LITTLE THERAPY, LITTLE PHYSICAL ACTIVITY: REHABILITATION WITHIN THE FIRST 14 DAYS OF ORGANIZED STROKE UNIT CARE
Julie Bernhardt, PhD1,2,3, James Chan, BSc, PT4,5, Ilona Nicola, BSc, PT1,3,4 and Janice M Collier, PhD1
From the 1National Stroke Research Institute, Austin Health, Heidelberg, 2School of Physiotherapy, Faculty of Health Science, La Trobe University, Bundoora, 3Royal Melbourne Hospital, Parkville, 4School of Physiotherapy, University of Melbourne, Melbourne and 5Nepean Rehabilitation Hospital, Frankston, Australia
OBJECTIVE: To examine rehabilitation interventions and resulting physical activity patterns of patients managed in acute stroke units to help inform development of a randomized controlled trial of very early rehabilitation.
DESIGN: An open observational study of patient activity and therapist report of patient interventions. A survey of stroke unit resources.
METHODS: Patients less than 14 days post-stroke from 5 metropolitan stroke units were observed over 2 consecutive weekdays at 10-minute intervals between 08.00 h and 17.00 h. Physical activity, location and person(s) present were ascertained at each observation. Therapists completed treatment records. Senior staff completed stroke unit surveys.
RESULTS: Patients after stroke (n=58) were with therapists 5.2% of the observed day. Few patients (17.1%) received daily therapy by more than one therapist. When patients received therapy, average session times were 24 minutes of physio therapy, 23 minutes of occupational therapy and 33 minutes of speech pathology. The more time that family members were present, the longer the treatment time. Four to 11 min of upper-limb therapy was provided. Muscle weakness and left hemiparesis were associated with less upper-limb activity.
CONCLUSION: These acute stroke care units were resourced according to recommended staff-patient ratios. Patients received little therapy and had low levels of physical activity.
Key words: stroke, rehabilitation, physical activity, upper limb, acute.
J Rehabil Med 2007; 39: 43–48
Correspondence address: Julie Bernhardt, National Stroke Research Institute, Level 1, Neurosciences Building, Austin Health, Heidelberg Repatriation Hospital, 300 Waterdale Road, Heidelberg Heights, 3081, Victoria, Australia. E-mail: j.bernhardt@unimelb.edu.au
Submitted February 28, 2006; accepted July 3, 2006.
Introduction
It is well accepted that stroke rehabilitation should commence as early as possible for optimal recovery to be achieved. Exactly how early rehabilitation should start is less well accepted. In recent years, evidence that stroke unit care results in better outcome, with fewer deaths and lower disability (1) has led to positive changes in stroke service delivery around the world. Multi-disciplinary care is an important feature of effective stroke units (2). Early intervention by the multi- disciplinary team may help to prevent secondary complications, such as pneumonia and deep venous thrombosis, commonly seen within the first week following stroke (3, 4) and promote brain reorganization and recovery (5). In reality, little is known about the rehabilitation provided to patients during the very early phase of stroke care.
As part of a planned series of studies to inform the development of a randomized controlled trial of very early rehabilitation (AVERT) with a focus on mobilization, we described the physical activity patterns of patients within the first 14 days post-stroke, managed in 5 acute stroke units (6). We found that patients spent more than half the day in bed and only 13% engaged in standing and walking activities with the potential to prevent complications and improve recovery of mobility. Additional data from observational and therapist records from this study provided an opportunity to detail the rehabilitation therapy provided to patients after stroke within organized stroke care settings.
In this paper, we describe the therapy provided to patients within the first 14 days of stroke. It is our intention to focus on physical rehabilitation (usually provided by occupational therapists, physiotherapists and nurses) and to identify factors that might contribute to the amount of therapy provided. Data from speech pathologists were included for completeness. We were interested in both whole-body activities: defined as those motor tasks involving coordinated movement of the whole body (e.g. sitting tasks including activities of daily living (ADL), sit to stand, standing, walking), and upper-limb activity: defined as any movement, with or without help, of either upper limb separately (affected or unaffected), or both arms at the same time (bilateral).
Specifically, our aims were to: (i) describe the observed levels of (a) whole-body and (b) upper-limb activity of patients when alone or with others (e.g. nurses, therapists); (ii) identify patient characteristics (e.g. side and type of stroke, upper-limb strength) associated with observed upper-limb activity patterns; (iii) describe the average intensity and frequency of therapy provided by physiotherapists (PT), occupational therapists (OT) and speech pathologists (SP) to patients, including upper-limb therapy; and (iv) identify whether a relationship existed between patient characteristics (e.g. stroke severity) and time spent with a therapist.
Methods
Study design and location
This was an open observational behavioural mapping study, including a survey of stroke unit resources and acquisition of detailed summaries of therapist interventions.
The study was undertaken in 5 of the 7 acute stroke units in metropolitan Melbourne (population 3.2 million), all of which are located at major teaching hospitals with active stroke research programs. Approval for this study was obtained from the ethics committee of each institution.
Patients
All cases of confirmed stroke (World Health Organization definition (7)) admitted less than 14 days after a first or recurrent stroke were suitable for inclusion, with the exception of those receiving palliative care. Patients were told that observations would help improve our understanding of stroke unit care.
Therapists
All therapists (PTs, OTs and SPs) providing an intervention to patients after stroke recruited to the observational study completed records of the amount and type of therapy provided in each session.
Therapists and nursing staff were told that the study aimed to provide information about the structure and current processes of care.
Data acquired by observation
Each participant was observed over 2 consecutive weekdays, from 08:00 h to 17:00 h. Observations were recorded every 10 minutes, except for 4 randomly scheduled 10-minute breaks throughout the day. At each observation point, category of physical activity (e.g. sitting, walking), the people present (e.g. family, staff), and the location of activity (e.g. bathroom) were recorded. The observational method, detailed previously (6), has been shown to be reliable.
Classification of observed level of physical activity
At each observation, patient activity could be classified into one or more of 15 motor activities. These included 11 whole-body activities (e.g. lying, sitting, walking) and 2 (affected and unaffected) upper-limb activity categories. The whole-body activities were grouped into 5 pre-specified activity categories (ACs) judged by experienced clinicians to reflect the degree of physical work during these activities. These were: no activity (AC 0, asleep, inactive), non-therapeutic activity (AC 1, eating, watching television in bed), minimal therapeutic activity (AC 2, transfer by hoist, sit in chair), moderate therapeutic activity (AC 3, standing, sit unsupported), and high therapeutic activity (AC 4, walking, stairs) (6). ADL activities were classified according to the extent of movement required by the patient to complete the activity. For example, upper body dressing conducted with the patient seated in a chair would fit under AC2 (sitting) and include counts of upper-limb activity. When patients were seen to be moving either upper limb separately, or both together (bilateral), activity was recorded.
People in attendance and location of activity
There were 11 possible categories, ranging from family, nurses, medical staff, therapists (e.g. OT, PT, SP), porters and others. The 5 locations were bedroom, bathroom, hall, therapy area and off ward.
Data acquired from therapists
Therapists completed a treatment record for all patient interactions during the observation period. The treatment record focused on the patients’ physical activity resulting from the treatment (not the treatment approach of the therapist e.g. Bobath, motor relearning program etc). Seven physical activities were specified; bed mobility, sitting, sit to stand, standing, early gait, advanced gait and upper-limb activities. Behavioural operational definitions were provided for each activity. An “other” category was used to record assessments, language therapy, etc, that did not fit into the specified activity categories. Therapists recorded the time (minutes) the patient spent on each activity. Physiotherapists’ recording of treatment category and time in this way has been shown to have good accuracy, with very little over- or under-estimation of time (8). A priori, the 6 whole-body physical activity categories in the treatment record were matched to the activity categories (AC 0–4) detailed above to allow consistent reporting of the level of activity engaged in by the patient when they were directly observed or being treated by a therapist.
Additional pre-specified data
Stroke type was classified using the Oxfordshire Community Stroke Project Classification (9). Neurological impairment was determined using the National Institutes of Health Stroke Scale (NIHSS) (10) obtained retrospectively from the medical record (11). Patients were grouped into mild (NIHSS <8), moderate (NIHSS 8–16) and severe (NIHSS >16) stroke categories (12), to allow for examination of therapy interventions according to stroke severity. The NIHSS has established reliability and validity in acute stroke patients (11). Living arrangements prior to stroke were recorded. Pre-stroke mobility was classified as independent (with or without aids), supervised or dependent. It was noted whether English was the patient’s first language. Mobility at time of observation was recorded using the Mobility Scale for Acute Stroke patients (MSAS) (13). Performance on 5 activities (bridging, supine to sit, sitting, standing up and walking) is examined, with an MSAS score of 0 indicating the patient is unable to perform the activity, and a score of 6 indicating they are unassisted and safe. The MSAS has good reliability and validity in acute stroke patients (13, 14). Hand dominance, as reported by the patient or family was recorded, together with best strength of the affected shoulder (using the 0–5 shoulder component of the Motricity Index (15)) This widely used clinical test scores the capacity of the patient to move their limb against gravity, with a score of 0 indicating no movement and score of 5 indicating “normal power”. Inter-rater reliability has been established for the Motricity Index (15). Upper-limb sensation was tested using a routine clinical test of light touch with cotton wool. Sensation was categorized as intact (all 6 touches to the limb felt), impaired (< 6 felt) or absent (no touches felt). Although standardized across patients, no formal reliability or validity testing has been conducted.
Stroke unit data
A survey was used to gather descriptive data about the stroke unit, including size, length of stay, staffing (both usual and at time of observation), ward layout and rest routines of each unit observed.
Data management and statistical analysis
The database (Microsoft Access) was designed to automatically calculate the highest level of whole-body activity for data obtained from direct observation and the therapist records from AC 0 (no activity) to AC 4 (high activity). Systat version 10 (SPSS Inc.) was used for all analyses. When averages are reported, observed data and therapist data are pooled across sites and over days.
To address the stated aims of the study, we:
• calculated the proportion of the observed day that the patient was engaged in (i) whole-body and (ii) upper-limb activity; when alone, or in the presence of others.
• performed a stepwise, one-way ANOVA (p <0.05) to examine factors associated with affected upper-limb activity. Factors included side of stroke, stroke type, shoulder strength, sensory deficit, and whether the dominant hand was the affected limb. Factors associated with amount of whole-body activity have been reported elsewhere (6).
• calculated the average intensity (minutes per session) and frequency (number of sessions per day) of all PT, OT and SP sessions and determined the average intensity and frequency of affected upper-limb therapy provided within each session.
• performed stepwise, one-way ANOVAs (p <0.05) to identify factors associated with (i) being treated by a therapist and (ii) the intensity of treatment by a therapist. Factors included patient age, number of days post stroke, proportion of time family were present, stroke unit site, and stroke severity (NIHSS). The Fisher exact test was used to test for differences in therapy provided to those with first or recurrent strokes and those for whom English was a first or second language.
Results
Patients
All patients meeting inclusion criteria were invited to participate in this study (n=66). A total of 64 consented and 58 participants completed both days of observation. Drop-outs comprised 5 patients discharged early and one transferred to palliative care. The average number of days post-stroke at time of first observation was 5.6 (ranging from day 0 to day 14 post stroke). Patients had a mean (standard deviation) age of 71.3 (12.6) years ranging from 30 to 96 years; with equal numbers of males and females. Thirty-eight patients (65.5%) were admitted with first-ever stroke and 51 (88.0%) were infarcts. The proportions of patients with left- and right-sided strokes were similar, with 26 left- and 32 right-sided lesions. Most patients were living alone (24.1%) or with family (67.3%) prior to the stroke and the majority (98.3%) were independently mobile. Upper-limb characteristics of patients are reported in Table I.
| Table I. Upper-limb characteristics (n = 58) | |
| n (%) | |
| Dominant hand Left Right | 4 (6.9) 54 (93.1) |
| Sensation Total loss Impaired Intact | 3 (5.2) 13 (22.4) 42 (72.4) |
| Shoulder strength 0: No movement 1: Palpable contraction but no movement 2: Visible movement but not full range or against gravity 3: Full range against gravity but not resistance 4: Full strength against resistance but weaker than other side 5: Full strength / normal power | 15 (25.9) 2 (3.4) 2 (3.4) 6 (10.4) 13 (22.4) 20 (34.5) |
Therapists
Twenty-five therapists participated in this study, 12 PT, 8 OT and 5 ST. Their post graduate clinical experience ranged from 6 months to 15 years. Staff/patient ratios for each discipline in the stroke units were: 1:10–1:12 (PT); 1:11–1:14 (OT); and 1:20–1:24 (SP). Nurse/patient ratios were uniform at 1:4.
Stroke unit characteristics
Stroke unit size ranged from 6 to 20 beds, with average length of stay ranging from 6.2 days to 14.0 days. Only one site had a therapy room on the same floor as the stroke unit. On 2 of the 5 stroke units rest periods for patients were strictly enforced.
Observed whole-body activity alone and with others
We were unable to ascertain activity on only 25 occasions (0.4% of observations). Fig. 1 shows the level of activity (AC 0–4) patients after stroke engaged in when they were alone (60.4% of the day), and with family, therapists, nursing and medical staff. Patients were most active when with a PT, OT or nurse. When alone, patients spent less than 10% of the day engaged in standing and walking (AC 3 or 4) activity. On closer inspection, those patients unable to walk (MSAS=0) spent 98.1% of the day in bed (AC 0 or 1) and 0.2% of day in high activity. Patients able to walk independently (MSAS=6) still spent 40.5% of the day in bed, but also spent 31.0% of the day in moderate to high activity (AC 3 or 4). As expected, these results indicate that patients able to walk independently accounted for most of the observed standing and walking activity when patients were alone. A small number of patients judged by staff to require supervision when walking (n=7) were also observed to be walking or standing 10.5% of the time they were alone.
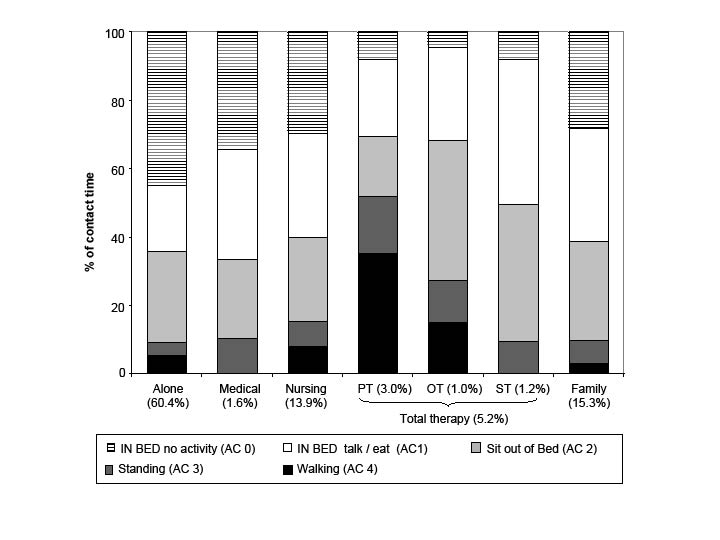
Fig. 1. Proportion of the day when patients were alone or with key others (accounting for 96.4% of the day) and their physical activity patterns during this time.
Observed upper-limb activity alone and with therapists
Fig. 2 illustrates upper-limb use both in the presence of a therapist (5.2% of the day) and when not in the presence of a therapist (94.8% of the day). In both cases, 67% of the time the affected upper limb was not observed to be moving. Affected upper-limb activity accounted for 6% of time when a therapist was present and 1% when a therapist was not present.
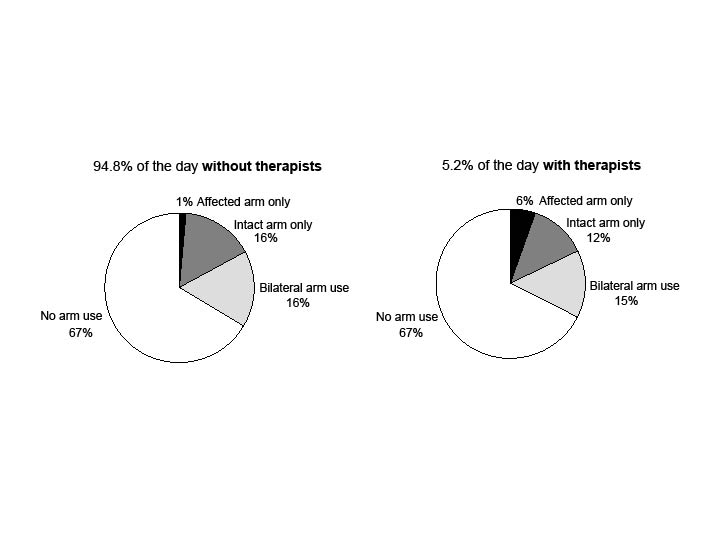
Fig. 2. Observed upper-limb activity over 94.8% of the day (08.00–17.00 h) when not in therapy and over 5.2% of the day when a therapist was present. These figures show little affected upper-limb activity (most use in bilateral activities), irrespective of a therapist being present.
Factors related to observed affected upper-limb activity
Prior to the analysis, a square root transformation of the data was performed as residuals did not conform to assumptions. Of the factors examined, only side of stroke (p=0.012) and shoulder strength (p<0.0001) were independently associated with the amount of affected upper-limb activity observed. The affected limb was observed to move less in those patients with left-sided hemiparesis (right-sided stroke), and those with moderate or severe shoulder weakness (strength score 0–3). Whether the affected hand was the patients’ dominant hand was not independently related to the amount of affected upper-limb activity.
Therapy provided
In total, 148 treatments were provided by therapists over the 2 observation days, but not all patients were seen by a therapist and treatment by more than one therapist on consecutive days was uncommon (Table II). Unlike many rehabilitation programs, therapists did not schedule patient treatments. Individual therapists reported treatment goals in the history, but there were no team records of goals. Only 0.2% of the time, patients were treated in a dedicated therapy area. Most of the time (98.0%), therapy occurred at the patient’s bedside, with the remainder occurring in the hall. Although therapy was delivered between 08.20 h and 17.00 h, highest activity (59%) occurred between 09.00 h and 12.30 h. Enforced afternoon rest periods at 2 units contributed to this finding. Both PTs and OTs provided therapy for the upper limb, with OTs more commonly incorporating the upper limb into therapy sessions.
| Table II. Intensity and frequency of therapy provided by physiotherapists (PT), occupational therapists (OT) and speech pathologists (SP) (n=58). Total therapy and upper-limb components are reported | |||
| PT | OT | SP | |
| All therapy | |||
| Sessions | |||
| Total number of sessions | 84 | 37 | 24 |
| Average number (%) of patients treated per day | 43 (74.1) | 27 (46.6) | 18 (31.0) |
| Number (%) of patients treated by both PT and OT on any 1 day | 24 (41.4) | ||
| Number of patients (%) treated on 2 consecutive days | 38 (65.5) | 10 (17.2) | 6 (10.3) |
| Number of patients (%) treated on 2 consecutive days by both PT and OT | 10 (17.2) | ||
| Intensity | |||
| Average minutes (SD) per session | 24.5 (12.3) | 22.8 (11.8) | 32.5 (18.5) |
| Range per session (minutes) | 3–65 | 2–52 | 5–60 |
| Frequency | |||
| Average number of sessions per day | 0.74 | 0.47 | 0.31 |
| Number of patients treated > once on any day | 3 | 0 | 0 |
| Upper-limb therapy component | |||
| Number (%) of patients treated | 26 (46.6) | 22 (37.9) | Not applicable |
| Average minutes (SD) per session | 4.1 (3.1) | 11.2 (8.0) | Not applicable |
| Range per session (minutes) | 1–20 | 1–40 | Not applicable |
| SD: standard deviation. | |||
Patients were off the ward for investigations and therefore unavailable for treatment for 6% of the day (approximately 32 minutes). Investigations ranged in length from 10 minutes (X-ray) to 30–60 minutes (MRI).
Factors associated with treatment by a therapist and intensity of treatment
Of the factors examined, only stroke unit site was independently associated with whether or not a patient received therapy. Patients managed in one stroke unit were less likely to be seen by a therapist. This stroke unit had similar characteristics to other observed sites, with an enforced rest period and no therapy treatment area. Staffing levels on the days of observation were normal. On average, patients who were seen by a therapist were less severe, with lower NIHSS scores (mean 9.3), than those not seen by a therapist (mean NIHSS 13.0). This difference approached significance (p=0.083).
The amount of time family were present was the only factor associated with treatment intensity (p=0.006). Patients with family present more often throughout the day had longer treatment sessions. This was an interesting finding. On looking more closely at the data, we determined that family were present for only 19.7% of total therapy time. Most of the time (80.3%) therapists were alone with the patient or with other therapists or nurses. We looked more closely at patient activity when both the therapist and family were present to see whether interaction or information exchange between the therapist and the family (with the patient doing nothing) might account for a large proportion of time. This proved not to be the case. We found that patients were inactive (AC O) only 15% of the time, that is, the majority of time family were present (85%) patients were active and engaged in therapy.
Stroke severity and therapy
As expected, the physical activity patterns of patients during PT and OT varied according to stroke severity. Patients with severe stroke (NIHSS >16) were treated by a PT and received longer treatment sessions than patients after mild stroke. OT saw two patients for assessment (without the patient moving) (Fig. 3).
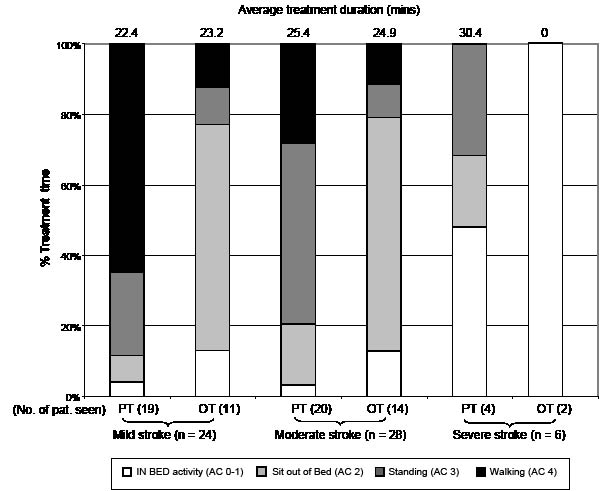
Fig. 3. Whole-body activity categories of patients during treatment by physiotherapists (PT) and occupational therapists (OT), grouped according to stroke severity: mild (NIHSS < 8); moderate (NIHSS 8–16); severe stroke (NIHSS > 16). Number of patients in each severity group that were seen by an OT or PT on at least one day of observation is shown in brackets. PTs spent greater treatment time with patients engaged in standing and walking activities than OTs. Average treatment duration in minutes is shown at the top of the figure.
DISCUSSION
An important first step in the development of our very early rehabilitation trial was to understand current practice. This study was necessary because little was known about the therapy provided by OT, PT and SP in the first 14 days after stroke and how their input might influence the physical activity patterns of patients. We acknowledge that our approach, combining detailed patient observation and therapist self-report over several days, has limitations. However, these methods allow a window into clinical practice not easily accessed by any other means.
We found that therapists were present for only a small proportion of the patients’ day. However, when PTs and OTs were present, patients were more frequently engaged in standing and walking activities. On average, when patients were seen by a PT or OT, the sessions lasted approximately 24 minutes, which may have included 4–11 minutes of upper-limb training. The limited time spent treating the upper-limb was not surprising, given that even in subacute rehabilitation (generally better resourced than acute services), patients after stroke receive an average of 5 minutes of upper-limb therapy per day (16).
As expected, SP spent little time standing or walking with the patient or facilitating upper-limb activity. Most speech and swallowing interventions were performed whilst the patient was sitting in bed or out of bed. Nurses however, spend more time with patients than all other staff and play a key role in helping patients to move. We found that approximately 12 min of moderate to high level activity occurred in the presence of nurses each day. Although therapists, especially PT, and nurses helped patients engage in higher levels of activity when they were present, most of the day patients were alone. As expected, patients with mobility limitations (requiring assistance to move) did not stand or walk when alone. However, even patients who were independently mobile spent a large part of the day lying down or sitting in a chair. This finding was interesting, reinforcing that even those with mild strokes should be included in our early mobilization trial.
Staff to patient ratios will obviously play some role in determining the interventions provided to patients after stroke. Other factors, such as patient selection criteria, model of stroke unit, e.g. acute assessment, comprehensive stroke unit (acute plus rehabilitation) etc, philosophy of care and policies and procedures (17) may also play a significant role in determining the level of active rehabilitation received by patients early after stroke. Based on their systematic review of stroke units, Langhorne & Dennis (18) propose that an effective 10-bed stroke unit might employ 1–2 PTs, 0.9–1.3 OTs and 0.2–0.6 SPs. The staff ratios of the units included in the current study were similar to the lower ends of the range for PT, and OT, and the higher end of the range for speech pathology. Although the stroke units we observed were staffed in line with recommended ratios, very low levels of physical activity were found. Staffing levels were not responsible for our finding that patients managed in one of the stroke units in this study received therapy less frequently than patients in the other 4 units.
Whether 24 minutes of occupational and/or physiotherapy a day is sufficient to prevent secondary complications or disuse deconditioning or promote faster recovery is unknown. We do know, however, that stroke units with proven effectiveness in reducing death and disability report a median intensity of 45 min of physiotherapy per patient per weekday, and occupational therapy of 40 minutes per patient per weekday (2). However, all of the 11 units included in this detailed survey provided either acute plus rehabilitation care (comprehensive stroke unit), or subacute rehabilitation care (rehabilitation stroke unit). The stroke units we studied provided substantially less physiotherapy and occupational therapy per day.
Only one unit in this study was described as a comprehensive stroke unit (combining acute and rehabilitative care). In the case of the other 4 stroke units, the treating team viewed their role as assessing all newly admitted patients and then prioritized their intervention in order to minimize acute length of stay, i.e. they were acute (semi-intensive) units. Staff reported that patients coming into their unit are “triaged” as either suitable for: (i) discharge home from the acute setting (with or without rehabilitation); (ii) transfer to inpatient rehabilitation; (iii) transfer to nursing home care; or (iv) palliation. Patients judged to require nursing home care long-term are generally considered a low priority for therapy as they are already at a functional level consistent with their destination. Patients suitable for discharge home from the acute setting are given priority to expedite discharge. In these types of acute units, less therapy is not unexpected. Interestingly, the recently updated systematic review of stroke units indicates that there is currently insufficient data to conclude that acute (semi-intensive) units reduce death and dependency. In contrast, stroke units that incorporate rehabilitation have proven benefit (19).
While evidence in support of stroke rehabilitation is strong, research seeking to establish the optimal timing, intensity and frequency of therapy is sparse. This is particularly true in the very early period (first 7 days) after stroke. Given that research from animal studies (20, 21) has led to concern that intensive exercise commenced very early after stroke may do more harm than good (22), safety studies of very early interventions are required. Phase 2 (safety and feasibility) of AVERT, commenced in May 2004. We hope in time to contribute to the refining of rehabilitation practices in stroke unit care models through provision of high-quality evidence about timing, intensity and frequency of interventions promoting mobility.
ACKNOWLEDGEMENTS
We are grateful to the patients and therapists who participated in this study. Dr Bernhardt was supported throughout this study by an NHMRC Training Fellowship (#157305), and with grants from the Austin Medical Research Fund, and Perpetual Trustees.
References
1. Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke (Cochrane Review). Oxford; Update Software: Cochrane Library; 2001.
2. Langhorne P, Pollock A. What are the components of effective stroke unit care? Age Ageing 2002; 31: 365–371.
3. Bamford J, Dennis M, Sandercock P, Burn J, Warlow C. The frequency, causes and timing of death within 30 days of a first stroke: the Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatry 1990; 53: 824–829.
4. Langhorne P, Stott D, Robertson L, MacDonald J, Jones L, McAlpine C, et al. Medical complications after stroke: a multicenter study. Stroke 2000; 31: 1223–1229.
5. Nudo RJ. Functional and structural plasticity in motor cortex: implications for stroke recovery. Phys Med Rehabil Clin N Am 2003; 14: S57–S76.
6. Bernhardt J, Dewey HM, Thrift AG, Donnan GA. Inactive and alone: physical activity in the first 14 days of acute stroke unit care. Stroke 2004; 35: 1005–1009.
7. Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 1976; 54: 541–553.
8. Wittwer J, Goldie PA, Matyas TA, Galea MP. Quantification of physiotherapy treatment time in stroke rehabilitation – criterion-related validity. Aust J Physiother 2000; 46: 291–298.
9. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991; 337: 1521–1526.
10. Brott T, Adams H, Olinger C, Marler J, Barsan W, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870.
11. Kasner S, Chalela J, Luciano J, Cucchiara B, Raps E, McGarvey M, et al. Reliability and validity of estimating the NIH stroke scale score from medical records. Stroke 1999; 30: 1534–1537.
12. Briggs D, Felberg R, Malkoff M, Bratina P, Grotta J. Should mild or moderate strokes be admitted to an intensive care unit? Stroke 2001; 32: 871–876.
13. Simondson JA, Goldie P, Brock K, Nosworthy J. The Mobility Scale for Acute Stroke Patients: intra-rater and inter-rater reliability. Clin Rehabil 1996; 10: 295–300.
14. Simondson JA, Goldie P, Greenwood KM. The Mobility Scale for Acute Stroke patients: Concurrent validity. Clin Rehabil. 2003; 17:558–564.
15. Collin C, Wade D. Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry 1990: 576–579.
16. Goldie P, Matyas T, Kinsella G. Movement rehabilitation following stroke. Research report to the Department of Health, Housing and Community Services. Melbourne, Australia: Department of Physiotherapy, La Trobe University; 1992.
17. Cadilhac D, Ibrahim J, Pearce D, Ogden K, McNeil J, Davis SM, et al. Multicenter comparison of processes of care between stroke units and conventional care wards in Austarlia. Stroke 2004; 35: 1035–1040.
18. Langhorne P, Dennis M. Stroke Units: an evidence based approach. London: BMJ Books; 1998.
19. Langhorne P, on behalf of the Stroke Unit Trialists’ Collaboration. The effect of different types of organised inpatient (stroke unit) care: an updated systematic review and meta-analysis. Cerebrovas Dis 2005; 19 suppl 2: 17.
20. Humm JL, Kozlowski DA, James DC, Gotts JE, Schallert T. Use-dependent exacerbation of brain damage occurs during an early post-lesion vulnerable period. Brain Res 1998; 783: 286–292.
21. Risedal A, Zeng J, Johansson BB. Early training may exacerbate brain damage after focal brain ischaemia in the rat. J Cereb Blood Flow Metab 1999; 9: 997–1003.
22. Pomeroy V. Need to focus research in stroke rehabilitation. Lancet 2000; 355: 836–837.
