Hidetoshi Shibuta, MS1, Takeru Abe, PhD2, Hidekazu Miyamoto, PhD1 and Akihito Hagihara, DMSc, MPH1,3
From the 1Kyushu University Graduate School of Medicine, Department of Health Services, Management and Policy, Maidashi, Higashi-ku, Fukuoka, 2Medical Center, Yokohama City University, Urafunecho, Minami-ku, Yokohama, Kanagawa and 3Kyushu University Graduate School of Medicine, Department of Health Care Administration and Management, Maidashi, Higashi-ku, Fukuoka, Japan
BACKGROUND: Patients’ functional abilities after hospital discharge are influenced by rehabilitation during their hospital stay and their use of community-based services after hospital discharge. This study examined the interaction between rehabilitation during hospital stay, the use of community-based rehabilitation and non-rehabilitation services and their influence on patients’ subsequent functional abilities.
METHODS: This cohort study included 509 inpatients who underwent rehabilitation between 2008 and 2011 in Japan. Participants were categorized into 2 groups based on their condition: stroke and other. Interaction effects between the change in Functional Independence Measure (FIM) and the use of community-based rehabilitation and non-rehabilitation services on patients’ subsequent functional abilities were estimated by sequential linear regression analyses in which the dependent variable was the FIM score 3 months after hospital discharge.
RESULTS: A significant interaction between the change in FIM and the use of community-based rehabilitation or non-rehabilitation services after hospital discharge was observed among stroke and other patients.
CONCLUSION: Rehabilitation during hospital stay and the use of community-based rehabilitation or non-rehabilitation services interacted to influence the subsequent functional abilities of patients discharged home. These findings may be useful for maintaining patients’ functional abilities after hospital discharge.
Key words: rehabilitation; service; interaction.
J Rehabil Med 2016; 48: 307–315
Correspondence address: Akihito Hagihara, Kyushu University Graduate School of Medicine, Department of Health Services, Management and Policy, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan. E-mail: hagihara@hsmp.med.kyushu-u.ac.jp
Accepted Nov 13, 2015; Epub ahead of print Feb 4, 2016
INTRODUCTION
It is important for rehabilitation patients to maintain a high level of functional abilities after discharge from hospital to home (1). Functional ability after hospital discharge can be influenced by various factors, including rehabilitation during the hospital stay, discharge destination, rehabilitation and use of community-based services after hospital discharge (2–7). Making use of the concept of the International Classification of Functioning, Disability and Health (ICF) by the World Health Organization (WHO), this paper summarizes findings concerning the functional ability of a rehabilitation patient who is discharged home (8). Specifically, the ICF framework consists of 2 parts: “Functioning and Disability” and “Contextual Factors”, in which “Functioning and Disability” includes “Body Functions and Structures” and “Activity and Participation”. “Contextual Factors” include “Environmental Factors” and “Personal Factors”. “Activities and Participation” is a key element of rehabilitation for patients who aim to be independent (9). A study related to “Activities and Participation” suggested that there was a beneficial effect on activities of daily living (ADL) when occupational therapists included instruction on functioning, the environment and education in elderly patients’ pre-discharge home visits (10). One study showed that elderly stroke patients had an increased chance of participation 3 months after discharge home, and that walking and acknowledgment of the stroke and depression were the best predictors of increased participation levels (11). Prior studies regarding “Functioning and Disability” and “Individual Factors” reported that there was a relationship between social capital and cause-specific mortality in stroke (12), and that the mortality of in-hospital patients undergoing rehabilitation increased at 80–180 days after discharge despite a reduction in the length of hospital stay (1). A recent study reported that there was no significant difference between discharged patients with and without rehabilitation therapy (13). As for the findings related to “Environmental Factors”, compared with patients who receive home rehabilitation, patients who utilize day hospital rehabilitation were at increased risk of re-hospitalization (14).
Thus far, very little is known about the interaction between “Functioning and Disability” and “Contextual Factors” in the ICF. In other words, very little is known about how rehabilitation during a hospital stay interacts with the use of community-based services after hospital discharge, or how this interaction influences patients’ functional abilities after hospital discharge. We hypothesized that there would be interaction effects between rehabilitation in the hospital and the use of community-based services after hospital discharge on patients’ subsequent functional abilities. Therefore, using data from inpatients transferred from other acute hospitals to a rehabilitation unit, we examined the interaction effects between rehabilitation during the hospital stay and the use of community-based rehabilitation or non-rehabilitation services after patients’ hospital discharge home on subsequent daily activity by disease type (i.e. stroke and others). Because the purpose of this study was to evaluate interaction effects between rehabilitation during hospital stay and the use of rehabilitation or non-rehabilitation services after hospital discharge on patients’ functional ability at 3 months after hospital discharge, the findings of this study will be useful for determining the type of community-based services that are necessary to maintain a patient’s functional ability after discharge home.
MATERIAL AND METHODS
Subjects
The subjects were consecutive patients who underwent rehabilitation from 1 April 2008 to 30 November 2011, in the recovery phase rehabilitation ward at D hospital in Fukuoka City, Japan, and who were later discharged home. Because patients discharged to a facility cannot utilize community-based services in Japan, the subjects of this study were limited to patients discharged home.
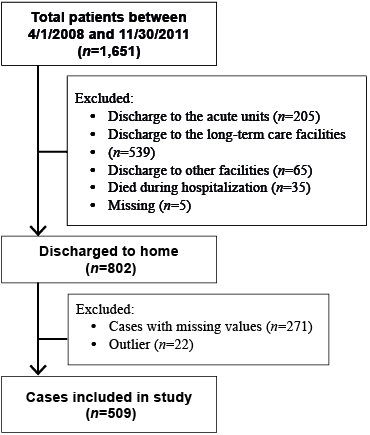
A total of 1,651 patients were admitted to the rehabilitation wards of D hospital and completed the rehabilitation programme during the study period (1 April 2008 to 30 November 2011) (Fig. 1). Patients from D hospital who were discharged to the acute unit (n = 205), to long-term care facilities (n = 539) and to other facilities (n = 65), as well as those who died during hospitalization (n = 35) and who were lost-to-follow after discharge (n = 5), were excluded. We attempted to contact patients discharged home (n = 802) 3 months after hospital discharge by therapists, although we were unable to contact all of the patients, as some of them had moved (n = 271). A total of 271 patients had missing data, and 22 patients were outliers with respect to the standardized residuals (rather than 3 SD); therefore, the remaining patients with complete data were used in analysis (n = 509). Based on their primary disease, patients were categorized into 2 groups: “stroke” and “other disease.” The stroke group included patients with cerebral infarction, subarachnoid haemorrhage, subdural haemorrhage, or intracranial haemorrhage. The other disease group included patients with muscle injury, femoral fracture, vertebral compression fracture, pelvic fracture, neuromuscular disease, cardiac disease, gastrointestinal disease, rheumatoid arthritis, respiratory disease, or other conditions, which were typically associated with mechanical or prescribed immobilization, severe pain, and/or an altered level of consciousness (15). The protocol of this study was approved by the ethics committee of D hospital in 2008.
Fig. 1. Study participant selection.
Study variables
The following information was ascertained during each patient’s stay in the rehabilitation ward: personal attributes, such as age, gender, tax-exemption status, and dementia; the key person at hospital discharge; and the Functional Independence Measure (FIM) score at hospital discharge. The tax-exemption status category was used to evaluate whether a patient’s household was tax-exempt and included the responses “yes” and “no.” The “yes” response means that that patient has a right to pay no more than 15,000 Japanese-yen, which was equivalent to 140 US dollars in October 2014, for the use of long-term care services. The key person at hospital discharge had 2 categories: “spouse” and “other.” Intensity of therapy was calculated as the total hours of therapy divided by the length of hospital stay (LOS) at the rehabilitation unit of D hospital in days (16, 17). The total therapy was the total amount of therapy provided by physiotherapists, occupational therapists, and speech therapists. The FIM score at the time of hospital discharge was measured by the physical and occupational therapists that were assigned to take care of the patient and was used to assess functional independence (18).
At the time of hospital discharge, the use of community-based rehabilitation and non-rehabilitation services and FIM change% were evaluated from medical charts. There are 6 types of community-based services available to patients discharged to their own homes: home-visit long-term care, home-visit nursing, home-visit rehabilitation, outpatient day long-term care, day service, and short stay (19). Home-visit long-term care includes assistance at home from a home-helper in bathing, toilet needs, eating, cooking, and cleaning. Home-visit nursing includes medical care and assistance from nurses at home following the physicians’ orders when the patients are not capable of making hospital visits. Home visit rehabilitation service includes rehabilitation services at home with the assistance of physiotherapists, occupational therapists, and speech therapists per the physicians’ orders. Outpatient day long-term care includes day-care assistance in day-to-day activities, such as eating, and rehabilitation services to sustain or improve vital functions that are provided at health service facilities for elderly people and at medical institutions. Day service includes assistance at day service centres in day-to-day activities, such as eating and bathing, and in the sustenance and improvement of functioning. Short stay services include assistance in day-to-day activities and functional training at welfare facilities. We counted the number of services that each patient used in the following 2 groups: the rehabilitation service use group (i.e. home-visit rehabilitation, and outpatient day long-term care) and the non-rehabilitation service use group (i.e. home-visit long-term care, home-visit nursing, day service, and short stay). Thus, in the rehabilitation service use group, the score takes on 1 of the following 3 values; “2”, when using home-visit rehabilitation and outpatient day long-term care; “1”, when 1 of the 2 services is used; and “0”, when there is no service use. In the non-rehabilitation service use group, similar to the rehabilitation service use group, the score ranged between 0 and 4 depending on the number of services used. Therefore, the subjects of this study included patients who received both rehabilitation services and/or non-rehabilitation services.
To evaluate the effectiveness of rehabilitation during the hospital stay, we calculated FIM change% based on FIM effectiveness. FIM effectiveness is the difference between FIM scores at the time of hospital admission and at the time of hospital discharge (20, 21). It is quite difficult to increase the FIM score when the score at hospital admission is high, whereas it is relatively easy to increase the FIM score when the score at hospital admission is low. When evaluating the effectiveness of rehabilitation during the hospital stay, FIM effectiveness simply calculates the difference between FIM scores at 2 time-points and does not consider whether the baseline FIM score (i.e. the FIM score at hospital admission) is high or low. Thus, to remedy this problem and to evaluate the effectiveness of rehabilitation during the hospital stay more adequately, we used FIM change% based on FIM effectiveness (20–22). The FIM change% was calculated by dividing the difference between the FIM scores at the time of hospital admission and hospital discharge by the FIM target score (i.e. the FIM maximum score: 126) minus the FIM score at the time of hospital admission (23–25).
Statistical procedures
Sequential regression analyses were performed for each patient group (26). In the analyses, following the models suggested by Harrell (27), models in which the dependent variable was the FIM score at 3 months after hospital discharge (rather than the difference between the FIM scores at the time of hospital discharge and at 3 months after hospital discharge) were used. In the last step, an interaction term between rehabilitation during hospital discharge and the use of community-based services was entered into a regression model. In each step of the regression analyses, the variance inflation factor (VIF) was calculated to check for multicollinearity. To test the assumptions of the multivariate analysis, we checked the normality and homoscedasticity of the residuals using scatter plots and a histogram of the residuals. In addition, we used 3 standardized residuals to detect outliers and defined cases that had greater than 3 standardized residuals as outliers, and these cases were excluded from the multivariate analysis. To accurately evaluate the effect of an interaction term between 2 variables, centring was performed before sequential regression analyses (28). Specifically, before constructing the interaction term, we centred FIM change% and the use of community-based services by subtracting the mean score of the sample from each individual’s score (28). To determine the significance of each interaction, post hoc analyses were conducted. For the final model, to confirm the validity of the regression analyses, regression diagnostics, including checking the residuals, multicollinearity, outliers, and influential observations, were performed.
For comparisons between the 2 disease groups, based on whether the patient’s condition was caused by damage to the central nervous system, we used the χ2 test and Student’s t-test. These analyses were performed using SPSSx Version 19 software, Chicago, IL, USA, and p-values < 0.05 were considered to indicate statistical significance.
RESULTS
Table I provides a description of the study variables in the 2 patient groups. There were 113 and 396 patients in the stroke and other groups, respectively. There were no significant differences between the groups with respect to the means or proportions of the study variables.
|
Table I. Patients’ characteristics categorized by type of disease |
||||
|
|
Stroke patients (n = 113) |
Other disease patients (n = 396) |
p-value |
|
|
Age, years, mean (SD) |
80 (11) |
78 (13) |
0.172 |
|
|
Gender, female, n (%) |
72 (64) |
277 (70) |
0.208 |
|
|
Tax-exemption status, yes, n (%) |
26 (23) |
126 (32) |
0.071 |
|
|
Dementia, yes, n (%) |
24 (21) |
106 (27) |
0.235 |
|
|
Key person at hospital discharge, spouse, n (%) |
34 (30) |
127 (32) |
0.689 |
|
|
Intensity of therapy, mean (SD) |
1.6 (3.6) |
1.6 (2.0) |
0.962 |
|
|
Rehabilitation services use |
|
|
|
|
|
0 services |
78 (69) |
252 (64) |
0.290 |
|
|
1 service |
33 (29) |
137 (34) |
0.284 |
|
|
2 services |
2 (2) |
7 (2) |
0.999 |
|
|
Non-rehabilitation services use |
|
|
|
|
|
0 services |
64 (57) |
254 (64) |
0.146 |
|
|
1 service |
35 (31) |
106 (27) |
0.378 |
|
|
2 services |
12 (10) |
33 (8) |
0.450 |
|
|
3 services |
2 (2) |
3 (1) |
0.336 |
|
|
4 services |
0 (0) |
0 (0) |
– |
|
|
FIM score at hospital admission, mean (SD) |
96 (22) |
95 (23) |
0.635 |
|
|
FIM score at hospital discharge, mean (SD) |
107 (18) |
106 (20) |
0.591 |
|
|
FIM change%a, mean (SD) |
42 (32) |
43 (32) |
0.925 |
|
|
FIM score at 3 months after hospital discharge, mean (SD) |
105 (19) |
104 (22) |
0.551 |
|
|
aFIM change % = |
(the FIM score at hospital discharge)–(the FIM score at hospital admission) |
× 100 |
||
|
(the FIM maximum score (i.e., 126))–(the FIM score at hospital admission) |
||||
|
Student’s t-test for continuous variables and χ2 test for categorical variables. FIM: Functional Independence Measure. |
||||
Table II illustrates the FIM score at 3 months after hospital discharge and FIM change% in the rehabilitation or non-rehabilitation service use groups. There was a significant difference in the number of rehabilitation or non-rehabilitation service use groups, which implies that the amount of services used would be decided by the available services in accordance with the functional abilities of the patients in the long-term care insurance system.
|
Table II. Functional Independence Measure (FIM) change% and the FIM score at 3 months after hospital discharge in the rehabilitation and non-rehabilitation services use groups |
|||
|
|
FIM change%a Mean (SD) |
FIM score 3 months after hospital discharge Mean (SD) |
|
|
Rehabilitation services use |
|||
|
0 services (n = 330) |
45 (32) |
106 (22) |
|
|
1 service (n = 170) |
36 (28) |
101 (20) |
|
|
2 services (n = 9) |
33 (23) |
97 (13) |
|
|
|
p = 0.036 |
p < 0.001 |
|
|
Non-rehabilitation services use |
|||
|
0 services (n = 318) |
49 (33) |
112 (16) |
|
|
1 service (n = 141) |
29 (27) |
94 (21) |
|
|
2 services (n = 45) |
29 (23) |
84 (26) |
|
|
3 services (n = 5) |
29 (30) |
72 (38) |
|
|
4 services (n = 0) |
– |
– |
|
|
|
p < 0.001 |
p < 0.001 |
|
|
aFIM change % = |
(the FIM score at hospital discharge)– (the FIM score at hospital admission) |
× 100 |
|
|
(the FIM maximum score (i.e., 126))– (the FIM score at hospital admission) |
|||
|
Kruskal-Wallis test. SD: standard deviation. |
|||

Tables III and IV illustrate the results of the sequential regression analyses in the stroke patient group. In the analysis focusing on the interaction between FIM change% and the use of rehabilitation services after hospital discharge (Table III), the independent variables related to the patient attributes were included in step 1 of the analysis and explained a significant portion of the variance in the equation (p < 0.001). In step 2 of the analysis, FIM change% was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). In step 3 of the analysis, the use of rehabilitation services was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). However, the use of rehabilitation services was not related to the FIM score at 3 months after hospital discharge (p = 0.072). In step 4 of the analysis, an interaction term between FIM change% and the use of rehabilitation services was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). The interaction between the 2 variables was related to an increase in the FIM score at 3 months after hospital discharge (B = 12.094; p = 0.003). In the analysis focusing on the interaction between FIM change% and the use of non-rehabilitation services after hospital discharge (Table IV), independent variables were included in step 1 of the analysis and explained a significant portion of the variance in the equation (p < 0.001). In step 2 of the analysis, FIM change% was entered, and in step 3, the use of non-rehabilitation services was entered into a regression model and both were shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001 and p < 0.001, respectively). In step 4 of the analysis, an interaction term between FIM change% and the use of non-rehabilitation services was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). However, the interaction between the 2 variables was not related to the FIM score at 3 months after hospital discharge (B = 5.247; p = 0.075).
|
Table III. Sequential regression analysis of factors related to the Functional Independence Measure (FIM) score at 3 months after hospital discharge among the stroke patients: the interaction between FIM change% and the use of rehabilitation services (n = 113) |
|||||
|
Variables |
B |
p-value |
R2 change |
p-value |
|
|
Step 1: Patients’ characteristics |
|
|
0.807 |
< 0.001 |
|
|
|
Age |
0.039 |
0.604 |
|
|
|
|
Gender, female |
2.651 |
0.142 |
|
|
|
|
Tax-exemption, yes |
–2.922 |
0.139 |
|
|
|
|
Dementia, yes |
–11.225 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.009 |
0.592 |
|
|
|
|
Intensity of therapy |
1.163 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–5.155 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.622 |
< 0.001 |
|
|
|
Step 2: FIM change% |
|
|
0.096 |
< 0.001 |
|
|
|
Age |
0.021 |
0.700 |
|
|
|
|
Gender, female |
0.695 |
0.592 |
|
|
|
|
Tax-exemption, yes |
–1.983 |
0.161 |
|
|
|
|
Dementia, yes |
–6.642 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.837 |
0.534 |
|
|
|
|
Intensity of therapy |
0.856 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–3.957 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.598 |
< 0.001 |
|
|
|
|
FIM change% |
19.529 |
< 0.001 |
|
|
|
Step 3: Rehabilitation services use |
|
|
0.003 |
< 0.001 |
|
|
|
Age |
0.006 |
0.917 |
|
|
|
|
Gender, female |
0.527 |
0.682 |
|
|
|
|
Tax-exemption, yes |
–2.344 |
0.098 |
|
|
|
|
Dementia, yes |
–6.044 |
0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.565 |
0.673 |
|
|
|
|
Intensity of therapy |
0.898 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–3.491 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.618 |
< 0.001 |
|
|
|
|
FIM change% |
20.042 |
<0.001 |
|
|
|
|
Rehabilitation services use |
2.336 |
0.072 |
|
|
|
Step 4: Interaction term |
|
|
0.008 |
< 0.001 |
|
|
|
Age |
0.011 |
0.831 |
|
|
|
|
Gender, female |
0.216 |
0.862 |
|
|
|
|
Tax-exemption, yes |
–1.874 |
0.171 |
|
|
|
|
Dementia, yes |
–5.359 |
0.002 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.296 |
0.819 |
|
|
|
|
Intensity of therapy |
0.975 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–3.468 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.648 |
< 0.001 |
|
|
|
|
FIM change% |
21.149 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
3.457 |
0.009 |
|
|
|
|
Interaction term Rehabilitation services use × FIM change% |
12.094 |
0.003 |
|
|
|
|
R2 total |
|
|
0.913 |
< 0.001 |
|
|
Adjusted R2 |
|
|
0.904 |
|
|
Bold texts represent variables entered into each step of the sequential regression model. |
|||||
|
Table IV. Sequential regression analysis of factors related to the Functional Independence Measure (FIM) score at 3 months after hospital discharge among the stroke patients: the interaction between FIM change% and the use of non-rehabilitation services (n = 113) |
|||||
|
Variables |
B |
p-value |
R2 Change |
p-value |
|
|
Step 1: Patients’ characteristics |
|
|
0.774 |
< 0.001 |
|
|
|
Age |
0.033 |
0.688 |
|
|
|
|
Gender, female |
2.855 |
0.144 |
|
|
|
|
Tax-exemption, yes |
–3.083 |
0.153 |
|
|
|
|
Dementia, yes |
–11.254 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
0.395 |
0.845 |
|
|
|
|
Intensity of therapy |
1.193 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
2.480 |
0.188 |
|
|
|
|
FIM score at hospital admission |
0.690 |
< 0.001 |
|
|
|
Step 2: FIM change% |
|
|
0.116 |
< 0.001 |
|
|
|
Age |
0.001 |
0.984 |
|
|
|
|
Gender, female |
0.532 |
0.699 |
|
|
|
|
Tax-exemption, yes |
–2.364 |
0.118 |
|
|
|
|
Dementia, yes |
–5.770 |
0.002 |
|
|
|
|
Key person at hospital discharge, spouse |
0.366 |
0.795 |
|
|
|
|
Intensity of therapy |
0.893 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
3.851 |
0.004 |
|
|
|
|
FIM score at hospital admission |
0.661 |
< 0.001 |
|
|
|
|
FIM change% |
21.415 |
< 0.001 |
|
|
|
Step 3: Non-rehabilitation services use |
|
|
0.015 |
< 0.001 |
|
|
|
Age |
0.006 |
0.917 |
|
|
|
|
Gender, female |
0.527 |
0.682 |
|
|
|
|
Tax-exemption, yes |
–2.344 |
0.098 |
|
|
|
|
Dementia, yes |
–6.044 |
0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.565 |
0.673 |
|
|
|
|
Intensity of therapy |
0.898 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
2.336 |
0.072 |
|
|
|
|
FIM score at hospital admission |
0.618 |
< 0.001 |
|
|
|
|
FIM change% |
20.042 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–3.491 |
< 0.001 |
|
|
|
Step 4: Interaction term |
|
|
0.003 |
< 0.001 |
|
|
|
Age |
0.018 |
0.730 |
|
|
|
|
Gender, female |
0.273 |
0.831 |
|
|
|
|
Tax-exemption, yes |
–2.090 |
0.137 |
|
|
|
|
Dementia, yes |
–5.796 |
0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.118 |
0.930 |
|
|
|
|
Intensity of therapy |
0.823 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
1.760 |
0.182 |
|
|
|
|
FIM score at hospital admission |
0.601 |
< 0.001 |
|
|
|
|
FIM change % |
21.147 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–3.483 |
< 0.001 |
|
|
|
|
Interaction term Non-rehabilitation services use × FIM change% |
5.247 |
0.075 |
|
|
|
|
R2 total |
|
|
0.909 |
< 0.001 |
|
|
Adjusted R2 |
|
|
0.899 |
|
|
Bold texts represent variables entered into each step of the sequential regression model. |
|||||
Figs 2 and 3 display the relationships between the use of rehabilitation or non-rehabilitation services and the FIM score at 3 months after hospital discharge, as mediated by FIM change% among stroke patients. The slopes of the 2 lines in Figs 2 and 3 were calculated by using the partial regression coefficients of the interaction term, FIM change%, and the use of rehabilitation or non-rehabilitation services (28). As shown in Fig. 2, the slope for the higher FIM change% (mean +1 SD) increases significantly when the level of rehabilitation services use moved from the mean –1 SD to +1 SD (p < 0.001), while the slope for the lower FIM change% (mean – 1 SD) remained at the same level when the levels of rehabilitation services increased from the mean –1 SD to +1 SD (p = 0.74). As shown in Fig. 3, the slope for the higher FIM change% (mean +1 SD) remained at the same level irrespective of the level of non-rehabilitation services use (p = 0.35), while the slope for the lower FIM change% (mean – 1 SD) decreased when the level of non-rehabilitation services use increased from the mean –1 SD to +1 SD (p < 0.01).
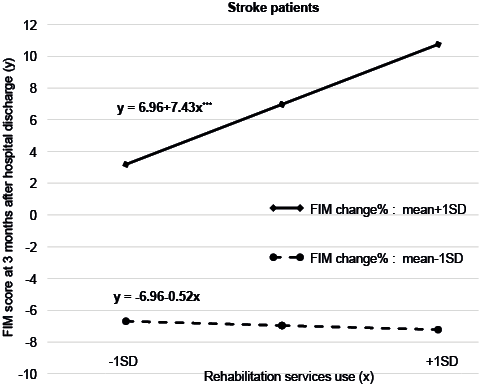
Fig. 2. Effect of interaction between rehabilitation potential and use of community-based rehabilitation services after hospital discharge on the Functional Independence Measure (FIM) scores at 3 months after hospital discharge among stroke patients discharged home. The slopes of the 2 lines are significantly different (p = 0.03). ***p < 0.001.
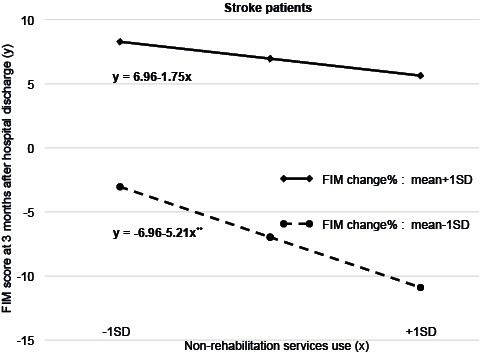
Fig. 3. Effect of interaction between rehabilitation potential and use of community-based non-rehabilitation services after hospital discharge on the Functional Independence Measure (FIM) scores at 3 months after hospital discharge among stroke patients who were discharged home. The slopes of the 2 lines are not significantly different (p = 0.08). **p < 0.01.
Tables V and VI show the results of the sequential regression analyses in the other patient group. In the analysis focusing on the interaction between FIM change% and the use of rehabilitation services after hospital discharge (Table V), which was step 4 of the analysis, an interaction term between FIM change% and the use of rehabilitation services was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). The interaction between the 2 variables was related to an increase in the FIM score at 3 months after hospital discharge (B = 12.557; p < 0.001). In the analysis focusing on the interaction between FIM change% and the use of non-rehabilitation services after hospital discharge among other disease patients (Table VI), which was step 4 of the analysis, an interaction term between FIM change% and the use of non-rehabilitation services was entered into a regression model and was shown to contribute to a significant increase in explained variance of the FIM score (p < 0.001). Specifically, the interaction between the 2 variables was related to the FIM score at 3 months after hospital discharge (B = 15.268; p < 0.001).
|
Table V. Sequential regression analysis of factors related to the Functional Independence Measure (FIM) score 3 months after hospital discharge among the other disease patients: the interaction between FIM change% and the use of rehabilitation services (n = 396) |
|||||
|
Variables |
B |
p-value |
R2 Change |
p-value |
|
|
Step 1: Patients’ characteristics |
|
|
0.789 |
< 0.001 |
|
|
|
Age |
0.105 |
0.011 |
|
|
|
|
Gender, female |
1.206 |
0.308 |
|
|
|
|
Tax-exemption, yes |
–1.498 |
0.176 |
|
|
|
|
Dementia, yes |
–7.564 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.770 |
0.501 |
|
|
|
|
Intensity of therapy |
–0.207 |
0.414 |
|
|
|
|
Non-rehabilitation services use |
–4.631 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.673 |
< 0.001 |
|
|
|
Step 2: FIM change% |
|
|
0.116 |
< 0.001 |
|
|
|
Age |
0.011 |
0.698 |
|
|
|
|
Gender, female |
0.980 |
0.217 |
|
|
|
|
Tax-exemption, yes |
–0.997 |
0.180 |
|
|
|
|
Dementia, yes |
–3.064 |
0.002 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.884 |
0.015 |
|
|
|
|
Intensity of therapy |
–0.064 |
0.707 |
|
|
|
|
Non-rehabilitation services use |
–2.758 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.665 |
< 0.001 |
|
|
|
|
FIM change% |
25.274 |
< 0.001 |
|
|
|
Step 3: Rehabilitation services use |
|
|
0.005 |
< 0.001 |
|
|
|
Age |
0.003 |
0.913 |
|
|
|
|
Gender, female |
1.158 |
0.135 |
|
|
|
|
Tax-exemption, yes |
–1.215 |
0.095 |
|
|
|
|
Dementia, yes |
–2.777 |
0.004 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.975 |
0.009 |
|
|
|
|
Intensity of therapy |
–0.161 |
0.337 |
|
|
|
|
Non-rehabilitation services use |
–2.013 |
0.001 |
|
|
|
|
FIM score at hospital admission |
0.689 |
< 0.001 |
|
|
|
|
FIM change% |
26.152 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
3.186 |
< 0.001 |
|
|
|
Step 4: Interaction term |
|
|
0.007 |
< 0.001 |
|
|
|
Age |
–0.001 |
0.963 |
|
|
|
|
Gender, female |
0.805 |
0.282 |
|
|
|
|
Tax-exemption, yes |
–0.912 |
0.193 |
|
|
|
|
Dementia, yes |
–3.013 |
0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.322 |
0.071 |
|
|
|
|
Intensity of therapy |
–0.154 |
0.340 |
|
|
|
|
Non-rehabilitation services use |
–2.034 |
0.001 |
|
|
|
|
FIM score at hospital admission |
0.695 |
< 0.001 |
|
|
|
|
FIM change% |
27.079 |
< 0.001 |
|
|
|
|
Rehabilitation services use |
3.561 |
< 0.001 |
|
|
|
|
Interaction term Rehabilitation services use × FIM change% |
12.557 |
< 0.001 |
|
|
|
|
R2 total |
|
|
0.917 |
< 0.001 |
|
|
Adjusted R2 |
|
|
0.915 |
|
|
Bold texts represent variables entered into each step of the sequential regression model. |
|||||
|
Table VI. Sequential regression analysis of factors related to the FIM score 3 months after hospital discharge among the other disease patients: the interaction between FIM change% and the use of non-rehabilitation services (n = 396) |
|||||
|
Variables |
B |
p-value |
R2 change |
p-value |
|
|
Step 1: Patients’ characteristics |
|
|
0.776 |
< 0.001 |
|
|
|
Age |
0.110 |
0.010 |
|
|
|
|
Gender, female |
1.182 |
0.333 |
|
|
|
|
Tax-exemption, yes |
–1.800 |
0.116 |
|
|
|
|
Dementia, yes |
–9.556 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
0.053 |
0.964 |
|
|
|
|
Intensity of therapy |
–0.252 |
0.339 |
|
|
|
|
Rehabilitation services use |
1.772 |
0.097 |
|
|
|
|
FIM score at hospital admission |
0.716 |
< 0.001 |
|
|
|
Step 2: FIM change% |
|
|
0.132 |
< 0.001 |
|
|
|
Age |
0.003 |
0.914 |
|
|
|
|
Gender, female |
1.134 |
0.149 |
|
|
|
|
Tax-exemption, yes |
–1.322 |
0.073 |
|
|
|
|
Dementia, yes |
–3.513 |
< 0.001 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.651 |
0.029 |
|
|
|
|
Intensity of therapy |
–0.172 |
0.310 |
|
|
|
|
Rehabilitation services use |
3.824 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.706 |
< 0.001 |
|
|
|
|
FIM change% |
26.847 |
< 0.001 |
|
|
|
Step 3: Non-rehabilitation services use |
|
|
0.003 |
< 0.001 |
|
|
|
Age |
0.003 |
0.913 |
|
|
|
|
Gender, female |
1.158 |
0.135 |
|
|
|
|
Tax-exemption, yes |
–1.215 |
0.095 |
|
|
|
|
Dementia, yes |
–2.777 |
0.004 |
|
|
|
|
Key person at hospital discharge, spouse |
–1.975 |
0.009 |
|
|
|
|
Intensity of therapy |
–0.161 |
0.337 |
|
|
|
|
Rehabilitation services use |
3.186 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.689 |
< 0.001 |
|
|
|
|
FIM change% |
26.152 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–2.013 |
0.001 |
|
|
|
Step 4: Interaction term |
|
|
0.014 |
< 0.001 |
|
|
|
Age |
–0.008 |
0.747 |
|
|
|
|
Gender, female |
1.396 |
0.050 |
|
|
|
|
Tax-exemption, yes |
–0.849 |
0.204 |
|
|
|
|
Dementia, yes |
–2.040 |
0.022 |
|
|
|
|
Key person at hospital discharge, spouse |
–0.978 |
0.162 |
|
|
|
|
Intensity of therapy |
–0.138 |
0.368 |
|
|
|
|
Rehabilitation services use |
2.602 |
< 0.001 |
|
|
|
|
FIM score at hospital admission |
0.683 |
< 0.001 |
|
|
|
|
FIM change% |
28.510 |
< 0.001 |
|
|
|
|
Non-rehabilitation services use |
–0.573 |
0.325 |
|
|
|
|
Interaction term Non-rehabilitation services use × FIM change% |
15.268 |
< 0.001 |
|
|
|
|
R2 total |
|
|
0.925 |
< 0.001 |
|
|
Adjusted R2 |
|
|
0.923 |
|
|
Bold texts represent variables entered into each step of the sequential regression model. |
|||||
Figs 4 and 5 illustrate the relationship between the use of rehabilitation or non-rehabilitation services and the FIM score at 3 months after hospital discharge as mediated by FIM change% among other disease patients. As a sensitivity analysis, the difference in the FIM was entered into 4 regression models instead of FIM change%. None of the interactions between the 2 variables were related to the FIM score at 3 months after hospital discharge. This finding implies that FIM change% reflected the effectiveness of rehabilitation more accurately than did the simple amount of change, such as the difference in FIM.
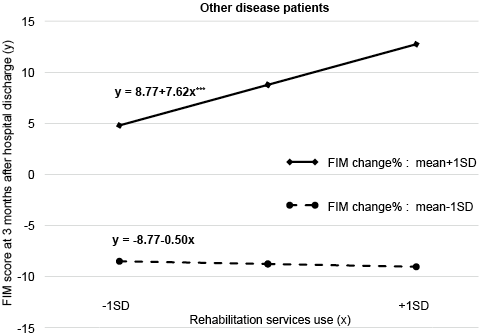
Fig. 4. Effect of interaction between rehabilitation potential and use of community-based rehabilitation services after hospital discharge on the Functional Independence Measure (FIM) scores at 3 months after hospital discharge among other disease patients discharged home. The slopes of the 2 lines are significantly different (p < 0.001). ***p < 0.001.
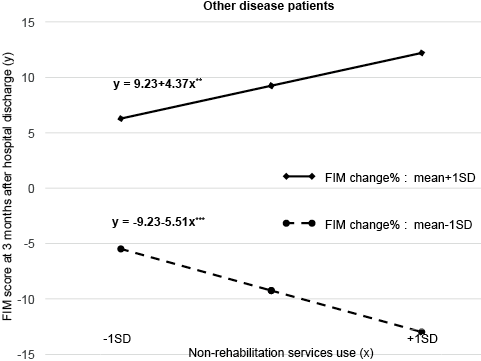
Fig. 5. Effect of interaction between rehabilitation potential and use of community-based non-rehabilitation services after hospital discharge on Functional Independence Measure (FIM) scores at 3 months after hospital discharge among other disease patients discharged home. The slopes of the 2 lines are significantly different (p < 0.001). **p < 0.01, ***p < 0.001.
DISCUSSION
There were several notable findings in this study. First, although community-based rehabilitation services were effective in improving or maintaining the functional ability of a stroke patient who is discharged home, community-based non-rehabilitation services were not. Secondly, although community-based rehabilitation services were effective in improving or maintaining the functional ability of other disease patients who were discharged home, the efficacy of community-based non-rehabilitation services was limited to those who had effective rehabilitation during their hospital stay.
Effectiveness of rehabilitation, limit to the total amount of services
Community-based rehabilitation services are provided by a rehabilitation therapist, while non-rehabilitation services are provided by caregivers other than a rehabilitation therapist. A rehabilitation therapist can evaluate a patient’s rehabilitation needs individually and deliver necessary interventions to the patient in the rehabilitation service. A British study reported that patients whose rehabilitation needs were unmet were more dependent and less integrated 1 year after hospital discharge than those whose rehabilitation needs were met (29). Thus, in the present study, the subsequent FIM score of stroke patients and other disease patients whose FIM change% were higher became larger when they received more community-based rehabilitation than when they received less community-based rehabilitation. Among stroke patients and other disease patients whose FIM change% were lower, the FIM score 3 months after hospital discharge remained at the same level irrespective of the quantity of community-based rehabilitation they received. In addition, among stroke patients and other disease patients who received both rehabilitation services and non-rehabilitation services, mean FIM score at 3 months after hospital discharge decreased from that at hospital discharge. Only one patient received 2 types of rehabilitation services, and her subsequent FIM score remained at the level of hospital discharge. Community-based non-rehabilitation services were effective in improving functional ability at 3 months after hospital discharge for other disease patients whose FIM change% were higher, but not for stroke patients whose FIM change% were higher. It is notable that stroke patients had damage to the central nervous system, while other disease patients had no such damage. In addition, non-rehabilitation services did not meet the needs of stroke patients. Among stroke patients and other disease patients whose FIM change% were lower, the FIM scores 3 months after hospital discharge decreased as the quantity of their community-based non-rehabilitation increased. Under long-term care insurance, there is a limit to the total amount of community-based services a patient can use. It is probable that the quantity of that community-based rehabilitation service that they receive might shrink when the quantity of non-rehabilitation use increases. Concomitantly, among the other disease patient group, the mean rehabilitation use scores were 0.43 (SD 0.54) in the lower non-rehabilitation service use group and 0.30 (SD 0.47) in the higher non-rehabilitation service use group. Among stroke patients, the mean rehabilitation use scores were 0.42 (SD 0.56) in the lower non-rehabilitation service use group and 0.20 (SD 0.41) in the higher non-rehabilitation service use group. Under the long-term care insurance system in Japan, the total amount of usable services is limited by the functional abilities of the patients and by the fact that the price of rehabilitation services is higher than that of non-rehabilitation services. The decreased use of rehabilitation services among the higher non-rehabilitation service users might be attributable to this finding.
Practical implications
Maintaining functional ability after completing a rehabilitation programme during the hospital stay is extremely important for patient quality of life and for containing healthcare costs. Although Japanese patients discharged home have been reported to show a gradual decline in daily living activities over time (30), factors that support the maintenance of the functional ability of such patients have not been reported. Currently, there is no transition-support programme for rehabilitation patients who are discharged home in which a patient would be allowed to go back and forth between home and a facility to gradually adjust to the home environment without full recovery (31–33). Patients discharged home tend to seek healthcare services based on price and convenience (e.g., distance and driving time), rather than with regard to necessity (34). Most previous studies have examined the associations between patient attributes and the type of discharge destination after hospital rehabilitation (2–4, 16, 17, 35–37). Although some of these factors are related to the functional abilities of patients, the interactions between them have not been elucidated.
This is the first study to demonstrate that rehabilitation during hospital stay and the use of community-based rehabilitation or non-rehabilitation services interact to influence functional ability at 3 months after hospital discharge in stroke and other patients. Thus, the findings of this study are theoretically and practically important. The practical implications of the present findings are straightforward: (i) community-based rehabilitation services are recommended to maintain or improve the functional ability of patients who are discharged home from a rehabilitation unit; (ii) community-based non-rehabilitation services are recommended only to non-stroke patients who have received effective rehabilitation during their hospital stay and are discharged home; (iii) social capital has been shown to be related to mortality due to stroke (12). Thus, according to the present study, stroke patients might benefit from outpatient day long-term care that can provide rehabilitation services while simultaneously strengthening community support.
Study limitations
There are several caveats and limitations to the present study. First, the medical care delivery system unique to Japan might have influenced the findings. Specifically, it is probable that interaction effects between rehabilitation and the use of community-based services after hospital discharge and the subsequent functional abilities of patients discharged to their own homes may have been influenced by the Japanese medical care delivery system. Every Japanese citizen is insured under the health insurance system, and elderly citizens can utilize nursing care under the long-term care insurance system. Thus, caution is warranted with regard to the external validity of this study’s findings. Secondly, the data were collected at a single hospital. Because factors other than those used as explanatory variables in this study might also influence the dependent variable, additional studies including more variables in other settings with different healthcare delivery systems are necessary. Thirdly, the use of community-based services between hospital discharge and 3 months after hospital discharge was surveyed at the time of hospital discharge. The content of community-based services use might have changed during the 3 months of the study period. However, because the study period was short, we believe that any changes in the content of social services use might be negligible.
Conclusion
In conclusion, this study demonstrated that rehabilitation during a hospital stay and the use of community-based rehabilitation or non-rehabilitation services interacted to influence the functional abilities of patients who were discharged home. The present findings may be useful for maintaining patients’ functional abilities after hospital discharge and could be utilized in a future transition-support programme for rehabilitation patients who are discharged home.
REFERENCES
