OBJECTIVE: To document the prevalence of shoulder pain, associated patient characteristics, and intensity and interference with shoulder function in activities in wheelchair users.
DESIGN: A cross-sectional survey.
Patients: Individuals with a thoracic spinal cord injury.
METHODS: A 3-part questionnaire on patient characteristics, medical history, supplemental questions, and the Wheelchair Users Shoulder Pain Index was administered to 101 patients.
RESULTS: Of the 88 subjects (87%) who completed the questionnaire, 40% reported experiencing current shoulder pain, often chronic in nature. The highest median intensity of shoulder pain was reported for pushing the wheelchair up ramps or inclines outdoors. Reports of limitations regarding the ability to use the shoulder in activities were common. Most subjects used no upper extremity assistive devices during transfer or wheelchair propulsion. Of those with current shoulder pain, 37% had not sought medical attention. Age was associated with ongoing shoulder pain.
CONCLUSION: Shoulder pain is a common problem in wheelchair users with a thoracic spinal cord injury, it seems more likely to occur with increased age, and is a potential cause of activity limitations. The findings indicate a need to develop programmes of prevention, patient education, diagnosis and treatment, possibly including more frequent use of upper extremity assistive devices.
Key words: shoulder pain, spinal cord injuries, paraplegia, wheelchairs.
J Rehabil Med 2008; 40: 277–283
Correspondence address: Marie Alm, Spinalis SCI Unit, Karolinska University Hospital, SE-169 89 Stockholm, Sweden. E-mail: marie.alm@karolinska.se
Submitted May 15, 2007; accepted December 18, 2007
Introduction
The shoulder has been reported to be the joint most commonly associated with pain above the level of injury in individuals with paraplegia following spinal cord injury (SCI) (1). The reported prevalence of shoulder pain in paraplegic individuals is high, usually between 30% and 70% (2–7). The results of prevalence studies are difficult to generalize due to large variations in study populations concerning diagnosis, age, level of injury, and time since injury. Prevalence appears to vary depending on the time since the SCI. The risk of shoulder pain and musculoskeletal disorders appears to increase as a person with a SCI ages and to occur at a younger age compared with an able-bodied population (8).
Shoulder pain in the acute injured individual has been described to be due to high demands on weak or unconditioned muscles (1), whereas shoulder pain in the chronic phases is believed to be partly a result of overuse (1, 9). Individuals who use a wheelchair for mobility and have poorly innervated trunk muscles must rely on their upper extremities for stability and mobility. In the chronic stage after SCI, soft tissue structures are exposed to overuse in activities of daily living, for example, in wheelchair propulsion and transfer in which the shoulder becomes a weight-bearing joint. Subacromial impingement (9, 10) with bursitis; tendinopathy; and tears of the rotator cuff (especially the supraspinatus), the biceps tendon, or both (2, 11) are the most common diagnoses of individuals with paraplegia suffering from chronic nociceptive shoulder pain. Findings such as radiographic bone and joint abnormalities, that is, acromioclavicular joint space narrowing and osteolysis of the distal clavicle, have also been found to be common (12, 13). Further complications described in paraplegic wheelchair users, especially in wheelchair athletes, are peripheral neuropathies where the median nerve is the most commonly affected nerve and a high prevalence of carpal tunnel syndrome (2, 3).
Shoulder pain in individuals with paraplegia is believed to be multi-factorial, but the aetiology and associated factors have not been investigated fully. Some studies report that the prevalence of shoulder pain in subjects with paraplegia increases the longer the time since injury (2–4). Others failed to observe any differences regarding time since injury and age in subjects with and without shoulder pain (7, 13). Few studies have carefully addressed the association of age and time of wheelchair use with shoulder pain or possible interactions between these factors (6).
Gender differences have also been suggested, and although an association of female gender and development of degenerative changes has been documented (14, 15), gender differences regarding the prevalence of shoulder pain have not been well studied. Level of injury has also been described to be associated with the prevalence of rotator cuff disease and shoulder pain intensity (6, 16), where paraplegics with a high level of injury are believed to be more exposed than individuals with a low level of injury.
High levels of activities of daily living, for example, repetitive load from propulsion and transfer (2, 9, 15, 17), are other factors thought to contribute to shoulder pain. Few studies have investigated differences in shoulder pain among paraplegic wheelchair users regarding different levels of activity and fitness. Fewer degenerative changes have been documented in active than in inactive persons (18), and less pain has been reported in athletes than in non-athletes (19). In contrast, other authors found no differences in prevalence of shoulder pain between athletic and non-athletic wheelchair users (20).
Few studies have described which activities cause the most intense pain, how pain interferes in daily living, and what the individual consequences of shoulder pain are (5–7). Only one study addressed the consequences and prevalence of shoulder pain in individuals with SCI in Sweden (7).
Objectives
The main objectives of this study were to describe the prevalence of shoulder pain, associated patient characteristics, and pain intensity and interference with shoulder function in activities in Swedish full-time wheelchair users with a thoracic SCI.
Specific aims were to study:
• Prevalence of shoulder pain and its association with subject characteristics such as age, gender, years of wheelchair use, level of injury and level of activity.
• Daily activities in which shoulder pain frequently appears and the ability to use the shoulder in daily activities and in sports and leisure activities.
• The use of upper extremity assistive devices during transfer and wheelchair propulsion.
• To what extent shoulder pain is followed by medical attention, clinical examination, and treatment.
Methods
Subjects
Subjects were recruited from patient records at the SCI unit. Inclusion criteria were: Swedish speaking, age 18–70 years, SCI of more than one year, neurological level of injury between T2 and T12, full-time wheelchair user, normal motor and sensory functions in the upper extremities according to the classification system of the American Spinal Injury Association (ASIA) (21), and total loss of motor function in the lower extremities (motor score 50/100, ASIA impairment grade A or B). Exclusion criteria were: pre-pubertal onset of SCI, an additional neurological diagnosis such as brain injury or stroke with a cognitive disorder, and cervical post-traumatic myelopathy with a current impact on motor or sensory function in the upper extremities.
Instrumentation
Study participants were asked to complete a self-reported, 3-part questionnaire comprising questions on patient characteristics and medical history, supplementary questions, and the Wheelchair Users Shoulder Pain Index (WUSPI) to determine patient characteristics, lifestyle, upper extremity pain, shoulder pain intensity and interference of shoulder function in activities.
The section on patient characteristics and medical history included questions on age, gender, marital status, occupational and recreational activities, past and present shoulder pain, shoulder(s) involved, and treatment received (5, 22).
The following supplementary questions were asked:
1. If you use an electrical wheelchair, what type do you use?
2. Do you use additional help or assistive devices during transfer? If yes, what kind?
3. If you drive a car, do you load your wheelchair into the car yourself?
4. Do you participate regularly in sports or leisure activities or other physical activities? If yes, what activities are you involved in and how many times per week and how many hours per week do you participate in each activity?
5. Have you experienced shoulder pain in the past week?
6. Have you experienced shoulder pain in the past month? If yes, how long have you had your problems?
7. If you have sought medical attention for your shoulder problems, were your problems examined and diagnosed?
Furthermore, 4 questions modified from the reliability tested Swedish version of the Shoulder Rating questionnaire (23) were used to determine the presence and severity of shoulder pain at rest and during activities and the ability to perform daily activities and sports and leisure activities. The questions were modified by changing the time aspect from past month to past week.
The WUSPI consists of 15 items where shoulder pain based on activities performed in the past week is reported on a visual analogue scale (VAS) with scores from 0 to 10 (22). For each item, additional options exist to mark “no pain” and to mark if the activity had not been performed in the past week. Face validity of the WUSPI have previously been established by asking wheelchair users to review and confirm the inclusion of relevant functional activities in instrument items (22) and previous studies have reported the WUSPI to have concurrent validity with loss of active range of shoulder motion, high internal consistency, and high test-retest reliability (22, 24). A Swedish translation of the WUSPI and the section on patient characteristics and medical history was used in the present study (7).
Content validity and equivalence of instrumentation
The former Swedish translation of WUSPI by Samuelsson et al. (7) was made from the original version by a qualified translator. Both versions were reviewed by a second translator for equivalence. A group of experts reached consensus on a final version with cultural adaptation of the instrument by changing the endpoints of the VAS from “worst pain ever experienced” in the English version to “worst pain imaginable” in the Swedish version because this endpoint is more common on the VAS in Sweden (Samuelsson, personal communication).
To ensure equivalence between content in the original and the Swedish version of the WUSPI, we used proposed guidelines for translation and cross-cultural adaptation (25). Two Swedish versions of the WUSPI, the version by Samuelsson et al. (7) and a newly translated Swedish version made from the original source, were back-translated into English, and all translations were reviewed by a multidisciplinary group of experts (n = 4). The Swedish versions were considered to be equivalent to each other and to the original English version. The modification made by Samuelsson et al. (7), of the right endpoint of the VAS, was considered to be the most appropriate to establish cultural validity of the instrument.
Content validity (face validity) of the WUSPI and the questions in the different sections in our questionnaire was tested in a sample of patients with paraplegia (n = 5), who were interviewed regarding relevance, ease of completion, and comprehensibility of the questionnaire. All group members found the WUSPI to be relevant, easy to complete, and comprehensible, as were the questions in the other sections of the questionnaire. A few comments such as on layout were made concerning the sections “supplemental questions” and “medical history and patient characteristics”, but these were considered to be of minor importance.
Procedure
In all, 101 subjects met the inclusion criteria. They were sent a coded, self-reported questionnaire, including a cover letter and a pre-stamped envelope, by post. By returning the questionnaire, the subjects gave their informed consent to participate in the study. The subjects who currently experienced shoulder pain, had experienced shoulder pain in the past week, or both were asked to fill in all supplementary questions and the WUSPI. A reminder was sent 3 weeks later to the subjects who had not returned the questionnaire. A final reminder by telephone was made after 5 weeks. The study was approved by the Regional Ethics Approval Board.
Statistics
Patient characteristics, medical history and answers to supplementary questions were analysed with descriptive statistics (number of observations, mean, standard deviation (SD), and percentage by group of subjects with and without shoulder pain). Associations of the patient characteristics age, gender, years of wheelchair use, level of injury (high vs low) and level of activity (defined as employed/student vs not working; hours/week working/studying categorized as 0, 1–20, or 21–40; driving vs not driving; wheelchair transfers/day categorized as 1–10, 11–20, or > 20; regular physical activity vs no regular physical activity; hours/week of physical activity categorized as 0, 1–3, 4–10 and > 10) with ongoing shoulder pain was tested in logistic regression analyses to discriminate between characteristics in subjects who currently experienced pain or had experienced pain in the past week (n = 36) and subjects with no pain (n = 52). Results are presented as odds ratios (ORs), where an OR > 1 is considered to be positively associated with pain, and corresponding 95% confidence intervals (CIs). The scores of individual items on the WUSPI were analysed with Friedman’s analysis of variance (ANOVA) to determine differences between items (activities) concerning pain intensity. All tests were 2-sided at the 0.05 level of significance. All calculations were made using STATISTICA 7:1 (Statsoft Inc.).
Results
Subject characteristics
Eighty-eight (87%) of the 101 subjects, 70 men and 18 women, returned the questionnaire. The mean age of the subjects was 47 years (SD 11.9, range 21–69 years): 46 (SD 12.2) years for men and 48 (SD 11.2) years for women. Mean wheelchair use was 19 years (SD 11.9, range 1–47 years): 19 years (SD 12.3) for men and 18 (10.0) years for women. Fifty-eight subjects had high levels of lesions (T2–T8) and 30 subjects low (T9–T12). We chose this division because individuals with lesions at the T9–T12 level often have trunk muscle activity, which aids erect posture and upper extremity tasks (26). Seventy-seven subjects were classified as having an ASIA impairment grade A, and 11 subjects ASIA impairment grade B. Table I lists the subject characteristics. The drop-out rate was 13%. Of the 13 subjects who did not return the questionnaire, 9 were men and 4 women, mean age 47 years (SD 12.5).
| Table I. Descriptive statistics (frequency, percentage, mean, and standard deviation (SD)) for subject characteristics according to presence and absence of shoulder pain and for the total group |
| Subject characteristics | Total group (n = 88) | Subjects with pain† (n = 36) | Subjects with no pain (n = 52) |
| Gender, n (%) |
| Male | 70 | 31 (44) | 39 (56) |
| Female | 18 | 5 (28) | 13 (72) |
| Age, mean (SD) | 46.7 (11.9) | 49.8 (12.2) | 44.6 (11.4) |
| 21–30 | 9 | 3 (33) | 6 (67) |
| 31–40 | 18 | 4 (22) | 14 (78) |
| 41–50 | 26 | 10 (38) | 16 (62) |
| 51–60 | 22 | 12 (55) | 10 (45) |
| 61–70 | 13 | 7 (54) | 6 (46) |
| Mean (SD) years of wheelchair use | 18.7 (11.9) | 20.6 (13.1) | 17.4 (10.8) |
| Level of SCI, n (%) |
| High | 58 | 24 (41) | 34 (59) |
| Low | 30 | 12 (40) | 18 (60) |
| Marital status*, n (%) |
| Single | 50 | 23 (46) | 27 (54) |
| Consensual union | 38 | 13 (34) | 25 (66) |
| Occupation*, n (%) |
| Employed/student | 47 | 20 (43) | 27 (57) |
| Not working | 41 | 16 (39) | 25 (61) |
| Hours per week at work/school*, n (%) |
| 0 | 41 | 16 (39) | 25 (61) |
| 1–20 | 23 | 9 (39) | 14 (61) |
| 21–40 | 24 | 11 (46) | 13 (54) |
| Wheelchair transfers/day*, n (%) |
| 1–10 | 33 | 13 (39) | 20 (61) |
| 11–20 | 37 | 14 (38) | 23 (62) |
| > 20 | 18 | 9 (50) | 9 (50) |
| Regularly in to sports/leisure/physical activity*, n (%) |
| Yes | 49 | 23 (47) | 26 (53) |
| No | 39 | 13 (33) | 26 (67) |
| Hours per week of sport/leisure/physical activities*, n (%) |
| 0 | 39 | 13 (33) | 26 (67) |
| 1–3 | 11 | 6 (55) | 5 (45) |
| 4–10 | 32 | 16 (50) | 16 (50) |
| > 10 | 6 | 1 (17) | 5 (83) |
| Driving, n (%) |
| Yes | 67 | 27 (40) | 40 (60) |
| No | 21 | 9 (43) | 12 (57) |
| Hours per week driving*, n (%) |
| 0 | 21 | 9 (43) | 12 (57) |
| 1–10 | 60 | 24 (40) | 36 (60) |
| 11–20 | 6 | 3 (50) | 3 (50) |
| > 20 | 1 | 0 (0) | 1 (100) |
| *Data from original reports were regrouped into the categories presented. †Subjects who experienced current shoulder pain, shoulder pain the past week, or both. SCI: spinal cord injury. |
Pain prevalence
Few of the 88 subjects reported that they had experienced shoulder pain before becoming a wheelchair user (8%), whereas 59 subjects (67%) reported a history of shoulder pain since becoming a wheelchair user. Hand or elbow pain was also relatively common since the beginning of wheelchair use. Thirty-five subjects (40%) reported current shoulder pain, usually bilateral or left sided (Table II). Most subjects with current shoulder pain (32/35, 91%) had chronic pain (pain > 3 months), and 26 subjects (74%) reported long-lasting shoulder pain for more than one year. Of all subjects, 43 (49%) had experienced shoulder pain in the past month and, of these, 35 (81%) reported chronic shoulder pain.
| Table II. Descriptive statistics of medical history of upper extremity pain and the prevalence of shoulder pain (n = 88) |
| | n | % |
| Shoulder pain prior to wheelchair use | | |
| Yes | 7 | 8 |
| No | 81 | 92 |
| Shoulder pain since becoming a wheelchair user | | |
| Yes | 59 | 67 |
| No | 29 | 33 |
| If yes, which shoulder | | |
| Left | 15 | 25 |
| Right | 13 | 22 |
| Bilateral | 31 | 53 |
| Hand or elbow pain or injuries since becoming a wheelchair user | | |
| Yes | 52 | 59 |
| No | 36 | 41 |
| Current shoulder pain | | |
| Yes | 35 | 40 |
| No | 53 | 60 |
| If yes, which shoulder | | |
| Left | 11 | 31 |
| Right | 7 | 20 |
| Bilateral | 17 | 49 |
| Shoulder pain the past month | | |
| Yes | 43 | 49 |
| No | 45 | 51 |
| If yes, for how long? | | |
| 1–3 months | 8 | 18 |
| 4–6 months | 3 | 7 |
| > 6 months | 5 | 12 |
| > 1 year | 27 | 63 |
Subject characteristics associated with shoulder pain
Age was significantly associated with ongoing shoulder pain, with risk increasing with age, OR = 1.05 (95% CI = 1.01–1.10, p = 0.03), i.e. 5% per year. No other subject characteristics were found to be significantly associated with shoulder pain.
Pain intensity and interference with shoulder function in activities
Subjects who experienced current shoulder pain, shoulder pain in the past week, or both, were analysed regarding pain intensity and interference with shoulder function in activities (Table III). Most of these subjects (32/36, 89%) reported shoulder pain at rest in the past week and 22/36 subjects (61%) reported considerable pain during rest (moderate, severe, or very severe pain). All subjects reported shoulder pain during activities in the past week. As many as 31/36 (86%) reported considerable pain (moderate, severe, or very severe pain during activities). Limitations regarding the ability to use the shoulder in daily activities were reported by 32/36 subjects (89%), and 17/36 (47%) reported this limitation to be considerable (moderate, severe, and very severe limitation). Limitations regarding the ability to use the shoulder in sports and leisure-time activities were reported by 26/31 subjects (84%), and considerable limitations by 18/31 (58%) (Table III).
| Table III. Descriptive statistics of activity-related pain in subjects with current shoulder pain, shoulder pain the past week, or both |
| | n |
| Shoulder pain at rest the past week (n = 36) |
| Very severe | 1 |
| Severe | 2 |
| Moderate | 19 |
| Mild | 10 |
| None | 4 |
| Shoulder pain during activities the past week (n = 36) |
| Very severe | 1 |
| Severe | 11 |
| Moderate | 19 |
| Mild | 5 |
| None | 0 |
| Ability to use your shoulder in daily activities such as dressing, grooming, driving, household chores the past week (n = 36) |
| Very severe limitation | 1 |
| Severe limitation | 8 |
| Moderate limitation | 8 |
| Mild limitation | 15 |
| No limitation | 4 |
| Ability to use your shoulder in sports and leisure activities the past week (n = 31) |
| Very severe limitation | 1 |
| Severe limitation | 6 |
| Moderate limitation | 11 |
| Mild limitation | 8 |
| No limitation | 5 |
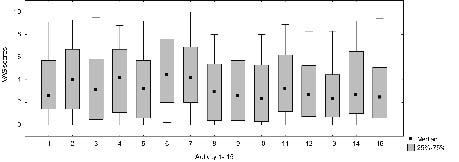
The WUSPI was completed by 34 subjects (94%) with current pain, pain the past week, or both and further analysed. Intensities of shoulder pain varied significantly between the WUSPI items (p = 0.0047). The highest median intensities of shoulder pain on the WUSPI were reported for the following activities: pushing up ramps or inclines outdoors (median 4.4), loading the wheelchair into the car (median 4.2), lifting objects down from an overhead shelf (median 4.2), and transferring from a wheelchair to a car (median 4.0) (Fig. 1).
Fig. 1. Box-plots illustrate pain intensity as assessed with the visual analogue scale (VAS) for 15 daily activities according to the Wheelchair Users Shoulder Pain Index (WUSPI) in subjects with current shoulder pain, shoulder pain the past week, or both (n = 34). (1: transferring from bed to a wheelchair (n = 34); 2: transferring from a wheelchair to a car (n = 31); 3: transferring from a wheelchair to the tub or shower (n = 32); 4: loading your wheelchair into a car (n = 26); 5: pushing your wheelchair for 10 min or more (n = 33); 6: pushing up ramps or inclines outdoors (n = 29); 7: lifting objects down from an overhead shelf (n = 33); 8: putting on pants (n =34); 9: putting on a T-shirt or pullover (n = 34); 10: putting on a button-down shirt (n = 31); 11: washing your back (n = 31); 12: usual daily activities at work or school (n = 28); 13: driving (n = 28); 14: performing household chores (n = 34); 15: sleeping (n = 34)).
Assistive devices
All 88 subjects used a manual wheelchair; 72 of them (82%) used only a manual wheelchair, and 16 (18%) a combination of manual and power wheelchair. None of the subjects used a push-rim activated power-assisted wheelchair. Most subjects (68%) did not use any help or upper extremity assistive devices during daily transfers, whereas 28/88 subjects (32%) used additional help or assistive devices; 20 subjects occasionally and 8 regularly in every transfer. Fifteen subjects used a slide board, 13 had help from another person, 9 used a lift, and 4 used other kinds of assistance. Most car drivers, 58/67 (87%), lifted the wheelchair in and out of the car with no assistance.
Medical attention
More than half of the subjects with current shoulder pain (22/35) reported having sought medical attention for their problems, whereas 13/35 (37%) had not. Physiotherapists, physicians, (or both) commonly provided medical attention (16/22 and 15/22, respectively). Few had been treated by chiropractors (4/22) or other professionals (3/22). Of those with current shoulder pain who had sought medical attention, only 14/22 (64%) felt that their problems had been examined and diagnosed, but most subjects (21/22) had undergone some kind of conservative treatment, often multiple therapies, to relieve their shoulder pain. Treatments commonly received were; exercise (17/22), medication (15/22), rest (15/22) and heat (14/22). Few subjects who reported current shoulder pain or shoulder pain since becoming a wheelchair user (4/59, 7%) reported undergoing surgical treatment to relieve shoulder pain.
Discussion
This study found that shoulder pain is a common problem in a Swedish paraplegic population and that the symptoms are often chronic in nature. Of the subject characteristics studied, age was found to be associated with ongoing shoulder pain. The highest median intensities of shoulder pain according to the WUSPI were reported for daily activities such as pushing the wheelchair up ramps or inclines outdoors, loading the wheelchair into the car, lifting objects from an overhead shelf, and transferring to a car. The majority of subjects suffering from shoulder pain reported limitations regarding the ability to use the shoulder in daily activities and in sports and leisure activities. Upper extremity assistive devices were rarely used during wheelchair propulsion and relatively rarely used during wheelchair transfer. Most subjects with current shoulder pain had sought medical attention for their problems and often received conservative treatment, but more than one-third of these subjects felt that they had not been examined or diagnosed.
The strengths of the present study were the high response rate of 87% and the relatively homogenous patient group. After analysing the drop-outs regarding age and gender, we concluded that because the gender and age distribution in both groups is similar, the group of drop-outs probably had no effect on the results. One limitation of the study is the cross-sectional study design. In addition, a larger study group would be preferable, which could increase the statistical power to detect other factors that may be associated with shoulder pain. The lack of significant results for factors associated with shoulder pain should not be interpreted as evidence for an absence of association with shoulder pain. It would also have been preferable to use an existing uniform Swedish validity and reliability tested instrument designed to fit the paraplegic population, but no such instrument exists. The Swedish version of the section on patient characteristics and medical history and the WUSPI were considered to be the most suitable instrument, but to cover more aspects of shoulder pain, supplemental questions including general questions from the Swedish version of Shoulder Rating Questionnaire were added.
Pain prevalence
Upper extremity pain (shoulder, elbow, and hand) was found to be common after becoming a wheelchair user, which agrees with previous studies on paraplegic populations (3–7). The prevalence of current shoulder pain was also similar to that reported in other comparable studies on full-time wheelchair users with paraplegia and a similar age distribution and duration of injury (4). The only previous Swedish study of shoulder pain in subjects with paraplegia documented a similar prevalence to the one we found (7), whereas a higher prevalence (67%) was reported in a similar paraplegic population by Gironda et al. (6), although the response rate was low. Lack of information on age, duration of injury, injury level, and diagnosis, for instance, makes it difficult to compare present results in detail with several previous publications.
By using the inclusion criteria of normal motor and sensory function in the upper extremities according to the classification of ASIA and injury levels at T2 and below, the present study tried to exclude persons with impaired innervation of their upper extremity muscles and persons suffering from neuropathic pain.
Subject characteristics associated with shoulder pain
Shoulder pain appeared to increase with age in our studied subjects who had suffered from an SCI for at least one year. Gironda et al. (6) found time of wheelchair use (but not age) to be associated with current shoulder pain (OR = 1.03, 95% CI = 1.01–1.06). The clinical relevance of both studies is that ageing with an SCI seems to increase the risk of shoulder pain, indicating that shoulder pain is a general problem in the paraplegic population and that all patients ought to undergo a preventative regime.
Pain intensity in activities
The highest median intensities of shoulder pain according to the WUSPI in our study agreed with our clinical experience and the studies of Gironda et al. (6) and Samuelsson et al. (7). The highest pain intensity was reported for pushing the wheelchair up ramps or inclines outdoors, which involves high compression forces on the glenohumeral joint and loading of structures such as the rotator cuff muscles and the subacromial bursa. Lifting objects down from an overhead shelf and loading the wheelchair into the car are also demanding activities involving shoulder elevation and abduction and a possible risk of subacromial impingement. The WUSPI seems to be a useful instrument for determining the most painful activities on both an individual and a group level, for which prevention and treatment can be addressed.
Assistive devices
Even though modification of biomechanical load (e.g. education in joint protective techniques in daily activities and more frequent use of assistive devices) has been described as an essential part in prevention and treatment programmes of individuals with SCI (27–29), studies have found that changes in daily routines to reduce shoulder pain are rare (4). In line with previous studies (5, 6), we found a dominance of manual wheelchair use in the present study. Upper extremity assistive devices seemed to be an unused option for treatment and prevention of shoulder problems, since most subjects did not use upper extremity assistive devices during wheelchair propulsion and transfers. A more frequent use of assistive devises may therefore be a possible area for prevention and treatment without jeopardizing the independence of the individual.
Medical attention
Considering that the majority of subjects with current shoulder pain were suffering from long-lasting shoulder pain, the number of non-consulters was large. Other authors have also reported that an unsatisfactory low number of subjects seek and receive medical attention for shoulder problems (5, 27). Patient education on the importance of early detection and treatment in our sample seemed to be adequate, as did education on individual shoulder pathology, since some subjects felt they had not been examined or diagnosed despite seeking medical attention. In accordance with other studies (30), surgical treatment of shoulder pain was an unused treatment option in the present study. Even though shoulder surgery in individuals with SCI is not well evaluated, it might be valuable to improve co-operation between neurological and orthopaedic specialists, and to include a more structured examination from an orthopaedic viewpoint in the treatment programme. Treatment for current shoulder pain seemed to be unsatisfactory in alleviating shoulder pain since many subjects reported long-lasting pain for more than one year.
conclusion
Shoulder pain, often chronic in nature, is a common problem in wheelchair users with a thoracic SCI, and pain seems more likely to occur with increased age. Shoulder pain is a potential cause of activity limitations, both in daily activities and in sports and leisure activities. The findings of this study indicate a need to develop programmes for prevention, patient education, diagnosis and treatment, possibly including more frequent use of upper extremity assistive devices during transfer and wheelchair propulsion.
Acknowledgements
This work was supported by the Spinalis Foundation, the Promobilia Foundation, Karolinska University Hospital, and the Foundation for Survivors of Traffic Accidents and Polio in Stockholm. The authors thank the patients of the SCI Unit for their contribution and Jan Kowalski, statistician, for valuable help.
References
1. Apple D. Pain above the injury level. Top Spinal Cord Inj Rehabil 2001; 7: 18–29.
2. Gellman H, Sie I, Waters RL. Late complications of the weight-bearing upper extremity in the paraplegic patient. Clin Orthop Relat Res 1988; 233: 132–135.
3. Sie IH, Waters RL, Adkins RH, Gellman H. Upper extremity pain in the post rehabilitation spinal cord injured patient. Arch Phys Med Rehabil 1992; 73: 44–48.
4. Pentland WE, Twomey LT. Upper limb function in persons with long term paraplegia and implications for independence: part Ι. Paraplegia 1994; 32: 211–218.
5. Curtis KA, Drysdale GA, Lanza RD, Kolber M, Vitolo RS, West R. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil 1999; 80: 453–457.
6. Gironda RJ, Clark ME, Neugaard B, Nelson A. Upper limb pain in a national sample of veterans with paraplegia. J Spinal Cord Med 2004; 27: 120–127.
7. Samuelsson KAM, Tropp H, Gerdle B. Shoulder pain and its consequences in paraplegic spinal cord-injured, wheelchair users. Spinal Cord 2004; 42: 41–46.
8. Waters RL, Sie IH. Upper extremity changes with SCI contrasted to common aging in the musculoskeletal system. Top Spinal Cord Inj Rehabil 2001; 6: 61-68.
9. Bayley JC, Cochran TP, Sledge CB. The weight-bearing shoulder: the impingement syndrome in paraplegics. J Bone Joint Surg Am 1987; 69: 676–678.
10. Burnham RS, May L, Nelson E, Steadward R, Reid DC. Shoulder pain in wheelchair athletes. The role of muscle imbalance. Am J Sports Med 1993; 21: 238–242.
11. Escobedo EM, Hunter JC, Hollister MC, Patten RM, Goldstein B. MR imagining of rotator cuff tears in individuals with paraplegia. AJR AM J Roentgenol 1997; 168: 919–923.
12. Roach NA, Schweitzer ME. Does osteolysis of the distal clavicle occur following spinal cord injury? Skeletal Radiol 1997; 26: 16–19.
13. Boninger ML, Towers JD, Cooper RA, Dicianno BE, Munin MC. Shoulder imaging abnormalities in individuals with paraplegia. J Rehabil Res Dev 2001; 38: 401–408.
14. Lal S. Premature degenerative shoulder changes in spinal cord injury patients. Spinal Cord 1998; 36: 186–189.
15. Boninger ML, Dicianno BE, Cooper RA, Towers JD, Koontz AM, Souza AL. Shoulder magnetic resonance imaging abnormalities, wheelchair propulsion, and gender. Arch Phys Med Rehabil 2003; 84: 1615–1620.
16. Sinnott KA, Milburn P, McNaughton H. Factors associated with thoracic spinal cord injury, lesion level and rotator cuff disorders. Spinal Cord 2000; 38: 748–753.
17. Newsam CJ, Lee AD, Mulroy SJ, Perry J. Shoulder EMG during depression raise in men with spinal cord injury: the influence of lesion level. J Spinal Cord Med 2003; 26: 59–64.
18. Wylie EJ, Chakera TM. Degenerative joint abnormalities in patients with paraplegia of duration greater than 20 years. Paraplegia 1988; 26: 101–106.
19. Fullerton HD, Borckardt JJ, Alfano AP. Shoulder pain: a comparison of wheelchair athletes and nonathletic wheelchair users. Med Sci Sports Exerc 2003; 35: 1958–1961.
20. Finley MA, Rodgers MM. Prevalence and identification of shoulder pathology in athletic and nonathletic wheelchair users with shoulder pain: a pilot study. J Rehabil Res Dev 2004; 41: 395–402.
21. Maynard FM, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal cord 1997; 35: 266–274.
22. Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Development of the Wheelchair User´s Shoulder Pain Index (WUSPI). Paraplegia 1995; 33: 290–293.
23. Dahlgren G, Hjalmarsson U, Lundin-Olsson L. Reliabilitetstestning av den svenska versionen av Shoulder Rating Questionnaire, SRQ-S. [Reliability testing of the Swedish version of Shoulder Rating Questionnaire, SRQ-S.] Nordisk Fysioterapi 2002; 6: 134–143 (in Swedish).
24. Curtis KA, Roach KE, Applegate EB, Amart T, Benbow CS, Genecco TD, et al.. Reliability and validity of the Wheelchair User’s Shoulder Pain Index (WUSPI). Paraplegia 1995; 33: 595–601.
25. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993; 46: 1417–1432.
26. Minkel JL. Seating and mobility considerations for people with spinal cord injury. Phys Ther 2000; 80: 701–709.
27. Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord 1999; 37: 191–195.
28. Hastings J, Goldstein B. Paraplegia and the shoulder. Phys Med Rehabil Clin N Am 2004; 15: 699–718.
29. Kirshblum S. New rehabilitation interventions in spinal cord injury. J Spinal Cord Med 2004; 27: 342–350.
30. Goldstein B, Young J, Escobedo E. Rotator cuff repairs in individuals with paraplegia. Am J Phys Med Rehabil 1997; 76: 316–322.