Nicolas Roche, MD, PhD1, Raphaël Zory, PhD1,3, Antoine Sauthier1, Celine Bonnyaud, PhD1,2, Didier Pradon, PhD1,2 and Djamel Bensmail, MD, PhD1,2
From the 1The group of clinical and technological research on motor disabilities (EA 4497), CIC-IT 805, University of versailles Saint Quentin en Yvelines, 2Department of Physical Medcine and Rehabilitation, Raymond Poincaré Hospital AP-HP Garches and 3Laboratory of Human Motricity, Sport, Education and Health, University of Nice, Sophia Antipolis, France
BACKGROUND: Botulinum toxin injections are used to treat spasticity in stroke. Although this treatment is effective on muscle tone, its effect on functional gait-related activities remains uncertain.
OBJECTIVE: The aim of this randomized controlled trial was to determine the effect of a self-rehabilitation programme as an adjunct to botulinum toxin injections on gait-related activities in patients with chronic hemiparesis.
METHODS: Thirty-five outpatients were included. Each patient was randomized to 1 of 2 groups: botulinum toxin + standardized self-rehabilitation programme (R group, n = 19) or botulinum toxin alone (C group, n = 16). Each patient was evaluated with the following tests before botulinum toxin injections and one month afterwards: 10-m timed walk, Timed Up and Go, distance covered in 6 min over an ecological circuit, and the stair test.
RESULTS: There were significant improvements in the R group compared with the C group: maximal gait speed improved by 8% (p = 0.003); distance covered in 6 min over an ecological circuit increased by 7.1% (p = 0.01); and time to ascend and to descend a flight of stairs decreased by 9.8% (p = 0.003) and 6.6% (p = 0.009), respectively. The self-rehabilitation programme was well tolerated and safe.
CONCLUSION: These results strongly suggest that a standardized self-rehabilitation programme constitutes a useful adjunct to botulinum toxin injections in order to improve gait-related activities.
Key words: stroke; hemiplegia; botulinum toxin injection; self-rehabilitation programme; gait; functional activities.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Nicolas Roche, APHP, Hôpital Raymond Poincaré, Service de physiologie et d’explorations fonctionnelles, Groupement de Recherche Clinique et Technologique sur le Handicap (EA 4497), CIC-IT 805, CHU Raymond Poincaré, Garches, FR-92380 Garches, France. E-mail: roche.nicolas@rpc.aphp.fr
Accepted Jun 10, 2014; Epub ahead of print Sep 29, 2014
Introduction
An estimated 25–74% of the 50 million stroke survivors worldwide require some assistance or are fully dependent on caregivers for activities of daily living (ADL) (1). Gait is the most important factor related to independence in these activities (2). Chronic stroke patients frequently have persistent gait abnormalities related to paresis and spasticity, which limit their capacity to climb stairs, walk long distances, increase gait speed and step over obstacles. Post-stroke gait is characterized by a decrease in cadence, stride length and speed (3–7). It is also characterized by kinematic alterations, such as decreased peak hip flexion (6), peak knee flexion (8) and peak ankle dorsiflexion (9). Some of these kinematic abnormalities are mainly the result of spasticity; for example, decreased peak knee flexion during the swing phase of the gait cycle is frequently caused by spasticity of the rectus femoris (RF) (8). However, decreased peak knee flexion can also be due to other causes, such as weakness of the hip flexors, decreased peak ankle plantarflexion moment, or a decrease in knee angular velocity at toe-off. Similarly, decreased peak ankle dorsiflexion in the swing or stance phase is commonly due to spasticity of the triceps surae (TS) (9), but can also be caused by weakness of the ankle dorsiflexor muscles.
The main treatment for such focal spasticity is botulinum toxin (BoNT-A) injection. Several studies have shown that BoNT-A injections in the RF or TS muscles, respectively increase peak knee flexion during the swing phase of the gait cycle (range 5° and 9°, respectively) (10–13) and peak ankle dorsiflexion during the stance phase (9, 14–16). However, although BoNT-A improves kinematic gait parameters, few studies have reported a concomitant benefit in functional tests, such as gait speed, walking distance, stair climbing and transfers, which have an impact on gait-related ADL (11, 14). Indeed, Pittock et al. (9) showed that BoNT-A injections in the plantarflexor muscles reduced resistance to passive ankle dorsiflexion rated on the modified Ashworth scale, but with no significant improvement in gait velocity. Conversely, Mancini et al. (14) found a significant increase in gait velocity after a similar treatment. Likewise, Robertson et al. (11) showed that BTI injection in the RF muscle significantly improved peak knee flexion in the swing phase of the gait cycle, but tended to improve only the 10-m walking test, 6MWT, TUG test and time to ascend and descend a flight of stairs. In addition, Caty et al. (13) showed that even multifocal BoNT-A injections (in the RF, TS and hamstring muscles) did not improve gait speed despite improvements in kinematic parameters. Thus, it appears that the effect of BoNT-A on gait-related activities is small. These results suggest that novel strategies should be developed for the management of spasticity in order to optimize the effects of BoNT-A injections on functional gait-related activities in stroke patients.
To that end, Carda et al. (17) combined BoNT-A injections with several non-invasive techniques, such as casting, taping and stretching. They compared the effects in chronic stroke patients, and showed that both casting and taping associated with BTI in the TS muscle improved walking distance, but walking speed was increased only by casting after BoNT-A injections. Other studies have assessed the effect of BTI combined with functional electric stimulation (FES) in stroke patients. Johnson et al. (18) evaluated the effect in spastic drop foot. They found greater improvements in gait speed (109%) compared with other studies that assessed the effects of BoNT-A alone (17% according to Burbaud and 21% according to Hesse) or the effects of FES alone (13% according to Burridge and 26% according to Taylor) (15, 19–21). Taken together, these results suggest that non-invasive rehabilitation techniques may potentiate the effects of BTI on gait-related functional activities.
Effective stroke rehabilitation is based on the principles of task-specific training goals relevant to patients’ needs, as well as high-intensity practice with a sufficient number of repetitions. However, the effect of combining BoNT-A injections and self-rehabilitation to improve gait-related functional activities has, to our knowledge, not been evaluated in hemiparetic patients. This is all the more surprising, since several meta-analyses have shown that: (i) task-oriented exercises focusing on balance control, transfers, gait and gait-related activities (22–25); (ii) strengthening programmes; and (iii) stretching programmes are effective for the improvement of gait in these patients.
The aim of this study was to compare the effect of a combined treatment consisting of BoNT-A injections in the paretic lower limb and a self-rehabilitation programme, with BoNT-A injections alone on gait-related activities in chronic hemiparetic outpatients. We hypothesized that the combination of self-rehabilitation and BoNT-A injections in these patients would be: (i) more effective in improving gait-related-activities than BoNT-A alone; (ii) a safe treatment strategy; and (iii) well-accepted by the patients.
MethodS
A total of 35 outpatients with hemiplegia were included in this randomized controlled study. The patients’ characteristics are shown in Table I. Each patient was routinely followed-up in the spasticity management unit of a university hospital and regularly underwent BoNT-A injections. Inclusion criteria were: troublesome spasticity causing gait abnormalities, age over 18 years, hemiparesis due to a single hemispheric stroke, ability to walk 6 min with or without an assistive device, and a time lapse of at least 4 months since the last BoNT-A injections. Patients were excluded if they had severe muscle contractures, any comorbid disability other than stroke, such as visual impairment or musculoskeletal, cardiovascular, or severe cognitive disorders that would interfere with the study. They were also excluded if they had contracture of the triceps surae, defined as follows: peak ankle dorsiflexion less than 0° with the knee extended.
|
Table I. Patient characteristics |
||
|
Rehabilitation group (n = 19) |
Control group (n = 16) |
|
|
Age years, mean (SD) |
47.8 (14.4) |
51.5 (13.5) |
|
Sex ratio, M/F, n |
14/5 |
11/5 |
|
Height, cm, mean (SD) |
171.5 (8.4) |
168.2 (6.0) |
|
Weight, kg, mean (SD) |
73.7 (17.2) |
77.4 (17.4) |
|
Side of hemiparesis (left/right), n |
12/7 |
9/7 |
|
Time since stroke, years, mean (SD) |
15.7 (6.9) |
7.3 (3.6) |
The patients’ usual physiotherapy regimen was maintained unchanged (intensity frequency and content) throughout the protocol period, and if any home exercises were prescribed by their regular physiotherapists the patients were allowed to perform them. All subjects gave written consent before participation. The study was performed in accordance with the ethics codes of the World Medical Association (Declaration of Helsinki) and was approved by the local ethics committee (CPP Ile de France-Ambroise Paré).
Study design
Each patient attended 2 sessions:
V1 Inclusion: during this visit, a clinical examination and functional tests were carried out before BoNT-A injections. At the end of the visit, each patient was randomized to 1 of 2 groups: the R group (rehabilitation) who received combined BoNT-A and self-rehabilitation or the C group (control) who underwent BoNT-A injections alone. Botulinum toxin type A Botox® (Allergan Inc., Irvine, CA, USA) was used. All the injections were performed under electrical stimulation (5 mA). The dose per muscle was at the discretion of the physician according to patients’ needs and the physicians’ routine clinical practice. The dilution was 100 U/2.5 ml. The mean dose per muscle is reported for both groups in Table II.
V2 Evaluation: this visit took place 1 month after V1; during this visit the same clinical examination and the same functional tests as in V1 were carried out.
|
Table II. Mean dose of botulinum toxin type A injected per muscle (in units) |
||||||||
|
Group |
Gluteus magnus |
Rectus femoris |
Cruralis |
Hamstring |
Soleus |
Calf muscles |
Flexor digitorum brevis |
Flexor digitorum longus |
|
Rehabilitation group |
75.0 |
123.6 |
125.0 |
70.0 |
57.0 |
74.6 |
33.3 |
33.8 |
|
Control group |
66.6 |
104.0 |
118.0 |
116.6 |
59.0 |
64.5 |
36.7 |
37.5 |
Clinical assessment. Spasticity was assessed with the Modified Ashworth Scale (MAS) (26, 27). The Medical Research Council scale (MRC) was used to assess the motor command of the hip, knee and ankle flexor and extensor muscles. All clinical examinations were performed by the same investigator.
Functional tests. To avoid bias, all tests were performed by the same investigator. Patients were allowed to use their usual assistive devices or orthoses during the functional tests.
The ABILOCO Scale comprises 13 items and evaluates locomotion abilities in adult patients with stroke (28).
The 10-Meter Timed Walk Test (10MTWT) was used to assess maximal gait speed. The subject was instructed to walk as quickly as possible over a distance of 10 m with a 2-m run up. The time was recorded in seconds using a stopwatch.
In the TUG Test patients were required to stand up from a chair with armrests, walk 3 m, turn around, return to the chair and sit down again as quickly as possible. The time taken to complete this task was recorded in seconds using a stopwatch (29). Three trials were recorded for each patient.
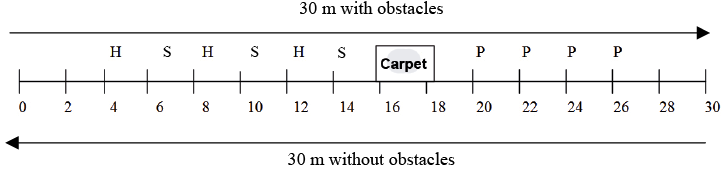
The distance covered in 6 min over an ecological circuit test (6MWT – Modified) (30) assesses walking capacity, endurance, dynamic balance and speed with and without obstacles. Subjects were asked to walk as quickly, but as safely, as possible, around a circuit comprising 30 m with obstacles and 30 m without obstacles for 6 min. The obstacles were arranged as shown in Fig. 1. Patients were instructed to: step over hurdles and slats, walk over a gym mat, and slalom around cones (2 m). Mean gait speed for both parts of the circuit (with, 6MWT – WO and without obstacles, 6MWT – NO) and maximal distance covered in 6 min were recorded.
In the Stairs Test subjects were asked to ascend and descend a flight of 15 stairs once, as quickly but as safety as possible, according to the method described by Flansbjer (31). They were asked to stand at the bottom of the first step, to go up the stairs, turn around on the top step, and come all the way back down until both feet were on the floor. The handrail could be used. The time taken to complete this task was measured in seconds with a stopwatch, which was stopped when the patient reached the top of the stairs and restarted when he/she began the descent.
Fig. 1. Representation of the ecological circuit. H: hurdle; S: slats; P: cones; Carpet: gym mat.
Intervention
The patients randomized to the R group followed a standardized home-based self-rehabilitation programme that consisted of 3 parts (10 min each). The exercises were chosen, firstly, to be safe and achievable for most patients and, secondly, with the aim of improving the most common impairments and functional deficits observed in chronic stroke patients. Three types of exercises were included, relating to 3 dimensions: task-oriented exercises focusing on locomotor activities, strengthening and stretching. Task-oriented exercises included: walking over obstacles and slaloming. These tasks corresponded to the functional gait-related difficulties most commonly encountered by patients as reported by Dean et al. (32) and van Duijnhoven et al. (33). Strengthening targeted the most frequently impaired muscle groups that affect locomotor activities: the hip flexors (34) and ankle plantarflexors (35). Stretching targeted the most commonly shortened muscle groups that affect locomotor activities: the hamstrings the rectus femoris and ankle plantarflexor muscles. The complete programme is shown in Appendix S11.
The R group performed the entire self-rehabilitation programme under guidance at the end of V1. The physiotherapist also answered any questions raised by the patients. The patients were asked to perform these exercises every day for 4 weeks. They were allowed to carry them out in 3 separate 10-min periods during the day. To help the patients to remember the exercises and to ensure that they were performed in optimum and safe conditions, they were given a workbook illustrating the whole programme at the end of V1 (see Appenix S1). In addition, the physiotherapist made a follow-up phone call 2 weeks after V1 to ensure compliance with, and the safety of, the programme. During this phone call the patient was asked: (i) if he/she had any difficulties performing the home-exercises, (ii) if he/she felt any pain during or after the exercises; (iii) if he/she had fallen during the training, and (iv) the mean time per day spent carrying out the home training programme. In addition, to assess compliance, patients were asked to complete a logbook each time they carried out the programme. They were asked to note the exercises carried out and the duration of each exercise.
Data analysis
The mean value of each functional test and its standard error were calculated for V1 and V2 for each group. For each patient in each group, the percentage improvement from V1 to V2 was calculated using the following formula: ((functional test performance at V2–functional test performance at V1)/functional test performance at V1)*100. For the parameters for which improvement was defined by a decrease in its value, the same formula was used, but multiplied by (–1) so that all improvements in parameters between V1 and V2 were associated with a positive value and vice versa. The mean percentage improvement and its standard error were then calculated for each group (R and C).
Statistical analysis
Normal distribution and homogeneity of the parameters tested were verified using the Shapiro–Wilk procedure. The tested parameters were not normally distributed and non-parametric statistical tests were therefore applied. Non-parametric paired Wilcoxon tests were carried out for each group (R and C) to assess within-group differences between V1 and V2. A non-parametric Mann–Whitney test was carried out to compare the characteristics of both groups. This test was also used to compare the percentage change in the functional test scores between groups. The significance level was fixed at p < 0.05 for all statistical analyses. All the statistical analyses were carried out using Statistica® version 7.1 software. Data from the clinical evaluation were described quantitatively and not analysed statistically because the scales used were ordinal (MAS and MRC).
Results
No significant differences were found between the 2 groups for age, sex, time since stroke, side of hemiplegia and mean dose of BoNT-A injected per muscle.
Clinical evaluation
There were small differences between groups for the level of spasticity in the tested muscles. Indeed, the level of spasticity was higher in the R group for the RF and TS muscles. The MAS score decreased by approximately 1 point in the muscles injected with BoNT-A. There was no difference in the reduction in MAS score between groups. All the results of the MAS are summarized in Table III. The strength of the tested muscle groups (MRC scale) did not change after BoNT-A injections in either group (Table IV).
|
Table III. Degree of spasticity for each muscle group (Modified Ashworth score for each muscle group (median value) |
||||||||
|
Spasticity |
RF V1 |
RF V2 |
H V1 |
H V2 |
Triceps V1 |
Triceps V2 |
GM V1 |
GM V2 |
|
Rehabilitation group |
2 |
1+ |
1+ |
1 |
3 |
2 |
0 |
0 |
|
Control group |
1+ |
1 |
0 |
0 |
2 |
1+ |
0 |
0 |
|
RF: rectus femoris muscle; H: hamstring muscles; triceps: soleus + gastrocnemius muscles; GM: gluteus muscles; V1: visit 1; V2: visit 2. |
||||||||
Functional tests
Baseline comparison of the 2 groups. At baseline, there were no significant differences between groups for any of the functional tests: ABILOCO scale (p = 0.12), TUG test performance (p = 0.87, Table IV), maximal speed on the 10 m-timed walk test (p = 0.75, Table IV), maximal distance covered in 6 min over an ecological circuit (p = 0.93) and the time to ascend and descend a flight of stairs (p = 0.53 and p = 0.99, respectively).
|
Table IV. Median Medical Research Council scale score for each muscle group |
||||||
|
Strength |
Quadriceps V1 |
Quadriceps V2 |
Hamstrings V1 |
Hamstrings V2 |
Triceps V1 |
Triceps V2 |
|
Rehabilitation group |
4 |
4 |
3 |
3 |
3 |
3 |
|
Control group |
4 |
4 |
3 |
3 |
3 |
3 |
|
V1: visit 1; V2: visit 2. |
||||||
Intra-group comparison of results. In C group, the only functional test that changed significantly 1 month after BoNT-A injection was the time to descend a flight of stairs (p = 0.04). In R group, significant improvements occurred for maximal walking speed (p = 0.10), time to perform the TUG test (p = 0.01) and time to ascend and descend the stairs (p = 0.01 and 0.04, respectively). There was no significant change in the ABILOCO Scale score for either group.
Inter-group comparison of results. The percentage improvement in maximal gait speed, the distance covered during the 6MWT–modified and the time to carry out the 6MWT–WO were significantly greater in R group than in C group (p = 0.003, p = 0.01 and p = 0.004, respectively; Table V). The percentage improvement in the time to ascend and descend the stairs was also significantly greater in R group compared with C group (p = 0.003 and p = 0.009, respectively).
|
Table V. Results of the functional tests |
||||||
|
Rehabilitation group |
Control group |
|||||
|
V1 Mean (SD) |
V2 Mean (SD) |
Difference % |
V1 Mean (SD) |
V2 Mean (SD) |
Difference % |
|
|
Maximal gait speed (m/s) |
1.2 (0.8) |
1.3 (0.8) |
8.3*, ** |
1.3 (0.8) |
1.2 (0.5) |
–4.4 |
|
Timed up and Go (s) |
15.7 (6.9) |
14.7 (5.9) |
5.4** |
14.6 (7.5) |
14.5 (7.4) |
–0.3 |
|
6MWT–modified (m) |
301.0 (130.5) |
315.5 (129.2) |
7.1* |
317.3 (114.5) |
312.6 (112.1) |
–1.0 |
|
6MWT–WO (m/s) |
0.78 (0.3) |
0.82 (0.3) |
6.9* |
0.83 (0.3) |
0.81 (0.3) |
–2.9 |
|
6MWT–NO (m/s) |
0.92 (0.4) |
0.95 (0.4) |
7.1 |
0.95 (0.3) |
0.95 (0.3) |
1.8 |
|
Time to ascend stairs (s) |
16.2 (5.8) |
14.7 (5.8) |
9.8* |
19.4 (15.1) |
21.1 (18.2) |
–6.3 |
|
Time to descend stairs (s) |
17.1 (8. 8) |
16.4 (10.0) |
6.6*, ** |
16.7 (9.3) |
17.9 (10.4) |
–7.8** |
|
*Mann-Whitney U test p < 0.05 for inter-group comparison (R vs C) of the percentage difference between V1 and V2. **Wilcoxon test p < 0.05 intra-group comparison between V1 and V2. |
||||||

Compliance with the self-rehabilitation programme (R group). Analysis of the logbook showed that, of the 19 patients, 16 (83%) reported that they performed the entire self-rehabilitation programme more than 5 days per week for the 4 weeks. One patient performed the programme 3 days per week and 2 reported that they performed it occasionally (fewer than 2 days/week). The mean time spent per section of the programme was 11.2 min/day for stretching, 11.9 min/day for functional task-oriented activities, and 11.2 min/day for strengthening, i.e. more than the intensity prescribed. No adverse events and, more specifically, no falls, were reported. Twelve patients reported that they needed help to carry out some exercises. 100% of the patients found the workbook useful, and 77% would have like to have this workbook on discharge home from their initial admission for stroke rehabilitation.
Discussion
The results of this study confirmed our initial hypothesis; that a self-rehabilitation programme combined with BoNT-A injections in the paretic lower limb of stroke patients would potentiate the functional effects of BoNT-A and improve functional gait performance. This has, to our knowledge, not been shown previouslye. Indeed, these results show that a self-rehabilitation programme performed in adjunction to BoNT-A improved: (i) maximal gait speed; (ii) the distance covered during the 6MWT-modified; (iii) maximal gait speed during the 6MWT-WO; and (iv) the time taken to ascend and descend a flight of stairs, compared with BoNT-A alone. The results of this study also show that this light self-rehabilitation programme based on stretching, strengthening and task-oriented gait training was well accepted by patients who were compliant and that the programme was safe.
As mentioned above, the present study showed that a self-rehabilitation programme combined with BoNT-A injections significantly improved the results of several functional tests that are not usually improved by BoNT-A alone. Close analysis of the results suggested that this improvement was not related to the decrease in spasticity, since the decrease was similar in both groups at V2. This suggests that the difference in results between the groups might be due, on the one hand, to the decrease in muscle strength and, on the other hand, to the specific task-oriented training performed by the R group.
With regard to the first hypothesis, Hameau et al. (36) recently assessed the impact of BoNT-A injections on muscle strength and spasticity of the paretic lower limb in chronic stroke patients using an isokinetic dynamometer. They showed that BoNT-A injections in the RF muscle: (i) reduced peak resistive torque during passive stretches; (ii) increased the angle at which peak resistive torque occurred; (iii) decreased knee extensor strength (the injected muscle); and (iv) increased knee flexor strength (the antagonist muscle), 1 month after the injections. These results encouraged us, firstly, to propose the self-rehabilitation programme immediately after BoNT-A injections and, secondly, to suggest that the strengthening exercises of the self-rehabilitation programme probably limit the impact of the decrease in muscle strength that occurs following BoNT-A injections. This would explain the significant improvement in performance in most of the functional tests in the R group compared with the C group, in which muscle strength decrease was not prevented.
Another hypothesis is that the task-oriented exercises carried out by the patients helped them to make use of the positive effects of BoNT-A to improve their functional abilities. This assumption is supported by several studies. Bonnyaud et al. (37) showed that the gait parameter most related to performance in the timed up and down stairs-test in chronic stroke patients was the percentage of the gait cycle spent in single support phase on the paretic lower limb. During the task-oriented exercise in which the patient was asked to step over bottles it might be hypothesized that this specific gait parameter was trained and improved, which might explain the significant improvement in stairs-test performance in the R group. Similarly, the second task-oriented training exercise was to slalom between bottles. This task was present in the test, which assessed the distance covered in 6 min over an ecological circuit. It could therefore explain the improvement in both total distance covered during the 6MWT–modified and gait speed in the 6MWT–WO, which only occurred in the R group. Similarly Dean et al. (38) found an improvement in TUG performance in chronic stroke subjects following task-oriented training involving overground walking, treadmill walking and functional tasks. The self-rehabilitation programme proposed in the present study focused on: (i) overground walking, and (ii) turning. It is likely that training in both of these activities specifically improved TUG performance in the R group. Although there was a similar decrease in the level of spasticity in the 2 groups after BoNT-A, it should not be concluded that stretching exercises are not useful. Indeed, it is likely that they optimize the effect of BoNT-A on spasticity, allowing patients to perform the self-rehabilitation programme more easily and perhaps more safely.
In addition, the results of the present study are in accordance with those obtained in studies of the upper limb in stroke patients. Sun et al. (39) assessed the effect of BTI combined with modified constraint-induced movement therapy. They showed that this adjunctive treatment improved arm function significantly more than BTI alone. Arm function is a voluntary activity, whereas locomotion is considered to be a semi-automatic task. In consequence the physiological mechanisms that underlie the functional motor improvements found in the study by Sun et al. might be different from those that underlie the improvements found in the present study. However, these results confirm our hypothesis that a rehabilitation programme prescribed in adjunction to BTI in the paretic lower limb can potentiate the functional effects of BTI and improve gait-related activities in chronic stroke patients.
The lack of change in the C group is not so surprising, since similar results have been reported previously in the literature. Pittock et al. (9) assessed the effects of BTI in the plantarflexor muscles in hemiparetic patients and found a reduction in passive resistance to ankle dorsiflexion, measured by the modified Ashworth scale, with no significant improvement in gait velocity. Conversely, Mancini et al. (14) and Hesse et al. (15) both showed that BoNT-A injections in the plantarflexor muscles improved gait velocity in chronic hemiplegic adults. Similarly, Robertson et al. (2009) showed that BoNT-A injection in the RF muscle significantly improved peak knee flexion in the swing phase of gait, but did not significantly modify the 10-m walk test, 6MWT, TUG test or time to ascend and descend stairs (11). In contrast, Hutin et al. (12) showed that BoNT-A in the RF muscle not only significantly improved peak knee flexion, but also gait velocity by approximately 21%. It thus appears that BoNT-A injected in either the RF or TS might have an impact on gait-related activities, but the effect is modest and inconsistent. All these results also suggest that: (i) the simultaneous decrease in muscle tone and improvement in various kinematic parameters does not guarantee that performance in commonly used functional tests will improve; (ii) clinicians who use BoNT-A to improve gait-related activities in stroke patients should try to define new strategies to improve its impact.
Study limitations
It is possible that the self-rehabilitation programme evaluated in this study would be more effective if it was personalized and adapted to target the specific muscle weakness and spasticity of each patient. We chose to design a standardized programme for the purpose of this study in order to evaluate patients’ acceptance and toleration and the safety of the programme. Our programme fulfilled all these objectives, since it was well-accepted by patients (the mean time per day spent carrying out the programme was in fact more than the time prescribed), it was well-tolerated and safe (no adverse events were reported). Future studies should evaluate personalized programmes, taking into account patient characteristics and targeting the muscles treated with BoNT-A, in order to assess whether they are more effective than a standardized programme.
Table V shows that, at V1, the level of performance on the functional gait test was relatively good. This is probably due to the inclusion criteria, which required patients to be able to walk with or without an assistive device for at least 6 min without stopping. Thus the results of this study are mainly transposable to patients with moderate to good recovery.
Another possible limitation is the dose of BoNT-A injected per muscle. However, as can be seen in Table II, which reports the mean dose per muscle used in both groups (R and C), there were no significant differences between groups. Moreover, the decrease in spasticity after BoNT-A was similar in both groups (Table III). Therefore, it seems likely that the difference in the results is mainly due to the self-rehabilitation programme.
Conclusion
These results strongly suggest that a standardized self-rehabilitation programme is a useful adjunct to BoNT-A injections in order to improve gait-related activities since, for the first time, improvements occurred in all the functional tests commonly used in clinical practice, which are rarely modified when BoNT-A is used alone. Further studies will be necessary in order to optimize the content of the self-rehabilitation programme and improve patients’ autonomy in gait-related activities of daily living.

1http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-1887
References
