Vera Storm, MSc1, Juliane Paech, PhD1, Jochen P. Ziegelmann, PhD2 and Sonia Lippke, PhD1,3
From the 1Department of Psychology and Methods, Jacobs University Bremen, Bremen, 2German Centre of Gerontology, Berlin and 3Bremen International Graduate School of Social Sciences, Bremen, Germany
OBJECTIVE: Physical exercise recommendations become particularly effective when embedded into medical rehabilitation. However, little is known about long-term behaviour maintenance and its effect on sickness absence and subjective employability. The current longitudinal observational study investigated self-reported physical exercise, sickness absence and subjective employability over a period of 8 years.
SUBJECTS: A total of 601 (T0) outpatients (mean age 45.14 years; standard deviation 10.73 years, age range 18–65 years) with different orthopaedic disorders were recruited during their 3-week medical rehabilitation in Germany. Of these, 61.7% (n = 371) were female. Follow-ups were carried out at 6 months (T1, n = 495), 12 months (T2, n = 340), 3 years (T3, n = 296) and 8 years (T4, n = 142) after baseline.
METHODS: Patient characteristics, exercise status, social-cognitive variables, sickness absence and subjective employability were obtained via self-report questionnaires. SPSS hierarchical regression models were used for data analysis, controlling for baseline measures and sociodemographic variables.
RESULTS: Physical exercise status 6 months after rehabilitation treatment (T1) predicted sickness absence at 12 months (T2). Inactive people were 3.28 times more likely to be on sick leave at T2. In addition, physical exercise at T1 predicted subjective employability 12 months (T2) and 3 years (T3) later. Those who met the recommendations to be physically active for at least 40 min a week were more likely to feel able to work.
CONCLUSION: Exercise appears to play an important role in reducing sickness absence and subjective employability and should be promoted within and after rehabilitation treatment.
Key words: medical rehabilitation; musculoskeletal diseases; physical exercise; sickness absence; subjective employability.
J Rehabil Med 2016; 48: 541–546
Correspondence address: Vera Storm, Jacobs Center on Lifelong Learning, Jacobs University Bremen, Campus Ring 1, DE-28759 Bremen, Germany. E-mail: v.storm@jacobs-university.de
Accepted Mar 31, 2016; Epub ahead of print May 30, 2016
INTRODUCTION
Over the past several years, the demand for rehabilitation services has grown. Patients undergoing rehabilitation due to musculoskeletal diseases (MSD) make up the largest proportion of rehabilitation patients in industrialized countries (1). MSD, such as joint or spinal injuries, as well as pain in the nerves and muscles, are the most common cause of chronic severe pain, long-term physical disability, work limitations and unemployment (1, 2). The prevalence of many of these conditions increases markedly with age and is often affected by lifestyle factors, such as physical inactivity (3). Physical exercise, as a target health behaviour in MSD rehabilitation programmes, is well known for its positive effects on physical and mental health (4). Physical exercise programmes usually include the domains of muscle, strength and endurance training (5).
Much research has been carried out on functional performances, reported level of pain, or disability improvement after rehabilitation (6). However, researchers now increasingly recognize that successful return to work (RTW) and fewer sick days are also key outcomes in determining the effectiveness of rehabilitation.
Patients with MSD report multiple difficulties when trying to return to, or remain at, work. Difficulties include pain, its impact on work performance and fear of re-injury (7, 8). It is likely that physical exercise not only improves people’s functioning in terms of flexibility, strength, endurance and reduction in pain (9), but it might also have an indirect effect on feeling able to work, by means of an improvement in health status (10). In recent reviews regarding the long-term effects of rehabilitation exercise therapy, researchers have found evidence for a reduction in sick days (6) and faster RTW outcomes (11, 12).
After discharge from rehabilitation treatment, patients are usually highly motivated to practice the intended behaviour. However, it is difficult for many patients to adopt and, in particular, to maintain, the recommended behaviours, even if they strongly intend to do so (13, 14). From a prevention perspective, screening for predictive factors and obstacles associated with long-term health behaviour change and employability offers a promising avenue for medical rehabilitation. Work resumption is an important goal, not only for economic reasons, but also because it benefits most patients’ mental and physical health status (10, 15). Since long-term outcomes are of importance to the individual and society, the authors of the longitudinal study presented here will assess the contribution of physical exercise to sickness absence and subjective employability up to 8 years after discharge from rehabilitation treatment. Therefore, we hypothesize that physical exercise not only predicts sickness absence at the different follow-ups (hypothesis 1), but that physical exercise also predicts subjective employability at the different follow-ups (hypothesis 2).
METHODS
Design
An 8-year prospective longitudinal design was used for this observational study, performed between 2001 and 2009 in Berlin, Germany.
Procedure and participants
The first measurement point of the study (T0) was conducted in an outpatient orthopaedic rehabilitation centre, where participants underwent daily exercise therapy for 3 weeks. All rehabilitation patients who met the inclusion criteria, such as: (i) being at least 18 years old; (ii) no cognitive impairments; (iii) being capable of exercising on their own; and (iv) German language proficiency, were approached in a face-to-face meeting by their physicians and invited to participate.
After obtaining informed consent, 637 persons were assessed with paper-and-pencil questionnaires. Physicians diagnosed patients with different musculoskeletal diseases, such as back pain, disc disorders, joint conditions and injuries. The goal of the rehabilitation programme was to improve their level of functioning, enhance their ability to work, and increase their chances of returning to work, i.e. feeling able to return to work.
Thirty-six people who were either younger than 18 years (n = 1) or older than 65 (n = 35) years at T0 were excluded in order to obtain a representative sample of the German working population. The final sample comprised 601 people, with a mean age of 45.14 years at baseline, standard deviation (SD) 10.73 years, and age range 18–65 years), 61.7% (n = 371) were female. Of the participants, 68.7% (n = 413) were living with a partner and 71.5% were employed either full-time, part-time or self-employed; of these, 50.1% were on sick leave.
Follow-ups were carried out at intervals of 6 months (T1, n = 495), 12 months (T2, n = 340), 3 years (T3, n = 269) and 8 years (T4, n = 142) after baseline T0 (Fig. 1). For each measurement point only people up to the maximum age of 65 years were included as this was representative for the German working population. The follow-up questionnaires (including prepaid reply envelopes) were sent by the project staff via mail. Those who did not respond after 4 weeks were sent a reminder letter, along with another copy of the questionnaire and a prepaid envelope. The completion of each questionnaire took approximately 15 min. Participation in the study was voluntary and data were anonymized.
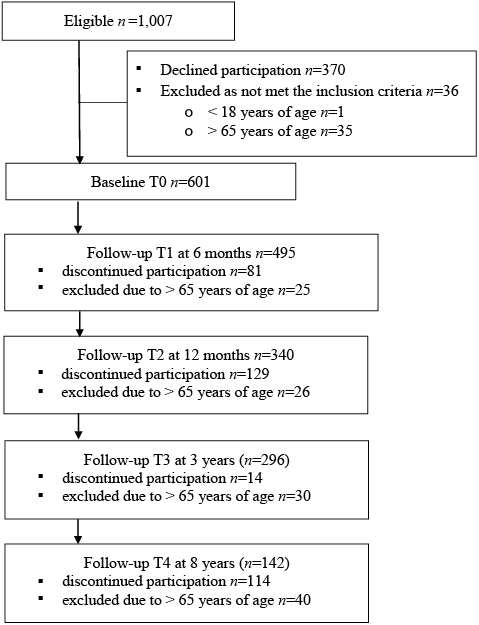
Fig. 1. Participant flow through study.
Measures
Demographic variables. Socio-demographic information, such as gender, year of birth, partner status and highest level of education, was assessed in the baseline questionnaire (T0). Height and body weight, used to calculate body mass index (BMI), were also reported by the participants on all measurement points (T0, T1, T2, T3, T4). All item examples given below are translations from German.
Sick leave and return to work rates. At baseline T0, 50.1% of the participants (n = 301) reported currently being on sick leave. For each follow-up measurement point, we calculated the proportion who had returned to work after being on sick leave at baseline. Percentages refer to the sample size at the respective follow-up. Six months after rehabilitation (T1) 61 people (13%) had still not returned to work. Twelve months after rehabilitation (T2) 35 participants (10.3%) had not resumed work, whereas after 3 years (T3) 32 participants (10.8%) and after 8 years (T4) 14 participants (9.9%) were on sick leave.
Subjective employability. Participants were asked to rate their subjective ability to work at T1, T2, T3, and T4 by answering whether they felt able to work full-time or part-time, which they answered as either “not true” (1), “hardly true” (2), “rather true” (3) or “definitely true” (4).
Physical exercise. Physical exercise was assessed at T0, T1, T2, T3, and T4, with a modified version of the International Physical Activity Questionnaire (IPAQ) (16). The IPAQ has been shown to be a valid reliable instrument among rehabilitation patients and beyond (17). We exclusively used targeted physical activity (endurance sports, muscle training, game sports) for data analysis because this subset constituted the best match with the exercise recommendations of the rehabilitation clinic. To compute exercise duration, we multiplied minutes of exercise per day with exercise days per week. This is a common routine in IPAQ research (17). Based on Tabachnick & Fidell’s definition (18), 18 values higher than 3 SD were defined as outliers and were re-coded to the closest non-outlying value in the data distribution. People who reported that they would exercise less than 40 min per week were categorized as inactive as this was the minimal recommendation by the doctors overseeing the rehabilitation (19).
Intention. Exercise intentions (Cronbach’s α = 0.68) were assessed at T0, T1, T2, T3 and T4, with 9 items, such as “I intend to exercise for 20 min or longer on at least 2 days per week on a regular basis health.” Participants rated all answers of the intention variable on a 4-point scale from “not at all true” (1), “not true” (2), “a little true” (3), to “exactly true” (4). Exercise intentions have shown validity within and beyond rehabilitation samples (20, 21).
Table I provides a summary of all descriptions regarding the measured variables.
|
Table I. Summary of the main study variables |
||||||||||||||
|
Measure |
T0 n = 601 |
|
T1 n = 495 |
|
T2 n = 340 |
|
T3 n = 296 |
|
T4 n = 142 |
|||||
|
Mean (SD) |
Range |
|
Mean (SD) |
Range |
|
Mean (SD) |
Range |
|
Mean (SD) |
Range |
|
Mean (SD) |
Range |
|
|
Intention |
3.47 (0.48) |
1.25–4.0 |
3.48 (0.51) |
1.38–4 |
3.44 (0.55) |
1–4 |
|
3.44 (0.52) |
1.38–4 |
3.22 (0.56) |
1.13–4 |
|||
|
Subjective employability |
3.47 (0.48) |
1–4 |
|
2.86 (1.22) |
1–4 |
|
3.04 (1.17) |
1–4 |
|
2.99 (1.20) |
1–4 |
|
2.86 (1.27) |
1–4 |
|
Age, years |
45.14 (10.73) |
18–65 |
|
46.24 (10.56) |
20–65 |
|
47.22 (10.49) |
21–65 |
|
48.56 (10.13) |
23–65 |
|
52.03 (9.30) |
26–65 |
|
|
n (%) |
|
n (%) |
|
n (%) |
|
n (%) |
|
n (%) |
|||||
|
Physical exercise Inactivea Active |
308 (51.2) 293 (48.8) |
|
121 (25.8) 348 (74.2) |
|
92 (27.1) 248 (72.9) |
|
100 (33.8) 196 (66.2) |
|
54 (38.0) 88 (62.0) |
|||||
|
aInactive: < 40 min physical exercise/week, active: > 40 min physical exercise/week. SD: standard deviation. |
||||||||||||||
Data analysis
The data were analysed with SPSS version 22 software. Dropout analyses were performed with t-tests for the continuous variables and χ2 test for the categorical variable gender.
First, we used hierarchical logistic regression to investigate whether the dichotomized predictor physical exercise (0 = active, 1 = inactive) would predict sickness absence at the different follow-ups (hypothesis 1). As the participants showed their maximum levels of physical exercise at T1, we used exercise status at T1 as a predicting variable. The results of the logistic regression analyses are presented as an odds ratio (OR). The reliability of the OR is expressed as a 95% confidence interval (CI). Statistical significance was set at p < 0.05 for the multiple regression analyses.
Secondly, we used hierarchical linear regression to analyse the effect of the dichotomized predictor physical exercise (0 = active, 1 = inactive) and assumed that it would predict subjective employability at the different follow-ups (hypothesis 2).
In recent reviews, age and BMI were found to be strong predictors of the development and progression of certain musculoskeletal diseases, such as osteoarthritis of the hand, knee and hip (22). Therefore, besides education, family status, T0 physical exercise, T0 intentions, and T0 subjective employability, age and T0 BMI were used as control variables.
RESULTS
Preliminary analysis
We found significant age differences between dropouts and those who participated in all follow-up questionnaires (T0: t(600) = 7.52, p = 0.006; T1: t(494) = 7.58, p = 0.006; T3: t(339) = 4.62, p = 0.032). The dropouts after baseline were significantly older and the dropouts after 6 months and after 3 years were significantly younger than those who completed all measurement points. Regarding gender, there were no differences in dropout rates after 6 months (T1), 12 months (T2) and 3 years (T3) (all: p > 0.248). In addition, participants who dropped out after 6 months (T1), 12 months (T2) or 3 years (T3) reported no significant differences regarding baseline exercise behaviour (all: p > 0.241). Those who dropped out after 6 months (T1) and 12 months (T2) did not differ in terms of subjective employability (T1) (all: p > 0.115) from those who completed all measurement points. However, those who dropped out after 3 years (T3) showed significantly lower levels of T1 subjective employability than those who also completed the T4 measurement point (t(295) = 4.61, p = 0.032).
Main analysis
First, we performed multiple logistic regression to analyse the predictive value of physical exercise (0 = active, 1 = inactive) for sick leave absence (0 = no sickness absence, 1 = sickness absence). Results are shown in Table II. T1 physical exercise predicted sickness absence at T2 (OR: 3.28, 95% CI: 1.05–2.16, p = 0.002). The odds of being on sick leave at T2 was 3.28 times higher in people who were inactive at T1, irrespective of sociodemographic variables and baseline physical exercise (T0). There were no effects of physical exercise on sick leave at T3 or on T4 absence.
|
Table II. Hierarchical regression results on sickness absence |
||||||||
|
|
Sick leave T2, n = 340 (Ref: on sick leave) |
|
Sick leave T3, n = 96 (Ref: on sick leave) |
|
Sick leave T4, n = 142 (Ref: on sick leave) |
|||
|
OR (95% CI) |
p-value |
|
OR (95% CI) |
p-value |
|
OR (95% CI) |
p-value |
|
|
Step 1 |
|
|
|
|
|
|
|
|
|
Control variablesa |
|
0.868 |
|
|
0.630 |
|
|
0.295 |
|
Nagelkerke‘s R2 |
0.02 |
|
|
0.03 |
|
|
0.19 |
|
|
Step 2 |
|
|
|
|
|
|
|
|
|
Physical activity T1 Ref: inactiveb |
3.28 (1.52–7.06) |
0.002 |
|
0.96 (0.35–2.64) |
0.939 |
|
1.18 (0.20–6.90) |
0.851 |
|
Nagelkerke‘s R2 |
0.07 |
|
|
0.04 |
|
|
0.20 |
|
|
Step 3 |
|
|
|
|
|
|
|
|
|
Physical activity T2 Ref: inactiveb |
3.13 (1.41–6.96) |
0.005 |
|
1.73 (0.65–4.64) |
0.274 |
|
1.79 (0.29–11.17) |
0.536 |
|
Nagelkerke‘s R2 |
0.12 |
|
|
0.04 |
|
|
0.21 |
|
|
Step 4 |
|
|
|
|
|
|
|
|
|
Physical activity T3 Ref: inactiveb |
|
|
|
0.81 (0.32–2.05) |
0.661 |
|
3.02 (0.53–17.31) |
0.216 |
|
Nagelkerke‘s R2 |
|
|
|
0.04 |
|
|
0.25 |
|
|
Step 5 |
|
|
|
|
|
|
|
|
|
Physical activity T4 Ref: inactiveb |
|
|
|
|
|
|
0.65 (0.09–4.59) |
0.667 |
|
Nagelkerke‘s R2 |
|
|
|
|
|
|
0.26 |
|
|
aControl variables: gender, education, intention T0, body mass index (BMI) T0, sick leave T0, physical exercise T0. bInactive: < 40 min physical exercise/week, active: > 40 min physical exercise/week. OR: odds ratio; CI: confidence interval. |
||||||||
|
Table III. Hierarchical regression results of physical exercise on subjective employability |
|||||||||||
|
|
T2, n = 340 |
|
T3, n = 296 |
|
T4, n = 142 |
||||||
|
ß |
p-value |
F |
|
ß |
p-value |
F |
|
ß |
p-value |
F |
|
|
Step 1 |
|
|
|
|
|
|
|
|
|
|
|
|
Control variablesa |
|
|
|
|
|
|
|
|
|
|
|
|
R2 |
0.33 |
|
|
|
0.29 |
|
|
|
0.15 |
|
|
|
∆R2 |
0.33 |
< 0.001 |
|
|
0.29 |
< 0.001 |
|
|
0.15 |
0.049 |
|
|
Step 2 |
|
|
|
|
|
|
|
|
|
|
|
|
Physical exercise T1b |
–0.10 |
0.035 |
–2.12 |
|
–0.18 |
0.002 |
–3.07 |
|
–0.06 |
0.608 |
–0.52 |
|
R2 |
0.34 |
|
|
|
0.32 |
|
|
|
0.15 |
|
|
|
∆R2 |
0.01 |
0.035 |
|
|
0.03 |
0.002 |
|
|
< 0.01 |
0.608 |
|
|
Step 3 |
|
|
|
|
|
|
|
|
|
|
|
|
Physical exercise T2b |
–0.16 |
0.001 |
–3.25 |
|
< 0.01 |
0.962 |
–0.05 |
|
–0.07 |
0.597 |
–0.53 |
|
R2 |
0.37 |
|
|
|
0.32 |
|
|
|
0.15 |
|
|
|
∆R2 |
0.02 |
0.001 |
|
|
< 0.01 |
0.962 |
|
|
< 0.01 |
0.597 |
|
|
Step 4 |
|
|
|
|
|
|
|
|
|
|
|
|
Physical exercise T3b |
|
|
|
|
–0.04 |
0.547 |
–0.60 |
|
< 0.01 |
0.995 |
–0.01 |
|
R2 |
|
|
|
|
0.33 |
|
|
|
0.15 |
|
|
|
∆R2 |
|
|
|
|
< 0.01 |
0.547 |
|
|
< 0.01 |
0.995 |
|
|
Step 5 |
|
|
|
|
|
|
|
|
|
|
|
|
Physical exercise T4b |
|
|
|
|
|
|
|
|
–0.16 |
0.218 |
–1.24 |
|
R2 |
|
|
|
|
|
|
|
|
0.41 |
|
|
|
∆R2 |
|
|
|
|
|
|
|
|
0.02 |
0.218 |
|
|
aControl variables: gender, education, intention T0, body mass index (BMI) T0, subjective employability T0, physical exercise T0. bInactive: < 40 min physical exercise/week, active: > 40 min physical exercise/week. |
|||||||||||
Our second aim was to test the relationship between physical exercise and subjective employability. Therefore, we ran hierarchical regressions with physical exercise predicting subjective employability at the 12-month (T2), 3-year (T3) and 8-year (T4) follow-ups. Results are shown in Table III. T1 physical exercise significantly predicted subjective employability 12 months (ß = –0.10, p = 0.035, R2 = 0.34) and 3 years (ß = –0.18, p = 0.002, R2 = 0.32) after baseline when controlling for sociodemographic variables, baseline subjective employability and baseline physical exercise. T1 physical exercise was not predictive of subjective employability at T4.
DISCUSSION
This study investigated the effect of physical exercise on sickness absence and subjective employability among former musculoskeletal rehabilitation patients and covered the durations of 6 months, 1 year, 3 years and 8 years. Long-term follow-ups over extended periods of time after discharge from rehabilitation are scarce in the current literature. Therefore, the aim of this study was to enhance understanding of the longitudinal outcomes in the domain of work ability.
The results showed that being physically active for at least 40 min a week 6 months after rehabilitation treatment reduces sick leave during the first follow-up year. This is in line with Kool et al. (6), who investigated the effect of physical exercise treatment on sickness absence in a meta-analysis with 22 randomized controlled trials. However, in our study there was no effect of physical exercise status on sick leave in the longer run (e.g. 3 and 8 years later). It is possible that the effects of physical exercise decline with increasing follow-up duration. This might be due to the fact that other factors might influence sickness absence, such as an individual’s profession, stressors in the work and social environment (23, 24) or non-changeable risk factors, such as age, gender and genetic predispositions for certain health problems (25). For future studies, a core set of confounding factors to describe participants in a standardized way would enable comparison of the effectiveness of physical exercise treatments for different working populations (6, 24).
We also found that being physically active for at least 40 min a week is positively associated with the subjective ability to work, in agreement with Arvidson et al.’s results (26), also in the medical rehabilitation setting. Those people who had become regularly active since rehabilitation treatment were more likely to feel able to work, not only in the short term, but also 3 years later, regardless of age, gender and baseline behaviour. It is well known that exercise not only improves muscle strength and endurance (27), but can also help people to cope with stress, anxiety, and depression (28), resulting in more work-related self-confidence. It is not only the individual worker who can benefit from long-term rehabilitation effects on work-related outcomes. Sustained employability and fewer sick days also provide benefits to the employer, such as lower presenteeism and absenteeism, reduced staff attrition and training costs by retaining experienced employees and maintaining improved productivity (29).
Potential limitations of the study should be discussed. The first drawback is the measurement of patient’s subjective employability. To measure subjective employability more elaborately, we recommend the use of the Work Ability Index by Ilmarinen (30) or the Readiness To Return To Work Scale by Franche et al. (31). This enables the researcher to consider individual and social factors that influence an individual’s return to work after an injury and has been shown to have validity among musculoskeletal patients (32). Furthermore, not only a measure of ability, but also of a desire to work would be of interest in future studies, as desire may be influenced by job resources, physical job demands, certain personality characteristics or income (33, 34). Of course, changes in the labour market and social insurance system might also have an impact.
Secondly, the measurement of our criterion variable physical exercise needs to be discussed. Our exercise data are based on self-report only and might be prone to bias. However, there is evidence for the reliability and validity of physical activity self-reports, such as the short version of the IPAQ (17). Future studies should consider more objective measures in addition to self-report, such as pedometers, which are already frequently applied in physical activity research (35). In addition, physical activity at work might also be worth measuring to be included as a covariate.
Thirdly, our study participants form a rather heterogeneous group, as we included patients with different MSD, such as back pain, disc disorders, joint condition and injuries, and did not control for their conditions. The findings of Hubertsson et al. (25) show that duration, as well as age and sex distribution concerning sick leave, vary considerably between different diagnostic codes within the group of MSDs. This underlines the importance of considering diagnosis in sick leave research. A physician rating or objective index of medical severity should therefore be included in future studies. Thus, the generalizability of our findings for a specific study group needs to be viewed with caution, and future studies should include larger sample sizes and frequent follow-up participation.
Finally, the study results are based on a longitudinal, but only observational, design. The cause-and-effect relationships found are based on theory or time lag and not on experimental manipulation. From the results of our study, we conclude that active people need less sick leave. However, the exact direction of the effect remains uncertain. We do not know whether people are less physically active because they are sick more often, or whether physical activity has health effects that result in less sick leave. Although longitudinal analyses reflect the relationship between being active and decreased sick leave, the extent to which these associations are caused by a within-worker or a between-worker relation remains unclear. Intervention studies are needed that specifically address the impact of physical exercise on work-related outcomes, including yearly follow-up measurement points.
In conclusion, identifying predictors for subjective employability and sickness absence is essential in order to plan optimum individual rehabilitation. Our finding that physical exercise for 40 min a week may be effective at reducing sick leave is important information, not only for the individual, but also from an economic perspective.
Because patients undergoing rehabilitation show high motivation to exercise when they end their rehabilitation treatment, but then face a decrease in motivation over time, they need to be supported in order to maintain their motivation. Aftercare programmes could be a promising tool to maintain rehabilitation outcomes and support people in changing their lifestyles by improving motivation, self-efficacy and planning strategies (36, 37).
ACKNOWLEDGEMENTS
This research was supported by Grant GK 429/2-03 from the German Research Foun-dation (DFG) and by the Wilhelm-Stiftung für Rehabilitationsforschung within the Donors’ Association for the Promotion of Humanities and Sciences in Germany. The manuscript was proofread by Mentorium GmbH.
REFERENCES
