Emmanuel Aboagye, MSc, Malin Lohela Karlsson, PhD, Jan Hagberg, PhD and Irene Jensen, PhD
From the Intervention and Implementation Research Unit, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden
OBJECTIVE: To evaluate the cost-effectiveness of medical yoga as an early intervention compared with evidence-based exercise therapy and self-care advice for non-specific low back pain.
DESIGN: Randomized controlled trial with a cost-effectiveness analysis.
SUBJECTS: A total of 159 participants randomized into the medical yoga group (n = 52), the exercise therapy group (n = 52) and the self-care advice group (n = 55).
METHODS: The health outcome measure EQ-5D was applied to measure quality of life data combined with cost data collected from treatment groups from baseline to 12 months follow-up. Outcome measure was health-related quality of life (HRQL). Incremental cost per quality adjusted life year (QALY) was also calculated. Cost-effectiveness analysis was conducted primarily from the societal and employer perspectives.
RESULTS: Medical yoga is cost-effective compared with self-care advice if an employer considers the significant improvement in the HRQL of an employee with low back pain justifies the additional cost of treatment (i.e. in this study EUR 150). From a societal perspective, medical yoga is a cost-effective treatment compared with exercise therapy and self-care advice if an additional QALY is worth EUR 11,500. Sensitivity analysis suggests that medical yoga is more cost-effective than its alternatives.
CONCLUSION: Six weeks of uninterrupted medical yoga therapy is a cost-effective early intervention for non-specific low back pain, when treatment recommendations are adhered to.
Key words: medical yoga; low back pain; cost-effectiveness analysis; occupational health services.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Malin Lohela Karlsson, Karolinska Institutet, Intervention and Implementation Research Unit, Nobels väg 13, Solna, Box 210, SE-171 77 Stockholm, Sweden. E-mail: malin.lohela.karlsson@ki.se
Accepted Aug 27, 2014; Epub ahead of print Nov 14, 2014
Introduction
Low back pain (LBP) has been described as a recurring condition and a costly public health problem (1, 2). It is one of the most common reasons why working adults take days off work or become disabled (3). Thus the cost, both economic and human, of LBP can be high if the appropriate early treatment is not sought (4).
There are a variety of therapies for managing LBP, but there is limited knowledge about their effectiveness with regards to improvement in health-related quality of life (HRQL). Exercise therapy is one of the commonly used interventions for managing LBP as an alternative to usual care (i.e. evidence-based advice). Exercise therapy can encompass many types of interventions with regards to method and design (5). However, it has been shown that supervised exercise therapy, including individually designed stretching or strengthening, have positive effects on pain and back function in people with non-specific LBP (6).
Some complementary and alternative medicine (CAM) therapies have been used for LBP (7, 8). Yoga can also be used, mainly for pain management (9). In addition to its suitability for a number of conditions, medical yoga has been shown to alter the experience of pain and to have positive and sustainable effects on back function (9). However, screening generally precedes treatment with medical yoga, so that training and physical posture instructions can be individually designed.
The significant outcomes in studies that have evaluated the effectiveness of yoga for managing LBP include: reduced pain intensity and greater improvement in physical and functional disabilities (10, 11). However, there has been little research into improvement in HRQL from early treatment and the cost-effectiveness of yoga for LBP. In a multicentre randomized control trial, yoga compared with usual care was shown to improve quality of life and be cost-effective among patients with chronic LBP (12). It is therefore imperative to conduct studies on the effects and cost-effectiveness of medical yoga therapy as an early preventive intervention for LBP.
Aim
To evaluate the cost-effectiveness of medical yoga as an early intervention for managing LBP compared with 2 evidence-based interventions; exercise therapy and self-care advice.
Hypotheses
Our first hypothesis was that medical yoga will improve HRQL more than exercise therapy and self-care advice, and, secondly, that medical yoga is more cost-effective than either exercise therapy or self-care advice.
Methods
The study was a single-blinded randomized control trial with a 12-month follow-up that compared medical yoga with exercise therapy and self-care advice. The participants were randomized to 1 of 3 interventions after undergoing an initial medical examination to screen for comorbidities and serious illnesses. The examination was performed by back specialists. A block randomization was utilized using the pre-randomization technique and participants were picked consecutively by a research assistant. After randomization, the back specialist met with the participants and gave them background information about the intervention they were being offered. Previous studies (13) have shown that expectations of treatment and response levels differ depending on, whether the treatment is physically or psychologically oriented. Therefore, the 2 training interventions (yoga and exercise therapies) were both presented as well-established training therapies, to improve the level of participation and to equalize the participants’ expectations of the treatment and its outcomes. During the assignment of study participants to intervention groups, assessors (those collecting outcome data) were blinded to group allocation and the patients were blinded with respect to other intervention options. All researchers analysing the results were blinded to group allocation until the analyses were complete and the manuscript had been written.
Interventions
Medical yoga was a Kundalini-based standardized programme performed in groups, twice a week for 6 weeks and led by an experienced medical yoga instructor. Participants received a CD with instructions, and written information about the programme, and were encouraged to perform the programme as often as possible between the medical yoga sessions. After 6 weeks, the participants were to carry on practicing medical yoga no less twice per week.
Exercise therapy was a 6-week individual, standardized strength training programme followed up by an experienced physiotherapist in groups once every second week. In the first week of intervention start, the participants and the physiotherapist met twice in order to individually design the training programme. Participants were followed-up after 2, 4 and 6 weeks. Subsequently, participants were to continue practicing the exercise therapy programme at least twice per week.
In the evidenced based self-care advice group, individuals received brief oral recommendation from a back specialist to stay active and a booklet containing self-care advice. Brief advice to staying active has been shown to have positive effects on pain and improvement in physical function among individuals with LBP (14).
Ethical considerations
All 3 groups received treatment based on ethical grounds. The study was approved by the Regional Ethics Committee (2010/108-31/3) and registered in the clinicaltrials.gov protocol registration system (NCT01653782).
Data collection
Participants were recruited through the Occupational Health Services (OHS) and by advertisement in the local media in Sweden’s Stockholm County. People of working age with neck/back pain were invited to apply for participation in the study. Then, a screening questionnaire was posted to those who responded to the invitation to participate in the study. Those who scored 90 points or more, i.e. fulfilling the requirements for psychosocial risk profile, on the Örebro Musculoskeletal Pain Screening Questionnaire (OMPSQ) (15) were invited for further physical examination.
Inclusion criteria were: having non-specific LBP; age range 18–60 years; having scored 90 points or more on the OMPSQ screening questionnaire; and having a sufficient command of Swedish. Exclusion criteria were: pregnancy; comorbidities that could affect the ability to perform exercise; ongoing regular weekly yoga practice or strength training; and ongoing sickness absences of 8 weeks or more.
Of the total of 310 people who responded to the OMPSQ screening questionnaire, 138 were excluded because they scored less than 90 points (Fig. 1). The 172 subjects who remained were assessed for eligibility and 13 were excluded at the enrolment stage for not fulfilling the inclusion criteria. The remaining 159 participants who qualified for inclusion were randomized to 1 of the 3 treatment groups, resulting in 52 in the medical yoga group, 52 in the exercise therapy group and 55 in the self-care advice group that were included in the analysis.
Data on participants’ adherence to treatment, back pain and sickness absence were collected during the follow-up period via text messages sent out once a week for 6 weeks, and then once a month until the 12th month. Sickness absence was absence due to all types of illness.
Outcome measurement
The primary outcome was HRQL measured with EQ-5D at baseline and each follow-up (6 weeks, 6 months and 12 months). This instrument measures the individual’s health state on 5 scales: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The responses were weighted with the time trade-off method, which gives quality adjusted life year (QALY) values anchored between 0 and 1, where 1 is a year lived in full health and 0 (zero) represents death (16). The Danish tariff was used since there were no time trade-off estimates for the Swedish population (17).
Costs of intervention
The estimated costs were based on the number and type of activities in each treatment group, the amount of resources consumed and duration of use of resources. The cost in the medical yoga group included the cost of the yoga trainer, the cost of the materials used and physician assessment (screening) cost based on the primary care reference cost per visit by a physician. Costs associated with the exercise therapy included: the cost of physician assessment, the cost of the first visit to a physiotherapist and repeat visits, the cost of an exercise training activity based on the market price if the participant received physical activity on prescription, the back book and an exercise ball. The cost in the self-care advice group was based on physician assessment and self-care advice as well as the back book. The intervention costs were incurred regardless of the number of classes participants attended after allocation to a treatment group. Therefore, participants were assigned the same costs based on allocation to treatment group. All costs of resources were collected retrospectively. Discounting was not necessary as costs and consequences occurred within a year after recruiting participants (18). The total cost of resources used in the trial reflects 2011/2012 prices, since the follow-up period occurred within this interval.
Statistical and economic analysis
HRQL was estimated using regression analysis. In order to evaluate the intervention effect on HRQL, the utility were adjusted for baseline utility scores and the resulting coefficient for the treatment dummy was stated as the mean incremental QALY (19). The adjustment was important, since the baseline EQ-5D score tends to correlate with the follow-up scores of participants (19).
Interactional effects between the treatment groups and the number of days a participant trained were also considered, since our initial analysis showed that there was a strong interaction between treatment group and training frequency per week. A generalized linear model was used for dichotomous outcomes and a linear model for continuous outcomes to account for such strong interactional effects. For each number of training days, a unique difference between treatment groups was calculated with corresponding confidence intervals. Baseline age and mean number of training days were used as covariates in the model. The analyses were performed in SPSS version 20.
The costs in the intervention groups were derived by multiplying the length of time used in the assessment, the number of resources consumed and the total number of participants in one treatment group, and then summarized for each treatment group. The mean cost in each treatment group was used to calculate the mean incremental cost, i.e. the differences in the mean cost between medical yoga and its comparators.
The cost-effectiveness of the interventions was calculated as the incremental cost-effectiveness ratio (ICER) and estimated using mean incremental cost and the adjusted mean incremental QALY. The analysis was conducted from the societal perspective. The societal perspective included all costs associated with the intervention and production loss as a result of sickness absence. Production losses resulting from sickness absences were estimated as the mean hourly earnings of the employee multiplied by the number of days off work. In addition to the hourly earnings (20), additional compensation-holiday allowances (13%), labour (31.42%) and pension contributions (10%) paid on top of employee earnings were included. These payments in themselves will not represent any additional consumption of resources from the standpoint of society. However, these earnings are included as costs to society only as a proxy of lost productivity, i.e. reduced work production due to sickness absences. The analysis was also performed from the employer’s perspective including the intervention costs.
Since uncertainty can arise about the use of, for instance, negative ICER in a cost-effectiveness analysis for decision-making (18). Incremental net benefit (INB) was also estimated. The INB is a linear expression of the cost-effectiveness decision rule that can trace the net benefits of the intervention after accounting for the additional cost of implementing an intervention. The INB was estimated by multiplying the adjusted incremental QALY by the willingness to pay less the mean incremental cost (18). The INB provides evidence that an intervention is cost-effective if the net benefit is greater than zero (21). The willingness to pay value assumed was EUR 11,500, equivalent to SEK 100,000 per QALY, which is the lower limit consistent with the recommendations of the Swedish National Board of Health and Welfare for a cost-effective intervention (22).
Sensitivity analysis of the economic evaluation
The sensitivity analysis focused on the productivity losses that resulted from sickness absences. The cost of lost production is estimated by multiplying the daily wage rate by the number of absent days (18). However, extant research suggests that this conventional approach may underestimate the true cost of lost production from sickness absence (23). Therefore, in estimating the cost of absenteeism, the difficulty of finding a perfect substitute for the absent worker, the role of the absent employee in teamwork, and the time-sensitivity of employees’ output should be taken into consideration. One-way sensitivity analysis was used to estimate the total absenteeism cost by multiplying number of days off work by the median multiplier 1.28 times the mean daily wage rate (23). The median multiplier was used because of the nature and diversity of jobs that participants were engaged in at the beginning of the study.
Results
Description of participants at baseline
The total number of participants was 159 (Fig. 1) and the response rate for the 3 follow-up periods after the baseline assessment was 89% for medical yoga, 69% for exercise therapy and 63% for self-care advice. All participants were of working age and were at the beginning of the study working and not on sick leave. The proportion of women differed somewhat between the groups (Table I). The mean age was 47 years in the medical yoga group, 46 years in exercise therapy and 44 years in the self-care advice group.
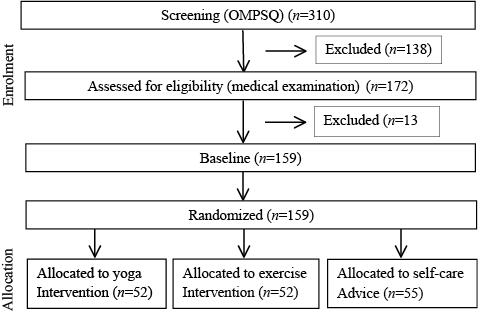
Fig. 1. Flowchart of participant selection process. OMPSQ: Örebro Musculoskeletal Pain Screening Questionnaire.
|
Table I. Description of study participants |
|||
|
Variables |
Yoga (n = 52) |
Exercise (n = 52) |
Advice (n = 55) |
|
Sex, female, n (%) |
37 (71.7) |
32 (61.5) |
44 (80) |
|
Age, years, mean (SD) |
46.9 (9.6) |
46.3 (9.3) |
43.9 (11.7) |
|
Education, n (%) |
|||
|
Elementary/junior high |
25 (47) |
29 (55.8) |
32 (58.1) |
|
Higher education |
27 (51) |
23 (44.2) |
21 (36.8) |
|
Lived in Sweden, n (%) |
|||
|
Always |
37 (69.8) |
38 (73) |
35 (63.6) |
|
< 5 years |
2 (3.8) |
1 (1.9) |
1 (1.8) |
|
> 5 years |
50 (96.2) |
51 (98.1) |
52 (94.5) |
|
Additional pain sites, n (%) |
|||
|
Neck pain |
34 (64) |
34 (65) |
36 (63.2) |
|
Upper back pain |
27 (51) |
28 (54) |
26 (45.6) |
Outcome of the intervention
Descriptive data on overall HRQL and for the interaction term, i.e. training ≥ 2 times per week, are shown in Table II. Differences in HRQL between individuals adhering to treatment recommendation (i.e. training at least 2 times per week) and those who were not are shown. Participants in the exercise therapy and self-care advice groups had higher mean EQ-5D scores at baseline than did individuals in the medical yoga group. However, during each follow-up period individuals in the medical yoga group had higher mean scores than did those in the exercise therapy and self-care advice groups. Therefore, the baseline EQ-5D scores were used as a covariate for the adjustment.
|
Table II. Health outcome according to treatment adherence within treatment groups |
||||||||
|
|
Medical yoga (n = 52) |
Exercise therapy (n = 52) |
Self-care advice (n = 55) |
|||||
|
< 2 times/week |
≥ 2 times/week |
< 2 times/week |
≥ 2 times/week |
< 2 times/week |
≥ 2 times/week |
|||
|
HRQL, mean (SD) |
||||||||
|
Baseline |
0.72 (0.20) |
0.71 (0.20) |
0.76 (0.14) |
0.74 (0.17) |
0.70 (0.20) |
0.73 (0.22) |
||
|
6 weeks |
0.64 (0.31) |
0.80 (0.11) |
0.81 (0.08) |
0.78 (0.16) |
0.74 (0.11) |
0.70 (0.22) |
||
|
6 months |
0.77 (0.17) |
0.77 (0.15) |
0.81 (0.08) |
0.76 (0.21) |
0.72 (0.21) |
0.70 (0.28) |
||
|
12 months |
0.73 (0.21) |
0.79 (0.14) |
0.75 (0.16) |
0.79 (0.13) |
0.73 (0.15) |
0.75 (0.23) |
||
|
p-values < 2 times/week are 0.177 and 0.073 for comparing medical yoga with exercise therapy and self-care advice, respectively. p-values ≥ 2 times/week are 0.574 and 0.031 for comparing medical yoga with exercise therapy and self-care advice, respectively. HRQL: health-related quality of life; SD: standard deviation. |
||||||||
Statistical analyses revealed that medical yoga had a significant (p = 0.031) and better effect on HRQL than did evidence-based self-care advice, taking into account the interaction effect (i.e. training 2 times/week or more). The difference between medical yoga and exercise therapy was not significant (p = 0.574) even when controlling for the interaction effect. Thus our first hypothesis, which says medical yoga will improve HRQL more than will exercise therapy and self-care advice, is partly verified.
Cost analysis of interventions
The direct and indirect costs (i.e. production losses) of each intervention, are shown in Table III. The cost of resources used in each treatment group differed depending on the type of health personnel, the length of time used in assessing participants and the amount of resources used. In an OHS setting, the mean cost of combined preliminary assessment by a physician, other health personnel, and materials used, was estimated at EUR 255 for those who were offered medical yoga, EUR 461 for those in the exercise therapy group, and EUR 106 for those in the self-care advice group (Table III).
Table III presents the mean number of days of sickness absence at the 1-year follow-up, separated by the interaction break-point. For the overall group, the average participant in the medical yoga group reported 12.4 days (standard deviation (SD) 17.1) off work as a result of LBP during the 1-year period, whereas for the exercise therapy and self-care advice groups the sickness absence numbers were higher: 22.4 days (SD 41.6) and 29.6 days (SD 67.0), respectively.
|
Table III. Intervention costs by treatment group |
|||
|
Cost per intervention, EUR |
|||
|
Medical yoga (n = 52) |
Exercise (n = 52) |
Advice (n = 55) |
|
|
Cost items |
|||
|
Direct costs |
|||
|
Physician assessment |
3,588 |
3,588 |
3,795 |
|
Physician advice |
– |
– |
1,898 |
|
Yoga trainer |
9,568 |
– |
– |
|
Physiotherapists |
– |
19,061 |
– |
|
Material/equipment |
120 |
1,316 |
127 |
|
Total direct costa |
13,276 |
23,965 |
5,819 |
|
Mean direct cost |
255 |
461 |
106 |
|
Indirect cost |
|||
|
Cost of productivity lost |
84,591 |
152,907 |
214,529 |
|
Mean productivity lost |
1,627 |
2,941 |
3,900 |
|
Total societal costb |
97,867 |
176,872 |
220,348 |
|
Mean societal cost |
1,882 |
3,401 |
4,006 |
|
Sickness absence (days) after 1-year follow-up |
|||
|
Training days/week |
|||
|
< 2 times |
24 (19) |
31 (30) |
22 (43) |
|
≥ 2times |
9 (15) |
18 (50) |
52 (108) |
|
aTotal direct cost of intervention (i.e. cost of preliminary screening + treatment and material costs in Occupational Health Services setting). bTotal societal cost (i.e. total direct cost of intervention and cost of productivity lost) is from the societal perspective. We refer to minimum earnings per day of SEK 1,145 from Statistics Sweden, equivalent to EUR 132. Totals may not add up to the stated value due to rounding-off of figures. |
|||
The mean cost of productivity lost (Table III) from sickness absence was, EUR 1,627 in the medical yoga group, EUR 2,941 in the exercise therapy group and EUR 3,900 in the self-care advice group. This implies that the mean societal cost was EUR 1,519 and EUR 2,124 more in the exercise therapy and self-care advice groups, respectively, than the mean societal cost in the medical yoga group.
Cost-effectiveness of the intervention
Employer’s perspective. The cost-effectiveness of the interventions is shown in Table IV. From the employer perspective, medical yoga costs EUR 150 more than self-care advice, yielding an ICER of EUR 4,984 per QALY. This implies that medical yoga is more expensive than self-care advice, but is beneficial, if adherence to the recommendations is taken into account. Thus medical yoga can be considered cost-effective if an employer considers that the improvement in HRQL of an employee justifies the additional resources required for medical yoga treatment.
Again, medical yoga cost EUR 206 less than exercise therapy. However, the improvement in HRQL did not appear to be significantly better, which implies that both interventions result in equal improvement in HRQL. Medical yoga has an advantage over exercise therapy as the cost-effective alternative because it is associated with lower cost.
|
Table IV. Incremental cost effectiveness ratio (ICER) of medical yoga compared with exercise therapy and self-care advice |
||
|
Medical yoga vs self-care advice |
Employer’s perspective Mean (95% CI) |
Societal perspective Mean (95% CI) |
|
Incremental cost |
150 |
–2,124 |
|
Incremental QALY |
0.036 (–0.033; 0.11) |
0.036 (–0.033; 0.11) |
|
ICER (cost per QALY) |
4,984 |
Cost-effective |
|
Medical yoga vs exercise therapy |
||
|
Incremental cost |
–206 |
–1,519 |
|
Incremental QALY |
0.023 (–0.05; 0.073) |
0.023 (–0.05; 0.073) |
|
ICER (cost per QALY) |
Cost-effective |
Cost-effective |
|
Cost is in EUR. EQ-5D scores are adjusted for QALYs. ICERs indicated cost-effective yield negative incremental cost per individual. QALY: quality-adjusted life year; CI: confidence interval. |
||
Societal perspective
Considering the intervention cost and production losses to society due to sickness absence, medical yoga costs EUR 1,519 and EUR 2,124 less per individual, compared with exercise therapy and self-care advice, respectively. Medical yoga will be chosen compared with exercise therapy as a cost-effective alternative only in terms of cost. However, medical yoga is both beneficial with regards to improvement in HRQL and cost compared with self-care advice.
If it is assumed that a QALY is worth EUR 11,500, then medical yoga could be worthwhile from the societal perspective, with an INB of EUR 1,749 and EUR 2,469 compared with exercise therapy and self-care advice, respectively. The positive INB implies that medical yoga can be implemented over both interventions with regard to societal willingness to pay for the treatment. This confirms the second hypothesis that medical yoga is more cost-effective than both exercise therapy and self-care advice, from the societal perspective.
Sensitivity analysis
The cost-effectiveness result, including the estimation of the multiplier effect on production losses resulting from sickness absence, suggests that the incremental cost is largely sensitive to changes in cost of productivity. The analysis shows that it will cost EUR 1,887 and EUR 2,761 less per individual to treat LBP with medical yoga, compared with exercise therapy and self-care advice, respectively. Sensitivity analysis therefore indicates that medical yoga remains a cost-effective intervention compared with exercise therapy and self-care advice.
Discussion
This study shows that medical yoga is associated with greater health benefits and a greater improvement in HRQL compared with evidence-based self-care advice given by a back pain specialist. The results show that the improvement in HRQL was not statistically significant for the overall group, but when the frequency of training days was controlled for participants who trained 2 times or more per week, significant improvement in HRQL was found. Thus medical yoga seems to improve HRQL more than self-care advice, but not more than exercise therapy. The results emphasize the importance of adherence to treatment recommendations, in this case training a minimum of 2 times per week, and the relevance of accounting for adherence in the analysis when looking at the effects on HRQL. Differences between intervention groups are shown in the adherence rate. The differences may imply that motivation of subject in the interventions groups differed and/or their preference for type of training. It could also be that it is easier to adhere to medical yoga than to exercise intervention.
Cost-effectiveness analysis was performed on all subjects included in the trial (intention-to-treat analysis), accounting for the group effect of the intervention. From a societal perspective, medical yoga seemed to be the least costly treatment compared with both alternatives, exercise therapy and self-care advice. Thus, medical yoga is more likely to be cost-effective compared with exercise therapy and self-care advice from a societal perspective. The result also suggests that medical yoga can be a cost-effective treatment from the employer’s perspective, considering that the increase in the employee’s HRQL can translate into productivity benefits, thus justifying the additional resources required for medical yoga treatment implemented within the OHS setting.
As highlighted earlier in the analysis, the incremental cost of medical yoga is much lower than that of exercise therapy and self-care advice from a societal perspective. The observed cost savings are mainly due to differences in production loss, which was lower in the medical yoga group than in the other groups. This implies that the avoided production loss due to fewer sickness absence days in the medical yoga group balanced the cost of implementing the medical yoga. The cost of lost production could either be borne directly by the employer or by society, depending on, for example, the length of sickness absence, ability to replace the employee or whether the person is unemployed. Independently, the impact of production loss is highly relevant for decision-makers as presented here in the economic analysis. The cost of sickness absence used as a proxy measure of lost productivity illustrates the impact of counting the full value of societal costs. Again, it may have been relevant also to include the cost of production loss from an employer perspective. However, in this study we were not able to differentiate the cost of forgone production borne by the employer from the overall societal cost. Therefore, no reduction or increase in cost is included from this perspective.
In line with previous studies, we found that yoga therapies have positive effects for managing physical pain and functional disabilities related to LBP. The study’s analysis confirms that managing non-specific LBP with medical yoga gives positive effects, echoing the conclusions of previous studies (9–11, 24). This study differs from previous studies, however, in the sense that while previous studies on using yoga therapies for treating LBP included participants who had chronic LBP, the participants in this study had non-specific LBP that required early initiation of an intervention. Consequently, this study involved a more prevention-oriented intervention for people with LBP. This could also explain the modest improvements in HRQL after baseline adjustment to the EQ-5D scores.
The possibility of medical yoga being cost-effective is supported by the economic evaluation, as in previous studies (12). Although the estimation of incremental QALY gain was comparable with the findings of previous studies, the study also highlights, in the analysis, the effects of treatment on health if training recommendations are followed. The incremental costs of medical yoga intervention compared with exercise therapy and self-care advice were also considerably lower compared with previous studies. The lower costs may be explained by this study’s use of participants with non-specific LBP. It is worth mentioning that in previous studies different types of yoga were used for treating LBP, and that the subjects in those studies also included chronic LBP patients who may have required extensive treatments.
Study limitations
Although the analyses from a societal perspective included cost of productivity lost to sickness absences, the opportunity costs of time used during the yoga and exercise therapies were not included in the analysis. The rationale was that the opportunity costs of the lost productivity were expected to be less for both yoga and exercise therapy participants because training sessions were held on weekday evenings (25). Moreover, participation in this trial was voluntary, with participants (78%) reporting strong satisfaction with the treatment. This implies that participants incurred no appreciable opportunity costs (26).
The cost of medication and other private expenses to relieve back pain were not included in the analyses. This could affect the cost-effectiveness of the yoga intervention to which the study refers. However, the results based on the trial confirm outcomes in other studies. Moreover, other health and non-health benefits for the individual, employer and society in general (such as reduced healthcare utilization, reduced productivity loss of family caregivers, benefits of reduced pain and suffering) may offset these costs over the long term if treatment benefits of medical yoga are achieved. No side-effects were reported in all intervention groups with regards to treatment outcomes, which should have been considered as costs rather than benefits.
Conclusion
This study makes a contribution to research on early interventions for non-specific LBP. The study attaches importance to participant adherence to treatment and concludes that an early intervention for LBP using medical yoga can have far-reaching benefits for employees who show early signs of LBP. The study also highlights the main determinants of costs to the employer and to society associated with treating LBP with medical yoga. In summary, the result of this economic evaluation supports the use of medical yoga as an early intervention for treating LBP in an OHS setting. From a decision-making standpoint, the treatment choice to which a decision-maker can channel resources is medical yoga, which is associated with better improvement in HRQL and positive incremental net benefits. The health gains from medical yoga are also cost-efficient from the societal perspective, albeit marginally compared with exercise therapy and self-care advice. Based on these results, if all 3 interventions are constrained by resources, medical yoga treatment is the optimal choice.
Acknowledgements
The authors gratefully acknowledge the assistance of FORTE, the Swedish research council for health, working life and welfare, for funding the study.
The authors have no conflict of interest to declare.
References
