OBJECTIVE: To investigate the distribution of segmental flexion mobility in the cervico-thoracic spine of men and women with whiplash-associated disorders. The study also assesses the relationship between cervical mobility and segmental flexion mobility, and whether hypomobility in C7–T1 is associated with neck pain and weakness in the hands. Finally, the study investigates the impact of fear of movement/(re)injury and pain intensity on cervical mobility.
Method: The data in this longitudinal study was obtained from a previous trial on 47 patients. Assessments were performed at baseline and 3 and 9 months following randomization using a cervical range of motion instrument, the cervico-thoracic ratio, a Grippit, a visual analogue scale, a Painmatcher, and the Tampa Scale for Kinesiophobia.
RESULTS: Women exhibited hypomobility in C7–T1. There was no significant association between the 2 cervical measurement techniques. The correlation between flexion mobility in C7–T1 and grip strength was weak but significant (r = –0.3) (p < 0.05). There was also a weak but significant negative correlation between total cervical mobility and neck pain intensity. No significant correlation was found between fear of movement/(re)injury and cervical mobility.
CONCLUSION: Women with whiplash-associated disorders seem to exhibit flexion hypomobility in C7–T1. The flexion mobility in C7–T1 was weakly, but significantly, correlated with grip strength, but was not shown to predict neck pain. Neck pain may give rise to restricted range of motion.
Key words: whiplash-associated disorders, cervical range of motion, pain, fear of movement/(re)injury.
J Rehabil Med 2008; 40: 418–425
Correspondence address: Lina Bunketorp Käll, The Sahlgrenska Academy at Göteborg University, Institute of Neuroscience and Physiology, Department of Occupational Therapy, Audiology and Physiotherapy, Box 455, SE-405 30 Göteborg, Sweden. E-mail: lina.bunketorp@gu.se
Submitted August 30, 2007; accepted January 2, 2008
Introduction
Neck pain and disability resulting from motor vehicle accidents, so called whiplash-associated disorders (WAD) (1), is one of the most controversial topics in medicine. The disorder involves both physical and psychological disturbances and remains a poorly understood and challenging clinical entity, both as an economic burden and in terms of patient suffering. Limitation of neck mobility is a symptom frequently reported by patients (2). Cervical motion is suggested to be the most accurately and reproducibly measured parameter relating to functional assessment of the neck (3) and many methods have been developed to assess spinal mobility. A cervical range of motion (CROM) device can easily be implemented in an ordinary clinical setting. In previous studies (2–7), CROM was significantly reduced in patients with WAD compared with healthy subjects in the acute and chronic stage.
Most methods for spinal mobility assessment measure the overall range of spinal mobility. For description of the range of mobility, the methods assess either the surface curvature, altered angles, or skin distractions (8). In diagnostic radiology, a method described in a previous study (9) has been developed to study the motion in the cervical spine, C0–C7. Flexion-extension radiography has been used for over 50 years to detect abnormal segmental motion in the spine (10). A measuring technique used in the cervico-thoracic region, referred to as the cervico-thoracic ratio (CTR; Segmo-Graph AB, Stockholm, Sweden), is a method that allows the examination of segmental flexion mobility in the cervico-thoracic spine in a clinical setting (8). The method is intended to be used as a complement to other methods examining mobility in patients with neck- and shoulder pain (8). The CTR technique is developed to measure and assess the distribution of segmental flexion mobility in the cervico-thoracic articulations between C7 and T5. By means of the CTR, a mobility pattern of invariably reduced mobility in motion segment C7–T1, the inverse C7–T1 function, has been identified. It is defined as equal or less mobility in motion segment C7–T1 compared with T1–T2 (11). Inverse C7–T1 function was shown to be a predictor of development of neck-shoulder pain in a previous study (11). Furthermore, another previous cross-sectional study (12) demonstrated that reduced relative flexion mobility in segments C7–T1 and T1–T2 significantly predicted weakness in the hands.
In a previous study (3), fear of pain was suggested to be a possible source for submaximal performance of CROM. In a study by Klein et al. (13), patients with chronic WAD were, due to existing pain or fear of pain, either unable or unwilling to move the cervical spine into regions that required high muscle activity. In the presence of exaggerated fear of movement/(re)injury and fear of provocation of pain, a patient with WAD may presumably not move his or her head to the end of the existing range. In the aforementioned study (3), a small percentage of patients who were classified as atypical in terms of their motion profile had extreme personality and functional scores. It is also possible that perceived pain limits the range of motion, i.e. that there is an inverse relationship between cervical motion range and pain ratings, as shown previously (2).
The primary aim of this study was to evaluate whether women and men suffering from subacute WAD exhibit a characteristic pattern of distribution of segmental flexion mobility in the cervico-thoracic spine. In addition, the study aimed to assess the relationship between cervical flexion mobility according to a CROM instrument and segmental flexion mobility in the cervico-thoracic spine at different segments, and total CROM (including all directions) and segmental flexion mobility, and whether a possible hypomobility in C7-T1 is associated with future neck pain and weakness in the hands. Finally, the study aimed to investigate the relation between fear of movement/(re) injury and CROM, and between pain intensity and CROM.
Methods
Study design
The data in the present longitudinal study was obtained from a previous randomized controlled trial (RCT) (14). The RCT was conducted at an interdisciplinary rehabilitation centre specializing in patients with WAD. Patients were included in the RCT based on the following criteria: report of subacute WAD following a whiplash-type trauma to the neck, defined as a musculo-ligamental sprain or strain of the cervical region; no fractures; and no dislocations of the cervical spine. The exclusion criteria were: (i) time interval between the whiplash trauma and randomization of < 6 weeks or > 3 months; (ii) X-ray evidence of traumatic or severe degenerative lesions of the cervical spine; (iii) unrelated disease or additional injury that precluded completion of the questionnaires or would make evaluation difficult; (iv) previous severe neck pain causing more than one month of sick leave or disabled pension in the year preceding the accident; and (v) unable to understand and speak Swedish. The study was approved by the regional ethics review board.
Patients
All patients seeking treatment at the rehabilitation centre were invited to participate in a group session on a regular basis with a team physiotherapist and psychologist who presented information on symptoms and reactions in connection with whiplash trauma. The session aimed to reduce fear and anxiety and to give advice about self-management and recuperation. If interested in consulting a physiotherapist after the session, the patient could schedule an appointment in the regular treatment programme. After receiving an appointment, a recruitment letter for the RCT (14) was sent to 212 patients with subacute WAD, of whom 63 (30%) were willing to participate. Six of these patients were excluded because of unrelated diseases making evaluation difficult and 8 due to sick leave because of neck pain during the year preceding the accident. Six of these latter patients had been on sick leave due to a previous whiplash trauma. Forty-nine patients who fulfilled the criteria were included in the RCT and randomized into 2 physiotherapy interventions: group A, a home training group (25 patients); or group B, a supervised and individually tailored training group (24 patients). All patients were offered an individualized interdisciplinary rehabilitation programme including counselling by a physician, a psychologist, and a social worker working together in a team. Due to the detection of a severe, unrelated disorder and the receipt of a magnetic resonance imaging scan with evidence of severe degenerative lesions of the cervical spine prior to the trauma, 2 patients in group B became ineligible and were thus excluded following randomization. Forty-seven patients were finally included in the study, 30 women (64%) and 17 men (36%) with a mean age of 31 years (range 18–61 years). The whiplash trauma had occurred on average 64 days (range 42–121 days) before the start of the study. Among the patients 45 (96%) had been exposed to motor vehicle accidents and the remaining 2 patients (4%) had been involved in fall accidents. Patients who were excluded or were not willing to take part in the study entered the regular treatment programme at the rehabilitation centre. After a maximum of 3 months of physiotherapy interventions and after an additional 6 months, evaluation took place including all measures presented below. Differences between groups at baseline were non-significant (14), and the analyses in the present study were made regardless of group allocation in the RCT.
Measurements
A CROM (Lic Rehab Svetsary, Solna, Sweden) instrument was used to assess active cervical mobility. The CROM instrument is a measurement helmet equipped with a Myrin meter. Separate inclinometers are used for sagittal and lateral planes to eliminate relocation during measurements. A compass allows rotation measurements to be made in the preferred upright position. The range of motion was recorded in degrees in flexion, extension, lateral flexion, and rotation with the subject occupying a comfortable chair.
The CTR technique was used to assess segmental flexion mobility in the cervico-thoracic spine. The method describes what is defined as relative flexion mobility (CTR%) in terms of differences in segmental mobility between C7 and T5. The relative flexion mobility is a calculated ratio based on absolute values of skin distraction between C7 and T5. As the height of one disc and one thoracic vertebral body is approximately 3 cm, the distance of 3 cm marked, in the upright posture has been used as the definition of one motion segment (8). Absolute flexion mobility is defined as the measured alteration in cm between 3 cm interdistant skin markings marked from C7 down to T5 and measured with a tape measure after a maximal forward flexion of the trunk and neck from an upright posture (8) (Fig. 1). The CTR technique measures both partly segmental and total skin distractions. It compares the degree of segmental flexion mobility by establishing a ratio between partly segmental and total skin distractions. In a radiological evaluation it was shown that skin distraction, measured with a tape measure, approximately reproduces the segmental flexion mobility taking place between C7 and T5 (17). The CTR technique also describes a model for classification of mobility in 3 different classes, ordinary, hyper- and hypo-mobility (8). These mobility classes are defined from a population of healthy subjects. The CTR technique has been developed and described by Norlander et al. (8, 11) and is shown to be a valid and reliable method (17).
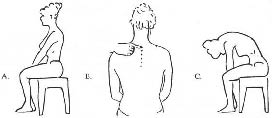
Fig. 1. Examination procedure. (A) Upright starting posture; (B) marking of 3-cm intervals between C7 and T5; (C) flexed posture during examination of absolute flexion mobility. (As described by Norlander et al. (17)).
A Grippit (AB Detektor, Göteborg, Sweden) was used to measure grip strength. The Grippit is a portable instrument that consists of an elliptical handle with electronic force transducers based on strain gauges placed on a base where an arm guide is mounted. Peak force and average value over 10 sec were registered. The grip strength is automatically recorded every half-second. The range of measurement was 0–999 N. Before the clinical measurements, the instrument was calibrated mechanically. The reliability of the Grippit has been demonstrated to be good (18).
The sensory dimension of the neck pain was assessed with a traditional 100-mm visual analogue scale (VAS) with the end-points 0 (no pain) and 100 (worst pain). The VAS has been demonstrated to have good reliability and validity (19, 20).
Secondly, a pain intensity matching device, PM (Cefar Medical AB, Lund, Sweden) was used, producing perceptual matching by gradually increasing electrical impulses between 2 fingers. The patient was instructed to hold the PM with the electrical stimulation unit between the right thumb and index finger with a firm grip. The PM causes an increasing electrical current that eventually becomes painful, and the patient is told to match the ongoing neck pain intensity to the physical sensation between the fingers. The electrical stimulation started by the patient, delivers electrical pulses with increasing intensity at random velocity. When the experienced neck pain corresponded in amplitude to the sensation of pain in the right hand, the patient was told to release the fingers from the PM, stopping the electrical stimulation unit, and a value was automatically recorded on a liquid crystal display (LCD) screen. The PM gives constant electrical stimulation controlled by a microprocessor, delivering rectangular pulses with the frequency of 10 Hz and amplitude of 15 mA. The pulse width is gradually increasing in 99 steps, with increments of 4 µs from zero to a maximum of 396 µs. The value reached between 0 and 99 is directly related to the pulse width, and as soon as the electrical circuit is detected by releasing the fingers from the electrode device, the electrical stimulation halts. PM is based on a random variation of the time it takes to increase stimulation. That way, the measurement is determined only by what the patient feels, not how long the measurement takes. The PM meets international ethical norms, because the patient can interrupt the stimulation at any moment. The measurement procedure is harmless, involves no intervention, and has no side-effects. The PM has demonstrated good reliability (21–23).
Fear of movement/(re)injury was assessed using the Swedish version of the Tampa Scale for Kinesiophobia (TSK). The scale was previously translated into Swedish in a forward and backward translation procedure (24). The TSK contains 17 statements developed to identify fear of (re)injury due to movement or activities such as “It is not safe for a person with a condition like mine to be physically active.” Scores range from 1 (strongly disagree) to 4 (strongly agree). The scores on items 2, 4, 8 and 16 are reversed so that high scores on all items indicate high levels of fear. The total sum score ranges from 17 to 68. The reliability and validity of the Swedish version of the TSK has been established (24, 25).
Examination procedure
Initial baseline measurements including cervical mobility according to the CROM instrument and CTR, assessment of grip strength, and pain intensity according to PM and VAS were performed in a quiet room at room temperature without any external disturbing factors. The CROM instrument was set up by the examiner. The same examiner performed all measurements, thus eliminating errors because of inter-tester variation. The examiner demonstrated how the movements were to be performed at a steady speed (flexion and extension, lateral bending and horizontal rotation). During measurement the researcher manually stabilized the patient’s shoulders and visually controlled the trunk and thoracic spine while the patient was verbally instructed to perform every movement until muscle tightness or pain limited movement. In the case of substitutional cervical head or shoulder movement (e.g. elevating the shoulder during lateral flexion measurement) the score was registered at the point where the movement begun. During flexion and extension measuring, it was considered a substitutional movement if the shoulders and upper back left the chair-back. Before rotation measurements the compass was calibrated with the patient in the upright position. While measuring lateral flexion, the patients were instructed to look at a particular spot on the wall in front of them.
In the CTR examination, the first procedure is to measure what is defined as absolute flexion mobility. With the patient in a sitting position, the examiner palpates the reference point, the spinous process of C7, then while the patients takes an upright posture looking straight ahead (Fig 1A), the examiner marks the most prominent part of the spinous process of C7, and with 3 cm intervals, corresponding to 1 motion segment; consequently, C7–T1 = 0–3 cm, T1–T2 = 3–6 cm, T2–T3 = 6–9 cm, T3–T4 = 9–12 cm and T4–T5 = 12–15 cm (Fig. 1B). An ordinary pen was used for the skin markings. The patient was then instructed to keep his or her chin flexed forward against the trunk and to flex his neck and trunk forward as much as possible (Fig. 1C). A woven tape measure was used to measure the absolute flexion mobility (i.e. the extensions between each marked lines), which is shown by the alterations of skin markings between C7 and T5 (as described by Norlander et al. (8)).
When measuring grip strength, the patients were seated in front of the Grippit, which was placed on a table. The patients were sitting in an upright posture close to the table in an adjustable chair with the feet supported. The lowest rib was level with the edge of the table and the forearm was placed in the arm support, which positioned the elbow joint in approximately 90° of flexion. The patient was first instructed to try out the Grippit by squeezing the elliptical handle. The measurement started with the right hand and during the 10-sec measurement period the patient was instructed to grasp the Grippit as hard as possible.
The TSK was administered to the patients after the baseline measurements were completed.
Statistical analyses
Relative segmental flexion mobility was presented using descriptive statistics, i.e. mean, standard deviation (SD) and 95% confidence interval (95% CI). To compare gender differences at a group level with respect to segmental flexion mobility measured with the CTR technique independent samples t-tests were used. To explore the relationship between segmental flexion mobility as measured by the CTR technique, and CROM, correlations were calculated with the Pearson’s correlation coefficient.
The relation between relative flexion mobility in the segment C7–T1 and future neck pain was estimated by correlative analysis using the non-parametric Spearman’s rank-order correlation coefficient. The relation between relative flexion mobility in the segment C7–T1 and future weakness in the hands were estimated by linear regression (Pearson).
The Spearman’s rank-order correlation coefficient was also used to explore the relationship between: (i) the intensity of pain measured with a VAS (using median scores by summarizing 7 days assessment) and total CROM; (ii) the pain magnitude matching score as measured by the PM and total CROM; and, finally, (iii) fear of movement or/(re)injury and total CROM. For all analyses, two-sided tests were performed, and a p-value of less than 0.05 was considered statistically significant. Analyses were performed using the Statistical Package for Social Science (SPSS 13.0 for Windows).
Results
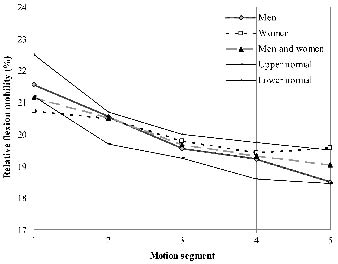
Analyses of the group as a whole did not show that the patients exhibited a characteristic pattern of distribution of segmental flexion mobility in the cervico-thoracic spine. However, when analysing men and women separately, the results revealed that the women exhibited hypomobility in the segment C7–T1 compared with men (Fig. 2). The relative flexion mobility in the segment C7–T1 was 20.7% in women, which is below the lower limit in ordinary mobility according to Norlander et al. (8). The men’s relative flexion mobility lies within the normal range considering all segments (Fig. 2).
Fig. 2. Mobility profile describing the distribution of mobility for motion segments C7 to T5 (1 = C7–T1, 2 = T1–T2, 3 = T2–T3, 4 = T3–T4, 5 = T4–T5) for men and women according to the cervico-thoracic ratio (CTR) technique (as described by Norlander et al. (15)).
The relative segmental flexion mobility at 3 and 9 months following baseline are presented in Table I (Test 2 and 3) and indicate stable measures (compared with the results at baseline). The mean relative flexion mobility for all 3 measurements is presented in Table II and there were significant gender differences in relative segmental flexion mobility in the segments C7–T1, T3–T4 and T4–T5. Fourteen women (47%) were presented with a so-called “inverse” C7–T1 function (defined as having greater or equal flexion mobility at level T1–T2 compared with level C7–T1 (11)). Six men (35%) had an “inverse” C7–T1 function.
| Table I. Relative flexion mobility describing the distribution of segmental flexion mobility (CTR%) in men and women |
| Motion segment | Test | Men Mean (SD) 95% CI (n = 17) | Women Mean (SD) 95% CI (n = 30) | p-value |
| C7–T1 Mean | 1 2 3 (1, 2, 3) | 21.9 (1.2) 21.3; 22.5 21.4 (1.2) 20.8; 22.0 21.2 (1.2) 20.5; 21.9 21.5 (1.2) 21.2; 21.9 | 20.7 (1.0) 20.4; 21.1 20.7 (1.0) 20.3; 21.0 20.9 (1.0) 20.4; 21.3 20.7 (1.0) 20.5; 21.0 | < 0.001 |
| T1–T2 Mean | 1 2 3 (1, 2, 3) | 20.9 (0.9) 20.4; 21.4 20.2 (0.6) 19.9; 20.5 20.5 (0.7) 20.1; 20.9 20.5 (0.8) 20.3; 20.8 | 20.4 (0.7) 20.2; 20.7 20.6 (0.8) 20.3; 20.9 20.5 (0.9) 20.1; 20.9 20.5 (0.8) 20.3; 20.7 | 0.84 |
| T2–T3 Mean | 1 2 3 (1, 2, 3) | 19.7 (0.7) 19.3; 20.0 19.6 (0.9) 19.1; 20.0 19.5 (0.9) 19.0; 20.0 19.6 (0.8) 19.4; 19.8 | 19.8 (0.6) 19.6; 20.1 19.9 (0.6) 19.6; 20.1 19.6 (0.6) 19.4; 19.9 19.8 (0.6) 19.7; 19.9 | 0.14 |
| T3–T4 Mean | 1 2 3 (1, 2, 3) | 19.1 (0.8) 18.7; 19.5 19.3 (0.6) 19.0; 19.6 19.4 (0.8) 18.9; 19.9 20.0 (1.4) 19.6; 20.4 | 19.4 (0.7) 19.1; 19.7 19.5 (1.0) 19.1; 19.8 19.2 (1.8) 18.4; 20.0 19.4 (1.2) 19.1; 19.6 | < 0.01 |
| T4–T5 Mean | 1 2 3 (1, 2, 3) | 18.6 (1.0) 18.1; 19.2 18.1 (4.9) 15.6; 20.8 19.4 (1.2) 18.7; 20.1 18.7 (3.0) 17.8; 19.6 | 19.6 (1.0) 19.2; 19.9 19.4 (0.9) 19.1; 19.8 19.8 (1.7) 19.1; 20.5 19.6 (1.2) 19.3; 19.8 | < 0.05 |
| CTR: cervico-thoracic ratio; SD: standard deviation; 95% CI: 95% confidence interval. |
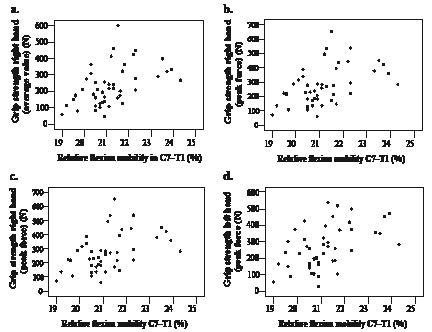
There was no significant association between cervical flexion mobility according to the CROM instrument and relative segmental flexion mobility in the cervico-thoracic spine at different segments, nor within the sexes. Furthermore, there was no significant correlation between the total CROM score and the segmental flexion mobility in the cervico-thoracic spine at different segments. There was no significant correlation between the relative segmental flexion mobility at different segments and future neck pain, i.e. hypomobility in the segment C7–T1 did not imply a significant increased risk for future neck pain. Analysing the relationship between the relative segmental flexion mobility in C7–T1 and the variable grip strength revealed weak but significant correlations, with generally low r-values considering both peak force and average value at both 3 and 9 months following baseline measurements (Table II). The relationship between the relative segmental flexion mobility in C7–T1 and the variable grip strength at 3 months following baseline is illustrated in scatter-plots in Fig. 3.
| Table II. Results of the regression analysis for the right and left hand grip strength, average and peak force values |
| Independent variable | Grip strength at 3 months following baseline | Grip strength at 9 months following baseline |
| Average value | Peak force | Average value | Peak force |
| B-value | p-value | r | B-value | p-value | r | B-value | p-value | r | B-value | p-value | r |
| Right hand |
| Segmental flexion mobility C7–T1 | 0.49 | < 0.01 | 0.24 | 0.48 | < 0.01 | 0.23 | 0.52 | < 0.001 | 0.27 | 0.53 | < 0.001 | 0.28 |
| Left hand |
| Segmental flexion mobility C7–T1 | 0.49 | < 0.001 | 0.25 | 0.50 | < 0.001 | 0.24 | 0.36 | < 0.05 | 0.13 | 0.42 | < 0.01 | 0.18 |
Fig. 3. Scatter plots describing the relationship between relative flexion mobility in the segment C7–T1 (%) and grip strength at 3 months following baseline in: (a) right hand (average value); (b) left hand (average value); (c) right hand (peak force); (d) left hand (peak force).
In the correlation analysis between total CROM and pain intensity according to VAS there was also a weak but significant negative correlation (r = –0.3) (p < 0.05) with subjects with restricted range of motion exhibiting higher pain intensity. A somewhat stronger significant negative correlation was also found between total CROM and the pain magnitude matching score measured with the PM (r = –0.43) (p < 0.01). There was no significant correlation between fear of movement/(re) injury and total CROM.
Discussion
The results in the present study showed that the women exhibited hypomobility in the segment C7–T1 according to the figures presented by Norlander et al. (8). The men’s relative flexion mobility lay within the normal range considering all segments. When analysing the group as a whole, the relative segmental flexion mobility lay within the normal range. Similar results are reported in the study by Norlander et al. (8) assessing segmental flexion mobility in 26 healthy female laundry workers and 95 male electricians and telephone workers. The male subjects showed a significantly greater degree of relative flexion mobility in both segment C7–T1 and T1–T2 compared with the female subjects. The relative flexion mobility in segment C7–T1 was 21.5% in women and 22.2% in men in the study by Norlander et al. (8) compared with 20.7% in the women and 21.6% in the men with WAD in the present study. However, the female laundry workers were not considered hypomobile in the segments C7–T1 in the study by Norlander et al. (8) as were the women with WAD in the present study.
In the classification by Norlander et al. (26), the limit for the hypomobility class of relative flexion mobility in segment C7–T1 is less than 21.2%. In the present study, the women were twice as many as the men, which resulted in segmental flexion mobility in the segment C7–T1 being just below the lower normal limit, when analysing the group as a whole. If there had been an equal number of women and men in the present study, presumably the segmental mobility in this segment would have been within the normal range. Fourteen women (47%) presented with a so-called “inverse” C7–T1 function (defined as having greater or equal flexion mobility at level T1–T2 compared with level C7–T1 (11) compared with 6 (35%) of the men. According to Norlander et al. (11), the occurrence of the inverse C7–T1 function is approximately 30% in a mixed female and male population. The hypomobility among the women in the present study, however, is a clear deviation from the normal distribution of mobility in this region according to a previous study (27). Whether the gender difference in mobility in the segment C7–T1 in the present study is caused by mechanical changes in the tissues, pain inhibition or is a biologically sound and normal difference and not a result of the whiplash trauma, is unclear from the results of the present study.
It is important to mention that the groups assessed in the present and the aforementioned study (8) might not be comparable with respect to segmental flexion mobility. However, the subjects included in the study by Norlander et al. (8) is the only study population in which the CTR measurement technique is used. In order to develop the concept of CTR, healthy subjects were examined and none of the 3 classes defined as ordinary, hyper- and hypomobility are regarded as having “pathological” mobility even though neck-shoulder pain has been found to be more frequent among subjects with hypomobility at level C7–T1 compared with subjects with ordinary hypermobility (8, 11, 12). Apart from the classification by Norlander et al. (8), no formal criteria have been established for abnormal motions of this part of the spine (28). Since no control group was included in the present study, the previously presented figures (8) were used for comparison.
There was no significant correlation between cervical flexion mobility according to the CROM instrument and segmental flexion mobility in the cervico-thoracic spine at different segments, nor between total CROM score and segmental flexion mobility, nor within the sexes in the present study. Furthermore, the reduced relative flexion mobility in the cervico-thoracic junction was not shown to be significantly correlated with future neck pain in the present study, which contradicts the previous findings showing that differences from normal relative flexion mobility in the segment C7–T1 is an indicative factor of musculoskeletal neck pain (11).
There was a weak but significant correlation between segmental flexion mobility in the segment C7–T1 and future grip strength, which is in accordance with a previous study (12) indicating that reduced mobility in this segment may increase the risk for weakness in the hands. However, in the previous study (12), the symptom weakness in the hands was subjectively reported and not objectively measured as in the present study. Norlander et al. mention in their study (12), that the motion segments C7–T1 and T1–T2 correspond to the spinal levels where the roots of the ulnar nerve and parts of the median nerves originate. The flexor muscles of the hand and the forehand are supplied by these nerves. From a neurological point of view, reduced grip strength as found in the present study and the sensation of weakness in the hands seem to be reasonable symptoms, as previously stated (12). A dysfunction at the cervico-thoracic junction might cause an experience of sensory feedback from joint afferents and, thus, weakness in the hands, as previously discussed (12), or lead to an objectively reduced grip strength due to a possible nerve root compression. However, these theories are highly speculative and are far from being established. It would be of interest to investigate this relationship further.
There are many factors, including psychological ones, that have been suggested to contribute to chronic neck pain and probably also influence neck range of motion (29, 30). However, in the present study, there was no significant correlation between loss of CROM and fear of movement/(re)injury, which is in accordance with previous findings (4) and contradicts others (3, 13). As previously suggested (31), the relationship between fear-avoidance beliefs and disability in patients with cervical pain may be weak compared with patients with lumbar pain. On the other hand, weak but significant negative correlations were found to exist between both the neck pain intensity score according to VAS and total CROM scores, and the PM magnitude matching score and total CROM scores, which is in accordance with previous findings (2), indicating that neck pain may give rise to a restricted range of motion. In another previous study (32), weak significant correlations were also found between CROM and corresponding pain ratings. Other studies (33, 34) have found either low or insignificant correlations between active CROM and self-rated pain. The reason for these contradictory results may be that in the studies indicating a weak or insignificant relationship, pain intensity while performing the measurement was recorded, and not the intensity of pain independent of motion as in the present and the aforementioned study (2).
It is argued that measurements using the CTR technique have to be repeated in order to determine whether the observed segmental mobility is occasional and can be regarded as a normal biological variation of mobility, or whether the possible dysfunction remains and seems to become permanent (11). In the previous study by Norlander et al. (11), the risk of developing neck-shoulder pain increased significantly when the reduced mobility in the segment C7–T1 was established 3 or more times during the follow-up period. In the present study, 3 measurements during the follow-up period were therefore registered, and indicated that the segmental flexion mobility including the hypomobility presented among the women was permanent rather than occasional.
The significance of measuring neck range of motion in WAD is a debated subject in the literature (29). In the Quebec Task Force grading system for WAD, the criterion restricted neck range of motion is present from Grade 2 upward (1). For clinicians and therapists, it is a common clinical practice to measure neck range of motion both as a diagnostic tool and as a sign of progress. It is argued that the lack of significance may be due to the fact that there are not many reliable and clinically applicable objective methods that measure segmental mobility (12). However, for interpretation on an individual level, a consensus on normal range of motion is of utmost importance, although initial individual values may serve as a reference in a rehabilitation situation as Kaale et al. state in their study (7).
The patients in the present study were selected from an interdisciplinary rehabilitation centre whose patients, in general, are considered to exhibit a more complex picture, being more emotionally or physically affected, or both, than patients with WAD are on average. The selected group was, however, considered to be a representative sample of those who remain disabled beyond the healing of any tissue damage in the natural recovery following a whiplash trauma when pain-related cognitions are still a problem, which constitutes the target group in our study. All sought care because of subacute WAD, mostly on their own initiative.
There are limitations in the present study that restrict the conclusions that may be drawn. The major limitation of the present study is that no control group was included representing the general population. Furthermore, the small number of patients included and the different number of women and men is another important limitation. One could further question whether it would be more correct to conclude that women exhibited less mobility than men rather than drawing the conclusion that women exhibited hypomobility in the segment C7–T1? In a previous study Norlander et al. (8) state that it must be emphasized that the purpose of using the CTR technique is not to decide the exact vertebral flexion angles for C7 to T5, but rather to describe the functional characteristics of mobility in this region, which are probably of greater interest when examining a patient with neck-shoulder pain.
Another weakness is that even though the present study has a longitudinal design, the analyses remain strictly correlative and the assumptions such as direction of causality should be avoided. It is therefore not possible to determine whether reduced total cervical mobility is a result of pain, or is a factor eliciting pain. It is, however, unlikely that weakness in the hands would have an impact on segmental flexion mobility in the cervical spine instead of the other way around, as indicated in the results. One might, however, have assumed that this correlation would emerge, since women who exhibited hypomobility would be unlikely to have the same grip strength as men, which might thus be the reason for the correlation shown. Moreover, the r-values in the correlation analyses are low and it would be of interest to investigate the relationships further.
Whether the differences in segmental mobility between men and woman have a physiological and/or biological explanation remains to be investigated. Another weakness is that the groups assessed in the present and the aforementioned study (8) might not be comparable with respect to segmental flexion mobility due to their varying background. As previously mentioned, however, no formal criteria have been established for abnormal motions of the spine (28) apart from the classification by Norlander et al. (8). The subjects in the study by Norlander et al. (8), which is the only study population in which the CTR measurement technique is used, was therefore chosen for comparison.
The upper cervical spine segments are commonly injured in whiplash traumas (35). A limitation with the CTR measurement technique is that it only measures relative flexion mobility in the cervico-thoracic junction and the upper thoracic spine. Some patients in the present study may have had abnormal segmental motion in the upper cervical spine segments that was not possible to register using the methodology presented. This questions the clinical significance of the results in the present study and raises the question as to whether the CTR technique is a valuable tool in evaluative contexts. The inverse C7–T1 function however, is regarded as a dysfunction that can give rise to “motion segment related pain” and has been shown to be an important factor in the assessment of neck-shoulder pain (26). Further research is thus necessary evaluating the clinical value and research importance of the CTR technique, as well as the validation of the clinical significance of invariable inverse C7–T1 function. Furthermore, in addition to a control group representing the general population it would be necessary to include a larger cohort and enable analysis of all cervical segments to address the limitations in the present study.
In conclusion, women with subacute WAD seem to exhibit flexion hypomobility in segment C7–T1 compared with men. There was no significant correlation between CROM and segmental flexion mobility. Segmental flexion mobility in C7–T1 was weakly, but significantly, correlated with the variable grip strength, but was not shown to be a predictor of future neck pain. Neck pain may give rise to restricted range of motion, while fear of movement/(re)injury does not seem to affect CROM. However, due to low r-values in the statistical analyses further studies are required.
References
1. Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine 1995; 20: 1S–73S.
2. Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Staehelin Jensen T. Headache, neck pain, and neck mobility after acute whiplash injury: a prospective study. Spine 2001; 26: 1246–1251.
3. Prushansky T, Pevzner E, Gordon C, Dvir Z. Performance of cervical motion in chronic whiplash patients and healthy subjects: the case of atypical patients. Spine 2006; 31: 37–43.
4. Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Development of motor system dysfunction following whiplash injury. Pain 2003; 103: 65–73.
5. Kasch H, Bach FW, Jensen TS. Handicap after acute whiplash injury: a 1-year prospective study of risk factors. Neurology 2001; 56: 1637–1643.
6. Antonaci F, Bulgheroni M, Ghirmai S, Lanfranchi S, Dalla Toffola E, Sandrini G, et al. 3D kinematic analysis and clinical evaluation of neck movements in patients with whiplash injury. Cephalalgia 2002; 22: 533–542.
7. Kaale BR, Krakenes J, Albrektsen G, Wester K. Active range of motion as an indicator for ligament and membrane lesions in the upper cervical spine after a whiplash trauma. J Neurotrauma 2007; 24: 713–721.
8. Norlander S, Aste-Norlander U, Nordgren B, Sahlstedt B. A clinical method for measuring segmental flexion mobility in the cervico-thoracic spine and a model for classification. Scand J Rehabil Med 1995; 27: 89–98.
9. Van Mameren H, Drukker J, Sanches H, Beursgens J. Cervical spine motion in the sagittal plane (I) range of motion of actually performed movements, an X-ray cinematographic study. Eur J Morphol 1990; 28: 47–68.
10. Knuttson F. The instability associated with disc generation in the lumbar spine. Acta Radiol 1944; 25: 593–609.
11. Norlander S, Aste-Norlander U, Nordgren B, Sahlstedt B. Mobility in the cervico-thoracic motion segment: an indicative factor of musculo-skeletal neck-shoulder pain. Scand J Rehabil Med 1996; 28: 183–192.
12. Norlander S, Nordgren B. Clinical symptoms related to musculoskeletal neck-shoulder pain and mobility in the cervico-thoracic spine. Scand J Rehabil Med 1998; 30: 243–251.
13. Klein GN, Mannion AF, Panjabi MM, Dvorak J. Trapped in the neutral zone: another symptom of whiplash-associated disorder? Eur Spine J 2001; 10: 141–148.
14. Bunketorp L, Lindh M, Carlsson J, Stener-Victorin E. The effectiveness of a supervised physical training model tailored to the individual needs of patients with whiplash-associated disorders – a randomized controlled trial. Clin Rehabil 2006; 20: 201–217.
15. Tousignant M, de Bellefeuille L, O’Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine 2000; 25: 324–330.
16. Kapandji IA, editor. The physiology of the joints. Vol. 3: Churchill Livingstone; 1970.
17. Norlander S, Aste-Norlander U, Nordgren B, Sahlstedt B. A clinical method for measuring the distribution of segmental flexion mobility in the cervico-thoracic spine. Ups J Med Sci 1995; 100: 151–160.
18. Lagerstrom C, Nordgren B. On the reliability and usefulness of methods for grip strength measurement. Scand J Rehabil Med 1998; 30: 113–119.
19. Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983; 16: 87–101.
20. Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990; 13: 227–236.
21. Lundeberg T, Lund I, Dahlin L, Borg E, Gustafsson C, Sandin L, et al. Reliability and responsiveness of three different pain assessments. J Rehabil Med 2001; 33: 279–283.
22. Lund I, Lundeberg T, Kowalski J, Sandberg L, Budh CN, Svensson E. Evaluation of variations in sensory and pain threshold assessments by electrocutaneous stimulation. Physiother Theory Pract 2005; 21: 81–92.
23. Stener-Victorin E, Kowalski J, Lundeberg T. A new highly reliable instrument for the assessment of pre- and postoperative gynecological pain. Anesth Analg 2002; 95: 151–157, table of contents.
24. Lundberg MKE, Styf J, Carlsson GC. A psychometric evaluation of the Tampa Scale for Kinesiophobia – from a physiotherapeutic perspective. Physiother Theory Pract 2004; 20: 121–133.
25. Bunketorp L, Carlsson J, Kowalski J, Stener-Victorin E. Evaluating the reliability of multi-item scales: a non-parametric approach to the ordered categorical structure of data collected with the Swedish version of the Tampa Scale for Kinesiophobia and the Self-Efficacy Scale. J Rehabil Med 2005; 37: 330–334.
26. Norlander S, Gustavsson BA, Lindell J, Nordgren B. Reduced mobility in the cervico-thoracic motion segment – a risk factor for musculoskeletal neck-shoulder pain: a two-year prospective follow-up study. Scand J Rehabil Med 1997; 29: 167–174.
27. Andersson G. Biomechanics of the lumbar spine. Clin Rheumatic Dis 1980; 6: 37–49.
28. Kristjansson E, Leivseth G, Brinckmann P, Frobin W. Increased sagittal plane segmental motion in the lower cervical spine in women with chronic whiplash-associated disorders, grades I–II: a case-control study using a new measurement protocol. Spine 2003; 28: 2215–2221.
29. Puglisi F, Ridi R, Cecchi F, Bonelli A, Ferrari R. Segmental vertebral motion in the assessment of neck range of motion in whiplash patients. Int J Legal Med 2004; 118: 235–239.
30. Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol 1991; 69: 683–694.
31. George SZ, Fritz JM, Erhard RE. A comparison of fear-avoidance beliefs in patients with lumbar spine pain and cervical spine pain. Spine 2001; 26: 2139–2145.
32. Hagen KB, Harms-Ringdahl K, Enger NO, Hedenstad R, Morten H. Relationship between subjective neck disorders and cervical spine mobility and motion-related pain in male machine operators. Spine 1997; 22: 1501–1507.
33. Jordan A, Mehlsen J, Ostergaard K. A comparison of physical characteristics between patients seeking treatment for neck pain and age-matched healthy people. J Manipulative Physiol Ther 1997; 20: 468–475.
34. Ylinen J, Takala EP, Kautiainen H, Nykanen M, Hakkinen A, Pohjolainen T, et al. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur J Pain 2004; 8: 473–478.
35. Krakenes J, Kaale BR, Moen G, Nordli H, Gilhus NE, Rorvik J. MRI assessment of the alar ligaments in the late stage of whiplash injury – a study of structural abnormalities and observer agreement. Neuroradiology 2002; 44: 617–624.