient feels about their current health status, but it may also predict whether these individuals seek on-going treatment or therapy, or perhaps more importantly, whether they consider themselves to be successfully coping with their medical event.
Acknowledgements
This research was supported by funding from the National Institutes of Health and the National Institute of Aging for G. Ostir (R01-AG024806 & K01-HD046682), and K. Ottenbacher (K02-AG019736) and National Institutes of Child Health and Human Development for I. Berges (K12HD052023). The authors have no other funding or personal relationships to declare.
References
1. Scheier MF, Matthews KA, Owens JF, Magovern GJ Sr, Lefebvre RC, Abbott RA, et al. Dispositional optimism and recovery from coronary artery bypass surgery: the beneficial effects on physical and psychological well-being. J Pers Soc Psychol 1989; 57: 1024–1040.
2. Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiol Aging 2005; 26 Suppl 1: 108–112.
3. Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc Natl Acad Sci USA 2005; 102: 6508–6512.
4. Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol 2003; 84: 365–376.
5. Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol 2000; 55: 647–654.
6. Frankl VE, editor. Man’s search for meaning : an introduction to logotherapy. New York: Pocket Books; 1963.
7. Greer S, Morris T, Pettingale KW, Haybittle JL. Psychological response to breast cancer and 15-year outcome. Lancet 1990; 335: 49–50.
8. Mossey JM, Mutran E, Knott K, Craik R. Determinants of recovery 12 months after hip fracture: the importance of psychosocial factors. Am J Public Health 1989; 79: 279–286.
9. Reed GM, Kemeny ME, Taylor SE, Wang HY, Visscher BR. Realistic acceptance as a predictor of decreased survival time in gay men with AIDS. Health Psychol 1994; 13: 299–307.
10. Reed GM, Kemeny ME, Taylor SE, Visscher BR. Negative HIV-specific expectancies and AIDS-related bereavement as predictors of symptom onset in asymptomatic HIV-positive gay men. Health Psychol 1999; 18: 354–363.
11. Fredrickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn Emotion 1998; 12: 191–220.
12. WHO. Health topics. World Health Organization. 2007 Available at: URL: http://www.who.int/en/. Accessed on April 18, 2007.
13. Miller TQ, Markides KS, Black SA. The factor structure of the CES-D in two surveys of elderly Mexican Americans. J Gerontol B Psychol Sci Soc Sci 1997; 52B: S259–S269.
14. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401.
15. Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. J Am Geriatr Soc 2000; 48: 473–478.
16. Carter GM, Relles DA, Buchanan JL, Bean T, Donyo T, Rosenfeld L, et al. A classification system for inpatient rehabilitation patients: a review and proposed revisions to the Functional Independence Measure-Function Related Groups. Project memo (Final 31 Aug 95-3 Jul 97). Santa Monica, CA: RAND Corp; 1997, NTIS Order Number PB98–105992.
17. Stineman MG, Hamilton BB, Granger CV, Goin JE, Escarce JJ, Williams SV. Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil 1994; 75: 1277–1283.
18. Stineman MG, Escarce JJ, Goin JE, Hamilton BB, Granger CV, Williams SV. A case-mix classification system for medical rehabilitation. Med Care 1994; 32: 366–379.
19. Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil 1996; 77: 1226–1232.
20. Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fiedler R, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil 1996; 77: 1101–1108.
21. Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Inter-rater reliability of the 7-level functional independence measure (FIM). Scand J Rehabil Med 1994; 26: 115–119.
22. Bradburn NM, Caplovitz D, editors. Reports on happiness: a pilot study of behavior related to mental health. Chicago, Ill: Aldine; 1965.
23. Epel ES, McEwen BS, Ickovics JR. Embodying psychological thriving: physical thriving in response to stress. J Soc Issues 1998; 54: 301–322.
24. Damasio A. Fundamental feelings. Nature 2001; 413: 781.
25. Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol 2004; 86: 320–333.
26. Lazarus RS, editor. Emotion and adaptation. Cambridge, UK: Cambridge University Press; 1991.
27. Moskowitz JT, Folkman S, Acree M. Do positive psychological states shed light on recovery from bereavement? Findings from a 3-year longitudinal study. Death Stud 2003; 27: 471–500.
28. Wilkerson D, Shen D, Duhaime M. Performance Indicators for Rehabilitation Programs. Version 1.1. Tucson, Ariz: The Rehabilitation Accreditation Commission (CARF); 1998.
29. Granger CV, Cotter AC, Hamilton BB, Fiedler RC. Functional assessment scales: a study of persons after stroke. Arch Phys Med Rehabil 1993; 74: 133–138.
30. Ory MG, Williams TF. Rehabilitation: small goals, sustained interventions. Ann Am Acad Pol Soc Sci 1989; 60–71.
31. Bosma H, Van Jaarsveld CH, Tuinstra J, Sanderman R, Ranchor AV, van Eijk JT, et al. Low control beliefs, classical coronary risk factors, and socio-economic differences in heart disease in older persons. Soc Sci Med 2005; 60: 737–745.
32. Kristenson M, Eriksen HR, Sluiter JK, Starke D, Ursin H. Psychobiological mechanisms of socioeconomic differences in health. Soc Sci Med 2004; 58: 1511–1522.
33. Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Ann NY Acad Sci 1999; 896: 210–225.
34. Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol 1998; 74: 763–773.