OBJECTIVE: The aims of this study were to investigate the time-course of depressive mood in patients with coronary artery disease during a secondary prevention rehabilitation program, and to analyse how different pre-treatment levels of depressive mood during a treatment phase were related to the degree of lifestyle change at 36 months follow-up.
SUBJECTS: The study group comprised 109 of the original 183 consecutive coronary artery disease patients (91 male and 18 female) of whom 48 recently had experienced an acute myocardial infarction, 36 had been treated with coronary bypass surgery, 13 with percutaneous transluminal coronary angioplasty, and 12 had angina pectoris that had not been invasively treated. The subjects were divided into 3 subgroups based on their pre-treatment level of depressive mood.
METHODS: Depressive mood was assessed at baseline, after 4 weeks and 12 months, using the depression subscale of the Hospital Anxiety and Depression scale. Lifestyle changes analysed included diet, smoking, relaxation (stress management) and exercise.
RESULTS: Overall depressive mood ratings were significantly lower, both at the 4-week and 12-month assessments, compared with baseline, with the greatest improvements in patients with higher Hospital Anxiety and Depression measured depression. Original levels of depressive mood were not found to influence change of lifestyle habits during a 36-month follow-up period.
CONCLUSION: Depressive mood might not be an obstacle to lifestyle changes when participating in a behaviourally oriented rehabilitation program including exercise-training, which might be a component important for improved depressive mood.
Key words: depressive mood, depression, CAD, rehabilitation, lifestyle change.
J Rehabil Med 2007; 39: 412–417
Correspondence address: Eva Söderman, Department of
Social Sciences MidSweden University, SE-831 25 Östersund, Sweden. E-mail: eva.soderman@miun.se
Submitted April 20, 2006; accepted December 28, 2006
Introduction
Depression is highly prevalent in patients with coronary artery disease (CAD) (1) and generally has a negative impact on important coronary end-points, such as functioning (2–3) and recurrence of cardiac events (4), as well as on lifestyle changes. Ziegelstein et al. (5) found that depressed patients were less successful in reducing stress, and had lower adherence to a low-fat diet and regular exercise 4 months after acute myocardial infarction (AMI). Mayou et al. (3) reported that patients who were depressed in the hospital after AMI were more likely than non-depressed patients to report less exercise. They were also less successful in changing their diet and in maintaining smoking cessation at a 12-month follow-up.
The effects of cardiac rehabilitation interventions on depression have not been unequivocal. Several evaluations (e.g. 6–12) including some controlled studies have demonstrated beneficial effects on depressive mood. Other controlled trials have, however, resulted in less favourable results and often failed to influence depression in patients with CAD (13–19).
In an earlier study Lisspers et al. (20) reported a decreased level of Beck Depression Inventory (BDI)-measured depression after a 4-week in-patient phase in 40 patients with CAD following a 12-month behaviourally oriented rehabilitation program. At the end of the rehabilitation period this reduction was maintained among patients who at the start of the program were considered mildly depressed. On the other hand, patients with pre-treatment BDI-scores suggesting clinical depression levels relapsed to baseline levels. However, when diagnosing or measuring depression in patients with physical diseases, it is important to consider that symptoms of depression (e.g. fatigability, sleep disturbance and work inhibition) may as well be symptoms of the physical disease (21–22). Using the BDI (23) divided into a physical and a non-physical subscale, as suggested by Söderman & Lisspers (22), Lisspers et al. (20) reported that the observed relapse to high BDI scores among clinically depressed subjects was true only for the emotional/cognitive symptoms, while the physical symptoms were improved. In spite of this differential long-term development, subgroups did not differ on any of the lifestyle habits assessed (diet, smoking, relaxation and exercise).
Another frequently used inventory, developed specifically to detect emotional disturbances in non-psychiatric patients, is the Hospital Anxiety and Depression scale (HAD) (24). The HAD covers only non-physical items, all related to anhedonia, or absence of positive affect, on the assumption that physical symptoms may be related to the underlying medical disorder. The HAD has been used in several CAD rehabilitation studies (8–11).
The present study was designed partially to replicate our previous study (20) in a larger sample using the HAD scale for the assessment of levels of depressive mood. Consequently, the aim was to investigate the time-course of depressive mood in patients participating in a 12-month secondary prevention rehabilitation program and to analyse how different pre-treatment levels of depressive mood were related to the degree of lifestyle change during follow-ups.
MethodS
Patients
The final study group comprised 109 patients recruited consecutively and entering the program during 1995. To be eligible for the study, subjects had to fulfil the following inclusion criteria: (i) AMI, coronary artery bypass surgery (CABG) or percutaneous transluminal coronary angioplasty (PTCA) as the patients last diagnosis at the most 6 months before the start of the program, (ii) age below 60 years, (iii) employed, (iv) able to perform a bicycle ergometer test with a minimum capacity of 70 Watts, (v) absence of any other physical or psychiatric disease that would interfere with participation in the program.
Of the originally 183 patients, 74 (40%) patients were excluded from the study for different reasons. One patient refused to participate in the study at the start of the program, and for 15 patients pre-treatment data was missing due to administrative mistakes at the rehabilitation centre. At the 4-week and 12-month assessments data was not available for another 33 and 25 patients, respectively, due to the patients not having returned the questionnaires in spite of several reminders.
Of the remaining 109 patients (91 male and 18 female), 48 (44%) had recently experienced an AMI, 36 (33%) had recently been treated with CABG, and 13 (12%) with PTCA, and 12 (11%) patients suffered from angina pectoris, who had not been invasively treated. The minimum duration from the clinical coronary event to inclusion in the program was 2 weeks, 4 weeks and 6 weeks for PTCA, CABG and AMI, respectively, and the maximum duration was 6 months.
The rehabilitation program
The rehabilitation program used behaviourally oriented methods to promote long-term lifestyle behaviour changes (25). Lifestyle areas covered in the intervention included stress management (relaxation), diet, smoking and exercise habits. The program, which had a total duration of 12 months, started with a 4-week residential stay at the intervention unit, during which time a combination of group-oriented (5–8 participants) and individual intervention formats was used in lectures, discussion seminars and practical skills training. The participants were also given daily “homework” assignments in all lifestyle areas to be performed individually between the group sessions.
Each participant was assigned a specific staff member as a “case manager”, together with whom he/she had a series of individual, structured interview sessions. The aim of these sessions was to achieve an individualization of all material covered elsewhere and, hence, to promote motivation and preparedness for behaviour change. Spouses were invited to participate in the program during the third week.
After the in-patient phase, the intervention was continued with an 11-month home-based maintenance phase including regular follow-up contacts by post and telephone between the patient and his or her “case manager”. During the first 3 months after departure, patients kept a daily self-observation diary of their diet, smoking, relaxation and exercise habits. The diaries were posted to the “case manager” every fortnight, and feedback was sent back to the patients in form of graphs showing the behaviour change progress. From the fourth to the eleventh months such diaries were sent to the intervention unit and feedback was returned on a monthly basis. In addition, results of any medical check-ups were sent to the intervention unit. All this material formed the basis for telephone contacts between the nurse and the patient for verbal feedback, problem-solving and re-planning on at least 3 pre-planned occasions (3, 8 and 11 months after leaving the intervention unit).
The program was an exclusive CAD rehabilitation program and was not originally designed to include special treatment for depression. However, the cognitive-behavioural oriented program included components that might have some beneficial influences on depressive mood.
Assessments
The assessment procedures followed the standard protocol of the project described earlier (25) and were performed at the start of the program, after the 4-week in-patient intervention phase and at the 12-, 24- and 36-month follow-ups.
Depressive mood was measured using the depression subscale (HADD) of the HAD (24), which apart from the depression subscale also comprises an anxiety (HADA) subscale. The 2 subscales contain 7 items each on a 4-point Likert scale (ranging from 0 to 3). Zigmond & Snaith (24) suggested 2 cut-off scores for detecting anxiety and depression, respectively, 8 for doubtful cases and 11 for definite cases. There is, however, no single generally accepted cut-off score for the HAD (26), or cut-off scores corresponding to the “mild” and “clinical” depression of the BDI (23). Thus, in this study cut-off scores of HADD were calculated using the same proportions of subjects in each category of depressive mood (53% without, 28% with mild degree and 19% with higher degree of depressive mood) as in the study by Lisspers et al. (20) utilizing the BDI. This resulted in the operationally defined cut-off score of 5 for “mild degree”, and 9 for “higher degree” of depressive mood.
At baseline and at the 12-, 24- and 36-month follow-ups, different measures of lifestyle habits (diet, smoking, relaxation and exercise habits) were assessed using a self-report questionnaire developed for the project (25). Diet questionnaire data was analysed in terms of a crude diet index based on the average item scores (0–3) on questions regarding the type of food generally eaten (low-fat foods; high-fat foods; vegetables and fruits; fibre rich foods; root vegetables) emphasizing high-fat foods intake through multiplying the score by a factor of -3. Smoking was analysed in terms of number of cigarettes smoked per day. The frequency of relaxation was the average number of relaxation sessions over 5 minutes in length per week. Exercise occasions were defined as efforts corresponding to at least a brisk walk for 20 minutes or more and were analysed as frequency per week.
Statistical analyses
Differences between groups were calculated using one-way ANOVA and χ2 test for continuous and categorical variables, respectively. In order to eliminate pre-treatment differences, one-way ANCOVAs, with the baseline level of the dependent variables as covariates, were used. Differences between subgroups over time were analysed using two-way repeated measures ANOVA. The Tukey HSD test served as a post hoc test.
All tests were performed using SPSS for Windows version 12.0 or Statistica programs ‘98 edition. A significance level of 5% was adopted.
Results
The 109 patients included in the study differed from the 74 excluded only in terms of diagnostic entity. There were more patients with AMI, but less with PTCA in the included group. However, in the included group, there were no differences between the subgroups without depressive mood (HADD 0–4), mild degree (HADD 5–8) and higher degree (HADD 9–21) of depressive mood in terms of the average level of age, the distribution of clinical groups of CAD, or tobacco users. There was, however, a significant difference in gender distribution, with women proportionally less numerous in the group with mild degree of depressive mood than in the other 2 groups (Table I).
| Table I. Pre-treatment characteristics in the total sample and in the subgroups without, and with mild degree and higher degree of depressive mood. |
| | Total sample | Subgroups of depressive mood | p* |
| Without | Mild degree | Higher degree |
| Age (years) | 51.4 | 51.8 | 50.7 | 51.4 | 0.71 |
| Gender (% male) | 83 | 76 | 97 | 86 | 0.04 |
| Tobacco users (%) | 11 | 12 | 10 | 10 | 0.94 |
| Clinical group (%) | | | | | 0.11 |
| AMI | 44 | 23 | 12 | 9 | |
| CABG | 33 | 22 | 5.5 | 5.5 | |
| PTCA | 12 | 5 | 6 | 1 | |
| Angina pectoris | 11 | 4 | 3.5 | 3.5 | |
| *Differences between depressive mood subgroups. AMI: acute myocardial infarction; CABG: coronary bypass surgery; PTCA: percutaneous transluminal coronary angioplasty. |
Changes in depressive mood during the rehabilitation period
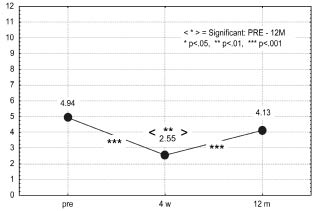
The mean baseline value of depressive mood across all subjects was 4.94, approaching the cut-off level for mild degree of depressive mood (5.0). After the 4-week in-patient rehabilitation phase the value had decreased to 2.55, and at the 12-month assessment the score was 4.13, F (2, 216) = 43.22, p < 0.001. Post hoc tests indicated a significant decrease at the 4-week assessment (p < 0.001), which, despite a subsequent significant increase (p < 0.001), was still significantly lower at the 12-month follow-up compared with the baseline level (p = 0.006, Fig. 1).
Fig. 1. Mean level of depressive mood for the total group at pre, 4-week and 12-month assessments.
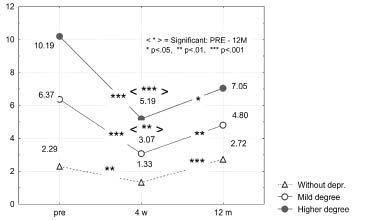
Analyses of changes in depressive mood in the different subgroups over time revealed a significant interaction effect, F(2, 212) = 14.28, p < 0.001, indicating a different pattern of change over time. As Fig. 2 implies, all subgroups displayed significantly lower scores of depressive mood at the 4-week assessment and a subsequent increase at the 12-month follow-up. The greatest improvements at the 4-week assessment appeared in the 2 groups with depressive mood (p < 0.001 for both groups). At the 12-month assessment lower scores in comparison with baseline levels were found in the subgroups with mild (p < 0.01) and higher degree of depressive mood (p < 0.001), whereas no significant change compared with baseline was found in the subgroup without such mood.
Fig. 2. Mean levels of depressive mood at pre, 4-week and 12-month assessments for subgroups with different baseline depressive levels. : without depression; : mild degree; : higher degree.
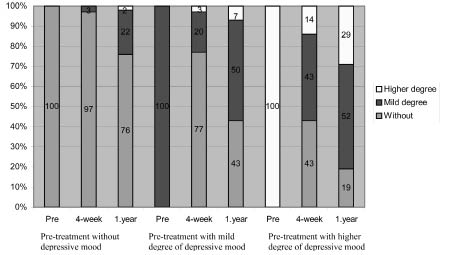
As shown in Table II the number of patients with depressive mood decreased by 59% (30 out of 51) at the 4-week assessment, but after 12 months the remaining decrease was only 6% (3 patients). Selecting only patients with higher degree of depressive mood, the number decreased by 81% (17 out of 21) at 4 weeks, and at 12 months there was still a remaining 57% (12 patients) decrease. The distribution of patients in different pre-treatment levels of depression and the subsequent change at 4 weeks and 12 months in the subgroups without, with mild and with higher degree of depressive mood, respectively, are presented in Fig. 3, expressed as percentages. Of the patients with mild degree of depressive mood, 23 out of 30 (77%) improved at 4 weeks and 13 of them (43%) were still without depressive mood at 12 months. Of the patients with higher degree of depressive mood 18 out of 21 (86%) improved at 4 weeks, half of them to the level without depressive mood, and at 12 months 15 of the 21 (71%) were still improved. Of the 41 patients who improved at 4 weeks 13 (32%) relapsed at 12 months, a higher proportion in patients with mild degree than in patients with higher degree of depressive mood, 10 out of 23 patients, (43%) and 3 out of 18 patients (17%), respectively.
| Table II. Distribution of patients in different categories of depressive mood at different assessment points. |
| | Pre | 4-week | 12-month |
| Without depressive mood | 58 | 88 | 61 |
| Mild degree of depressive mood | 30 | 17 | 39 |
| Higher degree of depressive mood | 21 | 4 | 9 |
Fig. 3. Distribution of patients, expressed as a percentage, in the different depressive categories at different assessment occasions, based on the baseline depressive levels. : higher degree; : mild degree; : without.
Associations between depressive mood and lifestyle changes
Across all subjects, significant changes in self-reported relaxation and dietary habits at the 12-, 24- and 36-month follow-ups emerged. Frequency of relaxation increased from 2.6 to 7.5, 6.2 and 4.9 times per week (F [3, 198] = 18.31, p < 0.001), and the diet index (healthy diet knowledge and diet habits), from 1.1 to 1.7, 1.6 and 1.6, (F [3, 207] = 19.78, p < 0.001). Exercise habits did not improve (F [3, 210], = 0.64, p = 0.59), although the exercise occasions per week increased slightly arithmetically from an already high level of 3.7 to 3.9, 3.7 and 4.0.
Subgroup differences in dietary-, relaxation, and exercise habits at the 12-, 24- and 36-month follow-ups were calculated separately. In order to eliminate pre-treatment differences between groups in measures of lifestyle habits, one-way ANCOVAs with a baseline level of the different dependent variables as covariates, were performed. As presented in Table III, no significant lifestyle habit differences due to group emerged at the different follow-up periods, indicating that the original level of depressive mood did not influence change of lifestyle habits. The same was true for the proportion of smokers at the 12-month (p = 0.84), 24-month (p = 0.57) and 36-month (p = 0.25) follow-up assessments.
| Table III. Differences between means of self-reported lifestyle variables in different subgroups originally without, and with mild degree and higher degree of depressive mood at the 12-, 24- and 36-month follow-ups with baseline values as covariates for relaxation-, diet-, and exercise habits. |
| | Without | Mild
degree | Higher degree | df | F | p |
| Mean (SD) | Mean (SD) | Mean (SD) |
| Relaxation habits* |
| 12 months | 7.33 (6.40) | 6.07 (3.84) | 9.90 (6.49) | 2, 99 | 1.76 | 0.18 |
| 24 months | 6.54 (6.72) | 5.76 (4.64) | 5.79 (4.30) | 2, 77 | 0.15 | 0.86 |
| 36 months | 5.52 (5.99) | 4.42 (3.51) | 6.88 (5.08) | 2, 84 | 0.76 | 0.47 |
| Diet habits† |
| 12 months | 1.61 (0.58) | 1.69 (0.48) | 1.45 (0.75) | 2, 10 | 1.13 | 0.33 |
| 24 months | 1.57 (0.58) | 1.52 (0.65) | 1.52 (0.83) | 2, 80 | 0.04 | 0.96 |
| 36 months | 1.62 (0.50) | 1.41 (0.61) | 1.66 (0.56) | 2, 88 | 1.87 | 0.16 |
| Exercise habits* |
| 12 months | 4.09 (2.44) | 4.79 (2.43) | 4.55 (2.76) | 2, 98 | 0.81 | 0.45 |
| 24 months | 3.32 (1.64) | 3.62 (2.22) | 4.64 (2.47) | 2, 75 | 2.53 | 0.09 |
| 36 months | 3.47 (1.79) | 4.43 (2.23) | 4.59 (2.81) | 2, 86 | 2.50 | 0.09 |
| *Average number of occasions per week. †Index. |
Discussion
Clinically significant depression tends to recur and to be chronic, especially if left untreated (27). In the present study, around 80% of the patients with higher degree of depressive mood improved after the 4-week inpatient phase. These results are in line with those reported by Milani et al. (6) who found that 67% of the pre-treatment depressed CAD patients in their study remitted after a 3-month rehabilitation program. The results at the 12-month assessment in the present study, with 32% relapsing, were less impressive compared with the distribution at 4 weeks. A comparable course has also been reported by Hance et al. (28), who found that 42% of patients diagnosed with minor depression developed major depression.
The patients with higher degree of baseline depressive mood at the start made the greatest improvements, both in terms of mean values and in terms of the proportion of patients who improved to a level with less or without depressive mood at 12 months. These results are partly at odds with findings in our previous study (20), suggesting both a short- and long-term (12 months) improvement on BDI measured mild depression, but an improvement restricted to the physical mood on the BDI among clinically depressed subjects.
As the aim of the present study was to investigate the time-course of depressive mood during participation in a rehabilitation intervention, as well as to analyse its relation to risk factor related lifestyle changes, the design lacks a randomized control group, and we are in no position to draw any casual conclusions as to the impact of the intervention per se on the course of depressive symptoms. However, the overall improved depressive mood corresponds with some controlled rehabilitation programs (9–11). On the other hand, the observed decreases in depressive mood during the long-term rehabilitation program do not correspond with some other psychological- and counselling-based programs (13–14, 17). These interventions lacked behavioural components, such as exercise training. The absence of exercise in this type of program may have been critical since exercise has been found to have an anti-depressive effect (29). Results are also at odds to a study by Sebregts et al. (19), which may be explained by the fact that in their study exercise training was included also in the control group. Exercise seems to be an important component in association to depressive mood in CAD rehabilitation even though not all studies support this suggestion (16, 18). Another indication of the importance of physical exercise is that individuals with low physical activity seem to have a greater risk of subsequent depression (30).
Depressive mood have been found to be associated with poorer adherence to cardiac risk factor modification and rehabilitation programs (31). Both Mayou et al. (3) using the HADD, and Ziegelstein et al. (5), using the BDI, reported lower adherence to recommended lifestyle changes in depressed patients than in non-depressed. In the present study, patients originally with depressive mood made lifestyle changes to the same degree as patients without depressive mood. As change of lifestyle has been found to decrease recurrent coronary events (32–34), it is an important observation that depressive mood does not seem to have an effect on change of lifestyle after participating in a behaviourally oriented rehabilitation program.
Apart from the above-mentioned lack of a control group, another limitation of the present study is that the sample size was quite small due to the high drop-out rate (40%) during the assessment period. Even though there was no pre-treatment depression level difference between the patients who accomplished the assessments and the drop-outs, it cannot be ruled out that drop-outs for different reasons got worse during the period. However, data from 30% of the drop-outs at the 12-month follow-up indicates that they did not differ on level of depressive mood from those who fulfilled all assessments. Anyway, even if most of the drop-outs had increased their depressive mood levels, the results of the present study indicate that this does not seem to influence the change of lifestyle pattern.
In summary, the course of depressive mood through the 12-month assessment period, showing an immediate improvement and a subsequent impairment for a number of patients, seems to be the normal progress. Nevertheless, depressive mood, both in the subgroups with mild and higher degree, was improved at 12 months compared with baseline. Although it could not be concluded that this decrease was caused by the rehabilitation intervention itself, it might be speculated, in line with some similar controlled studies (9–11), that the inclusion of exercise training may be important for the improved depressive mood as exercise has been found to be a high-quality antidepressant (35). Due to the non-randomized design, relatively small sample size and high drop-out rate results in the present study must, however, be interpreted with some caution.
Depression, and also milder forms of depressive mood, have a generally negative influence on CAD, but the results of the present study indicate that pre-treatment patients with depressive mood change their lifestyle to the same degree as patients not feeling depressed during a 36-month follow-up period. This indicates that depressive mood might not be an obstacle to lifestyle changes that might prevent recurrent coronary events after participating in a behaviourally oriented rehabilitation program including exercise training.
Acknowledgements
This study is one of the projects initiated by Professor Åke Nygren, Karolinska Institute, and was funded by the AMF Insurance Company and the SPP Insurance Company. We thank all the members of staff at the rehabilitation centre (Föllingekliniken).
References
1. Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol 2002; 7: 11–21.
2. Spertus JA, McDonell M, Woodman CL, Fihn SD. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am Heart J 2000; 140: 105–110.
3. Mayou RA, Gill D, Thompson DR, Day A, Hicks N, Volmink J, Neil A. Depression and Anxiety as predictors of outcome after myocardial infarction. Psychosom Med 2000; 62: 212–219.
4. Carney RM, Rich MW, Freedland KE, Saini J, teVelde A, Simeone C, Clark K. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med 1988; 50: 627–633.
5. Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med 2000; 160: 1818–1823.
6. Milani RV, Lavie CJ, Cassidy MM. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. Am Heart J 1996; 132: 726–732.
7. Turner SC, Bethell HJN, Evans JA, Goddard JR, Mullee MA. Patient characteristics and outcomes of cardiac rehabilitation. J Cardiopulm Rehabil 2002; 22: 253–260.
8. Thompson DR, Meddis RA. A prospective evaluation of inhospital counselling for first time myocardial infarction men. J Psychosom Res 1990; 34: 237–248.
9. Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M. Effects of self-help post-myocardial-infarction rehabilitation on psychological adjustment and use of health services. Lancet 1992; 339: 1036–1040.
10. Trzcieniecka-Green A, Steptoe A. The effects of stress management on the quality of life of patients following acute myocardial infarction or coronary bypass surgery. Eur Heart J 1996; 17: 1663–1670.
11. Johnston M, Foulkes J, Johnston DW, Pollard B, Gudmundsdottir H. Impact on patients and partners of inpatient and extended cardiac counseling and rehabilitation: a controlled trial. Psychosom Med 1999; 61: 225–233.
12. Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction (ENRICHD). JAMA 2003; 289: 3106–3116.
13. Jones DA, West RR. Psychological rehabilitation after myocardial infarction: multicentre randomised controlled trial. BMJ 1996; 313: 1517–1521.
14. Frasure-Smith N, Lespérance F, Prince RH, Verrier P, Garber RA, Juneau M, et al. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet 1997; 350: 473–479.
15. Taylor CB, Miller NH, Smith PM, DeBusk RF. The effect of a home-based, case-managed multifactorial risk reduction program on reducing psychological distress in patients with cardiovascular disease. J Cardiopulm Rehabil 1997; 17: 157–162.
16. Sundin Ö, Lisspers J, Hofman-Bang C, Nygren Å, Rydén L,
Öhman A. Comparing multifactorial lifestyle interventions and stress management in coronary risk reduction. Int J Behav Med 2003; 10: 191–204.
17. Murchie P, Campbell NC, Ritchie LD, Deans HG, Thain J. Effects of secondary prevention clinics on health status in patients with coronary heart disease: 4 year follow-up of a randomized trial in primary care. Fam Pract 2004; 21: 567–574.
18. Norrman S, Stegmayr B, Eriksson M, Hedbäck B, Burell G, Brulin C. Depressive mood after a cardiac event: gender inequality and participation in rehabilitation programme. Eur J cardiovasc Nurs 2004; 3: 295–302.
19. Sebregts E, Falger P, Appels A, Kester A, Bär F. Psychological effects of a short behavior modification program in patients with acute myocardial infarction or coronary artery bypass grafting. A randomized controlled trial. J Psychosom Res 2005; 58: 417–424.
20. Lisspers J, Söderman E, Sundin Ö, Nygren Å. The effects on and of depression – an exploratory study of rehabilitation and secondary prevention in coronary artery disease. Scand J Behav Ther 1999; 28: 9–18.
21. Cavanaugh S, Clark D, Gibbons R. Diagnosing depression in the hospitalized medically ill. Psychosomatics 1983; 24: 809–815.
22. Söderman E, Lisspers J. Diagnosing depression in patients with physical diseases using the Beck Depression Inventory (BDI). Scand J Behav Ther 1997; 26: 102–112.
23. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961; 4: 53–63.
24. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361–370.
25. Lisspers J, Hofman-Bang C, Nordlander R, Rydén L, Sundin Ö, Öhman A, et al. Multifactorial evaluation of a program for life-style behavior change in rehabilitation and secondary prevention after coronary artery disease. Scand Cardiovasc J 1999; 33: 9–16.
26. Herrman C. International experiences with the Hospital Anxiety and Depression Scale – A review of validation data and clinical results. J Psychosom Res 1997; 42: 17–41.
27. Lloyd GG, Cawley RH. Distress or Illness. A study of psychological symptoms after myocardial infarction. Br J Psychiatry 1983; 142: 120–125.
28. Hance M, Carney RM, Freedland KE, Skala J. Depression in patients with coronary heart disease: a twelve month follow-up. Gen Hosp Psychiatry 1996; 18: 61–65.
29. Lane D, Carroll D, Lip GYH. Psychology in coronary care. Q J Med 1999; 92: 425–431.
30. Camacho TC, Roberts RE, Lazarus NB, Kaplan GA, Cohen RD. Physical activity and depression: evidence from the Alameda County Study. Am J Epidemiol 1991; 134: 220–231.
31. Blumenthal JA, Williams RS, Wallace AG, Williams RB, Needles TL. Physiological and psychological variables predict compliance to prescribed exercise therapy in patients recovering from myocardial infarction. Psychosom Med 1982; 44: 519–527.
32. de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction. Final report of the Lyon Diet Heart Study. Circulation 1999; 99: 779–785.
33. Hedbäck B, Perk J, Wodlin P. Long-term reduction of cardiac mortality after myocardial infarction: 10-year results of a comprehensive rehabilitation programme. Eur Heart J 1993; 14: 831–835.
34. Oldridge NB, Gyatt GH, Fisher ME, Rimm AA. Cardiac rehabilitation after myocardial infarction: combined experience of randomized clinical trials. JAMA 1988; 260: 945–950.
35. North TC, McCullagh P, Tran ZV. Effects of exercise on depression. Exerc Sport Sci Rev 1990; 18: 379–415.