James W. Middleton, PhD1, Deborah Johnston, MBMSc1, Gregory Murphy, PhD2, Kumaran Ramakrishnan, MD1, Nerida Savage, Grad Dip Hlth Sc3, Rachel Harper, B Occ Th3, Jacquelyn Compton, B App Sci (Occ Thy)3 and Ian D. Cameron, PhD1
From the 1John Walsh Centre for Rehabilitation Research, Sydney Medical School Northern, The University of Sydney, Kolling Institute, Royal North Shore Hospital, St Leonards, 2Latrobe University, Melbourne and 3CRS Australia, Department of Human Services, Australia
OBJECTIVES: To describe a novel early vocational rehabilitation programme (In-Voc) for inpatients with spinal cord injury and to report early vocational outcomes.
DESIGN: Observational longitudinal cohort study.
SUBJECTS: One hundred adults with spinal cord injury admitted to spinal units in Sydney, Australia within a 24-month period.
METHODS: In-Voc was offered to all inpatients within the first 6 months of acquired spinal cord injury and was provided by trained vocational consultants. Baseline demographics, opinions about work readiness, details of the vocational services provided and preliminary employment outcomes were documented.
RESULTS: The In-Voc programme was relatively short in duration (median 11 weeks, range 3–39 weeks) with a median total of 9.1 h (range 1–75.2 h) of service delivered per participant. At case closure (median 3 weeks post-discharge), 29/84 (34.5%) of participants were in paid employment (7% full-time, 8% part-time, 7% on sick leave, and 12% working with hours unknown), 36% were unemployed (6% seeking work, 16% not seeking work, 14% job seeking status unknown), 13% were students or in-training, and 17% were in vocational rehabilitation.
CONCLUSION: Our research suggests that implementing an early vocational rehabilitation programme with individuals in the hospital setting is feasible and has good potential for enhancing post-injury labour-force participation.
Key words: spinal cord injury; inpatient; employment; vocational rehabilitation.
J Rehabil Med 2015; 47: 626–631
Correspondence address: James Middleton, John Walsh Centre for Rehabilitation Research, Sydney Medical School Northern, 2065 Sydney, Australia. E-mail: james.middleton@sydney.edu.au
Accepted Mar 27, 2015; Epub ahead of print Jun 1, 2015
INTRODUCTION
Spinal cord injury (SCI) commonly affects multiple body structures and functions, resulting in activity limitations and reduced community participation, such as employment. A review by Ottomanelli & Lind (1) concluded that the average rate of any remunerative employment for individuals after SCI is only approximately 35%, yet the benefits of employment are clear (2). In interpreting any aggregate post-SCI employment rate, it is important to note that, in the initial years after injury, vocational achievement is appreciably reduced. In their review of post-SCI employment rates (reported in over 20 studies conducted across 4 geographical regions), Young & Murphy (3) concluded that “employment data collected a year or less post-injury are associated with a much lower employment rate” (p. 7). In the North American studies reviewed by Young & Murphy, the employment rate at 1 year post-injury was approximately 14%. The steady rise in employment with increasing years post-injury is clear in the pattern of employment rates reported by Krause et al. (4) and confirmed by Young & Murphy (3), where the employment rates following SCI increased progressively at each of the 1, 2, 5 and 10-year follow-ups, plateauing at approximately 35% at 10 years, thereafter reaching 39% at the 20-year anniversary of injury.
In a recent review of models of effective vocational rehabilitation (VR) service delivery, provision of “Supported Employment” (SE) and inter-agency collaborations were found to be among the “best practices” (5). The Individual Placement and Support (IPS) model of SE has consistently demonstrated positive outcomes for individuals with mental health disorders in multiple randomized controlled trials (6). It was recently shown in a first ever randomized controlled trial among veterans with SCI in an outpatient and community setting to be 2.5 times more likely to result in competitive employment. It was suggested that, perhaps, better outcomes may be achieved if VR is offered closer to the time of initial injury before social disenfranchisement and reliance on disability benefits become ingrained (7).
VR is not generally provided during inpatient rehabilitation in Australian SCI units. Where services are available, they are typically delivered post-discharge from hospital with referral to a community provider. Due to the suboptimal return-to-work (RTW) rates achieved presently (3), there is a clear need to develop new models to improve vocational outcomes following SCI.
The aims of this paper are: first, to describe a novel pilot programme, called In-Voc, that provides early VR during the subacute phase of inpatient rehabilitation after an acquired SCI, and, secondly, to quantify its components and report early vocational outcomes.
The rationale for developing the programme was to promote early positive patient expectations, while incorporating clear and realistic RTW goals into the patients’ overall rehabilitation goals. It was also based on the realization that the delay in provision of employment services until after the patient is discharged from hospital might contribute to the loss of pre-injury vocation, a delayed return to work (RTW), or negative vocational outcomes (8).
METHODS
Description of In-Voc model and its implementation
In-Voc is a pilot programme developed and funded by the “Lifetime Care and Support Authority” (LTCSA), a state government statutory authority in New South Wales (NSW), Australia. Following a competitive tender process, the Commonwealth Rehabilitation Service, part of the Australian Government Department of Human Services (CRS Australia), was chosen from among established VR providers to develop and deliver an early intervention (inpatient) VR programme for people with SCI. Ethics approvals were received from the relevant Human Research Ethics Committees at each of the sites described below prior to commencement. Delivery of the In-Voc pilot programme began on 1 June 2011 and ran for 24 months until 30 May 2013.
The In-Voc pilot programme, inspired by the Kaleidoscope early-intervention VR programme (http://www.kaleidoscope.org.nz/), is based on an individualized case management model using a strengths-based approach (9) and the principles of motivational interviewing (10), underpinned by theories of work adjustment (11), self-efficacy (12), and positive coping and adjustment (13). Important aspects of In-Voc include detailed career planning to match the individual’s motivation, experiences and skills to the available job possibilities, on-going individual career coaching with a strong emphasis on the person with SCI doing as much of the work as possible for themselves, and post-placement support to ensure a smooth transition back into the workforce. In-Voc was implemented with 3 vocational consultants (VCs) working 2.2 full-time equivalents (FTE), employed by CRS Australia, each separately located at 1 of 3 specialized SCI units in Sydney at the Prince of Wales Hospital (acute care and rehabilitation units co-located), at Royal North Shore Hospital (acute care unit) and at Royal Rehabilitation Centre (rehabilitation unit). The contracted VCs possessed extensive experience in VR and counselling, having allied health professional backgrounds, with 2 being occupational therapists (0.4–0.8 FTE) and 1 being a rehabilitation counsellor/social worker (1 FTE). Relief was provided for an extended period of leave taken by a 0.4 FTE occupational therapist.
The VCs worked collaboratively with spinal unit clinical teams, attending case conferences, discharge planning and other relevant meetings, as well as contributing to medical records, to ensure integration of In-Voc into the overall inpatient rehabilitation programme. This enabled the VC to know about each person’s rehabilitation goals and psychological adjustment. Being onsite, rather than a visiting service, also afforded flexibility with scheduling client meeting times and the intensity of support provided, as each person’s focus on work and study changed over time.
In-Voc team training
Prior to delivery, VCs received 3 days of formal training in May 2011 by Kaleidoscope Consulting International (KCI), which focussed on improving knowledge about the psychosocial effects of SCI and specific issues pertaining to delivery of high-quality VR services in this group. Following this training, KCI provided ongoing support to the In-Voc team via regular teleconferences regarding its implementation, which afforded an opportunity for the consultants to learn from Kaleidoscope team case reviews to gain an understanding of the range of vocational services they offered. Further training (1 day) by KCI in September 2011, covered techniques for applied optimism, coaching and mentoring, and relationship building in people with SCI.
Description of intervention
In-Voc delivers VR services within the first 6 months of SCI in an inpatient hospital setting. For equity reasons during implementation, the In-Voc pilot programme was offered to every admitted person with SCI during the pilot study, regardless of time since injury. However, those over 6 months post-injury were excluded from formal evaluation based on the “early intervention” criterion. The evaluated group received 1.3 FTE of VC time (i.e. 60% of total 2.2 FTE).
Initial contact was made by a VC within 1–8 weeks from time of admission, after consultation with treating health professionals at case conference to check that the person was well enough (medically and psychologically) to be offered this intervention. The programme was firstly explained to the person with SCI by the VC and then given the option to participate. Having obtained informed consent, the VC would then work with the person with SCI to undertake comprehensive VR assessments for identifying barriers, solutions and initiatives to facilitate RTW and supporting development and implementation of an individual RTW plan.
In general, the first meeting focussed on obtaining background information about the person’s pre-injury status, developing rapport, understanding personal context and motivations, and gauging readiness to commence career planning. Clients who had a job to return to were encouraged to explore the pros and cons of retaining that role and consider issues impacting on return to their pre-injury work. If the pre-injury role was not their vocational goal or was no longer available or possible, support was provided to consider new options. Training courses could be commenced during admission with support to assist in the early stages of any course. Clients were also encouraged to explore study and volunteer positions.
The specific VR services provided by the VCs included engaging in vocational conversations about RTW expectations, promoting and facilitating a timely and safe RTW or return to study, vocational counselling to explore RTW options and liaison, education and negotiation with current or potential employers. Job-seeking skills-training, workplace assessment, task analysis, facilitating access to work experience and work trial opportunities were also provided where appropriate.
Re-training opportunities were explored through establishing relationships and refining processes with key service providers who could support and facilitate RTW, for example, Centrelink (the Australian government portal for income support), Technical and Further Education NSW (the largest vocational education and training provider in Australia) and Spinal Outreach Service (a community-based specialist multidisciplinary team that follows up people with SCI for 12 months post-discharge from hospital).
Referral to external service providers post-discharge was made as needed based on each person’s choice, ensuring VR continuity. This was done together with provision of information to patients and SCI unit clinical team about Australian commonwealth and state funded services and programmes that support RTW or study. In addition, the VCs’ roles involved communication, reporting and documentation as part of the research evaluation and also as required by the funder, LTCSA.
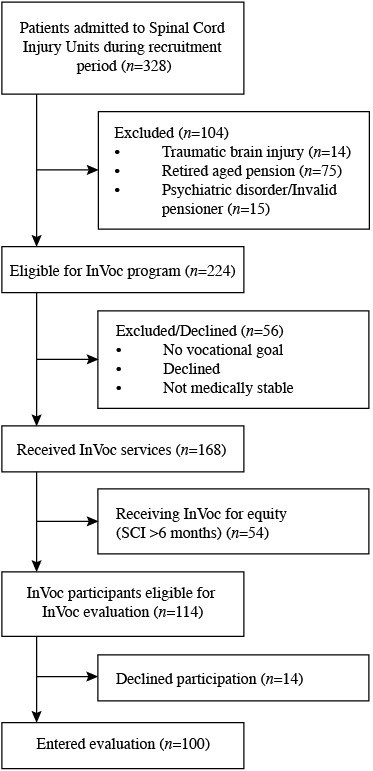
During the 2 years that the voluntary pilot was conducted, 51% (168 of 328 new admissions) of admitted patients from the SCI units participated in the programme. One-hundred and four patients were not approached, with the majority of those being retired elderly pensioners, and the remainder having medical or psychological issues and deemed unsuitable for vocational intervention by the treating team. Study recruitment and attrition is presented in Fig. 1.
Fig. 1. In-Voc evaluation recruitment.
Programme evaluation and recruitment
A total of 114 In-Voc participants were eligible for evaluation; being 16-years of age and older, English speaking, and having sustained SCI in the 6 months prior to enrolment. Fourteen participants declined evaluation, with the remaining 100 (88%) entering the programme evaluation by providing informed consent and completing baseline interviews consisting of demographic details and questionnaires concerning their RTW expectations and vocational opinions.
RESULTS
Evaluation participants
Baseline characteristics of evaluation participants are presented in Table I. The median age of evaluated In-Voc participants was 34 (range 16–76) years. The majority were males (82%), single (56%), spoke English as their first language (89%) and had completed high school education (69%). At the time of injury, 86% of participants were in paid employment (78% full-time, 8% part-time), 9% were unemployed (half of those seeking employment) and 5% were full-time students. There was a wide spread of occupations, with 52% in blue-collar roles. Level and extent of neurological impairment were specified according to the International Standards for Neurological Classification of SCI (14), including the American Spinal Injury Association (ASIA) impairment scale (AIS) grades A–D. Fifty percent of participants had tetraplegia (40% AIS grade A) and 50% had paraplegia (33% AIS grade A).
|
Table I. Baseline characteristics of In-Voc evaluation participants |
|
|
Characteristics (n = 100) |
|
|
Age, median (IQR) |
34 (23, 44) |
|
Sex, % male |
82 |
|
Nationality, % Australian/Indigenous |
79/4 |
|
Marital status (n = 100), n |
|
|
Single |
56 |
|
Married |
38 |
|
Divorced/separated |
6 |
|
Education (n = 99), % |
|
|
Primary school |
1 (n = 1) |
|
Year 10 High school |
30 (n = 30) |
|
Year 12 high school |
20 (n = 20) |
|
College/university – incomplete |
15 (n = 15) |
|
College/university – complete |
28 (n = 27) |
|
Postgraduate – complete |
6 (n = 6) |
|
Employment (n = 95), % |
|
|
Full-time |
78 (n = 74) |
|
Part-time |
8 (n = 8) |
|
Student |
5 (n = 5) |
|
Unemployed seeking work |
4 (n = 4) |
|
Unemployed not seeking work |
4 (n = 4) |
|
Occupation (n = 95), % |
|
|
Manager |
12 (n = 11) |
|
Professional |
18 (n = 17) |
|
Community/service worker |
4 (n = 4) |
|
Sales worker |
9 (n = 9) |
|
Clerical/administration |
5 (n = 5) |
|
Technician/trades worker |
32 (n = 30) |
|
Machinist/driver |
7 (n = 7) |
|
Labourer |
13 (n = 12) |
|
Level of injury (n = 98), % |
|
|
Tetraplegia |
50 (n = 49) |
|
40 AIS grade A |
|
|
Paraplegia |
50 (n = 49) |
|
33 AIS grade A |
|
|
AIS: American Spinal Injury Association (ASIA) Impairment Scale (which grades the extent of impairment from A to E (14)); IQR: interquartile range. |
|
In-Voc Service provision and return to work readiness
Participants were involved in the In-Voc pilot for a median duration of 11 weeks (range 3–39 weeks), being followed up in the community post-discharge from hospital for a median period of 3 weeks (range 0–19 weeks). The provision of programme services fell into 3 main categories; administration, pre-vocational services and vocational services. During In-Voc, the VCs recorded a median total of 9.1 h delivering programme services to their participants (n = 94, range 1–75.2 h). This total comprised 1.4 h (range 0–27.9 h) for administrative tasks; 3.4 h (range 0–27.7 h) for pre-vocational activities, and 1 h (range 0–46.3 h) for vocational activities; with 10.7 h (range 1–44.3 h) of uncategorized time recorded in the first 6 months of the programme (up to November 2011). A considerable amount of the face-to-face time with inpatients was spent exploring the demands of various vocational options, which often involved the person with SCI and/or VC exploring what is required (past experience/training, specific job duties, training and workplace modifications), undertaking workplace visits, exploring public transport and testing physical functioning with hands-on trials of simulated work activities or modified equipment on the rehabilitation ward.
A preliminary assessment of self-reported responses for RTW readiness against hours of In-Voc service delivery for 56 participants with complete data revealed that more hours were delivered across all categories (administration, pre-vocational and vocational) for participants who identified “work is an important part of my life”. Fewer hours were delivered across categories to those who believed they were unable to find employment “no matter what” (vocational category only), but also those who believed they were “capable of gaining employment within 6 months” (all).
Vocational achievement
In-Voc pilot programme discharge employment statistics were available for 84 of the 100 participants either at the time of programme discharge, or within the first 11 months when employment status was discovered by the VCs. At case closure, 29 (34.5%) participants were in paid employment (7% full-time, 8% part-time, 7% on sick leave, and 12% working with hours unknown). Of the 55 (65.5)% who were not in paid employment at case-closure, 36% were unemployed (6% seeking work, 16% not seeking work, 14% job-seeking status unknown), 13% were students or in-training, and 17% were in full-time VR with other providers.
Whilst the majority of those in paid employment had been employed prior to injury and had returned to the same employer in the same role, 3 participants had returned to the same employer, but with alternative duties. Notably, 2 participants who were not employed at the time of injury (1 person being a full-time student and the other being unemployed and seeking work) gained new employment.
The total hours received by the group who had regained paid employment by the time of In-Voc case closure compared with the unemployed group were similar. However, the employed group tended to receive more hours for administrative support and less pre-vocational hours than those who were unemployed or studying (Table II).
|
Table II. Hours of In-Voc service provision and employment status at case closure |
|||||
|
Status |
Administration Median (range) |
Prevocational Median (range) |
Vocational Median (range) |
Uncategorised Median (range) |
Total Median (range) |
|
Employed (n = 29) |
1.8 (0–15.8) |
2.5 (0–49.1) |
1.1 (0–13.9) |
10.4 (1.9–44.3) |
9.8 (1–78.8) |
|
Unemployed (n = 55) |
1 (0–27.9) |
4.2 (0–52.6) |
0.9 (0–13.7) |
10.7 (0.9–35.5) |
9.3 (0.9–90.2) |
It was hypothesized that higher RTW motivation would be associated with earlier employment. No significant differences were found in self-reported RTW readiness between clients who had and had not returned to paid employment by the time of case closure from In-Voc. The majority of all participants agreed that work was an important part of their life (96%), that it was their own actions that would affect whether they would get a job (84%), that the help of others would be required to secure a job (66%), and that they were capable of becoming employed within 6 months of the time of interview (63%). Most disagreed that whatever they did they could not find future employment (77%).
DISCUSSION
This paper describes the development, implementation and initial outcomes of a hospital-based early intervention VR programme (In-Voc) designed to fill a gap in SCI rehabilitation services offered to inpatients. Results from delivery of the programme and the initial achievement of the subgroup whose cases were closed suggested that the initial vocational achievements were above those reported by peers in the initial years post-injury. Krause et al. (4) in their large national study of over 3700 persons with traumatic SCI reported that, even among those with pre-injury employment (i.e. those with demonstrated higher vocational potential), less than 25% were working 2 years post-injury). In addition, our currently reported employment rates can be confidently expected to rise steadily over the next 2–5 years (3). The value of returning to work after SCI for personal, economic, social and health benefits is well recognized (15–17) and ideally VR should be an inherent part of any specialized inpatient multidisciplinary rehabilitation programme (18). Unfortunately, VR is often given little attention due to competing demands and shorter lengths of stay in hospital, as well as many health professionals not appreciating the health value of employment (19, 20).
Traditionally, VR commences only after the individual with SCI has completed an inpatient multi-disciplinary medical rehabilitation programme and been judged to be medically and psychologically ready. Our research suggests that implementing an early VR programme with individuals who are still in the hospital setting is feasible and has good potential for enhancing post-injury labour-force participation.
A main characteristic of this pilot study (which is unique in Australia) was its early intervention, with people being approached by a VC as early as 1–8 weeks post-SCI, with its successful introduction extending the range of community-based vocational services presently offered to SCI population (21). By changing this traditional gap in service within the SCI units, the In-Voc pilot introduced a service element that encouraged inpatients to see the possibility of returning to some form of future work and/or study and redevelop vocational identity, exploring what they could do at a time when they may have otherwise focused on losses. Others have highlighted the important role that hope and positive appraisals may play in the process of psychological adjustment to SCI (13).
Fadyl & McPherson (22) have previously drawn attention to the importance of early access to well-linked, vocationally-focussed support services, ideally being integrated into specialized inpatient rehabilitation. These authors noted that influences on decision-making about employment begin quite early after injury, involving factors such as self-confidence, perceptions about physical ability to work again and capacity to cope with everyday tasks necessary for an employed person (e.g. toileting), with the decision-making process often hampered by a lack of reliable occupational information, thereby creating uncertainty about job options and employer expectations.
The unknown impact of future health issues on general employability and job retention was also of concern. Similarly, in the present study, patients often presented with barriers based on their previous work knowledge and beliefs about perceived restrictions imposed by SCI. The In-Voc model seemed to have empowered and motivated individuals, building confidence that RTW is a realistic rehabilitation outcome, by focussing on achieving relevant goals, participating in successful experiences while in hospital, providing support to make informed decisions and developing an awareness of adaptations, modifications and assistive devices.
Integration with the inpatient rehabilitation team and their processes appeared central to the success of In-Voc. The VCs added specific vocation-related knowledge and skills, as well as dedicated time for vocational exploration that was otherwise lacking, thereby strengthening and complementing the rehabilitation programme. Prior to the pilot, vocational goals may well have been considered in the rehabilitation process; however, In-Voc provided the specialized services necessary to consider options and to maintain focus on existing employment options during the extended periods of hospitalization and inpatient rehabilitation following SCI.
Having the In-Voc team located on the SCI units made the VCs more accessible, involved and “part of the team”, ensuring that work or study goals could be included as an integral part of rehabilitation goal setting and discharge planning processes. This integration meant that it was possible to design and tailor experiences during rehabilitation so that clients could start to realize and explore the vocational possibilities, bringing work-related equipment and/or incorporating use of assistive technology into other therapy sessions. VCs were flexible with meeting times fitting in around other scheduled or unplanned appointments or tests, as well as with the intensity of support provided, as each client’s focus on work and study naturally changed over time.
Through regular observation and interaction during the inpatient stay, VCs developed good rapport, with detailed understanding of the person with SCI, their unique background, roles and family supports, and where employment fits into their life. Having developed an effective working relationship with the person (along with continuity, shared understanding and respect) became most valuable later on when addressing the wide range of personal or contextual issues that can impede RTW (23).
By the time of discharge, clients and the VC had a clear understanding of the ongoing vocational provider supports required. VCs were able to link clients with ongoing VR providers and facilitated meetings with the providers to continue the planning and job-seeking activities after discharge or, if clients had not been ready during hospital admission, refer to these community-based services to kick-start the process. Prior to discharge, clients were provided with information about funding possibilities and various supports and resources available. After discharge, VCs continued to be available and invited clients to make contact for follow-up assistance after they had returned home.
There are a variety of obstacles that may be encountered when trying to implement a model such as In-Voc into inpatient rehabilitation services in other states or countries. Attitudes of the clinicians within the rehabilitation team were paramount to ensuring the development of good working relations and cohesion between In-Voc VC and rehabilitation staff and this required a strong leadership model. Funding for such a programme within a health service environment that is activity-based and focussed on reducing lengths of stay will be challenging and requires strong advocacy with an innovative cross-sectoral government approach. Fear of loss of compensation entitlements or social security benefits are strong disincentives that must also be addressed by further education and advocacy for policy change with relevant government agencies to motivate RTW with incentives, such as maintained benefits or subsidies to offset the financial burden of healthcare and transport-related or other costs.
The aim of this paper was to describe the protocol and implementation of the In-Voc programme. One key limitation to note is inconsistency in the early recording of service provision data by VCs, resulting in “uncategorized” time records, which cannot be grouped as administration, pre-vocational or vocational. A second limitation is that the client outcome data presented were recorded at case closure (often within 3 weeks of discharge from hospital) and as such can only be considered as very early, preliminary results. Finally, not all patients of working age chose (or were fit) to participate in In-Voc, which may have introduced some bias.
Future directions for research should include replication within other service systems (states and countries) in SCI population with more focussed and standard, manualized training for VCs. Studies in future should longitudinally track individual pathways, following progress with re-training and RTW, including barriers and time frames depending on job types and vocational backgrounds, as well as concentrate more on follow-up post-RTW regarding career development, job preferences and work satisfaction (24). It would also be useful to include economic analyses to calculate cost-benefit of a model with VCs in situ in inpatient rehabilitation compared with community-based programmes post-discharge.
The In-Voc role could be usefully extended along the lines of the highly successful IPS/SE model (25, 26). It could also be incorporated with other models such as the North American Bridge programme (27), whereby regional “bridging” staff act as the case managers after discharge into the community to accomplish unfinished goals and set new ones, liaising with the inpatient rehabilitation team and a vocational specialist to advance RTW efforts. Developing close involvement of local business, a key feature of the Kaleidoscope programme in New Zealand, could help identify fruitful job search strategies for gaining employment within target industry sectors.
In conclusion, very few SCI rehabilitation studies to date have focussed on early interventions to accelerate RTW or make people with SCI more employable. In contrast to the traditional “medical rehabilitation” model, which tends to be focussed on pathophysiological changes, physical functioning and activity limitations, In-Voc creates a positive expectation about future participation at a time when patients may otherwise be feeling quite despondent and beginning to believe that they are unlikely ever to work again. Future reporting of vocational achievements for all individuals receiving In-Voc services at key intervals (e.g. 2 and 5 years post-injury) will allow determination of the programme’s true worth against existing rates of employment reported in the literature.
ACKNOWLEDGEMENTS
Funding for this service development initiative and related research was provided by the NSW Lifetime Care and Support Authority.
REFERENCES
