Elizabeth Taylor, MSc1, Christopher McKevitt, PhD1 and Fiona Jones, PhD2
From the 1Department of Primary Care and Public Health Sciences, Division of Health and Social Care Research, King’s College London and 2Faculty of Health, Social Care Sciences and Education, Kingston University and St George’s University of London, London, UK
OBJECTIVE: To investigate factors shaping the delivery of acute inpatient stroke therapy (i.e. occupational therapy, physiotherapy, and speech and language therapy).
DATA SOURCES: A systematic search using electronic databases: AMED, CINAHL, Medline, Web of Knowledge and EMBASE.
STUDY SELECTION: Qualitative studies (n = 31) investigating delivery of inpatient stroke therapy, published since 1998, were included.
DATA EXTRACTION: Narrative synthesis was used as the review method. Textual descriptions, tabulation and thematic analysis were used to categorize findings and explore relationships between studies.
DATA SYNTHESIS: Data synthesis generated the following themes: the need for a therapeutic environment; power and decision-making; intensity, motivation and appropriateness for active therapy; therapy behind the scenes; the role of teamwork in creating a therapeutic environment. Delivery of therapy was influenced by conceptual, individual and professional factors.
CONCLUSION: Conceptual, individual and professional factors impact on the delivery of rehabilitation. Further research is needed to examine how therapists negotiate the sometimes conflicting factors shaping delivery of therapy.
Key words: stroke; rehabilitation; therapy; stroke unit; hospital; inpatient.
J Rehabil Med 2015; 47: 107–119
Correspondence address: Elizabeth Taylor, Primary Care and Public Health Sciences, King’s College London, SE1 3QD London, UK. E-mail: elizabeth.taylor@kcl.ac.uk
Accepted Sep 15, 2014; Epub ahead of print Dec 1, 2014
Introduction
Stroke management underwent a paradigm shift at the end of the last millennium, from a prevailing attitude of passive pessimism regarding the fate of stroke survivors (1) to the emergence of stroke rehabilitation as an attractive and dynamic specialism with a growing evidence base (2). The value of stroke rehabilitation, provided by therapists to promote the restoration of lost function, independence and quality of life, was increasingly recognized and promoted (3–7).
Multi-disciplinary stroke teams typically include doctors, nurses, social workers, therapists, dieticians and psychologists. Occupational therapists (OTs), physiotherapists (PTs), and speech and language therapists (SLTs), are the primary members of the team concerned with providing therapy. Each therapy has different defining principles, but all share the aims of providing rehabilitation to maximize independence, reduce impairment and prevent further complications after a stroke (8). National guidelines in many countries recommend “increased therapy intensity” without further specification, whilst some specify a daily minimum (9–14). There is variation in the delivery of therapy internationally, and audits conducted in England and Wales suggest that the national standard regarding intensity is not being met (15–18). Quantitative studies investigating therapy delivery have focussed on quantifying time spent in physical activity or physical rehabilitation interventions (19–23). However, the varied content of therapy sessions cannot be captured by measuring physical activity, and the objectives of therapy sessions are not the same for all stroke patients (24). Qualitative studies lend themselves to investigating context and processes that may lead to variations in the delivery of therapies.
There is a need to improve understanding of the processes of stroke rehabilitation and contextual factors affecting the allocation of therapists’ time (18, 25, 26). We sought to address this by reviewing qualitative studies investigating the factors shaping delivery of inpatient therapy for stroke patients.
Review Methods
Narrative synthesis was chosen as the review method, as this provides a systematic, transparent approach, with guidance on enhancing trustworthiness (27). Narrative synthesis involves developing a theory at an early stage of the review; developing a preliminary synthesis; exploring relationships in the data; and assessing the robustness of the synthesis product (27). The theoretical basis of this review is that delivery of healthcare is shaped by structure and process, and that asking “what goes on” enables critical enquiry into elements of structure, process or outcome (28).
Data sources
The following electronic databases were searched: AMED, CINAHL, Medline, Web of Knowledge and EMBASE. Search terms included: stroke, rehabilitation, therapy, stroke unit, hospital and inpatient. Where possible a filter was used to select qualitative studies. Table I sets out the search terms and results. Reviews of relevant qualitative studies were checked for additional references (6, 29–34). The first author (ET) conducted the database searches and initiated analysis, which was checked by the 2 other authors (CM and FJ) at regular stages of the process.
|
Table I. Search terms |
|
|
Database |
Search terms |
|
EMBASE (Ovid) |
1 exp stroke/ or stroke* 2 exp rehabilitation/ or rehab* or therap*/ or therap* 3 exp Stroke unit/ or stroke unit* or hospital*/ or hospital* or inpatient*/ or inpatient 4 Filter (((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (interview* or discussion* or questionnaire*)) or (focus group* or qualitative or ethnograph* or fieldwork or “field work” or “key informant”)).ti,ab. or interviews as topic/ or focus groups/ or narration/ or qualitative research/ 5 1 and 2 and 3 and 4 |
|
AMED |
1 stroke or stroke* 2 rehabilitation or rehab* or therap* 3 “stroke unit*” or hospital* or inpatient* 4 1 and 2 and 3 |
|
CINAHL |
1 MH stroke+ or stroke* 2 MH rehabilitation+ or rehab* or MH therap* ((MH “Occupational Therapist Attitudes”) OR (MH “Physical Therapist Attitudes”) OR (MH “Occupational Therapists”) OR (MH “Physical Therapists”) OR (MH “Occupational Therapy”) OR (MH “Physical Therapy”) OR (MH “Speech Therapy”)) or therap* 3 MH stroke unit or stroke unit* or MH hospital* or hospital* or MH inpatient* or inpatient* 4 1 and 2 and 3 |
|
MEDLINE |
1 exp stroke/ or stroke* 2 exp rehabilitation/ or rehab* or therap*/ or therap* 3 exp Stroke unit/ or stroke unit* or hospital*/ or hospital* or inpatient*/ or inpatient 4 Filter (((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (interview* or discussion* or questionnaire*)) or (focus group* or qualitative or ethnograph* or fieldwork or “field work” or “key informant”)).ti,ab. or interviews as topic/ or focus groups/ or narration/ or qualitative research/ 5 1 and 2 and 3 and 4 |
|
Web of Science |
Databases=SCI-EXPANDED, SSCI, CCR-EXPANDED, IC Timespan=1997–2013 1 stroke* 2 rehab* or therap* 3 “stroke unit*” or hospital* or inpatient* 4 Topic=(((“semi-structured” OR semistructured or unstructured OR informal or “in-depth” OR indepth OR “face-to-face” OR structured OR guide) NEAR/3 (interview* OR discussion* OR questionnaire*))) OR Topic=((focus group* OR qualitative OR ethnograph* OR fieldwork OR “field work” OR “key informant”)) 5 1 and 2 and 3 and 4 |
Study selection
Studies published prior to 1998 were excluded, as the aim was to investigate inpatient therapy under the current paradigm. We sought to include studies published in English, using a qualitative method and relating to stroke rehabilitation or therapy provided by therapists in inpatient settings. Studies were excluded if they focussed on a specific tool, assessment or intervention (e.g. use of walking aids). Studies were excluded if they reported predominantly quantitative findings, as were studies in which qualitative and quantitative findings could not be separated. Studies investigating multiple settings were admissible, provided that an inpatient stroke setting was included. Quality assessment of qualitative studies has been noted to be problematic, as opinions differ on how quality should be assessed, and there is a risk that reducing qualitative research to a list of technical procedures can be overly prescriptive and counterproductive (35, 36). We chose to take an inclusive approach to study selection, but also used an established checklist to judge whether any studies were “fatally flawed” (35).
Data extraction and analysis
Data extraction and analysis were guided by the narrative synthesis approach (27). Data on study design, setting, participants, location, methods, quality, theoretical framework and key findings were extracted from the selected studies by 1 reviewer (ET), then checked independently by 2 reviewers (CM and FJ). Textual descriptions, tabulation and thematic analysis were used to categorize findings. The objective of the preliminary synthesis was to generate themes from the findings of included studies. Themes were adjusted, merged or excluded by a process of discussion between authors. Following preliminary data analysis, we explored relationships in the data in a secondary synthesis, in order to develop a richer understanding of factors shaping the delivery of therapy (27). We referred back to the initial theory, that structure and process shape healthcare delivery, and used narrative synthesis tools, including conceptual mapping and ideas webbing, to interpret the findings (27). Sticky notes were used to group patterns and themes into broader theoretical factors, and these were iteratively reviewed with all members of the review team, using a whiteboard to map out relationships between themes and factors. There was frequent and indepth discussion amongst the reviewers of the findings, their fit, and how synthesis could further understanding of factors shaping the delivery of inpatient stroke therapy.
Results
Summary of included studies
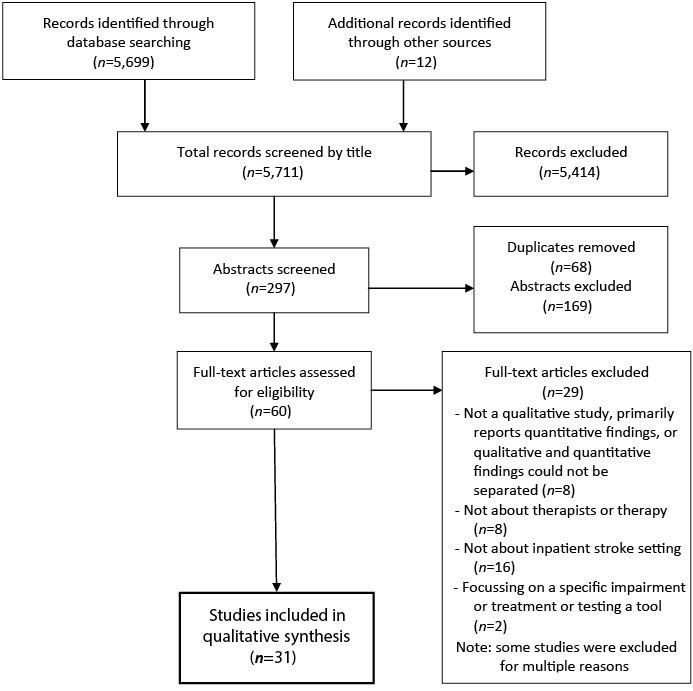
A flow diagram of the search process is shown in Fig. 1. Thirty-one studies were included; the characteristics of included studies are shown in Table II. Methods used in the studies included focus groups, interviews, observational studies and case studies. Participants included therapists, other members of the multi-disciplinary team, patients and carers. Eighteen of the 31 studies were based in the UK, with others set in Ireland (n = 2), the USA (n = 2), Canada (n = 1), Scandinavia (n = 4), Australia (n = 3), New Zealand (n = 1), The Netherlands (n = 1) and Belgium (n = 1). (Two studies were based in 2 countries). The studies were largely technically satisfactory in accordance with the checklist (35). The most common quality issues that arose were unclear reporting of sampling and data collection, and these are noted with the characteristics of included studies in Table II. Scale varied from a single case study to a large-scale study involving 1,400 stroke survivors in the USA and New Zealand. At least 22 of the studies included 10 or more participants, but this total excludes the minority of studies in which the sample was not clearly defined. For example, more than one observational study lacked details regarding the number of patients and staff members involved. All included studies were considered to make relevant contributions to the review question.
|
Table II. Characteristics of included studies |
||||
|
Reference and country |
Setting |
Participants |
Methods |
Relevant findings |
|
Allen et al., 2002 (62) UK (Wales) |
Acute and community stroke care in 2 health authorities. |
Four stroke patients with complex continuing care needs, and their “surrounding web of care”. |
Four case studies, involving interviews with stroke patients, interviews with those who delivered care (paid and unpaid), and observations of meetings and home visits. These took place across the acute and community pathway over 6 months. Setting not clearly described. Sampling not clearly described. |
Flexible working: health and social care providers worked together with flexible boundaries to ensure smooth transitions between services. Speech and language therapist (SLT) had key role in explaining patient’s communication problems in a range of environments, and gave advice to people working across the pathway. Lead professional: Could be any member of the team. Keyworker not always identifiable; authors reported a need to formalize this. General practitioners not very involved. Transition from hospital to home: Effective discharge planning involves skilful teamwork and management of health and social care interface. Time of anxiety for patients, with potential for problems occurring. Prognostic uncertainty and unknown impact of home environment and support networks make planning difficult. |
|
Allen et al., 2004 (57) UK (Wales) |
Acute and community stroke care in 2 health authorities. |
Eight stroke patients with complex continuing care needs and all those involved in their care (e.g. OT, nurse, consultant, general practitioner, PT, etc.). |
Eight case studies with snowball sampling to identify all those involved in their care. Continuing care explored using ethnographic methods (observation and interviews) for 6 months. Setting not clearly described. Sampling not clearly described. |
• Health and social care professionals are responsible for micro-level resource allocation, and are resourceful in findings ways of meetings the needs of individuals. • Patients without means to privately purchase equipment and services essential for discharge may remain in hospital longer, despite being clinically ready for discharge. • “Need” becomes narrowly defined in terms of risk management. Treatment may be revised to fit with the service available. • More pressure on services in areas of high socio-economic deprivation due to patients having complex needs and no private finance. • Conceptions of “deservingness” may influence decisions, specifically regarding discharge plans. Having family with private finance and social capital to “work the system” can also influence decisions. |
|
Baxter & Brumfitt, 2008, (63) UK |
Three teams providing stroke care: acute, stroke unit (SU) and community. |
Thirty-seven staff (nurses, PT, OT, SLT, non-qualified, other professionals). |
Multiple case study, interviews. Reports on interviews but does not explain if “multiple case study” involved additional forms of data collection. |
• Advantages of teamwork include: providing a supportive environment for staff and patients; sharing information and knowledge to enhance clinical problem-solving and decision-making; gaining a more “whole-person” view of the patient; timeliness of care; shared and consistent decisions. • Concerns regarding the need to balance patient contact time against team-working time, e.g. meetings, team record-keeping and goal-planning. |
|
Bayley et al., 2012 (59) Canada |
Five inpatient stroke rehabilitation centres. |
Seventy-nine rehabilitation professionals (23 OTs, 17 PTs, 23 nurses, 16 managers). |
Twenty-one focus groups of 3–9 participants each. |
• Barriers to implementation of evidence-based recommendations: time constraints, staffing issues, training/education, therapy selection and prioritisation, equipment and team functioning/communication. • Individual recommendations were reportedly easier to implement than a complete package due to time constraints. Insufficient interaction between professionals and a short-term focus on individual tasks was said to be exacerbated by staffing shortages. |
|
Bendz, 2000 (53) Sweden |
Acute stroke ward and community follow-up. |
Twelve people following first incidence of stroke, under 65 years, admitted to the hospital over 1 year. |
Discourse analysis, using interviews with stroke survivors and transcripts from their medical records for the first 3 months after the stroke. |
• Patients perceived training of their impaired body parts as their means to recovery, and perceived that more training would lead to better recovery. They placed trust in therapists as experts and expect them to design and assess their training, including the quantity and timing. This passive role in hospital was in contrast to the experience of returning home. • Therapy entries in medical records had a biomedical focus, describing impairments, risk and disability. • Patients considered recovery in terms of returning to their previous lives, whereas therapists had a more limited construct of recovery in terms of certain functional abilities. |
|
Table II. Contd. |
||||
|
Reference and country |
Setting |
Participants |
Methods |
Relevant findings |
|
Bendz, 2003 (54) Sweden |
One stroke unit. Interviews were conducted in patient’s home after discharge. |
Fifteen patients. |
Interviews with patients, and analysis of health-professionals’ documentation (including doctors, nurses and therapists). |
• Patient records focussed on reduced functions and training. • Patients expressed anxieties about loss of control, relapse and fatigue that were not reflected in the formal notes written by professionals. |
|
Booth, 2002 (45) UK |
Ten inpatient stroke rehabilitation settings in urban hospitals, each in a different health authority. |
Eighteen therapists (9 OTs and 9 PTs). |
Semi-structured interviews. |
• Main components of OT and PT and role overlap were presented. • OTs and PTs felt there were some aspects of role overlap, but that the professions had different philosophical backgrounds and therapeutic approaches. • OTs and PTs felt that the role of OTs was less well known and had the potential to be misunderstood. • Positive collaboration in teams was associated with reduced anxiety about role overlap experienced by OTs and PTs. |
|
Bowman, 2006 (65) Australia |
Stroke services in 2 acute hospitals, 2 rehabilitation centres and 2 community centres. |
Ten OTs: 6 working in hospital (2 acute, 2 rehabilitation centres) and 4 community based. |
Three focus groups. |
• OTs found measuring their effectiveness difficult. • Challenges in clearly articulating the OT role. The primary goal of OT was found to be to maximize occupational independence in order to allow clients to safely participate in life roles that were important or meaningful to them. • OTs viewed their role as broad and complex. Concerned that having to focus on discharge planning prevented them from providing occupation-focused interventions. |
|
Cavanaugh & Schenkman, 1998 (46) USA |
Inpatient rehabilitation unit. |
One stroke patient. |
Case history. Sampling not clearly described, i.e. rationale for selecting this patient for single case study. Therefore not clear whether this is presented as a typical or unusual case. |
• The purpose was to illustrate the decision making process used by a PT. • Concluded that therapists require a complete understanding of case complexities to develop efficient therapeutic intervention. • Efficiency is critical. • Therapists need to accurately articulate and interpret clinical findings and use theoretical constructs to aid the decision-making process. |
|
Clarke, 2010 (2) UK |
Two SUs in northern England. |
Thirty-four team members (OTs, PTs, health care assistants, doctors, social workers, etc.). Eight patients. |
Interviews and participant observation. |
• People working on SUs had a positive attitude to stroke rehabilitation. • Rehabilitation on the SU was enhanced by teamwork and use of “Opportunistic dialogue”, an inclusive team culture and learning and working together. |
|
Cowdell & Garrett, 2003 (39) UK |
Rehabilitation ward in an acute hospital with 12 stroke beds on 24 bed ward. |
Seven stroke patients. |
Interviews. Grounded theory approach. Sampling not clearly described, other than “purposeful sampling”. |
• Participants discussed feeling bored and wanting to engage in recreational activity as a purposeful, rehabilitative tool. • Authors suggested a need to reduce demarcation between medicine, nursing, PT and OT and create a culture in which the whole inpatient experience embraces rehabilitation. |
|
Daniels et al., 2002 (43) The Netherlands and Belgium |
OTs working in rehabilitation units/rehabilitation centres. |
Thirteen OTs with at least 3 years of experience of inpatient stroke rehabilitation. |
Focus groups using a case example for discussion. |
• OTs experienced dilemmas: • Focussing on adaptation while the person is focused on recovery. • Being client-centred and protective simultaneously. • Setting meaningful goals in an institutional context. |
|
Table II. Contd. |
||||
|
Reference and country |
Setting |
Participants |
Methods |
Relevant findings |
|
DeJong et al., 2004 (64) USA and New Zealand |
Seven sites in USA, one in New Zealand. Part of the Stroke Rehabilitation Outcome study. |
1,400 stroke survivors (200 in each site). |
Clinical practice improvement method. A standard form for recording therapy intervention was developed. Clinical specialists, physicians, OTs, PTs, SLTs, psychologists, nurses, social workers and rehabilitation therapists conducted conference calls to discuss which interventions to include. The form was piloted for 1 month with stroke patients. |
• A taxonomy of rehabilitation interventions was developed. This included neuromuscular interventions, functional activities, cardiopulmonary interventions, cognitive/perceptual sensory interventions, education, musculoskeletal interventions, patient assessment, and equipment related activities. This was intended to be applicable to OT, PT and SLT interventions. |
|
Eames et al., 2010 (50) Australia |
Major metropolitan hospital acute SU |
Thirty-four patients and 18 carers. |
Semi-structured interviews, prior to discharge and 3 months later. |
• Barriers to accessing information were reported by patients. These included limited availability and suitability of information, continuity of care and communication in the SU, and lack of time and resources in the hospital environment. Patient and carer factors, such as memory problems, were also noted. |
|
Edmans, 2001 (47) UK |
Conventional wards and SU in 1 hospital. |
No mention of participants. The philosophies, policies and procedures of the wards were observed. |
Observational study comparing SU with conventional ward. Sampling and data collection not clearly described. |
• Pertinent difference between the policies, procedures and philosophies evident on an SU and conventional wards included having the multi-disciplinary team ward based, with all treatment being carried out on the ward, and improved communication and interaction between different disciplines on the SU. |
|
Galvin et al., 2009 (49) Ireland |
Two SUs. |
Ten people with stroke (interviewed) and 10 senior PTS (focus groups). |
Interviews and focus groups. |
• PTs and patients agreed that more PT would be beneficial, but patients thought it was needed in SUs and PTs thought it would be most beneficial on discharge. • Increased family involvement in rehabilitation recommended. • Characteristics desirable in a PT were identified by patients. |
|
Galvin et al., 2009 (60) Ireland |
Acute inpatient stroke rehabilitation. |
Mixed methods. Qualitative method: 10 PTs working in stroke rehabilitation. |
Mixed methods. Qualitative method: 2 focus groups. |
• PTs agreed patients could benefit from more physiotherapy, but this was depended of factors such as motivation, fatigue, medical complications and age. |
|
Higgins et al., 2005 (41) UK |
One London SU. |
Interviews with 29 participants (21 patients, 1 SLT, 2 nurses and 5 people working for the reading service). SU staff, readers and patients were observed. |
In-depth interviews and participant observation. |
• Formal therapy can be difficult and tiring for patients, but they can be bored when left with nothing to do. A reading service offered a break from boredom without the demands of therapy. • Some patients described feeling nobody had time for them on the SU. • People’s attitudes to therapy/recreation corresponded with their interpretation of therapeutic activity. Some interpret it as being aimed at a specific functional outcome; others perceive it as anything benefitting health or wellbeing in a broader sense. |
|
Horton et al., 2011 (52) UK |
Neuro-rehabilitation unit. |
Two patients with communication impairments following an acute stroke or head injury. Two OTs, 2 PTs, 2 SLTs. |
Discourse analysis after videoing 3 therapist sessions (OT, PT and SLT) for each patient. (Data presented formed part of a larger study). |
• Clinicians shared an ethos of a “right type” of therapy practice. • Instructional sequences were said to encourage patients to problem-solve, thereby promoting self-efficacy. • Therapeutic activity type was associated with different communication practices. Patients engaged in meaningful communication in sessions with a social and functional context. • Differences between different therapeutic activity type meant that patients were experiencing different levels of autonomy in sessions conducted across the week. • Harmonizing of the rehabilitation process was recommended, to improve consistency and quality of patient engagement. |
|
Table II. Contd. |
||||
|
Reference and country |
Setting |
Participants |
Methods |
Relevant findings |
|
Hubbard & Parsons, 2007 (42) Australia |
One SU. |
Two therapists (1 OT and 1 PT, both specialists in neurology). |
Mixed methods. Qualitative component used semi-structured interviews. |
• Therapists’ roles centred on initial investigations, discharge planning and creation of a hypothesis about a person’s outcome. • The institutional environment offered limited opportunities for participation. • Therapists conflicted between long-term functional frame of reference, but working in a short-term setting. |
|
Jones et al., 2008 (44) UK |
One Primary Care Trust and 3 acute hospital NHS Trusts. |
Reflection phase: 33 patients and 2 carers. Planning and Action phases: 130 service users, healthcare professionals, volunteers and researchers. 63 took part in workgroups. |
Action research. Reflection phase: Interviews and focus groups to identify service user experiences of stroke services. Planning and action phase: initial meeting followed by workgroups. |
• Priority areas for development included information provision, preparation for transfer of care and the integration of social and leisure activities. • In the SU patients appreciated being given “homework”, and many appreciated being given the opportunity to participate in rehabilitative activities, such as reading the newspaper and doing quizzes. |
|
Kilbride et al., 2011 (66) UK |
One SU in a London teaching hospital. |
Forty staff involved in service delivery including nurses, therapists, social worker, therapy assistants, healthcare assistants, managers, etc. |
Action research using: focus groups, fields notes, meeting minutes, interviews, National Sentinel Stroke Audit data. |
• Themes found to influence improvement were: building an interprofessional stroke team, developing practice-based knowledge and skills in stroke care, and creating an organizational climate for supporting improvement. |
|
Maclean et al., 2000 (37) UK |
One SU in an inner-city teaching hospital. |
Twenty-two patients (14 with “high motivation” and 8 with “low motivation”). |
Semi-structured interviews. |
• Patients considered to be highly motivated demonstrated a good understanding of rehabilitation and the roles of their therapists. The opposite was the case for patients considered to have “low motivation”. • Patients received mixed messages: e.g. therapists promoted independence in the gym and nurses discouraged this on the ward. • The ward was described as “depressingly unstimulating”. |
|
Maclean et al., 2002 (38) UK |
One SU in an inner-city teaching hospital. |
Thirty-two professionals, including PTs, OT, SLTs, nurses, doctors, psychologist, social worker. |
Semi-structured interviews. |
• Motivation was seen as an important determinant of rehabilitation outcome. • Professionals deemed patients to be motivated if they were proactive rather than passive, but boundaries were blurred. • Professionals felt they could influence motivation by building rapport and chatting with patients about their lives. |
|
Mold et al., 2006 (61) UK |
Two SUs and 3 boroughs associated with a stroke register. |
Forty-one professionals. (SU consultants, nurses, managers, SLTs, PTs, OTs, plus community SWs, SLTs, OTs and PTs). |
One to one focussed interviews. |
• Professionals reported that cognition, complex social issues and language/culture might negatively affect access to rehabilitation. • Not fitting the service as currently resourced was found to reduce access to specific components of care. |
|
Morris et al., 2007 (40) UK |
One SU and 2 stroke rehabilitation wards. |
Ten patients, 5 carers, 15 staff (SLT, psychologist, social worker, dieticians, PTs, OTs, nurses, healthcare assistants, doctors). |
Focus groups (patient group, carer group, 3 staff groups). |
• Patients and carers expressed a desire for more therapy and more activity due to feeling bored. • They also expressed a desire for individualized treatments and consideration of non-physical needs. • Team divisions and reduced availability of care prevented rehabilitation. Therapists expressed not feeling listened to or respected in the team. |
|
Table II. Contd. |
||||
|
Reference and country |
Setting |
Participants |
Methods |
Relevant findings |
|
Pound & Ebrahim, 2000 (48) UK |
One SU, 1 elderly care unit and 1 general medical ward across 2 different hospitals. |
Not specified. Observation was conducted on each ward and involving all staff. |
Non-participant observation. Sampling not clearly reported. |
• Nurses on the elderly care unit were better at having a rehabilitative approach than those on the SU. • The extent to which nurses and therapists worked together in a mutually respectful and supportive way also varied across the sites. |
|
Suddick & De Souza, 2006 (56) UK |
OTs and PTS on an SU, community team and a neuro-rehabilitation centre. |
Ten therapists (5 OTs and 5 PTs from 3 teams). |
Interviews. |
• Experiences and perceptions of teamwork varied across teams and individuals. • Different opinions were reported regarding who benefits from teamwork: patient, service or team. • The patient and their family were not generally considered to be part of the team. • Informal liaison was seen as important by therapists. |
|
Suddick & De Souza, 2007 (58) UK |
Three teams: 1 neuro-rehabilitation centre, 1 community neuro-rehabilitation team and 1 SU. |
Ten therapists: 5 OTs and 5 PTs. |
Interviews. |
• Effective and ineffective teamwork was perceived to impact on the team, patient, individual team members, and service. • Factors contributing to the quality of teamwork included shared and collaborative working practices, communication, team members’ characteristics, and specific organizational structures. |
|
Talvitie & Reunanen, 2006 (51) Finland |
One hospital, 1 rehabilitation centre, 3 health centres and 1 private clinic. |
Ten PTs working with stroke patients in 9 treatment sessions. |
Discourse analysis from video recorded sessions. |
• PTs were found to have an authoritarian use of power in therapy sessions with patients. • They did not discuss goals with the patients, but related therapy to physical impairments. |
|
Von Koch et al., 1998 (55) Sweden |
One SU and 1 community team. |
Three patients and 2 therapists (profession not specified). (1 patient was receiving community rehabilitation; 2 were inpatients). |
Case study: participant observation, interviews and documents. |
• Inpatients did not assume roles other than “patient”, “layman” or “student”. Community patients and therapists utilized an expanded role set including “guest/host” and “friend”. In the community a patient could be the “teacher” and “expert”, and could shift between roles with a more equal and flexible power dynamic noted. |
|
SU: Stroke Unit; UK: United Kingdom; USA: United States of America; PT: physiotherapist; OT: occupational therapist; SLT: speech and language therapist; SW: social worker; PCT: Primary Care Trust. |
||||
Preliminary synthesis
Factors shaping delivery were organized into 6 themes, as described below.
Need for a therapeutic environment. Therapy was typically delivered in isolated sessions, and it was noted that there was a lack of therapeutic activity for patients outside of these sessions. Five studies reported that inpatients felt bored and isolated for most of the day (37–41). Therapists reported that the inpatient setting offered limited opportunities for people to explore their abilities and disabilities, compared with the home environment (42, 43). Therapists in one stroke unit described the environment as stultifying and institutionalizing (38). They suggested that a stimulating ward environment incorporating shared meals, group sessions and a well-maintained day room would help to motivate patients. Patients who did engage in recreational activities on the ward found them purposeful and related to recovery, encompassing physical, psychological and educational elements (39, 44). Authors concluded that, in order to embrace a rehabilitative culture, therapists should work collectively with medical staff and nurses to integrate recreational activities into care plans and rehabilitation programmes (2, 45–48).
Therapeutic approaches. Therapy delivery was shaped by the theoretical approach to rehabilitation taken by therapists, as this could influence the activity, environment and interaction styles utilized (43, 45, 46, 49–52). Cavanaugh & Schenkman (46) suggested that therapists are required to know, understand and analyse underlying contributions to each individual’s functional limitations, and to apply theoretical constructs to complex decision-making processes. A treatment approach might alter due to analysis of specific impairments (such as reduced attention and poor safety awareness) and social or environmental elements (such as levels of motivation and family support) (46). OTs and PTs were noted to have different theoretical approaches despite role overlap (45).
Three studies found that patients desired an individualized focus on their wider, non-physical needs and measured recovery in terms of fully regaining their former identity, whilst therapists focussed on impairments and specific functional abilities (40, 53, 54). However, another study noted that rather than there being a clear-cut dissonance between the attitudes of therapists and patients, individuals from both groups varied in their expectations of “therapeutic activity” (41). This study also suggested that the types of activities that patients or staff considered worthwhile related to whether they adopted an impairment-focussed or holistic approach to therapeutic activity (50).
Power and decision-making. Power was identified as a theme from 8 studies, and included power exercised by therapists in therapy delivery; therapists’ role in determining the level of autonomy granted to patients over their decisions and actions; and the potential of therapy delivery to be empowering or disempowering to patients (43, 51–57). Discourse analysis of OT, PT and SLT sessions demonstrated that therapists use specific interaction strategies to encourage patients to problem-solve and promote self-efficacy, and that chosen strategies and activities lead to different levels of patient autonomy (51, 52). Both studies found that therapists placed importance on patients performing movements or tasks in the “right way” in order to be therapeutic or safe. In one study (51), this was interpreted as an authoritarian use of power by physiotherapists.
Three studies explored the power imbalance observed between patients and therapists, finding patients had a passive approach, whilst therapists took the role of experts who would decide what training should be done, when and for how long (51, 53, 55). Inpatient therapists were observed to be more likely to take the role of “expert”, and were less holistic and empowering in their approach to therapy delivery than community therapists (64). Four studies suggested patients should be empowered in planning and validating their rehabilitation, and that attention should be paid to psychological and social aspects of patients’ lives (51, 53–55).
Two studies noted that striving for a consistently person-centred approach to therapy delivery was problematic (43, 58). OTs discussed sometimes having a different perspective from patients regarding their rehabilitation needs, or feeling uncomfortable about informing patients about a change in their therapeutic approach (from remedial to adaptive) if it signified a loss of hope in their potential for recovery (43). Impaired insight could contribute to the dissonance in patient/therapist attitudes regarding appropriate therapy, and was seen as a reason to constrain autonomy. Three studies involving interviews or observation of therapists suggested that the extent to which patients are involved in decision-making is in the hands of professionals, and patients with questionable insight, cognition or social capital are unlikely to be granted autonomy (43, 57, 58).
Intensity, motivation and appropriateness for therapy. Ten studies explored patients’, carers’ or therapists’ views regarding allocation of face to face therapy time (37, 38, 41–43, 49, 57, 59–61). Therapists in a focus group study agreed that they select the type, duration and intensity of therapy that each patient should receive on a daily basis, and that stage of recovery, equipment and availability of space influenced the type of therapy delivered (59). Patients considered most appropriate for intensive rehabilitation included those with a borderline prognosis regarding whether they would be able to return to independent living, those who were younger, and those considered to be motivated (42, 60). For those with a clear prognosis therapists would focus on facilitating discharge (42).
Barriers to rehabilitation were found to include cognitive impairments, medical complications, social issues, language/culture and fatigue (60, 61). Mold et al. (61) discussed the role professionals have in matching patients to available resources, concluding that decisions are based on notions of clinical benefit, resource management and moral evaluations. Allen et al. (57) also noted that treatment may be revised to fit with service availability. The individual or their family’s ability to “work the system” was considered to influence team decisions. Therapists interviewed in 1 study reported believing that patients deserved equal encouragement, yet also reported being less likely to “push” unmotivated elderly patients than younger ones (38). Four studies reported that therapy work incorporated imparting information and encouraging motivation (37, 38, 41, 50).
There was no clear consensus regarding the intensity of preferred therapy. Galvin et al. (49) found that, whilst patients felt they needed more physiotherapy during their inpatient stay, physiotherapists suggested this would be more beneficial on discharge from hospital. It was noted that repetitive practice of activities or exercises could be facilitated by increasing family involvement (49). Some patients reportedly felt overwhelmed or over-worked due to the intensity of therapy sessions provided in hospital, such as 1 patient who stated that he could not keep up with the pace of “physio, physio, physio” but benefitted from engaging in recreation (41, p. 1395). Therefore, an expression of boredom and inactivity may need to be made distinct from a call for more active therapy, which may be demanding and tiring, and in some cases may not be considered beneficial.
Therapy work behind the scenes. Eleven studies discussed aspects of therapists’ work completed away from the patient (42–45, 57, 59, 60, 62–65). Some therapists perceived their role as primarily to assess patients, formulate prognoses about their potential for recovery, and use these to inform management plans (42, 43). This included preparing for discharge and making decisions regarding rehabilitation needs (42, 43, 49, 57).
Discharge planning was highlighted as a significant therapy role in 4 studies (42, 57, 62, 65). This took up a greater proportion of therapy work in socio-economically deprived areas, as individuals were likely to be more dependent on the multi-disciplinary team to make arrangements to enable them to leave hospital (57).
Assessment and administration to facilitate discharge from hospital appeared likely to take priority over “hands on” therapy (42, 65). Being involved in a well-coordinated discharge planning process was found to be important to carers and patients in one study: some expressed having difficult experiences due to poorly planned discharges; others appreciated experiencing a well-planned discharge (44). However, therapists differed in their attitudes regarding the short-term nature of their input and the time spent discharge planning. Some noted that getting home was in the interests of patients concerned, as well as being essential to make space for new admissions to the hospital who would be in more need of the resources in the inpatient setting (43). Others were concerned that the institutional goal, of ensuring patients could manage the basic functions necessary to return home, competed with professional goals such as considering patients’ long-term aspirations (42).
Role of teamwork in creating a therapeutic environment. Sixteen of the included studies highlighted the significance of teamwork, including communication and collaborative relationships between professionals, and practices such as multidisciplinary meetings (2, 37, 40, 44–48, 50, 52, 56, 58, 59, 62, 63, 66). Studies found that when delivery of therapy involved collaboration between staff, a more rehabilitative environment was promoted. Interdisciplinary teamwork with flexible role boundaries was found to be important, with positive and negative examples presented in different studies (45, 59, 62). Teamwork was frequently found to lead to a more supportive environment with better sharing of information, allegiance to a rehabilitation model, shared decision-making and problem-solving and more timely implementation of processes (2, 45–47, 56, 58, 63, 66). Information sharing amongst professionals was considered crucial to ensure consistent and appropriate management of the patient, such as ensuring that nurses were aware of SLT recommendations about the consistency of food that a patient could safely swallow (44, 50).
Therapists spending time on the ward (rather than delivering therapy off the ward) was said to promote respect and understanding of roles within the team (2, 47, 66). Studies gave examples of nurses and therapists working together to reposition patients or problem-solve the best way for them to get out of bed, finding this created opportunities to ask each other questions as well as leading to consistent practice on the ward. Unplanned and informal interaction was found to enable sharing of information, mutual learning and collaborative decision-making (2, 56).
Five studies found that an absence of collaboration negatively impacted on therapy delivery (37, 40, 44, 50, 52). Patients found “mixed messages” given by therapists and nursing staff discouraging and demotivating, and divisions between therapists, nursing staff and doctors were found to result in less therapy (37, 44). The reasons for this included patients not being washed and ready for therapy sessions and a lack of carry-over of therapy recommendations on the ward by nursing staff. It was claimed that therapists could do better at reinforcing their recommendations and therapeutic strategies to ensure these were incorporated into ward routines, thereby improving the consistency and quality of rehabilitation (50, 52).
However, teamwork practices were noted to be time-consuming and lead to a dilemma about whether to prioritize patient contact time or teamwork time, such as meetings (63). There was no evidence in the included studies to suggest how time should be distributed between teamwork practices and patient contact.
Exploring relationships in the data
Structure and process were considered relevant as a starting point, but further analysis and interpretation of the preliminary findings led to the identification of factors that did not fit into these categories.
The secondary level of synthesis suggested that delivery of rehabilitation was affected by 3 factors that mediated the delivery of therapy. These were conceptual, individual and professional factors. Fig. 2 shows how the preliminary themes related to factors identified in the secondary level of synthesis.
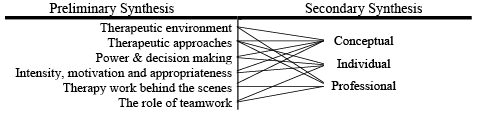
Fig. 2. Relationship between themes identified in preliminary synthesis and higher level factors identified in secondary synthesis.
Conceptual factors. Throughout the review we found ambiguities in key terms, such as “therapy”, “therapeutic activity” and “rehabilitation”. This lack of clear definition was a hidden factor affecting therapy delivery in its own right. “Therapy” was something done by therapists, but there was inconsistency about whether this term encompassed non-clinical aspects of their work, (such as administration, meetings and decision-making), or patient assessment and education. “Rehabilitation” and “therapy” could be used interchangeably, but “rehabilitation” could also be defined as an ethos that should be promoted by all members of the team, and not confined to isolated therapy sessions. Different interpretations of “therapeutic activity” highlighted that individuals hold different conceptualizations, which are likely to influence their expectations and willingness to engage in different types of therapeutic activity. These conceptualizations also relate to the model or approach adopted, for example, some patients and staff believed that “therapeutic activity” should target a specific impairment, whilst others defined it as any activity considered to improve wellbeing. This demonstrates that different underlying assumptions about what therapy should be are not ascribable to different groups (e.g. professionals or patients), but vary amongst all involved. This implicit lack of consensus is likely to underpin variation in therapy delivery, as well as rendering intensity measurement problematic.
Individual factors. Linked with this lack of consensus, we attended to the extent to which therapy delivery was shaped by individual variation on the part of therapists and patients. Whilst some studies reported that therapists select interaction styles, environments and activities that would offer opportunities for empowerment of the individual, other studies reported that therapists focussed on instructing patients in the correct performance of movements or tasks, perpetuating notions of expert therapists and passive patients. These differences across different studies suggest that delivery of therapy is shaped by the individual delivering it. Experiences and opinions regarding therapy provision were individualized. The manner in which information was provided was important to patients and families, and patients valued the individual characteristics of therapists who encouraged and motivated them through their use of communication and personality.
Individual factors, including social capital, age, previous lifestyle, cognitive ability, language and culture, influenced patients’ access to resources. Delivery of therapy therefore appears to be shaped by individual therapists, and is influenced by the characteristics of individual patients and their families.
Professional factors. Several areas of tension in relation to therapists’ fulfilment of their professional roles were noted. Core professional values, such as being holistic, person-centred and addressing patients’ long-term aspirational goals, were undermined by the short-term aims of the institution (e.g. reducing length of stay) and the restrictions of the environment. A primary aim of therapists presented in many studies was to facilitate timely discharge in order to meet the institutional goal of reducing length of admission. This involved assessment, prognosticating and discharge planning. Addressing complex social issues was presented as part of the team’s skillset. Due to the organizational goal of minimizing length of stay, “face to face” therapy was targeted at ensuring that patients could do the minimum necessary to be discharged. Patients with complex social or discharge planning needs were likely to require more “behind the scenes” time, and either require or receive less “face to face” therapy time. No study in the sythnesis suggested how conflicting demands should be prioritized. This is likely to reflect dilemmas and tensions in the delivery of therapy in practice.
Discussion
This systematic review and narrative synthesis was conducted against a backdrop of multiple quantitative studies and audits seeking to measure therapy activity, and concerns regarding failure to deliver therapy to intensity targets. We anticipated that synthesizing the qualitative literature would enable identification of structural and process factors shaping delivery, and improve understanding of contextual factors affecting allocation of therapists’ time. Themes identified in the preliminary analysis were the need for a therapeutic environment; therapeutic approaches; power and decision-making; therapy work behind the scenes; and the role of teamwork in creating a therapeutic environment. We believe these will enhance understanding of “what goes on” in therapy delivery. Moving beyond description to analysis and interpretation, the secondary level of synthesis identified that delivery is mediated by differing conceptions of the nature of therapy and the role of therapists, as well as individual and professional responses to opportunities and constraints of therapy delivery. We believe that the identification of these factors and their influence on therapy delivery is a new contribution to the literature.
Use of an established narrative synthesis framework increased the robustness and trustworthiness of the review (27), and an audit trail of search strategies and results was kept by ET and checked by CM and FJ. Initial database searches cast a wide net, and 5,711 titles were screened. Studies included in the final review were considered to be of the greatest relevance to the review question. Difficulties in judging whether studies met the selection criteria occasionally arose due to lack of clarity regarding the study settings. Having begun with the intention of exploring therapy on stroke units, it became apparent that looking more broadly at acute inpatient stroke therapy would be more feasible, as it was often not possible to distinguish whether a study had taken place in a designated stroke unit or other inpatient settings involving stroke patients. More than half of the studies were based in the UK, therefore our findings may be more likely to reflect UK therapy practice; nevertheless, common themes were identified from studies based in a range of countries. The analysis and synthesis of themes is inevitably subjective. The involvement of co-authors was intended to reduce this limitation. A possible criticism of the review is that quality appraisal was not used to exclude papers. Whilst recognizing the limitations of some of the included studies, as a body of work they represent an important step in developing understanding of the factors that underpin and shape delivery of inpatient stroke therapy.
In synthesizing the data and the relationships between studies, we found that therapy delivery was shaped by conceptual, individual and professional factors. We highlighted a lack of consensus regarding how inpatient stroke therapy or rehabilitation should be defined, tensions between professional ideals and institutional objectives, and variation in individual approaches and expectations.
We noted an absence of agreement regarding how therapists’ time should be divided between their various roles, or whether they are all equally important. Therapists were found to decide how to allocate their time amongst their patients on an individual basis, and may be influenced by factors such as the patient’s age, cognition, language and social context. Quantitative evidence suggest that stroke units with more restrictive admission criteria (e.g. excluding patients based on age, pre-morbid functional disability, or the presence of a social network or support at home) may deliver more hands-on therapy (67). Therefore, the relationship between case mix and use of therapy time may be worthy of exploration.
The significance of individual approaches and attributes of therapists is consistent with other studies that found that personal attributes of therapists were more important to patients than the quantity of therapy received (69, 70). Beyond this, we found that individual factors influenced the use of power in therapeutic relationships as well as the allocation of therapy among patients. It has been argued that healthcare settings incorporate complex and contingent power dynamics (68). Our findings suggest that the individual values and choices of therapists should be attended to as part of this complexity.
Conceptual assumptions regarding the purpose and nature of therapy underpin its delivery, yet in the absence of these assumptions being expressed, explored and debated it will be difficult to establish a consensus among patients, professionals and policy-makers about what should be delivered, and how. Agreed definition of fundamental concepts is needed in order to promote inpatient stroke therapy objectives that are shared, or at least understood, by all stakeholders.
Promoting increased inpatient rehabilitation may require a re-conceptualization of rehabilitation that is not restricted to temporally and spatially isolated therapy sessions. This would call for investigation of the feasibility, desirability and effectiveness of novel models of rehabilitation on stroke units. Further research is also needed to examine how therapists negotiate the different and sometimes conflicting factors shaping delivery of therapy. This includes understanding how they prioritize their time; how they reconcile potentially conflicting therapeutic approaches; how they negotiate issues relating to power and decision-making; and how they make decisions regarding intensity of rehabilitation delivery for patients in their care.
Acknowledgements
CM acknowledges the support of the NIHR Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. ET is supported by a grant from the Stanley Thomas Johnson Foundation.
References
