Louise A. Connell, PhD1, Naoimh E. McMahon, MA1, Janice J. Eng, PhD2 and Caroline L. Watkins, PhD2
From the 1Clinical Practice Research Unit, School of Health, University of Central Lancashire, Preston, UK and 2Department of Physical Therapy, University of British Columbia, Vancouver, BC, Canada
OBJECTIVE: To investigate the current practice of physiotherapists and occupational therapists in prescribing upper limb exercises to people after stroke and to explore differences between professions and work settings.
DESIGN: A cross-sectional survey design.
PARTICIPANTS: Occupational therapists and physiotherapists working in UK stroke rehabilitation.
RESULTS: The survey’s response rate was 21.0% (n = 322); with 295 valid responses. Almost two thirds of therapists (64.7%, n = 191) agreed that they always prescribe upper limb exercises to a person with stroke if they can actively elevate their scapula and have grade 1 finger/wrist extension. Most therapists (98.6%, n = 278) prescribed exercises to be completed outside of therapy time, with exercises verbally communicated to family. Standardised upper limb specific outcome measures were used to evaluate the prescribed exercises by 21.9% (n = 62) of therapists. Differences were found between professions and across work settings.
CONCLUSION: The majority of prescribed upper limb exercises were of low intensity (range of motion or stretching exercises) rather than repetitive practice or strengthening exercises. The use of standardised outcome measures was low. Progression of exercises and the provision of written instructions on discharge occur less frequently in inpatient settings than outpatient and community settings.
Key words: occupational therapy; physiotherapy; stroke; upper limb; exercise prescription.
J Rehabil Med 2014; 46: XX–XX
Correspondence address: Louise Connell, Senior Research Fellow, Brook 417, Clinical Practice Research Unit, School of Health, University of Central Lancashire, Preston, PR1 2HE, UK. E-mail: laconnell@uclan.ac.uk
Accepted Oct 10, 2013; Epub ahead of print Jan 28, 2014
INTRODUCTION
In England alone, there are approximately 110,000 strokes each year, and in 2010 there was an estimated 300,000 people living with moderate to severe disabilities as a result of stroke (1). Although almost 3 quarters of stroke survivors will regain the ability to walk, regaining function of the affected upper limb is much more problematic (2). Over 60% of stroke survivors with initial upper limb deficit fail to achieve full functional movement at 6 months (3). Upper limb function has been found to significantly influence participation and quality of life during stroke recovery (4).
Optimum strategies to facilitate motor recovery after stroke include early, intensive, and repetitive task-specific practice for a prolonged period of time (5–7), although the strength of evidence is greater for lower, than for upper limb (8). Guidelines for stroke in the UK recommend that patients with some arm movement be given every opportunity to practice activities within their capacity (9), as this increase in intensity may improve the motor function of the upper limb after stroke (10). Upper limb exercises can be undertaken during therapy, as well as prescribed as homework to be completed by the person with stroke outside of formal therapy time.
It is evident that exercise prescription is a key component of upper limb rehabilitation after stroke, but to date the practices of physiotherapists and occupational therapists’ in prescribing upper limb exercises is unknown. Previous research has investigated the content of therapy sessions generally in treating impairment after stroke (11–17) but only one study, conducted in 2003 (13), specifically investigated physiotherapy treatments for the upper limb after stroke. This study concluded that Irish physiotherapists were not making the best use of alternative methods, such as independent exercise and family involvement, to increase the intensity of therapy that the upper limb receives during rehabilitation.
This is the first study to investigate the current practices of both physiotherapists and occupational therapists in prescribing exercises for the upper limb. If we are to ensure that therapists working in stroke rehabilitation prescribe upper limb exercises that will facilitate optimum motor recovery after stroke, it is important to understand what they currently do, and the factors that influence them in prescribing, or not prescribing, exercise. In light of the best practice recommendations for post-stroke rehabilitation, our research questions were:
1. What factors influence whether or not therapists prescribe upper limb exercises?
2. If therapists prescribe exercises to people after stroke to be completed independently outside of formal therapy time, how are they prescribed, monitored and evaluated?
3. Are there differences between professions and work settings for prescribing upper limb exercises?
METHODS
Study design
A cross-sectional study design was used with data collected via an online self-administered questionnaire.
Participants
The sample population in this study was occupational therapists and physiotherapists working with people with stroke in the UK. These therapists were identified through the College of Occupational Therapists Specialist Section Neurological Practice (COTSSNP) and the Association for Chartered Physiotherapists Interested in Neurology (ACPIN).
The study was approved by the University of Central Lancashire Research Ethics Committee.
Instrument
A review of the literature was carried out to identify an existing tool with established reliability and validity for use in this study. No suitable data collection tools were identified and therefore an original questionnaire was developed using the online software tool SurveyMonkey™. The questionnaire had 3 sections (i) Demographics, (ii) Upper Limb Exercises after Stroke (see Appendix SI1) and (iii) Use of the Graded Repetitive Arm Supplementary Programme (GRASP). The results presented is this paper reflect sections (i) and (ii) of the survey. Section (iii) of the survey, will be presented elsewhere. There was a mix of open- and closed-ended questions along with 5 point Likert scale questions. A question logic step was included which redirected respondents to the end of the questionnaire if they were not currently working with people with stroke.
The face validity of the questionnaire was established through a panel of therapists and researchers with extensive experience of both survey design and upper limb exercise prescription after stroke. Prior to disseminating the survey two rounds of online piloting were carried out with clinicians (n = 5 and n = 3) and minor changes made to the questionnaire based on feedback received.
Procedure
Permission was obtained from ACPIN and the COTSSNP to have the survey link emailed to their members (which included the clinicians involved in the pilot). Therapists were sent an email from the respective organisations containing the survey link, a brief note outlining the nature of the research, and an invitation to complete the survey. A follow-up reminder e-mail was also sent two weeks later.
Data analysis
Data was analysed using PASW Statistics 20. Frequency distributions were run in order to describe, summarise and demonstrate the distribution of the data. As data were categorical or ordinal in nature, non-parametric tests were carried out including: Chi-square to examine relationships between categorical variables, Mann-Whitney to compare differences between two independent groups, and Kruskall-Wallis to compare differences between 3 or more independent groups i.e. profession, work setting, level of seniority, number of years working with patients with stroke. Post-hoc Mann-Whitney tests were run in order to determine between which groups differences existed. Significance levels were set at ≤ 0.001.
RESULTS
The survey link was emailed to members of ACPIN that had identified stroke as their main speciality (n = 608) and similarly to members of the COTSSNP (n = 917) on two occasions. As the survey link was sent out by the organisations it was not possible to identify the exact number of therapists that successfully received the survey link. In total 322 therapists responded to the survey giving an approximate response rate of 21.1%. Of these respondents, 7 therapists were not currently working with people with stroke and 20 therapists completed only the demographics questions of the survey. These responses were excluded from the analysis leaving 295 (19.3%) valid data sets for analysis. The characteristics of the responding therapists are summarised in Table I. Responses were achieved from all geographical areas of the UK (Fig. 1).
|
Table I. Respondent characteristics (n = 295) |
|
|
Variable |
Responses % (n) |
|
Job title |
|
|
Physiotherapist |
53.9 (159) |
|
Occupational Therapist |
46.1 (136) |
|
NHS Band |
|
|
Band 5 |
4.1 (12) |
|
Band 6 |
39.0 (115) |
|
Band 7 |
44.7 (132) |
|
Band 8a/8b |
9.1 (27) |
|
Other |
3.1 (9) |
|
Primary work setting |
|
|
Acute |
27.0 (78) |
|
Rehabilitation |
37.5 (108) |
|
Community |
35.6 (103) |
|
Other |
2.0 (6) |
|
Number of years working with people with stroke |
|
|
0–2 years |
9.8 (29) |
|
3–10 years |
48.1 (142) |
|
10+ years |
42.0 (124) |
|
People with stroke treated each week that have problems with their upper limb |
|
|
≤ 25% |
2.4 (7) |
|
≤ 50% |
19.7 (58) |
|
≤ 75% |
54.9 (162) |
|
≤ 100% |
23.1 (68) |
|
NHS Band: UK National Health Service Job Bands; Band 5: most junior, Band 8a/8b: most senior, generally managerial or clinical specialist. |
|
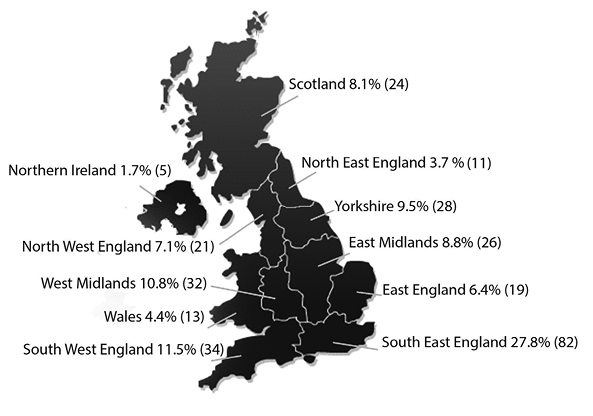
Fig. 1. Response rate % (n) per geographical location (n = 295).
Therapists’ responses to factors that may influence whether or not they prescribe upper limb exercises are shown in Table II. Almost two thirds of therapists (64.7%, n = 191) agreed or strongly agreed that they always prescribe upper limb exercises to person with stroke if they can elevate their scapula and have grade 1 finger wrist/extension, with physiotherapists agreeing significantly more with this statement than occupational therapists (U = 8,389.50, Z = –3.47, p = 0.001). No differences were detected between work settings for this statement. Occupational therapists were significantly more likely to agree that they tend not to prescribe upper limb exercises to people with shoulder pain (U = 6,521.50, Z = –6.60, p < 0.001) or increased tone (U = 7,566.50, Z = –5.01, p < 0.001). There was a significant difference between work settings for prioritising transfers and mobilising over upper limb exercises, with therapists working in acute settings more likely to agree with this statement compared to those working in community settings (U = 2,922.00, Z = –3.28, p = 0.001).
|
Table II. Therapists responses for statements relating to factors that influence exercise prescription (n = 295) |
|||||
|
Strongly agree % (n) |
Agree % (n) |
Neutral % (n) |
Disagree % (n) |
Strongly disagree % (n) |
|
|
I always prescribe upper limb exercises to a person with stroke if they can actively elevate their scapula and have grade 1 finger/wrist extension |
25.4 (75) |
39.3 (116) |
19.3 (57) |
13.9 (41) |
2.0 (6) |
|
I tend to prioritise transfers and mobilising over upper limb exercises for people with stroke |
3.7 (11) |
26.8 (79) |
12.2 (36) |
39.0 (115) |
18.3 (54) |
|
I tend not to prescribe upper limb exercises for people with stroke when they have shoulder pain |
2.4 (7) |
11.5 (34) |
11.2 (33) |
58.6 (173) |
16.3 (48) |
|
I tend not to prescribe upper limb exercises for people with stroke when they have increased tone |
1.4 (4) |
7.1 (21) |
9.2 (27) |
58.3 (172) |
24.1 (71) |
|
I tend not to prescribe upper limb exercises to people with stroke until they have regained normal movement patterns through facilitation and re-education |
1.7 (5) |
7.1 (21) |
5.4 (16) |
53.9 (159) |
31.9 (94) |
Therapists were asked if, when indicated, they prescribe upper limb exercises to the person with stroke to be completed independently outside of therapy time. The majority of therapists (n = 240, 85.1%,) answered ‘yes’ with just 4 (1.4%) answering ‘no’. Thirty-eight respondents (13.5%) answered ‘it depends’, outlining that the person with stroke’s ability, cognition, family support, prognosis and motivation were influencing factors in prescribing independent exercise. The type of exercise most frequently prescribed by therapists was found to be ‘range of motion/stretching exercises’ (n = 132, 46.8%,). Repetitive task specific practice was reported to be the most frequently prescribed upper limb exercise by 60 therapists (21.3%), with functional strengthening being ranked highest by thirty-nine therapists (13.8%). No significant differences were detected between types of exercises prescribed in the different work settings.
Therapists were also asked how they communicate, and to whom they communicate the prescribed upper limb exercises (Table III). Some form of written instructions were provided by 81.2% (n = 229) of therapists. Published manuals used by therapists include the GRASP and the Theraputty Hand Exercises Leaflet. Therapists reported relying primarily on verbal feedback from the person with stroke, family or carers and members of the multidisciplinary team to determine if the prescribed exercises were being completed. Almost all therapists (98.6%, n = 277) reported communicating the prescribed upper limb exercises to the family or carers of the person with stroke.
|
Table III. Therapist’s positive responses for how they communicate prescribed exercises, and to whom they communicate these exercises (n = 295) |
|
|
Do you communicate exercises: |
Yes % (n) |
|
Verbally |
95.0 (268) |
|
Using handwritten instructions |
81.2 (229) |
|
Using physio tools or a similar software |
51.4 (144) |
|
Using a locally developed manual |
26.2 (74) |
|
Using a published manual |
10.6 (30) |
|
To family/carers |
98.6 (277) |
|
To therapy assistants |
97.4 (262) |
|
To nursing staff |
46.5 (101) |
|
To occupational therapy staff |
92.4 (230) |
|
To physiotherapy staff |
93.6 (235) |
The survey included 4 questions asking therapists about their current practice in relation to progression of exercises, discharge and handover. Responses are shown by work setting in Table IV.
|
Table IV. Therapists responses, shown by work setting, for 4 questions relating to progression of exercises, discharge and handover (n = 277) |
||||||
|
Always % (n) |
Often % (n) |
Sometimes % (n) |
Rarely % (n) |
Never % (n) |
pa |
|
|
Do you progress the upper limb exercises you prescribe? |
||||||
|
Acute |
3.6 (10) |
11.6 (32) |
10.8 (30) |
1.4 (4) |
0.0 (0) |
< 0.001 |
|
Rehab |
7.6 (21) |
16.2 (45) |
11.6 (32) |
1.0 (3) |
0.0 (0) |
|
|
Community |
10.8 (30) |
20.2 (56) |
4.7 (13) |
0.0 (1) |
0.0 (0) |
|
|
Do you advise the person with stroke to continue the prescribed upper limb exercises on discharge? |
||||||
|
Acute |
10.5 (29) |
12.9 (36) |
3.2 (9) |
0.0 (2) |
0.0 (0) |
0.013 |
|
Rehab |
13.7 (38) |
15.5 (43) |
6.1 (17) |
0.0 (3) |
0.0 (0) |
|
|
Community |
19.5 (54) |
13.7 (38) |
2.5 (7) |
0.0 (0) |
0.0 (1) |
|
|
Do you provide the person with stroke up to date written instructions for their prescribed upper limb exercises on discharge? |
||||||
|
Acute |
2.8 (8) |
6.1 (17) |
10.1 (28) |
6.1 (17) |
2.1 (6) |
< 0.001 |
|
Rehab |
8.3 (23) |
12.2 (34) |
11.6 (32) |
2.9 (8) |
1.4 (4) |
|
|
Community |
10.5 (29) |
15.1 (42) |
7.9 (22) |
1.8 (5) |
0.0 (2) |
|
|
When the person with stroke moves to the care of another therapist or team is there a formal handover of the prescribed upper limb exercises? |
||||||
|
Acute |
7.6 (21) |
7.2 (20) |
7.5 (21) |
4.7 (13) |
0.0 (1) |
0.963 |
|
Rehab |
9.4 (26) |
11.9 (33) |
9.0 (25) |
5.8 (16) |
0.0 (1) |
|
|
Community |
11.1 (31) |
9.4 (26) |
8.7 (24) |
4.0 (11) |
2.9 (8) |
|
|
aKruskall-Wallis test. |
||||||
A significant difference was detected for work settings. Post-hoc analysis showed that therapists working in community settings progress prescribed exercises significantly more frequently than therapists working in acute settings (U = 2,421.00, Z = –4.471, p ≤ 0.001). Differences were also detected for the provision of up to date written instructions on discharge with therapists working in community (U = 2,120.50, Z = –5.207, p ≤ 0.001) and in rehabilitation settings (U = 2,685.00, Z = –3.546, p ≤ 0.001) more frequently providing instructions than those in acute settings. Therapists outlined in open-ended responses that the person with stroke would often be moved to another unit or team before there would be time to progress the prescribed exercises. It was also expected that the exercises would be reviewed when the person with stroke was followed up by the next team. Three therapists reported ‘time’ as a limiting factor in providing written instructions on discharge.
Therapists were asked to describe in an open text box how they measure the effectiveness of the prescribed upper limb exercises. Content analysis of the open-ended responses found that from 282 responses just over half of these reported using a standardised outcome measure (53.9%, n = 152). The remainder relied on generic measures, observation and subjective reports of functional change. The outcome measure was named in 39.0% (n = 110) of cases and in 21.9% (n = 62) of cases an upper limb specific outcome measure was used. In total over 30 different outcome measures were named. The most frequently used measures were the 9-Hole Peg Test (18), the Action Research Arm Test (ARAT) (19), the Arm Activity Measure (ArmA) (20), the Chedoke Arm and Hand Inventory (CAHAI) (21) and the upper limb section of the Rivermead Motor Assessment (22).
Respondents were asked who currently takes the lead on prescribing upper limb exercises to people after stroke in their work setting, and also who they thought should take the lead. There was a significant difference between the professions for both questions. Both physiotherapists and occupational therapists were significantly more likely to respond that their own profession currently leads (χ2(3) = 68.22, p < 0.001) and should lead (χ2(3) = 35.78, p < 0.001) on prescribing upper limb exercises to people after stroke. The majority of respondents (68.1%, n = 145) felt that ‘both’ professions should lead on prescribing exercises, with just over 10% of therapists (12.5%, n = 37) responding ‘it depends’. Analysis of open-ended responses showed that physiotherapists and occupational therapists feel that both skills sets are required, with physiotherapy input being more important for people with stroke with particularly low levels of ability or complications such as shoulder pain. Once there has been some improvement in motor control the role of the occupational therapist is deemed to be more important, where the gains made in physiotherapy are used to practice functional tasks and ADLs along with focussing on hand dexterity.
DISCUSSION
Almost two thirds of therapists, regardless of work setting, reported that they would always prescribe upper limb exercises to a person with stroke if they can actively elevate their scapula and have grade 1 finger/wrist extension. This is a positive finding, as the presence of this minimal level of motor ability has been found, on day two after stroke, to give a 98% probability of regaining some upper limb function at 6 months (23). However, a third of responding therapists did not agree that they would prescribe exercises to this population group. Therefore, there is the possibility that people with upper limb impairment after stroke, who have the baseline level of ability required to regain upper limb dexterity, are not receiving adequate therapy input in the form of prescribed upper limb exercises. The presence of pain, abnormal tone or abnormal movement patterns were not deemed to be factors that would prevent therapists from prescribing upper limb exercises.
This study also sought to find out if therapists prescribe upper limb exercises to people after stroke to be completed independently outside of formal therapy time. Almost all therapists in this survey reported that if the person with stroke has sufficient ability and cognition to successfully complete independent exercises then they would be prescribed. The importance of this finding cannot be overstated as, to date, the most promising methods of improving motor recovery of the upper limb after stroke have an element of self-administered exercise (24, 25). Therapists evidently identify self-administered exercises as a necessary and feasible means of increasing the intensity of practice that the upper limb receives during stroke rehabilitation. However, due to the self-report nature of this study, and considering the increasing pressures placed on health services resources, one must be cognisant that the responses in this survey may not be a completely accurate reflection of therapists’ day to day practices.
Interestingly in this study, the type of exercises that are reported to be most frequently prescribed by therapists, regardless of work setting, are range of motion and stretching exercises. This is despite the fact that best evidence recommends repetitive task-specific practice. Equally, strengthening exercises have been shown to improve upper limb strength and function after stroke (26) but appear not to be prescribed as frequently as they could or should be prescribed. A possible explanation for this finding is that perhaps the proportion of all patients that suffer upper limb impairment after stroke, and who are suited to engage predominantly with repetitive task specific and strengthening exercises, may be smaller than those who are not. However, it has also been well documented that therapists have difficulty in explaining their choice of treatment in stroke rehabilitation in light of the evidence base (15).
The inclusion of family members or carers in the delivery of exercises is another method to facilitate an increase in intensity of practice that the upper limb receives in stroke rehabilitation, and is one that has been shown to significantly improve motor recovery after stroke (27, 28). In this study it was found that almost all responding therapists reported communicating prescribed upper limb exercises to the family or carers of the person with stroke. However, it is noteworthy that more therapists report verbally communicating exercises to family or carers and therapy assistants than report communicating exercises using written instructions. This is somewhat of a contradiction, and raises the question that although therapists acknowledge the need for family involvement in the delivery of exercises, that due to constraints on resources and the challenges of inpatient settings, that more often than not exercises are communicated in an ad hoc manner, relying predominantly on verbal communication. It is a positive finding that therapists identify family or carers as an important resource in stroke rehabilitation and this finding is in contrast to previous research that found physiotherapists were not making the best use of alternative methods to increase intensity of therapy for the upper limb (13).
In this study a wide range of methods to measure the effectiveness of prescribed upper limb exercises are reported, with only one fifth of therapists using standardised upper limb specific outcome measures. The use of over 30 named measures in practice highlights the lack of a consensus within clinical practice which could be problematic when patients are being treated by different services throughout their rehabilitation. It is also becoming increasingly difficult to assess the cost-effectiveness of long-term rehabilitation interventions after stroke due to a lack of agreed measures and standards (1). Swinkels and colleagues (29) investigated the barriers to using standardised outcome measures by physical therapists in the Netherlands and concluded that lack of knowledge, lack of time and lack of managerial support were influencing factors. Importantly in the context of this study, Swinkels and colleagues outlined that despite positive attitudes towards the use of outcome measures and the advantages of their use, there existed a disparity between what therapists said they did and what they actually did in practice.
The final aim of this study was to investigate if differences existed between professions and work settings in prescribing upper limb exercises. An interesting dynamic exists between physiotherapists and occupational therapists working in stroke rehabilitation as at present it appears that both professions lead on prescribing upper limb exercises. Both professions think that this is the way it should remain, as both sets of knowledge, experience, and clinical perspectives are deemed to be necessary, and to be of benefit to the patient. These findings support those of both Booth and Hewison (30), and De Wit and colleagues (31). The most noteworthy difference detected in this study was between work settings. Therapists working in acute settings acknowledged that they are required to prioritise transfers and mobilising over prescribing upper limb exercises, that they have less opportunity to progress any prescribed exercises, and that they less frequently provide up-to-date written instructions of the prescribed exercises on discharge. Regardless of who is leading on prescribing upper limb exercises in stroke rehabilitation, it is clear that therapists working in inpatient settings, with the ever-decreasing average length of stay do not have the same opportunities, as those therapists working in rehabilitation and community settings, to address upper limb deficits. There is increasing emphasis being placed on the role of community teams in reviewing and following-up prescribed upper limb exercises.
Limitations
The response rate was low but not unexpected for this type of survey (32). Efforts were made to increase responses through reminder emails and the use of the professional organisations for distribution provided credibility and anonymity. As the sample size was over 150 the sampling error was reduced (33) but should still be acknowledged. The procedure used in this study allows for a self-selection bias where individuals with strong opinions or personal interest in the prescription of upper limb exercises after stroke may be over represented in the study findings, as opposed to individuals who are indifferent to the topic and less likely to respond. There is also the risk of a social desirability bias as this survey relied on self-reporting of current practice and therefore the responses of therapists may therefore not be a completely accurate reflection of daily practice. Prior to dissemination of the online survey every effort was made, through a number of rounds of piloting, to ensure questions were clear and easily understood, however there is always the risk of misinterpretation of what is being asked in the survey.
Conclusion
In the UK both physiotherapists and occupational therapists prescribe upper limb exercises to people after stroke at all stages of the stroke pathway. At present, the most frequently prescribed exercises are of low intensity, i.e. range of motion and stretching exercises, which may be reflective of the suitability of post-stroke patients with upper limb problems to engage in more evidence based repetitive task-specific practice. Therapists report prescribing upper limb exercises to be completed independently outside of therapy time, communicated most often in verbal format, however, evaluation of prescribed exercises using standardised measures is low. Innovative strategies are now required which facilitate clinicians to (i) effectively and efficiently communicate evidence-based exercises to people after stroke ensuring maximum opportunity for recovering and (ii) measure clinically meaningful change during rehabilitation.
ACKNOWLEDGEMENTS
The Association for Chartered Physiotherapists Interested in Neurology and the College of Occupational Therapists Specialist Section Neurological Practice are gratefully acknowledged for the assistance given in disseminating the survey to members of the therapy professions and the therapists that took the time to complete the survey.
The work presented here is the first phase of a 3-year National Institute for Health Research (NIHR) funded project which aims to develop a feasible structured upper limb exercise programme in UK stroke rehabilitation units. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS or the NIHR.

1http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-1268
REFERENCES
1http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-1268
