OBJECTIVE: To examine whether the addition of either electroacupuncture or interferential electrotherapy to shoulder exercises would be more effective in the management of frozen shoulder.
DESIGN: A double-blinded, randomized, controlled trial.
METHODS: A total of 70 subjects were randomly allocated to receive either: (i) electroacupuncture plus exercise; (ii) interferential electrotherapy plus exercise; or (iii) no treatment (the control group). Subjects in groups (i) and (ii) received 10 sessions of the respective treatment, while the control group received no treatment for 4 weeks. Each subject’s score on the Constant Murley Assessment and visual analogue scale were recorded at baseline, post-treatment session and subsequent follow-up sessions.
RESULTS: In both the electroacupuncture and interferential electrotherapy groups, the Constant Murley Assessment score increased and the visual analogue scale score decreased significantly (both p < 0.001). No significant change was found in any outcome of the control group, and no significant difference was found between the 2 intervention groups (all p > 0.05). The observed improvement was well maintained in both intervention groups at least until the 6-month follow-up session.
CONCLUSION: Either electroacupuncture or interferential electrotherapy in combination with shoulder exercises is effective in treating frozen shoulder patients. However, no significant difference was found between these types of treatment.
Key words: frozen shoulder, acupuncture, interferential electrotherapy, rehabilitation.
J Rehabil Med 2008; 40: 166–170.
Correspondence address: Gladys Cheing, Assistant Professor, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong. E-mail: gladys.cheing@inet.polyu.edu.hk
Submitted September 4, 2006; accepted September 28, 2007.
INTRODUCTION
Frozen shoulder (or adhesive capsulitis) affects 2–5% of the population and is usually found in people in the age range 40–60 years (1). It usually results in pain, decreased range of motion, and muscle weakness (2). Persistent shoulder pain and compromised mobility may cause difficulty in performing activities of daily living or even lead to disability. Approximately 20% of the people suffers from shoulder pain due to either intrinsic or extrinsic origin accompanied by disability (3).
Acupuncture is a treatment modality that originated in China more than 3000 years ago and is gaining popularity in Western countries. It is believed that acupuncture works by releasing endogenous opioids in the body that relieve pain, by overriding pain signals in the nerves, or by allowing energy (qi) or blood to flow freely through the body (4). Electroacupuncture (EA), the delivery of a pulsed electric current via acupuncture needles, is considered further to enhance the effectiveness of acupuncture analgesia. Sun et al. (5) found that needle acupuncture plus exercise produced significantly greater improvement in pain and functional mobility than exercise alone for patients with frozen shoulder.
Interferential electrotherapy (IFE) is a common physiotherapeutic treatment modality used in Western countries. Its high carrier frequency (around 4000 Hz) produces lower impedance to the skin and allows deeper penetration into tissue (7). IFE predominately excites large-diameter nerve fibres and reduces the transmission of nociceptive signals through small-diameter nerve fibres to the spinal dorsal horn by presynaptic inhibition (8–9), thus achieving pain modulation in the higher centre. Some studies have shown that IFE is effective in the management of various pain conditions (10–12), but not much work has been done on shoulder conditions. Van der Heijden et al. (13) reported negative findings of using IFE as an adjunct treatment to exercise therapy for shoulder disorders. However, this could be explained by the choice of inappropriate treatment parameters. Therefore, the aim of the present study was to examine whether the addition of either EA or IFE to a standard shoulder exercise programme would lead to better clinical outcomes in the management of frozen shoulder.
METHODS
Study design
The study was a double-blind, randomized, controlled clinical trial. An independent assessor was blind to the group allocation.
Participants
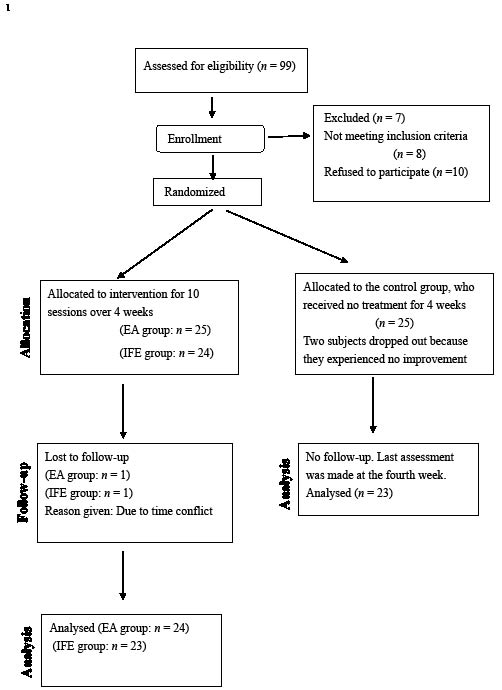
Seventy subjects (22 men, 48 women) with idiopathic frozen shoulder were diagnosed by an orthopaedic surgeon. Inclusion criteria were patients who reported localized pain over one shoulder, experienced night pain and had restricted active and passive shoulder motions. Exclusion criteria included a history of trauma, fractures, previous shoulder surgery, cervical or thoracic pain syndrome, complex regional pain syndrome, malignancies, on anti-coagulant therapy, or had received acupuncture treatment to the painful shoulder in the past 6 months. Written consent was obtained from all subjects. The study was approved by the local ethics committee. The subjects were randomly allocated into: (i) the EA group (n = 24); (ii) IFE group (n = 23); or (iii) control group (n = 23) (Fig. 1).
Fig. 1. Study design and flow of participants. EA: electroacupuncture; IFE: interferential electrotherapy.
Interventions
Electroacupuncture group. All the subjects in this group received EA treatment for 10 sessions over a 4-week period (2–3 times a week) from the same physiotherapist, who was accredited to practice acupuncture. The skin in the treatment area was first sterilized with an isopropyl alcohol skin wipe. Sterile stainless steel acupuncture needles (Dongbang Acupuncture Inc., Korea, DB100, size 0.30 × 40 mm) were then inserted 15–25 mm intramuscularly into 3 acupoints including one trigger point, one local point (LI 15: Jianyu), and one distal point (ST38: Tiaokou) (14). Trigger points were identified by areas of greatest tenderness around the painful shoulder that were determined on an individual basis. The selection of acupoints was based on recommendations made by Tukmachi (15). All needles were stimulated manually until the patient felt the sensation of de qi in that region. The 2 needles in the shoulder region (trigger point and LI 15) were connected to an EA device (Model: ES-160, ITO Co. Ltd, 3-3-3 Tpupta, al-Minami, Nerima-ku, Tokyo 176-8605, Japan) and stimulated with an alternating frequency of 2–100 Hz at a pulse duration of 100–400 μs for 20 min. The intensity of the stimulation was adjusted to a tolerance level of just below the pain threshold. The needle that was applied at the distal point ST38 (Tiaokou) was retained for 20 min, and was manually lifted and thrusted every 10 min.
In the first treatment session, the subjects were taught a home exercise programme. They were instructed to follow a chart and perform a standard set of shoulder mobilization exercises 5 times a day, which included 4 directions: (i) forward flexion – with the help of a overhead pulley system; (ii) external rotation – keeping the arm close to trunk, using a small bamboo to externally rotate the shoulder through pushing against the palm; (iii) horizontal adduction – pressing a horizontally adducted arm against the chest with the other arm to achieve horizontal adduction; and (iv) internal rotation – placing the affected arm behind the back and grasping one end of a towel, the other hand then pulling the opposite end of the towel to achieve maximum internal rotation. They were asked to practise the home exercise programme until the 6-month follow-up session. Each subject was given an exercise registration card to monitor his or her compliance with the home exercise programme.
Interferential electrotherapy group. The subjects in this group received IFE treatment for 10 sessions over 4 weeks. An IFE machine (a Phyaction Guidance E unit) delivered current swept from 80 to 120 Hz, and 4 suction-type electrodes were placed around the shoulder region in a coplanar arrangement. The intensity of the stimulation was adjusted to just below the pain threshold and the stimulation lasted for 20 minutes. The subjects were instructed to perform the same set of home exercise programmes as those in the EA group, and an exercise registration card was also given to each subject.
Control group. The subjects were recruited from a waiting list. They received no treatment for 4 weeks, but were invited to attend the assessment sessions at the baseline and at the end of the fourth week. Afterwards, they received regular physiotherapy treatments from other physiotherapists and no further data were extracted from them.
Outcome measures
Constant Murley Assessment (CMA) score. The CMA score is a reliable and valid instrument for assessing overall shoulder function, with low inter-rater and intra-rater error rates (16–17). It is a 100-point scale that is composed of 4 domains: (i) pain (15-point), (ii) activities of daily living (20-point), (iii) range of motion (40-point), and (iv) power (25-point) (16–18). The higher the score the better the overall functional performance, and vice versa.
Visual analogue scale (VAS). The VAS involves a 10-cm horizontal line with “No pain” anchored at the left end and “Pain as bad as it could be” anchored at the right end. The patient was asked to place a mark on the line that represented the severity of his or her pain at the moment.
Data analyses
The CMA score and VAS were both assessed at the baseline prior to the treatment, at the end of the treatment period (the fourth week), and at the 1-month follow-up, 3-month follow-up, and 6-month follow-up sessions. The CMA and VAS scores of the 3 groups obtained from the baseline to the post-treatment period, then from the 1, 3 and 6-month follow-up sessions were tested using a mixed model Analysis of Variance (ANOVA). Post hoc comparisons were carried out if significant differences existed. The level of significance was set at 0.05 for all analyses. Analyses were performed using SPSS for Windows statistical software (version 10.0, SPSS, Chicago, USA).
RESULTS
The age of participants ranged from 33 to 90 years. Their duration of onset ranged from 1 to 24 months (EA group: 6.71 (standard deviation (SD) 6.50) months; IFE group: 6.70 (SD 6.05) months; and control group: 8.26 (SD 7.94) months. Demographic data were compared and no significant difference was found between groups (all p-values > 0.05).
Constant Murley Assessment Scores
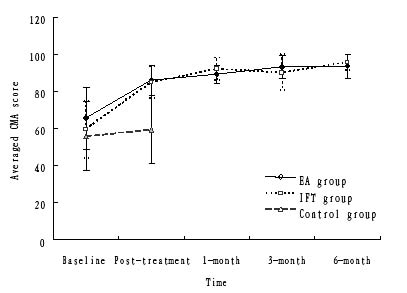
Fig. 2 shows the average CMA score measured at different time frames in the EA, IFE and control groups.
Fig. 2. Average Constant Murley Assessment (CMA) score measured at different time frames in the electroacupuncture (EA), interferential electrotherapy (IFE) and control groups. The error bars correspond to the standard deviation.
In the EA group, the average CMA scores improved significantly, from 65.5 (SD 16.7) at the baseline to 86.0 (SD 8.2) in the post-treatment session (the mean improvement was 31.5%; p < 0.001). The subjects in the IFE group showed similar improvement, with their CMA scores having increased from 59.6 (SD 15.4) at the baseline to 84.9 (SD 8.4) in post-treatment session (the mean improvement was 42.2%, p < 0.001). In contrast, the control group showed no significant change from the baseline to the fourth week (the mean improvement was 6.6%, p = 0.107).
A significant difference was found between the groups (p < 0.001). A post hoc comparison showed that significant differences came from the comparisons made between the EA and control group, and the IFE and control group (all p < 0.001). No significant difference was found between the EA and IFE groups (p = 0.138). On the fourth week, the subjects in the control group were discharged from the study and then received active treatment from other physiotherapists. Subsequent reassessments were made at the 1-, 3-, and 6-month follow-up sessions for the EA and IFE groups only.
Improvements were observed in the follow-up sessions. The average CMA scores of the EA group were 89.3 (SD 4.8) at the 1-month follow-up, 93.3 (SD 6.0) at the 3-month follow-up, and 93.8 (SD 6.4) at the 6-month follow-up sessions. For the IFE group, the average CMA score was 92.1 (SD 5.9) at the 1-month follow-up, 90.2 (SD 9.7) at the 3-month follow-up, and 95.5 (SD 4.1) at the 6-month follow-up sessions. A post hoc analysis showed that the CMA score at the 6-month follow-up session was significantly different from those at the post-treatment session for both the EA and IFE groups (p < 0.001). Therefore, the improvement in shoulder function seen in the post-treatment session could be well maintained in both treatment groups for at least up to the 6-month follow-up session.
Visual analogue scale
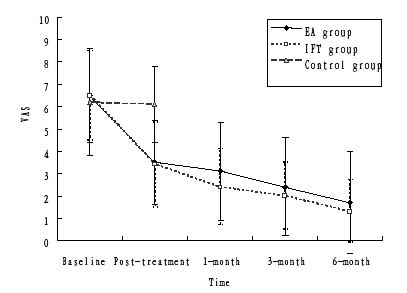
Fig. 3 shows the average VAS measured at different time frames in the EA, IFE and control groups. The VAS scores of the EA group were significantly reduced from 6.5 (SD 2.1) at the baseline to 3.5 (SD 1.9) in the post-treatment session (the mean improvement was 46.5%, p < 0.001). A similar trend was observed in the IFE group, with the VAS scores reduced from 6.5 (SD 2.0) at the baseline to 3.4 (SD 1.9) at the post-treatment measurement (the mean improvement was 48.6%, p < 0.001). In the control group, no significant change in VAS scores was found from the baseline to the fourth week (the mean improvement was 1.3%, p = 0.510). A significant between-group comparison was found (p < 0.001), and a post hoc analysis showed that the difference came from the comparisons made between either the EA or IFE groups to the control group. No significant difference was found between the EA and IFE groups (p = 0.801).
Fig. 3. Average visual analogue scale (VAS) measured at different time frames in the electroacupuncture (EA), interferential electrotherapy (IFE) and control groups. The error bars correspond to the standard deviation.
The VAS scores showed a progressive reduction over time in both treatment groups. The average VAS scores for the EA group were 3.1 (SD 2.2) at the 1-month follow-up, 2.4 (SD 2.2) at the 3-month follow-up, and 1.7 (SD 2.3) at the 6-month follow-up sessions. The average VAS scores for the IFE group were 2.4 (SD 1.7) at the 1-month follow-up, 2.0 (SD 1.5) at the 3-month follow-up, and 1.3 (SD 1.4) at the 6-month follow-up sessions. The treatment effect observed in the post-treatment session could be well maintained or even better than the measurement made at the post-treatment session.
Within the EA and IFE groups, a post hoc analysis showed that a significant reduction in the VAS score was found between the post-treatment session and the 6-month follow-up session.
DISCUSSION
These findings demonstrated that the addition of EA or IFE to exercise successfully alleviated shoulder pain and improved shoulder function for people with frozen shoulder. Ten sessions of EA produced a 31.5% increase in the scores and a 46.5% decrease in the VAS scores, however, no significant difference was found between the 2 active treatment groups. The observed improvements in pain and shoulder functions were comparable to similar previous studies (5, 19).
Guerra de Hoyos et al. (6) reported that EA produced a significantly greater reduction in pain intensity than did placebo acupuncture even at the 6-month follow-up. Our findings also demonstrated that CMA and VAS scores of the EA group were maintained by the 6-month follow-up. The carry-over results could be contributed by EA, home exercise programme, or natural recovery from the condition. It may be difficult to delineate which factor contributed most to the improvement.
Various mechanisms are involved in acupuncture analgesia, including a placebo component (20). Nevertheless, it is thought that the “de qi” sensation provoked by acupuncture is essential in producing the therapeutic analgesic effect (21). Needling is supposed to activate the small myelinated type II and III afferent nerve fibres, causing numbing and tingly “de qi” sensation. Afferent nerve fibres transmit these de qi impulses to the spinal cord, which in turn activates various parts of the central nervous system. In the spinal cord, acupuncture leads to the release of encephalin and dynorphin, which are natural pain-killing substances released by the body. These analgesic effects that are produced can be blocked by the opiate antagonist naloxone (21–22). In addition, acupuncture also activates the peri-aqueductal grey matter in the brain and increases the secretion of serotonin and noradrenaline (21). At the pituitary gland level, it leads to an increase in the release of adrenocorticotrophic hormones and beta endorphins (21). The needle is thought to act as a foreign body that may stimulate vascular and immunomodulatory factors (22). EA is thought to further enhance the acupuncture analgesic effects.
This is the first study to compare the effects of the addition of IFE or EA to shoulder exercises for people suffering from frozen shoulder. Our findings demonstrated that 10 sessions of IFE produced a 42.2% increase in CMA scores and a 48.6% reduction in VAS scores. This is contrast to the negative findings of using IFE for treating shoulder disorders, as reported by Van der Heijden et al. (13). The different results obtained in the 2 studies could be partly explained by the variation in patient selection and the choice of parameters. Van der Heijden et al. delivered IFE at 4 KHz with a frequency modulated between 60 and 100 Hz via 2 reusable hypoallergenic self-adhering electrodes. The present study delivered IFE at 80–120 Hz with suction cup electrodes.
Despite the wide use of IFE for managing different painful conditions, the analgesic mechanism of IFE is unclear. It is believed that the mechanisms might be similar to those in transcutaneous electrical nerve stimulation (23). The resulting current of IFE has a frequency that is modulated between 1 and 100 Hz, which is supposed to produce pain reduction through the gate control theory. Suction-type electrodes were used in the present study to produce gentle massaging effects. This stimulates cutaneous sensory nerves and causes slight vasodilatation (24), which may enhance the analgesic effects.
An exercise programme was added to both intervention groups that aimed to restore normal shoulder kinematics and muscle activity. Most of our subjects showed good compliance with the home exercise programme, as shown in the exercise registration cards. This may have contributed to the positive results achieved from the post-treatment session to the 6-month follow-up session. Clinically, patient education on self-care and exercise are crucial in achieving good functional outcomes and minimizing recurrences of frozen shoulder.
For ethical reasons, it was impossible to deprive patients of the opportunity to receive treatment for 6 months. Therefore, subjects from the control group received active treatment from the fifth week onwards, so no data from the control group could be provided in the follow-up sessions. This is a limitation of the present study. Also, we only showed the combined treatment effects of either EA or IFE with exercise, the net treatment effects produced by EA or IFE could not be determined from the present findings.
In conclusion, the addition of either EA or IFE to a specific shoulder exercise programme was similarly effective at reducing pain intensity and restoring shoulder function for people with frozen shoulder. Despite the different start times of the treatment (one month or more after the beginning of the onset of frozen shoulder), the results were the same for all. The improvement after 10 sessions of either EA or IFE was significantly greater than that observed with the control group at the end of the 4-week treatment period. The improvements observed in the EA and IFE group seem to be maintained until at least the 6-month follow-up session.
REFERENCES
1. Wolf JM, Green A. Influence of comorbidity of self-assessment instrument scores of patients with idiopathic adhesive capsulitis. J Bone Joint Surg Am 2002; 84: 1167–1172.
2. Lundberg BJ. The frozen shoulder. Acta Orthop Scand 1969; 119 Suppl l: 1–59.
3. Van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practise: incidence, patient characteristics and management. Ann Rheum Dis 1995; 54: 959–964.
4. Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005; 18: CD005319.
5. Sun KO, Chan KC, Lo SL, Fong DY. Acupuncture for frozen shoulder. Hong Kong Med J 200l; 7: 38l–39l.
6. Guerra de Hoyos JA, Andres Martin Mdel C, Bassas y Baena de Leon E, Vigara Lopez M, Molina Lopez T, Verdugo Morilla FA, et al. Randomised trial of long term effect of acupuncture for shoulder pain. Pain 2004; 112: 289–298.
7. Palmer S, Martin D. Interferential current for pain control. In: Kitchen S, editor. Electrotherapy evidence-based practice. Edinburgh: Churchill Livingstone; 2002.
8. Sato A, Schmidt RF. Somatosympathetic reflexes: afferent fibers, central pathways, discharge characteristics. Physiol Rev 1973; 53: 916–945.
9. Devor M. Peripheral and central nervous system mechanisms of sympathetic related pain. Pain Clinic 1995; 8: 5–14.
10. Werners R, Pynsent PB, Bulstrode CJ. Randomised trial comparing interferential electrotherapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine 1999; 24: 1579–1584.
11. Schmitz RJ, Martin DE, Perrin DH, Iranmanesh A, Rogol AD. Effect of interferential current on perceived pain and serum cortisol associated with delayed onset muscle soreness. J Sport Rehabil 1997; 6: 30–37.
12. DeDomenico GD. Pain relief with interferential electrotherapy. Aust J Physiother 1982; 28: 14–18.
13. Van der Heijden GJ, Leffers P, Wolters PJMC, Verheijden JJD, van Mameren H, Houben JP, et al. No effect of bipolar interferential electrotherapy and pulsed ultrasound for soft tissue shoulder disorders: a randomized controlled trial. Ann Rheum Dis 1999; 58: 530–540.
14. Gellman H, editor. Acupuncture treatment for musculoskeletal pain. A textbook for orthopaedics, anesthesia and rehabilitation. New York: Taylor & Francis; 2002.
15. Tukmachi ES. Frozen shoulder: a comparison of western and traditional Chinese approaches and a clinical study of its acupuncture treatment. Acupunct Med 1999; 7: 9–21.
16. Constant CR, Murley AH: A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987; 214: 160–164.
17. Conboy VB, Morris RW, Kiss J, Carr AJ. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br 1996; 78: 229–232.
18. Bankes MJ, Crossman JE, Emery RJ. A standard method of shoulder strength measurement for the constant score with a spring balance. J Shoulder Elbow Surg 1998; 7: 116–121.
19. Guerra J, Bassas E, Andres M, Verdugo F, Gonzalez M. Acupuncture for soft tissue shoulder disorders: a series of 201 cases. Acupunct Med 2003; 21: 18–22.
20. Razavi M, Jansen GB. Effects of acupuncture and placebo TENS in addition to exercise in treatment of rotator cuff tendinitis. Clin Rehabil 2004; 18: 872–878.
21. Ceniceros S, Brown GR. Acupuncture: a review of its history, theories, and indications. South Med J 1998; 91:1121–1125.
22. Sierpina VS, Frenkel MA. Acupuncture: a clinical review. South Med J 2005; 98: 330–337.
23. Cheing GLY, Hui-Chan CWY. Analgesic effects of transcutaneous electrical nerve stimulation and interferential currents on heat pain in healthy subjects. J Rehabil Med 2003; 35: 15–19.
24. Low J, Reed A, editors. Electrotherapy explained. Principle and practice. 2nd edn. Oxford: Butterworth Heinemann; 1998.