STRETCHING EXERCISES VS MANUAL THERAPY IN TREATMENT OF CHRONIC NECK PAIN: A RANDOMIZED, CONTROLLED CROSS-OVER TRIAL
Jari Ylinen, MD, PhD1, Hannu Kautiainen, BA2, Kaija Wirén, PT3 and Arja Häkkinen PhD1
From the 1Department of Physical Medicine and Rehabilitation, Jyväskylä Central Hospital, Jyväskylä, 2Rheumatism Foundation Hospital, Heinola and 3Jyväskylä Adult Centre of Education, Jyväskylä, Finland
OBJECTIVE: To compare the effects of manual therapy and stretching exercise on neck pain and disability.
DESIGN: An examiner-blinded randomized cross-over trial.
Patients: A total of 125 women with non-specific neck pain.
METHODS: Patients were randomized into 2 groups. Group 1 received manual therapy twice weekly and Group 2 performed stretching exercises 5 times a week. After 4 weeks the treatments were changed. The follow-up times were after 4 and 12 weeks. Neck pain (visual analogue scale) and disability indices were measured.
RESULTS: Mean value (standard deviation) for neck pain was 50 mm (22) and 49 mm (19) at baseline in Group 1 and Group 2, respectively, and decreased during the first 4 weeks by 26 mm (95% Confidence Interval 20–33) and 19 mm (12–27), respectively. There was no significant difference between groups. Neck and shoulder pain and disability index decreased significantly more in Group 1 after manual therapy (p=0.01) as well as neck stiffness (p=0.01).
CONCLUSION: Both stretching exercise and manual therapy considerably decreased neck pain and disability in women with non-specific neck pain. The difference in effectiveness between the 2 treatments was minor. Low-cost stretching exercises can be recommended in the first instance as an appropriate therapy intervention to relieve pain, at least in the short-term.
Key words: cervical pain, home exercise, massage, mobilization, rehabilitation, training.
J Rehabil Med 2007; 39: 126–132
Correspondence address: Jari Ylinen, Jyväskylä Central Hospital, Department of Physical and Rehabilitation Medicine, Keskussairaalantie 19, FIN-40620 Jyväskylä, Finland. E-mail:jari.ylinen@ksshp.fi
Submitted December 12, 2005; accepted October 11, 2006.
INTRODUCTION
Chronic neck pain is a common problem among the adult population in industrialized countries. In Finland the point prevalence is 7% in women and 5% in men (1). A similar prevalence has been reported in the UK (2). The prognosis for chronic neck pain is poor, as it seems to be a more persistent condition than low back pain (3). Chronic neck pain causes major financial loss, not only in terms of diagnosis and treatment, but also due to sick leave and premature retirement pensions (4). Despite the fact that they have been inadequately studied, massage and mobilization are among the most common forms of therapy used in the treatment of chronic neck pain (5–8). Recently, a systematic review concluded that massage is beneficial for patients with subacute and chronic non-specific low back pain, both reducing the symptoms and improving function (9). New research data, although limited, also supports the use of massage and mobilization for intensive chronic neck pain, at least at the start of therapy. Hoving et al. (10) found that manual therapy including massage, specific mobilization techniques involving low-velocity passive movements within the limit of joint range of motion and coordination or stabilization techniques, reduced neck pain significantly more effectively than treatment by a general practitioner, which included medication, information and a booklet containing ergonomic advice and home exercises and encouragement to await further recovery. Manual therapy was also more cost-effective than physical therapy or treatment by a general practitioner with regards to both direct and indirect costs during a 1-year follow-up (11).
Massage and mobilization are the most common forms of therapy used by physiotherapists for chronic neck pain in the private sector (7, 8). In the public sector, where resources are more limited, advice on ergonomics, posture and self-
administered stretching is more commonly the sole intervention by physiotherapists. However, there is insufficient evidence to allow conclusions to be drawn about the effectiveness of passive manual therapy compared with stretching exercises. Thus, the aim of the present study was to compare the effectiveness of passive manual therapy, consisting of massage, mobilization and stretching techniques, with self-administered stretching exercise performed at home on pain and disability in women with chronic, non-specific neck pain.
METHODS
Design and settings
Occupational healthcare services and office workers in the largest workplaces were directly informed about the study by an e-mail campaign in the town of Jyväskylä. The applicants were posted a questionnaire that combined items on their current health, neck symptoms and a pain drawing, to confirm their health status regarding the inclusion and exclusion criteria and to enable selection to be made prior to the medical examination. On the basis of the clinical examination, including an interview and manual examination, the physician confirmed the diagnosis and selected suitable patients from referrals and from patients applying directly for inclusion in the study. Radiographic imaging and electroneuromyography were evaluated, when needed for differential diagnosis. Group 1 received manual therapy for 30 minutes twice a week for 4 weeks, after which they were instructed to perform neck stretching exercises at home. Group 2 received the same therapies, but in reverse order. Both groups were followed up at 12 weeks. All the questionnaires were analysed blinded. Manual therapy was performed in the institute responsible for educating massage therapists. In the stretching group each patient was individually advised once about the proper way to perform exercises, by a physiotherapist in the department of physical medicine and rehabilitation at the central hospital. Patients also received written instructions about the exercises that they were to practice thereafter at home.
The study design was approved by the ethics committee of Jyväskylä Central Hospital, Finland. All the participants gave written consent before entering the study.
Study population
The following inclusion criteria were used: female, age range 25–53 years, permanently employed, motivated to continue working, motivated for exercising and treatment, and constant or frequently occurring neck pain of more than 6 months’ duration. Exclusion criteria were: specific disorders of the cervical spine, such as disc prolapse, spinal stenosis, postoperative conditions in the neck and shoulder areas, history of severe trauma, instability, spasmodic torticollis, migraine (frequency more often than twice per month), peripheral nerve entrapment, fibromyalgia, hypermobility syndrome, shoulder diseases (tendonitis, bursitis, capsulitis), inflammatory rheumatic diseases, severe psychiatric illness and other diseases that prevent physical loading, pregnancy and other on-going therapies. These states were assessed by questionnaires, medical history and a clinical examination before selection for the study. Out of 420 volunteers, 243 were excluded on the basis of the questionnaire alone, and 177 were invited to the clinic for a medical examination (Fig. 1). Of this number 45 did not meet the inclusion criteria and 7 failed to attend the clinic. The main reasons for exclusion were low neck pain on the visual analogue scale (VAS), cut-off point 45 mm (n = 112), on-going massage or physiotherapy (n = 70), duration of symptoms less than 6 months (n = 26), pain in the shoulder joint (n = 20) and fibromyalgia (n = 18). Finally, 125 women were randomized pair-wise into Group 1 (n = 62) and Group 2 (n = 63) by tossing a coin. The randomization was performed by a person who had not seen the patients. Demographic and clinical data for the patients are presented in Table I.
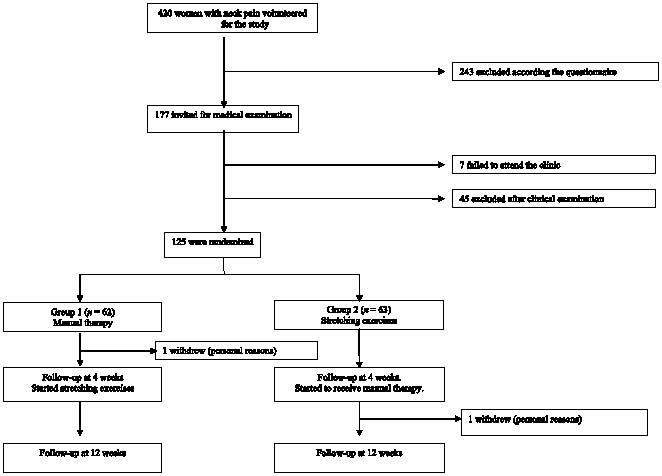
Fig. 1. Participant flowchart
| Table I. Demographic and clinical data of the patients in the two study groups at baseline. Values are mean (SD) where not otherwise stated | ||
| Group 1 (n=62) | Group 2 (n=63) | |
| Demographic | ||
| Age (years) | 42 (9) | 44 (8) |
| Height (cm) | 165 (5) | 166 (5) |
| Weight (kg) | 69 (13) | 70 (13) |
| Clinical | ||
| Duration of neck pain (years) | 3.8 (3.8) | 3.0 (3.0) |
| Sick leave due to neck pain during previous 12 months (days) | 8 (14) | 8 (17) |
| Using medication for neck pain, n (%) Daily or almost daily Occasionally None | 3 (5) 14 (22) 45 (73) | 4 (6) 19 (30) 40 (64) |
| Short Depression Inventory | 4 (3) | 5 (3) |
| Smoking, n (%) | 15 (26%) | 10 (17%) |
| Work | ||
| Length of working day (hours) | 37.5 (5.2) | 37.9 (3.5) |
| Physical loading of work, n (%) Light loading, sitting Moderate loading, sitting Light loading, standing Moderate loading, standing Heavy loading, standing | 34 (54) 1 (2) 11 (18) 13 (21) 3 (5) | 28 (45) 2 (3) 19 (30) 10 (16) 4 (6) |
| Leisure time activity Physical exercising (minutes/week) | 300 (217) | 267 (164) |
| SD: standard deviation. | ||
Outcome measures
Outcome measurements were taken at baseline, after the 4-week intervention and at the 12-week follow-up. The primary outcomes were average and night-time neck pain during the previous week, which were assessed by a 100-mm visual analogue scale (VAS) with no anchors between the ends, which were indicated by 0 (no pain) and 100 (unbearable pain) (12–14). Disability was assessed by the modified Neck and Shoulder Pain and Disability Index (15) and Neck Disability Index (16). Other studies have shown that the reliability and validity of the VAS and Neck Disability Index are acceptable or good (17–19). On each scale, the theoretical range is from 0 (no dysfunction) to 100 (maximal dysfunction). The other outcome measures were stiffness and numbness in the neck and shoulder region and intensity of headache analysed by the VAS, range from 0 (no symptoms) to 100 (severe symptoms and unbearable pain), and impairment in work and leisure activities, which were also assessed by VAS, range from 0 (no dysfunction) to 100 (maximal dysfunction). Mood was assessed by the Short Depression Inventory, theoretical range from 0 (no symptoms) to 21 (severe depression) (20). The intensity of physical activity at work was assessed on a scale accompanied by illustrations and descriptions of the various types of work corresponding to each scale point. The scale ran from 1 (light sedentary work) to 5 (heavy manual work). Participants were asked about their use of analgesics prior to the study and at the 4-week follow-up. Patients were instructed to keep a diary once a week to record the average neck pain experienced during the preceding week. At the follow-up, the subjective benefit of the intervention was assessed by asking the patients the effect of the manual treatment and stretching on their neck pain on a 5-point scale, range from 0 (no change) to 4 (complete relief from pain).
Interventions
Manual therapy group. Patients had 2 treatments weekly for 4 weeks. Treatment was performed in the standardized way and consisted of 3 components: (i) low-velocity osteopathic type mobilization of cervical joints for 10 minutes, (ii) traditional massage for 15 minutes, (iii) passive stretching for 5 minutes, as follows.
• Mobilization based on 8 osteopathic-type mobilization techniques, which were all performed while the patient was lying supine:
1) Translation upwards: the head and upper cervical spine is lifted up by pushing the spinous processes with both hands to apply force to the movement segment lying between the lifted vertebra and the one immediately below it.
2) Translation sideways: the cervical vertebra is pushed alternately towards the right and left side by force applied to each facet joint. Hands tightly support each side of the head and upper cervical column, which were moved directly sideways at each level being treated.
3) Side bending: the cervical spine is bent alternately to each side. Hands support along each side of the head and cervical column with the pads of the finger tips over the mobilized facet joint. The head and cervical column are bent to each side and finger tips are then moved upwards over the next facet joint.
4) Rotation and side bending in the same direction: the head is supported by the therapist's lower mid-abdomen and hands support the head and upper cervical spine. Hands overlie each other forming a bridge so that the heads of the metacarpal bones are over the facet joints. Prior to mobilization the cervical column is moved sideways and rotated in the same direction to about half of total range of movement (ROM). The movement is then continued so that connective tissues become stretched without causing pain. The head and neck is returned after each movement to its starting position. The head is rotated to the other side for the same treatment.
5) Rotation and side bending in the opposite direction: the technique is performed as in phase 4, but the head and cervical spine are rotated in the opposite directions.
6) Rotation with small ROM: the pads of the tips of the middle and the ring fingers are placed over the spinous processes and the fingers then are straightened so that the middle phalanx of the fingers is over the facet joint. The head is supported with the hand on the opposite side allowing the movement to happen and the head return to the middle position. The other side is treated by moving to the opposite side of the treatment table.
Mobilization treatments 1–6 are started about at the level of the fourth vertebra and each vertebra is moved 2–3 times. After reaching the head the direction is reversed and the vertebra below it is mobilized 2–3 times until the seventh cervical vertebra is reached.
7) Mobilization of upper cervical joints: both hands support the occiput with the tips of the middle and the ring fingers over the arch of the atlas on each side. The head is bent sideways slightly and turned in the opposite direction, causing the atlas to move against the finger tips. The mobilization is performed 3 times in each direction.
8) Mobilization of the jaw joint: the masticatory muscles are kept relaxed so that the mouth is slightly open. The thumb is placed just below the zygomatic arch and pushes towards the belly of the masseter muscle so that the jaw moves slightly in the opposite direction.
No manipulation, i.e. high-velocity thrusts with low-amplitude, was applied.
• Massage was performed in the prone position in the following order: lower and central part of trapezius, rhomboid, infraspinatus, teres minor and major, upper part of trapezius, supraspinatus, levator scapulae, splenius capitis, and cervicis muscles. Thereafter the patient turned to lie supine and the following muscles were treated: sternocleidomastoideus, scalene, pectoralis major and minor muscles. Deep massage treatment consisted of both longitudinal strokes along the muscle as well as transverse friction techniques, which have been described in detail elsewhere (21).
• Passive stretching techniques for 30 seconds were applied in the same order on the scalene, upper part of trapezius, pectoralis minor muscles and interspinous muscles and ligamentum nuchae (22).
Treatments were performed in the training centre clinic, which has no administrative connections with the hospital. The therapy was provided by 2 massage therapy students, who were halfway through their 1-year training period. They were taught a specific form of mobilization treatment by a registered osteopath (JY). The treatment was practised under supervision for 2 months. A check was made before the study started to ensure that both students performed the treatment in the same way and met the professional criteria with respect to the techniques used. In the second part of the study, treatments were performed for Group 2 by an additional 4 trainee massage therapists, who had also been taught same treatment techniques.
Stretching group. Exercises were performed in the following order; stretching towards lateral flexion for the upper part of the trapezius, ipsilateral flexion and rotation for the scalene and flexion for the extensor muscles, holding each movement for 30 seconds. Each exercise was repeated 3 times. Finally a neck straightening exercise was performed by retruding the head 5 times for 3–5 seconds. Patients were advised to perform the stretching program 5 times a week, a single session taking about 10 minutes to perform. Patients were also instructed to keep an exercise diary to monitor their exercise frequency.
Data analysis
The target sample size of 120 (60 in each group) was calculated to ensure at least 80% power to detect a difference of 30% between the groups at 2-side α=0.05 in pain measured with the VAS. A maximum drop-out rate of 10% was assumed.
Clinical outcome variables were analysed by the intention-to-treat approach. The results were expressed as means with standard deviations (SD) or with a 95% confidence interval (95% CI). The normality of variables was evaluated using the Shapiro-Wilk test. Statistical between-groups comparisons were made using the 2-tailed unpaired t-test. We analysed the continuous outcome variables using a covariance model (ANCOVA) including factors for treatment and baseline values. Variables with ordinal distribution were analysed by the Permutation test with Monte Carlo p-values and subjective benefit from the intervention was compared with the Fisher-Freeman-Halton Test. Correlation coefficients were calculated by the Pearson method. The α-level was set at 0.05 for all tests.
RESULTS
All the patients in Group 1 received 8 manual therapy sessions over a 4-week period as planned, except for one patient who withdrew for personal reasons. Mean stretching frequency in Group 2 according to the training diaries was 5 times a week during the same 4-week period. One patient withdrew for personal reasons from this group, but first during the manual therapy period.
The neck pain and disability indices were on the same level in both groups at baseline (Table II). These primary outcomes showed a significant decrease in both groups at the 4-week follow-up. Other outcomes, including stiffness and numbness of the neck and shoulder areas, headache, and impairment in work and leisure-time physical activities also decreased significantly in both groups compared with baseline. The neck and shoulder pain and disability index, stiffness in the neck and numbness in the shoulder region decreased significantly more in Group 1 compared with Group 2. After 4 weeks the therapies were switched; Group 2 now receiving manual therapy and Group 1 performing home exercises and at the 12-week follow-up no statistically discernible differences were found between the groups.
| Table II. Subjective ratings of the most prominent symptoms in patients with chronic neck pain at baseline and changes at 4-week and 12-week follow-ups. Group 1 started with manual therapy and continued with self-administered stretching after 4 weeks. Group 2 had the same therapies in the reverse order | ||||||||
| Baseline | Change from baseline to 4 weeks | Change from baseline to 12 weeks | ||||||
| Group 1 Mean (SD) | Group 2 Mean (SD) | Group 1 Mean | Group 2 Mean | Difference between the groups† | Group 1 Mean | Group 2 Mean | Difference between the groups† | |
| Neck pain* | ||||||||
| Average | 50 (22) | 49 (19) | –26 (–33 to –20) | –19 (–27 to –12) | 0.06 | –19 (–27 to –12) | –19 (–25 to –13) | 0.91 |
| Night time | 30 (22) | 31 (22) | –19 (–27 to –12) | –12 (–18 to –7) | 0.79 | –12 (–18 to –7) | –13 (–19 to –7) | 0.79 |
| Neck and Shoulder Pain | 33 (14) | 31 (13) | –15 (–19 to –12) | –9 (–13 to –6) | 0.013 | –14 (–18 to –10) | –12 (–15 to –9) | 0.48 |
| Vernon Neck Disability Index | 24 (9) | 26 (9) | –10 (–12 to –7) | –8 (–10 to –6) | 0.052 | –9 (–12 to –7) | –10 (–12 to –8) | 0.53 |
| Neck stiffness* | 49 (24) | 49 (25) | –27 (–33 to –21) | –19 (–26 to –13) | 0.01 | –19 (–26 to –13) | –17 (–23 to –11) | 0.98 |
| Neck numbness* | 21 (24) | 31 (26) | –16 (–21 to –11) | –14 (–20 to –9) | 0.06 | –14 (–20 to –9) | –16 (–22 to –9) | 0.87 |
| Headache* | 43 (25) | 43 (25) | –22 (–29 to –14) | –17 (–23 to –12) | 0.12 | –17 (–23 to –12) | –20 (–25 to –14) | 0.62 |
| Impairment in work* | 32 (20) | 31 (20) | –17 (–23 to –12) | –17 (–23 to –11) | 0.98 | –17 (–23 to –11) | –12 (–17 to –6) | 0.30 |
| Impairment in leisure time physical activities* | 35 (21) | 35 (20) | –17 (–23 to –12) | –17 (–23 to –10) | 0.97 | –17 (–23 to –10) | –16 (–21 to –11) | 0.70 |
| *Visual analogue scale (0–100 mm). †Analysis of covariance (ANCOVA) baseline values as covariate. SD: standard deviation; CI: confidence interval. | ||||||||
The decrease in neck pain was associated with reduced stiffness and numbness in the shoulder region and headache (range r=0.31–0.62, p-value from 0.003 to <0.001 and 95% CI 0.14–0.72) and with reduced impairment in work (r=0.49, p<0.001 and 95% CI 0.34–0.61) as well as leisure-time physical activities (r=0.42, p<0.001 and 95% CI 0.26–0.56). Furthermore, the initial level of neck pain was associated with the reduction in neck pain (r=0.56, p<0.001 and 95% CI 0.42–0.67).
Analgesics for neck pain had been used by 50% of the patients during the week prior to the intervention and 30% after the intervention, with no statistically discernible difference in use between the groups (Table III). Also, frequency of using analgesics was reduced in both groups at both follow-ups. One-third of those using analgesics reported receiving only little help from them. Sixty-four percent in Group 1 and 34% in Group 2 reported considerably or complete relief of neck pain at the 4-week follow-up (Table IV). The difference between groups was statistically significant (p=0.001).
| Table III. Number of patients (%) that used analgesics for neck pain and number of days per week they took analgesics | ||||||
| Days per week | 1st week | 4th week | 12th weeks | |||
| Group 1 | Group 2 | Group 1 | Group 2 | Group 1 | Group 2 | |
| None | 26 (42) | 36 (57) | 43 (69) | 47 (75) | 43 (69) | 44 (70) |
| 1–2 | 24 (39) | 22 (35) | 11 (18) | 11 (17) | 16 (26) | 16 (25) |
| 3–5 | 8 (13) | 5 (8) | 4 (7) | 5 (8) | 3 (5) | 3 (5) |
| 6–7 | 1 (2) | – | 1 (2) | – | – | – |
| Missing data | 3 (4) | – | 3 (4) | – | – | – |
| Table IV. Patient self-ratings of the benefit of the intervention at the 4-week follow-up | ||
| Pain | Group 1 (n=62) | Group 2 (n=63) |
| Reduced totally n (%) | 2 (3) | 0 |
| Reduced considerably n (%) | 38 (61) | 21 (34) |
| Reduced slightly n (%) | 19 (31) | 36 (57) |
| No change n (%) | 2 (3) | 4 (6) |
| Missing data | 1 (2) | 2 (3) |
DISCUSSION
At the 4-week follow-up neck pain had decreased by 52% in Group 1, which is a clinically significant change (23). Group 2 did almost as well and pain decreased by 39%. Although the difference was not statistically different between the groups, the subjective benefit reported for the manual therapy was significantly greater than that reported for the stretching exercise. This may reflect patients’ experience of the effectiveness of manual treatment in decreasing neck muscle stiffness, as shown also in the significant difference in the results between the groups.
The Neck and Shoulder Pain and Disability Index clearly favoured manual therapy at the 4-week follow-up. The Vernon Disability Index did not reach statistical significance. The former index has a continuous scale, while the latter uses a categorized scale, and the content of the individual questions also differ between the scales, which may explain the difference in the sensitivity of these instruments in assessing changes, as was also shown previously (8). We also evaluated the possible additional effects of stretching after the period of massage, and vice versa. However, no significant changes were found in results of the second treatment period.
Unfortunately we did not have a control group in the study, but several other studies have already shown manual therapy to be effective treatment in neck pain (10, 24–26). Brodin (24) reported that a group receiving osteopathic-type low-velocity cervical mobilization 3 times a week over 4 weeks showed significantly greater reduction in neck pain compared with either a group receiving massage, slight traction and electrical stimulation or controls. In randomized studies cervical mobilization has also been shown to reduce headache and pain in the upper extremities associated with neck pain (25, 26). The results after manual therapy in our study were similar to these obtained previously by Hoving et al. (10). They compared cervical mobilization to physical therapy, including manual therapy, and to continued care by a general practitioner. After 12 therapy sessions over 6 weeks, both interventions had better success rates compared with controls.
In our study, Group 2 had also received manual therapy before the 12-week follow-up and there were no longer any differences between the groups. The effect of manual therapy in Group 1 seemed to decline, but the changes still remained significant compared with baseline. In a randomized study, Levoska & Keinänen-Kiukaanniemi (27) also found that stretching, light exercises for muscles, clay and massage treatments 3 times a week over 5 weeks reduced the occurrence of chronic neck pain. Ylinen et al. (8) found, at a 12 months follow-up, a significant reduction in neck pain as a result of stretching exercise performed on average twice weekly. However, the effectiveness was significantly better when stretching exercises were combined either with neck muscle endurance or strength training.
The short follow-up time is a weakness of this study. However, manual therapy as the sole treatment for chronic neck pain has not been shown to have long-term effects in contrast to neck muscle training combined with stretching exercises (8, 25). In the clinic, manual therapy may sometimes be an essential support during the early stage of rehabilitation, and may be indicated in cases of severe neck pain in order to provide immediate relief and to make effective resistance training possible. Thus, the design of the study is well-founded on the basis of clinical practice.
There was no wash-out period after 4 weeks’ manual treatment or stretching, as we tested for a possible additional effect of massage followed by stretching and vice versa and found none. Of course, this does not exclude the possibility that additional intervention had some effect in maintaining the gains achieved.
Despite the presence of moderate or severe neck pain, only half of patients in the present study used medication to ease her neck symptoms. Several patients using analgesics did not experience much pain relief from them, which may also be one reason for the low compliance in the group not using them. Hurwitz et al. (28) also concluded on the basis of a systematic review that mobilization is probably more effective than muscle relaxants or routine medical care in producing short-term pain relief in cases of chronic neck pain. Continuing with ineffective medication or leaving patients without treatment are not acceptable choices. On the other hand, prescribing more effective painkillers, such as opiates, may do the patient a disservice, as it may reduce the possibilities for active rehabilitation due to central side-effects and the possible development of drug dependence. Stretching exercises and manual therapy are favourable treatment options, especially for patients who have experienced side-effects from drugs or for those at increased risk due to gastrointestinal bleeding or diseases of the heart, kidneys or liver.
It has been suggested that much of the benefit attributable to manual therapy is simply a placebo effect (29). This may be due to the experience therapists have in talking to and managing patients in such a way as to increase their faith in the treatment. In the present study the patients knew that the therapy was provided by students and thus it may be assumed that therapist charisma was small or insubstantial. With the standardized protocol, the therapist-related factors of increased experience and specialty certification status may not result in an improvement in patients (29). However, patients’ expectations are known to affect treatment outcomes (31, 32) and receiving hands-on treatment may contribute to the results. The main problem, common in non-medicine treatments in clinical research, is that it is impossible to conduct a placebo-controlled study of manual therapy. However, since patients` expectations have to be faced in everyday clinical practice, they are an important part of the results.
Patients were women from a city, both factors which must have affected the occupational status. Sex, age and occupation may affect the outcome. Thus, the results may not be generalized to the whole working population. Motivation depends greatly on psychosocial circumstances, which thus also have important effects on the results. Various stretching frequencies as well as doing exercises in different ways or doing completely different exercises or different massage therapies may influence the results. Individually adjusted stretching as well as massage treatment could also make some difference. However, because subjects at the end of the study had much less pain, and taking into account the amount of change in several other studies of treatments for chronic neck pain, it can be doubted whether such differences could have been significant.
Both stretching exercises and manual therapy considerably decreased both neck pain and disability, and the difference in effectiveness between the 2 treatments was minor. Low-cost stretching exercises used in common healthcare are still recommended as an appropriate therapy intervention to relieve pain, at least in the short term, as a preliminary to active neck muscle training. However, if this does not help sufficiently, manual therapy remains the treatment of choice.
Advice about stretching exercises and manual therapy are among the most commonly used treatments for chronic neck pain. However, their effectiveness has not been compared in randomized studies. Manual therapy, consisting of deep muscle massage, stretching and joint specific mobilization techniques, significantly reduced neck pain. It was a slightly more effective option in decreasing disability and neck stiffness compared with stretching exercise, and the patients clearly favoured manual therapy. However, regular self-administered stretching was as effective in abolishing pain and thus may be considered as a first choice since it is easy to perform and inexpensive to introduce in practice.
ACKNOWLEDGEMENTS
The authors thank Jyväskylä Adult Centre of Education for providing manual treatments and secretary, Auli Koukonen, for making arrangements for the questionnaires and follow-ups. The research project was supported by a grant from Jyväskylä Central Hospital.
REFERENCES
1. Aromaa A, Koskinen S, eds. Health and functional capacity in Finland. Baseline results of the Health 2000 health examination survey. Publications of the National Public Health Institute B3/2002, Helsinki, 2002.
2. Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine 2003; 28: 1195–1202.
3. Kjellman G, Öberg B, Hensing G, Alexandersson K. 12-year
follow-up of subjects initially sicklisted with neck/shoulder or low back diagnoses. Phys Res Inter 2001; 6: 52–63.
4. Borghouts JAJ, Koes BW, Vondeling H, Boulter LM. Cost of illness in neck pain in the Netherlands in 1996. Pain 1999; 80: 629–636.
5. Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990–1997. Results of a follow-up survey. JAMA 1998; 280: 1569–1575.
6. Irnich D, Behrens N, Molzen H, König A, Gleditsch J, Krauss M, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ 2001; 322: 1–6.
7. Wolsko PM, Eisenberg DE; Davis RB, Kessler R, Phillips RS. Patterns and perceptions of care for treatment of back and neck pain: results of a national survey. Spine 2003; 28: 292–297.
8. Ylinen J, Takala EP, Nykänen M, Häkkinen A, Mälkiä E,
Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA 2003; 289: 2509–2516.
9. Furlan AD, Brosseau L, Imamura M, Irvin E. Massage for low-back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2002; 27: 1896–1910.
10. Hoving JL, Koes BW, De Vet HC, Assendelft WJ, Van der Windt DA, Van Mameren H, et al. Manual therapy, physical therapy or continued care by the general practitioner for patients with neck pain: short-term results from a pragmatic randomized trial. Ann Intern Med 2002; 136: 713–722.
11. Korthals-de Bos IB, Hoving JL, van Tulder MW, Rutten-van Molken MP, Ader HJ, de Vet HC, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ 2003; 26; 326: 911–914.
12. Beurskens AJ, de Vet HC, Koke AJ. Responsiveness of functional status in low back pain: a comparison of different instruments. Pain 1996; 65: 71–76.
13. Grossman SA, Sheidler VR, McGuire DB, Geer C, Santor D,
Piantadosi S. A comparison of the Hopkins Pain Rating Instrument with standard visual analogue and verbal descriptor scales in patients with cancer pain. J Pain Symptom Manage 1992; 7: 196–203.
14. Dixon JS, Bird HA. Reproducibility along a 10-cm vertical visual analogue scale. Ann Rheum Dis 1981; 40: 87–89.
15. Viikari-Juntura E, Takala E-P, Alaranta H. Neck and shoulder
pain and disability. Scand J Rehabil Med 1988; 20: 167–173.
16. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipul Physiol Ther 1991; 14: 409–415.
17. Hains F, Waalen J, Mior S. Psychometric properties of the neck disability index. J Manipulative Physiol Ther. 1998; 21: 75–80.
18. Stratford PW, Riddle DL, Binkley JM, Spadoni G, Westaway MD, Padfield B. Using the Neck Disability Index to make decisions concerning individual patients. Physiother Canada 1999; 51: 107–112.
19. White P, Lewith G, Prescott P. The core outcomes for neck pain: validation of a new outcome measure. Spine 2004; 29: 1923–1930.
20. Keltinkangas-Järvinen L, Rimon R. Rimon’s brief depression scale, a rapid method for screening depression. Psychol Rep 1987; 60: 111–119.
21. Ylinen J, Cash M, eds. Sports massage. London: Stanley Paul; 1988.
22. Ylinen J, ed. Stretching therapy. Edinburgh: Churchill Livingstone, Elsevier Ltd; 2006.
23. Hägg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 2003; 12: 12–20.
24. Brodin H. Cervical pain and mobilization. Int J Rehab Res 1984; 7: 190–191.
25. Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. Manipulative therapy and a low load exercise regimen each reduced the frequency and intensity of cervicogenic headache. Spine 2002; 27: 1835–1843.
26. Coppieters MW, Stappaerts KH, Wouters LL, Janssens K. The immediate effects of a cervical lateral glide treatment technique in patients with neurogenic cervicobrachial pain. J Orthop Sports Phys Ther. 2003; 33: 369–378.
27. Levoska S, Keinänen-Kiukaanniemi S. Active or passive physiotherapy for occupational cervicobrachial disorders? A comparison of two treatment methods with a 1-year follow-up. Arch Phys Med Rehabil 1993; 74: 425–430.
28. Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine 1996; 21: 1746–1759.
29. Koes BW, Bouter LM, van Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, et al. Randomised clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one-year follow-up. BMJ 1992; 304: 601–605.
30. Whitman JM, Fritz JM, Childs MJD. The influence of experience and specialty certifications on clinical outcomes for patients with low back pain treated within a standardized physical therapy management program. J Orthop Sports Phys Ther 2004; 34: 662–675.
31. Kjellman G, Skargren E, Öberg B. Prognostic factors for perceived pain and function at one-year follow-up in primary care patients with neck pain. Disabil Rehabil 2002; 24: 364–370.
32. Skargren EI, Öberg BE. Predictive factors for 1-year outcome of low-back and neck pain in patients treated in primary care: comparison between the treatment strategies chiropractic and physiotherapy. Pain 1998; 77: 201–207.
