OBJECTIVE: To measure the effects of Bobath-based (BB) therapy on depression, shoulder pain and health-related quality of life (HRQoL) of patients during one year after stroke.
DESIGN: In a prospective, non-randomized design, the use of BB therapy was compared with a more task-oriented therapy and no BB therapy.
SUBJECTS: A total of 324 patients in 12 hospitals.
METHODS: Patients in the intervention group received BB therapy, whereas patients in the control group received no BB therapy and a more task-oriented therapy. HRQoL was measured using the SF-36; depression was measured with the Center of Epidemiological Studies Depression Scale and shoulder pain was measured with the Visual Analogue Scale at discharge, 6 and 12 months. Linear and logistic regression analyses were performed.
RESULTS: No effects of BB therapy on HRQoL or shoulder pain were found. After one year fewer patients were depressed in the BB group (30%) than in the non-BB group (43%); the adjusted odds ratio was 0.6 (95% confidence interval 0.3–1.0).
CONCLUSION: BB therapy did not have any effect on HRQoL or shoulder pain in stroke patients. Healthcare professionals should reconsider the use of BB therapy in the care of stroke patients.
Key words: stroke, Bobath therapy, health-related quality of life, depression, shoulder pain.
J Rehabil Med 2007; 39: 627–632
Correspondence address: Thora B. Hafsteinsdottir, Department of Neurology of the Rudolf Magnus Institute of Neurosciences, University Medical Center Utrecht, A.01.126, PO Box 85500, NL-3508 GA Utrecht, The Netherlands.
E-mail: t.hafsteinsdottir@umcutrecht.nl
Submitted May 30, 2006; accepted March 8, 2007
INTRODUCTION
Bobath-based (BB) therapy, also referred to as neurodevelopmental technique, is widely applied in stroke care (1). This technique aims to improve rehabilitation results of patients after stroke by stimulating the affected side and using reflex inhibiting positions and balance exercises to help patients to re-learn normal postural movement. The normalization of muscle tone represents the central aim of therapy (1). BB therapy, however, has been criticized for being costly and time-consuming, burdensome for patients and nurses, based on outdated theories, and for showing poor carry-over gains into real life (2, 3).
Health-related quality of life (HRQoL) is one of the most relevant outcomes in stroke research, and includes a person’s ability to engage in the activities of life, the satisfaction derived from these, including physical and emotional status and well-being (4). Stroke survivors generally experience much deterioration in HRQoL, which leaves them facing a multitude of challenges in restoring the highest HRQoL within the limitations of their residual impairment (5).
Depression is common after stroke, occurring in 10–40% of patients, and is associated with poor rehabilitation outcome and impedes the recovery process (6).
A painful shoulder is an important complication of stroke that interferes with recovery in up to 70% of patients (7). Various treatment methods have been studied, with contrasting findings on their effectiveness (8, 9).
Post-stroke rehabilitation interventions should improve not only the functional status of patients but also their HRQoL. Despite the paucity of studies supporting BB therapy, many studies have measured its effects by comparing the outcome of patients receiving BB therapy with other therapeutic approaches, such as traditional functional training, Electromyographic-biofeedback and Motor Relearning Programme (10–20). Of these studies, only 2 have shown positive effects on the patient’s functional status at discharge from hospital (16, 17). Other studies have shown no beneficial effects (10–12, 14, 15, 19, 21) and 2 have reported negative impacts, i.e. on functional outcome (13), and that patients receiving BB therapy stay considerably longer in hospital (ranging from 13 to 40 days longer) compared with those receiving no BB therapy (13, 20). However, many of these studies were hampered by methodological limitations. We recently investigated the impact of BB therapy on functional outcome in patients after stroke and found an adjusted odds ratio (OR) of 1.7 (95% confidence
interval (CI) 0.8–3.5) for poor outcome after one year, indicating no beneficial effects (22). In the present study we addressed the impact of BB therapy on HRQoL, depression and shoulder pain in patients over the course of one year after stroke.
METHODS
Design
With a prospective, non-randomized, parallel group design, 2 groups of patients after stroke from 12 hospitals were compared. In the experimental group, nurses and physiotherapists in 6 neurological wards used BB therapy, whereas the control group instead received a more task-oriented functional therapy and no BB therapy, as shown in the intervention studies (23, 24). Outcomes were assessed at discharge and after 6 and 12 months. Details of the study design have been described previously (22).
Subjects
The study focused on moderately disabled patients and disabled patients, because they are the most likely to benefit from rehabilitation intervention; using the following inclusion criteria; a diagnosis of ischaemic or haemorrhagic stroke (25), conscious at admission (Glasgow Coma Scale (GCS) > 14 (26), handicap at admission (Modified Rankin scale (MRS) > 3 (27), but not before the stroke onset (MRS < 3); no signs of dementia, measured with the Mini Mental Status Examination – 12 (MMSE > 7), informed consent and Dutch speaking. Patients were included within one week after stroke onset. Patients read and signed an Institutional Review Board / Ethics Committee approved informed consent before inclusion in the study.
Measurements
In the participating hospitals, specially trained research nurses conducted the baseline and discharge assessments. Patients were assessed when admitted to the stroke unit. Additional clinical details and demographic data were obtained from hospital records (Table I). Neurological examination was performed at admission. At follow-up, postal questionnaires were sent to the patients. Uniform study procedures were followed. Prior to the data collection, inter-rater reliability between the first author and the research assistants was measured, showing excellent agreement (kappa > 0.75).
HRQoL was assessed with the MOS 36-item short-form (SF-36), which is a self-administered questionnaire that has been validated for patients after stroke, containing 36 items within 8 domains, with scores from 0 to 100. An SF-score of 100 represents the best possible HRQoL (28). The physical functioning domain assesses limitations in physical activities such as walking and climbing stairs. The role physical and role emotional domains assess problems with work or other daily activities as a result of physical health or emotional problems. Bodily pain assesses limitations resulting from pain; vitality measures energy and tiredness. The social functioning domain examines the effect of physical and emotional health on normal social activities, and mental health assesses happiness, nervousness and depression. The general health perceptions domain evaluates the personal opinion of one’s health compared with that of one’s peers, as well as the expectations of changes in health. All domains are scored on a scale from 0 to 100 representing the best possible health state (28). Depression was measured with the Centre for Epidemiological Depression scale (CES-D). This is a 20-item scale, with 4 possible responses: 0 is “rarely or none of the time”, and 4 is “almost or all of the time”. Scores range from 0 to 60, with higher scores reflecting greater levels of depressive symptoms. A cut-off point of 16 was used, which showed good specificity (90%), sensitivity (86%) and a positive predictive value (80%) (29). Shoulder pain was measured with the Visual Analogue Scale (VAS), a 100-mm line. The patient was asked to indicate how much shoulder pain they had suffered in the last 24 h. A pre-defined VAS of 30 mm or higher was categorized as having considerable pain (30). The findings on functional outcomes have been presented in our previous study (22).
Treatment conditions
In the intervention group, BB therapy had already been implemented on the 6 wards before the start of the study. During the first phase of the study an intervention check was conducted to evaluate the nurses’ compliance with the BB instructions (23). Nurses (n = 144) were found to have adequate competence in BB nursing, as the mean score for each of these wards was above the preset limit of 60% (23). Also, the intervention of the physiotherapists in the 12 hospitals (n = 38) was measured with a questionnaire on their BB education and by means of a case vignette. Physiotherapists in the BB hospitals had sufficient competence in applying BB therapy, whereas in the non-BB hospitals they did not (24). In the control group, both nurses and physiotherapists had not followed courses on how to apply BB therapy and provided a more task-oriented functional care and no BB therapy, as shown by the findings of intervention studies (23, 24).
The patients in the intervention group continued to receive BB therapy after discharge, whereas the patients in the control group did not. This was confirmed by a survey conducted among the aftercare professionals. Also, a form was sent to the physiotherapist treating the patient after discharge, concerning the amount and type of therapy provided. This showed that the patients in the intervention group continued to receive BB therapy in nursing homes and rehabilitation centres after discharge, whereas the patients in the control group received no BB therapy.
The general quality of nursing care, not related to BB aspects of care, was measured on the 2 groups of wards in order to control for possible differences between the group of wards. An instrument was developed specifically for this purpose (31), based on 2 existing Dutch instruments (32, 33). Data were collected from the patients (n = 125), the nurses (n = 71) and hospital records (n = 125). No difference was found in the general quality of nursing care (p = 0.49), indicating good comparability between the groups (31).
Statistical analysis
Means and medians were calculated for outcomes at discharge and after 6 and 12 months. Mean differences were calculated for HRQoL (SF-36), depression (CES-D) and shoulder pain (VAS) with linear regression analysis, except for comparison of percentages of depression (CES-D) and shoulder pain (VAS), which were calculated with logistic regression analysis reporting OR. All effect estimates were adjusted for the differences at baseline between the groups on the following variables: age, living situation, education, MRS, Abbreviated MMSE, CES-D. Point estimates are given with corresponding 95% CI; if the neutral value of the point estimate (0 for mean differences and 1 for odds ratios) is contained in the 95% CI the result is not statistically significant (p > 0.05)).
All analyses were performed with SPSS statistical package software (version 12).
RESULTS
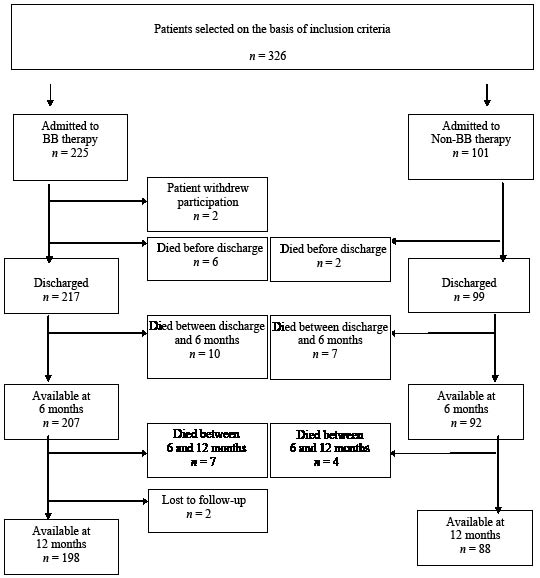
A total of 326 patients were included in the study. Two patients (BB group) withdrew from participation. The analysis was therefore based on data from 324 patients. One patient (BB group) was lost to follow-up (Fig. 1). The mean age for the BB group was 68 years (SD 13) and for the non-BB group 72 years (SD 11). The main characteristics of the patients are described in Table I.
Fig. 1. Details of patients included in the study. BB: Bobath-based therapy.
| Table I. Baseline characteristics of patients after stroke |
| | Bobath-based therapy | |
| | Yes (n = 223) | No (n = 101) | p-value |
| Interval between stroke onset and hospital admission, days mean (SD) | 0.3 (1.1) | 0.6 (2.4) | |
| Demographic characteristics |
| Female, n (%) | 101 (45) | 50 (50) | 0.481* |
| Age (years) mean (SD) | 68 (13) | 72 (11) | 0.001† |
| Living alone, n (%) | 75 (34) | 53 (53) | 0.001* |
| Qualifying stroke |
| Cerebral infarction, n (%) | 202 (91) | 91(90) | 0.328* |
| Intra-cerebral haemorrhage, n (%) | 21 (9) | 9 (9) | 0.328* |
| Motor function disorder |
| Can walk unassisted, n (%) | 6 (3) | 7 (8) | 0.032* |
| Left arm paresis, n (%) | 132 (59) | 53 (54) | 0.478* |
| Left leg paresis, n (%) | 130 (58) | 57 (57) | 0.996* |
| Right arm paresis, n (%) | 91 (41) | 44 (44) | 0.641* |
| Right leg paresis, n (%) | 89 (40) | 41 (41) | 0.907* |
| Hemianopia, n (%) | 64 (29) | 12 (12) | 0.001* |
| Apraxia, n (%) | 30 (14) | 12 (12) | 0.696* |
| Neglect, n (%) | 73 (33) | 10 (10) | 0.000* |
| Health status |
| GCS, median (IQR) | 14 (14–14) | 14(14–14) | 0.570‡ |
| MRS, median (IQR) | 4 (4–5) | 4 (4–5) | 0.008‡ |
| abMMSE, median (IQR) | 10 (8–11) | 9 (8–11) | 0.346‡ |
| CES–D, median (IQR) | 17 (14–20) | 16 (13–20) | 0.120‡ |
| Shoulder pain, VAS, mean (SD) | 14 (22) | 15 (23) | 0.706† |
| *χ2 test; †t-test; ‡Mann-Whitney test. GCS: Glasgow Coma Scale; MRS: The Modified Rankin Scale; abMMSE: Abbreviated Mini Mental Status Examination; CES-D: Center of Epidemiological Studies Depression Scale; VAS: Visual Analogue Scale; IQR: interquartile range; BB therapy: Bobath-based therapy; SD: standard deviation. |
The length of stay in hospital was 26 days for the BB group and 25 days for the non-BB group. The patients in the BB group received slightly more physiotherapy (5 times/week) and occupational therapy (2 times/week) than the non-BB group (physiotherapy 4 times/week; occupational therapy 1 time/week). More patients (34%) in the non-BB group were discharged home than in the BB group (30%). At 12 months, slightly more patients in the non-BB group were living at home (85%) compared with the BB group (84%) (Table II).
| Table II. Characteristics of therapy given during the hospitalization and transfer of patients |
| | Bobath-based therapy |
| Yes (n = 217) | No (n = 99) | p-value |
| Length of hospital stay days, median (IQR) | 26 (17–40) | 25 (16–34) | 0.417‡ |
| Physical therapy (times/week)
mean (SD) | 5 (2) | 4 (2) | 0.127† |
| Occupational therapy (times/week) mean (SD) | 2 (2) | 1 (2) | 0.000† |
| Speech language therapy (times/week) mean (SD) | 1 (2) | 1 (1) | 0.070† |
| Discharged from hospital to: | | | 0.084* |
| Home, mean (%) | 64 (30) | 34 (34) | |
| Nursing home, mean (%) | 74 (34) | 22 (22) | |
| Rehabilitation centre, mean (%) | 74 (34) | 37 (37) | |
| Other, mean (%) | 5 (2) | 6 (6) | |
| *χ2 test; †t-test; ‡Mann-Whitney test. IQR: interquartile range; SD: standard deviation. |
After simultaneous adjustment in a multivariate linear regression model for age, living situation, education, MRS score, MMSE score and CES-D score, no differences were found between the groups with respect to the HRQoL on any of the domains of the SF-36, either for 6 months or one year (Table III). The patients generally scored low on the physical functioning domain, where the median score for the BB group was 30 (interquartile range (IQR) 5–60) and for the non-BB group 25 (IQR 5–50). At 12 months the median score for this same domain for the BB group was 35 (IQR 10–60) and for the non-BB group 20 (IQR 10–50), with no significant differences between the groups. Also, for the emotional role limitation domain the median scores were low, with no differences between the groups. At 6 months, the median score both for the BB group and for the non-BB group was 33 (IQR 0–100 and 0–67, respectively). Again, at 12 months the median score for this domain for both groups was 33 (IQR 0–100). On the domain of bodily pain at 6 months, the median score was the same for both treatment groups; 62 (IQR 41–100), with an adjusted mean difference of 3.7 (95% CI –3.5 to 10.9), indicating no difference between the groups. At 12 months the median score for the BB group was 74 (IQR 49–100) and for the non-BB group 62 (IQR 41–100), with an adjusted mean difference of 4.7 (95% CI –2.9 to 12.3) (Table III).
Although more patients were found to be depressed (55%) in the BB group, than in the non-BB group (46%) at discharge, with adjusted OR of 1.3 (95% CI 0.8–2.2), these differences were not significant when adjusted for the confounding variables. At 6 months, 40% of the patients in the BB group were depressed, compared with 45% of the non-BB group, with adjusted OR of 0.7 (95% CI 0.4–1.2), showing no differences between the groups. At 12 months, the proportion of depressed patients was lower in the BB group (30%) than in the non-BB group (43%); the adjusted OR was 0.6 (95% CI 0.3–1.0). The overall percentage of depressed patients for both groups at 12 months was lower (33%) than at discharge (51%) (Table III).
No differences were found between the intervention and control groups on the variable of shoulder pain. At discharge 18% of the patients in the BB group experienced considerable shoulder pain (VAS ≥ 30 mm), compared with 22% of the non-BB group, with adjusted OR of 0.6 (95% CI 0.3–1.2), indicating no differences between the groups. At 6 months the proportion of patients with shoulder pain was somewhat larger for both BB group (22%) and non-BB group (28%). At 12 months 20% of the BB group and 19% of the non-BB group still had shoulder pain, with adjusted OR of 0.9 (95% CI 0.5–1.8) (Table III).
| Table III. HRQoL, depression and shoulder pain at discharge and follow-up |
| Outcome therapy | Bobath-based therapy | Adjusted difference* (95% CI) |
| Yes | No |
| Discharge | (n = 217) | (n = 99) | |
| Depression | | | |
| CES-D median (IQR) | 17 (14–21) | 16 (13–20) | 0.8 (–0.8–2.4) |
| Depressed, % (n) | 55 (115/210) | 46 (45/97) | 1.3 (0.8–2.2)† |
| Shoulder pain | | | |
| VAS mean (SD) | 14 (± 22) | 15 (± 23) | –3.1(–8.8–2.6) |
| Shoulder pain, % (n) | 18 (40/217) | 22 (22/99) | 0.6 (0.3–1.2)† |
| 6 months | (n = 206) | (n = 93) | |
| HRQoL SF-36 median (IQR) |
| Physical functioning | 30 (5–60) | 25 (5–50) | 1.8 (–4.8–8.5) |
| Physical role limitation | 0 (0–25) | 0 (0–25) | 2.2 (–10.6–6.2) |
| Emotional role limitation | 33 (0–100) | 33 (0–67) | 8.8 (–2.5–20.2) |
| Social functioning | 63 (38–88) | 63 (50–88) | 1.6 (–9.1–5.8) |
| Bodily pain‡ | 62 (41–100) | 62 (41–100) | 3.7 (–3.5–10.9) |
| Mental health | 68 (52–84) | 64 (41–84) | 2.4 (–2.9–7.8) |
| Vitality | 50 (35–65) | 50 (35–70) | 0.3 (–5.4–5.9) |
| General health perception | 47 (35–62) | 50 (35–65) | 2.8 (–7.7–2.1) |
| Change in General Health | 75 (50–100) | 75 (50–100) | 1.5 (–5.6–8.5) |
| Depression | | | |
| CES-D median (IQR) | 15 (12–20) | 16 (12–20) | 0.9 (–2.9–1.2) |
| Depressed, % (n) | 40 (82/203) | 45 (42/93) | 0.7 (0.4–1.2)† |
| Shoulder pain | | | |
| VAS mean (SD) | 18 (26) | 19 (25) | –2.0 (–8.7–4.7) |
| Shoulder pain, % (n) | 22 (46/207) | 28 (26/93) | 0.6 (0.3–1.2)† |
| 12 months | (n = 198) | (n = 85) | |
| HRQoL SF-36 median (IQR) |
| Physical functioning | 35 (10–60) | 20 (10–50) | 3.5 (–3.7–10.5) |
| Physical role limitation | 0 (0–50) | 0 (0–50) | 1.4 (–8.4–11.1) |
| Emotional role limitation | 33 (0–100) | 33 (0–100) | 2.9 (–9.2–15.1) |
| Social functioning | 63 (38–88) | 63 (50–88) | 0.7 (–8.4–6.9) |
| Bodily pain‡ | 74 (49–100) | 62 (41–100) | 4.7 (–2.9–12.3) |
| Mental health | 68 (52–84) | 68 (51–84) | 2.9 (–2.9–8.7) |
| Vitality | 55 (35–70) | 45 (35–63) | 6.1 (–0.2–11.9) |
| General health perceptions | 50 (35–60) | 45 (35–62) | 0.8 (–4.3–5.9) |
| Change in general health | 50 (25–75) | 50 (00–75) | 1.8 (–11.0–7.5) |
| Depression | | | |
| CES-D median (IQR) | 14 (10–18) | 16 (12–19) | 1.1 (–2.9–0.7) |
| Depressed, % (n) | 30 (60/198) | 43 (38/88) | 0.6 (0.3–1.0)† |
| Shoulder pain | | | |
| VAS mean (SD) | 15 (24) | 15 (25) | 0.0 (–6.7–6.7) |
| Shoulder pain, % (n) | 20 (39/198) | 19 (17/88) | 0.9 (0.5–1.8)† |
| *Adjusted effect measures: mean difference was calculated with linear regression analysis except for comparison of percentages logistic regression analysis (†) was conducted and odds ratios reported. All effect estimates are adjusted for differences at baseline between the groups on the following variables: age, living situation, education, Modified Rankin Scale, Abbreviated Mini Mental Status Examination, and CES-D. ‡In the domain of Bodily Pain (SF-36): 0 = much bodily pain; 100 = no bodily pain. CES-D: Center of Epidemiological Studies Depression Scale, scores 0–40 (score > 16 means depression); VAS: Visual Analogue Scale 0–100, low score = low level of shoulder pain; SF-36: Short Form 36, scores 0–100 (0 = maximum reduction in HRQoL; 100 = no reduction in HRQoL); IQR: interquartile range; HRQoL: Health Related Quality of Life; SD: standard deviation. |
DISCUSSION
The application of BB therapy provided by nurses and physiotherapists in the daily care of patients after stroke has no impact on HRQoL or shoulder-pain; after one year fewer patients were depressed in the BB group (adjusted OR 0.6; 95% CI 0.3–1.0). The lack of benefit on shoulder pain is disappointing, because many BB techniques focus on protection of the shoulder.
Most earlier studies have not demonstrated any benefits of BB therapy on the various outcomes, such as HRQoL (13), functional status (11, 12, 14, 18, 20, 34, 35), depression (12) or arm function (19). Only 2 studies have showed improved functional status as a result of BB therapy; one small retrospective study (16) and one comparing BB therapy with an orthopaedic treatment (17). Another 2 studies have reported negative results (13, 20), showing that BB patients stayed 40 days longer in hospital than patients who received traditional functional training (20) and that BB patients stayed 13 days longer in hospital than patients treated according to the Motor Relearning Programme (13). This indicates that the choice of therapy might have major cost and effectiveness implications for programme planning in the care of patients after stroke.
The lack of beneficial effects demonstrated by previous studies has been explained by small samples, and by inclusion of severely disabled patients. Despite the fact that our study dealt with these limitations, no beneficial effects were found.
A limitation of the present study may be the fact that it was impossible to randomize the patients between treatment groups, because a ward may or may not use BB therapy. To address the possible incomparability between the groups, extensive data were collected on determinants of outcome and the effect estimates were adjusted for group differences.
One previous study has measured the effects of BB therapy on HRQoL of patients with stroke in the acute phase of rehabilitation, also showing no effects (13). No differences were found between the groups on the domains of the SF-36 and no improvements were demonstrated during the study. The findings show that the patients generally experienced their HRQoL as low on all domains, both at 6 and 12 months, when compared with the normal values for people in the Netherlands in the same age group. This difference was largest for the domain of physical functioning, where the median score for the BB group was 30 (IQR 5–60) and for the non-BB group 25 (IQR 5–50), whereas the general Dutch population of the same age the scores ranged between 60 and 67 for this domain. Previous studies have reported reduced HRQoL after stroke. As long as 5 years after stroke, 61% of patients experienced decreased global HRQoL, mainly on the domains of sexual and leisure satisfaction. Nearly 30% of the non-impaired participants reported decreased global life satisfaction (36), showing that patients do not cope psychosocially with the stroke as such, nor with its sequel. This indicates that healthcare professionals need to focus therapy and treatment not only on the physical results of the stroke, but on all aspects of HRQoL and on the continuation of therapy provided in the long term.
Our study showed no effects of BB therapy on depression, as measured with the CES-D (discharge and 6 months). This was similar to the low median scores on the emotional role limitation domain of the SF-36 at 6 and 12 months. We cannot explain the difference in the prevalence of depression after one year, mainly because there were no differences at discharge and after 6 months. Only one study has measured the effects of BB therapy on depression in patients after stroke, showing no beneficial effects (12). The high prevalence of depression is likely to have a negative effect on the patient’s participation in rehabilitation and associated rehabilitation outcome. However, despite the fact that a high proportion of the total group was depressed at discharge (51%), there was an overall decline in depression experienced by the patients during the year (37%). This might suggest that after chronic stroke patients may improve their coping mechanisms with increasing time post-stroke. However, the high prevalence of depression may be explained by a lack of attention being paid to the psychological consequences of stroke by healthcare providers. Our findings underline the importance of early assessment and identification of depression after stroke and the importance of psychosocial support to be provided both by the rehabilitation team and from the environment in the long term.
Our study showed no beneficial effects of BB therapy on shoulder pain. Only 2 studies have measured the effects of BB therapy on shoulder pain, showing inconclusive evidence for its effects (18, 37).
The present study provides evidence that the widely used BB therapy does not improve the HRQoL of patients after stroke. We should bear in mind that BB therapy has operated on the basis of strong beliefs in pathophysiological concepts without scientific evidence of its efficacy, as shown by the increasing number of studies conducted. Based on the evidence from this and previous studies, we recommend that healthcare professionals focus therapy on all aspects of HRQoL. The patients in the control group received a more task-oriented functional care and no BB therapy. Evidence from earlier studies shows that recovery after stroke may best be stimulated by functional and task-oriented training, where the patient practises motor tasks under similar conditions of strength, speed and accuracy as in real life and with similar cognitive demands and where the patient is assisted in relearning motor control (38). To achieve this, healthcare professionals, physiotherapists, nurses and others need to collaborate according to these principles. More daily care situations with patients after stroke need to be used for rehabilitation purposes. Therefore, in collaboration with the rehabilitation team, nurses need to take a more active part in activating and training patients during daily care situations.
Of utmost importance is the potential negative effect of depression on the patient’s participation in rehabilitation and the associated rehabilitation outcome (6, 39). The data reveal that the patients in both groups experience real chronic psychosocial problems, on which healthcare professionals need to focus their attention. Based on the findings of this and previous studies, we recommend a structured approach focusing on early assessment and identification of depression after stroke. By involving nurses in screening for depression, its symptoms may be identified earlier and timely treatment started. This is likely to improve functional status and overall recovery, rehabilitation results and HRQoL of these patients and may lead to a decrease in healthcare costs.
The findings of this study, together with previous evidence, and taking the personal intensity and costs of BB therapy into account, shows that there is no place for this therapy in the stroke unit or in today’s healthcare. New efforts should concentrate on the evaluation of other evidence-based interventions in the field of rehabilitation.
ACKNOWLEDGEMENTS
The authors thank the following members of the Dutch Bobath Study Group for recruitment of patients and for facilitating the study: BovenIJ Hospital Amsterdam: Emmy Berends, Els Jansen, Maureen Koster, Yvette Schotsman, Ada Wimmers; Canissius Wilhelmina Hospital Nijmegen: Roel Dousi; Elizabeth Hospital Tilburg: Marcel Boonen, Cindy Franssen, Wim van Veenendaal; Gemini Hospital Den Helder: Hanneke Kuiper, Petra Schop; Kennemer Hospital Haarlem: Marion Baars, Anita
Sanders; Leyenburg Hospital Den Haag: Yvonne Drabbe, Karin
Gerbrands; Martini Hospital Groningen: Attie Nauta, Karin Strijker, Jantje Veen; VU University Medical Centre: Marian Baartscheer, Janine Boer, Lies Braam, Kees Goverde, Ans Kupper-Steenstra, Lies van der Weide; Spaarne Hospital Haarlem: Annemiek Koppenhol, Petra Romijn; University Medical Centre Nijmegen: Paul van Keeken, Henk Muessen, Theo de Waal, Jose van Welie; University Medical Centrum Utrecht: Caroline Ackermans, Florus Waszink; Zaans Medical Centrum Zaandam: Carien Biersteker, Anneke Mak, Els Scheepbouwer, Geert Schilstra.
This study was supported by grants from the University Medical Center Utrecht and the Janivo Foundation, Zeist, The Netherlands.
REFERENCES
1. Lennon S, Baxter D, Ashburn A. Physiotherapy based on the Bobath concept in stroke rehabilitation: a survey within the UK. Disabil Rehabil 2001; 15: 254–262.
2. Latash MA, Anson JG. What are “normal movements” in atypical populations? Behav Brain Sci 1996; 19: 55–106.
3. Davidson I, Waters K. Physiotherapists working with stroke patients: a national survey. Physiotherapy 2000; 86: 69–80.
4. Post MW, de Witte LP, Schrijvers AJ. Quality of life and the ICIDH: towards an integrated conceptual model for rehabilitation outcomes research. Clin Rehabil 1999; 13: 5–15.
5. Niemi ML, Laaksonen R, Kotila M, Waltimo O. Quality of life 4 years after stroke. Stroke 1988; 19: 1101–1107.
6. van de Weg FB, Kuik DJ, Lankhorst GJ. Post-stroke depression and functional outcome: a cohort study investigating the influence of depression on functional recovery from stroke. Clin Rehabil 1999; 13: 268–272.
7. Bender L, McKenna K. Hemiplegic shoulder pain: defining the problem and its management. Disabil Rehabil 2001; 23: 698–705.
8. Pomeroy VM, Niven DS, Barrow S, Faragher EB, Tallis RC. Unpacking the black box of nursing and therapy practice for post-stroke shoulder pain: a precursor to evaluation. Clin Rehabil 2001; 15: 67–83.
9. Snels IA, Beckerman H, Lankhorst GJ, Bouter LM. Treatment of hemiplegic shoulder pain in the Netherlands: results of a national survey. Clin Rehabil 2000; 14: 20–27.
10. Dickstein R, Hocherman S, Pillar T, Shaham R, Stern FM, Gorga D. Stroke rehabilitation. Three exercise therapy approaches. Phys Ther 1986; 66: 1233–1238.
11. Mulder T, Hulstijn W, van der Meer J. EMG feedback and the restoration of motor control. A controlled group study of 12 hemiparetic patients. Am J Phys Med 1986; 65: 173–188.
12. Wagenaar RC, Meijer OG, van Wieringen PC, Kuik DJ, Hazenberg GJ, Lindeboom J, et al. The functional recovery of stroke: a comparison between neuro-developmental treatment and the Brunnstrom method. Scand J Rehabil Med 1990; 22: 1–8.
13. Langhammer B, Stanghelle JK. Bobath or Motor Relearning Programme? A comparison of two different approaches of physiotherapy in stroke rehabilitation: a randomized controlled study. Clin Rehabil 2000; 14: 361–369.
14. Logigian MK, Samuels MA, Falconer JA, Agar R. Clinical exercise trial for stroke patients. Arch Phys Med Rehabil 1983; 64: 364–367.
15. Basmajian JV, Gowland C, Brandstater ME, Swanson L, Trotter J. EMG feedback treatment of upper limb in hemiplegic stroke patients: a pilot study. Arch Phys Med Rehabil 1982; 63: 613–616.
16. Lewis NA. Functional gains in CVA patients: a nursing approach. Rehabil Nurs 1986; 11: 25–27.
17. Wang RY, Chen HI, Chen CY, Yang YR. Efficacy of Bobath versus orthopaedic approach on impairment and function at different motor recovery stages after stroke: a randomized controlled study. Clin Rehabil 2005; 19: 155–164.
18. Luke C, Dodd KJ, Brock K. Outcomes of the Bobath concept on upper limb recovery following stroke. Clin Rehabil 2004; 18: 888–898.
19. Platz T, Eickhof C, van KS, Engel U, Pinkowski C, Kalok S, et al. Impairment-oriented training or Bobath therapy for severe arm paresis after stroke: a single-blind, multicentre randomized controlled trial. Clin Rehabil 2005; 19: 714–724.
20. Lord JP, Hall K. Neuromuscular re-education versus traditional programs for stroke rehabilitation. Arch Phys Med Rehabil 1986; 67: 88–91.
21. van Vliet P, Lincoln NB, Robinson E. Comparison of the content of two physiotherapy approaches for stroke. Clin Rehabil 2001; 15: 398–414.
22. Hafsteinsdóttir TB, Algra A, Kappelle LJ, Grypdonck MHF. Neurodevelopmental treatment (NDT) after stroke: a comparative study. J Neurol Neurosurg Psychiatry 2005; 76: 788–792.
23. Hafsteinsdóttir TB, Grypdonck M. NDT-nursing competence measured with nurses in the rehabilitation of stroke patients. J Neurosci Nurs 2004; 36: 289–294.
24. Hafsteinsdóttir TB, van Meeteren N, Grypdonck M. Is Bobath therapy used by physiotherapists in the care of stroke patients? Adv Physiother 2005; 7: 176–182.
25. World Health Organization. Recommendations on stroke prevention, diagnosis, and therapy: report of the WHO Task Force on Stroke and other cerebrovascular disorders. Stroke 1989; 20: 1407–1431.
26. Teasdale G, Murray G, Parker L, Lennet B. Adding up the Glasgow Coma Scale. Acta Neurochi (Wien) 1979; 28: 13–16.
27. Bamford JL, Sandercock PAG, Warlow CP, Slattery J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1989; 20: 828.
28. Ware JEjr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483.
29. Radloff LS, Teri L, editors. Use of the Center for Epidemiological Studies Depression scale with older adults. Clinical Gerontology. New York: The Hawthorne Press; 1986, p. 119–136.
30. Turner-Stokes L, Rusconi S. Screening for ability to complete a questionnaire: a preliminary evaluation of the AbilityQ and ShoulderQ for assessing shoulder pain in stroke patients. Clin Rehabil 2003; 17: 150–157.
31. Hafsteinsdóttir TB, Kruitwagen C, Strijker K, Van der Weide L, Grypdonck M. Assessing quality of nursing care as a confounding variable in an outcome study on Neurodevelopmental treatment. J Nurs Care Quality in press.
32. de Heide M, van de Mortel M. Measuring the quality of care with paralyzed patients: an instrument for measuring quality of care in a rehabilitation center. [Het meten van zorgkwaliteit bij dwarslesie-revalidanten; een kwaliteitsinstrument voor het revalidatiecentrum.] Lochem: De Tijdstroom; 1992 (in Dutch).
33. Visser G, Hollands L, de Bekker J, van Bergen B. The development and feasibility of an instrument for measuring the quality of nursing care in hospitals. [Beslag ten eis – Ontwikkeling en gebruik van referentiekaders voor verpleegkwaliteit in algemene ziekenhuizen.] Lochem: De Tijdstroom; 1992 (in Dutch).
34. van Vliet PM, Lincoln NB, Foxall A. Comparison of Bobath based and movement science based treatment for stroke: a randomised controlled trial. J Neurol Neurosurg Psychiatry 2005; 76: 503–508.
35. Salter J, Camp Y, Pierce LL, Mion LC. Rehabilitation nursing approaches to cerebrovascular accident: a comparison of two approaches. Rehabil Nurs 1991; 16: 62–66.
36. Viitanen M, Fugl-Meyer KS, Bernspång B, Fugl-Meyer AR. Life satisfaction in long-term survivors after stroke. Scand J Rehabil Med 1988; 20: 17–24.
37. Chantraine A, Baribeault A, Uebelhart D, Gremion G. Shoulder pain and dysfunction in hemiplegia: effects of functional electrical stimulation. Arch Phys Med Rehabil 1999; 80: 328–331.
38. Van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, Van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil 2004; 18: 833–862.
39. Nannetti L, Paci M, Pasquini J, Lombardi B, Taiti PG. Motor and functional recovery in patients with post-stroke depression. Disabil Rehabil 2005; 27: 170–175.