Kristina Åhlund, RPT, MSc1, Maria Bäck, RPT, PhD2,3 and Ninni Sernert, RPT, PhD4
From the 1Department of Physiotherapy, NU-Hospital Group, Trollhättan, 2Department of Physiotherapy and Occupational Therapy, Sahlgrenska University Hospital/Sahlgrenska, 3Institute of Medicine, Department of Molecular and Clinical Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg and 4Department of Research and Development, NU-Hospital Group, Trollhättan, Sweden
OBJECTIVE: The aim of this study was to examine fear-avoidance beliefs in patients after first-time myocardial infarction and to determine how such beliefs change over time. A futher aim was to analyse fear-avoidance beliefs and physical activity levels in patients attending exercise-based cardiac rehabilitation led by a registered physiotherapist, compared with a control group.
DESIGN: Prospective cohort study.
Patients: A total of 62 patients after first-time myocardial infarction were consecutively included in the study, mean age 61 years (range 42–73). Thirty-four patients chose exercise-based cardiac rehabilitation and 28 carried out the exercise regime on their own (controls). At follow-up, 57 patients (n = 30 and n = 27, respectively) responded.
METHODS: The Fear-Avoidance Beliefs Questionnaire and the Exercise and Physical Activity questionnaires were completed at 1 and 4 months post-infarction.
RESULTS: Clinically relevant fear-avoidance beliefs were seen in 48% of all patients at baseline, compared with 21% at follow-up (p = 0.01). Corresponding baseline values were 62% for the cardiac rehabilitation group and 29% for controls (p = 0.02). At follow-up, 4 months post-infarction, the difference between the groups was no longer seen. The total amount of physical activity increased over time for the cardiac rehabilitation group (p = 0.03), and this was also significant compared with the control group (p = 0.02).
CONCLUSION: Compared with controls, patients attending exercise-based cardiac rehabilitation led by a registered physiotherapist, demonstrated higher levels of fear-avoidance beliefs at baseline, which decreased over time. Furthermore, attendees increased their level of physical activity and exercise over time. Participation in exercise-based cardiac rehabilitation is therefore strongly recommended for patients with myocardial infarction, especially for those with increased fear of movement.
Key words: fear; avoidance; myocardial infarction; cardiac rehabilitation; physical activity; exercise.
J Rehabil Med 2013; 45: 00–00
Correspondence address: Kristina Åhlund, Department of Physiotherapy NÄL, NU-Hospital Group, Trollhättan, SE-461 85 Sweden. E-mail: kristina.ahlund@vgregion.se
Accepted May 31, 2013; Epub ahead of print Sep 3, 2013
Introduction
Cardiovascular diseases are the most frequent cause of death and disability worldwide, and are anticipated to continue to be so in the future (1).
Serious concern is common after an acute cardiac event, and approximately 50% of patients experience increased anxiety (2). The impact of exercise and multifactorial cardiac rehabilitation on improving psychological factors has been shown in a recent study (3). Clinical experience shows that patients are often afraid of physical movement and need guidance to find a suitable activity. In the acute phase after a cardiac event, fear may be regarded as a normal psychological reaction. In patients with chronic pain, fear and subsequent avoidance behaviour has been shown to be adaptive as a natural response to injury (4). There are, however, patients who cannot cope with their fear and who develop long-term avoidance behaviour (5). Studies are needed to investigate whether this fear-avoidance behaviour also relates to patients with myocardial infarction (MI).
Medical literature often uses the terms “fear of movement” and “kinesiophobia” synonymously, but there are some differences in meaning (6). Fear of movement is defined as a specific fear of movement and physical activity that is (incorrectly) assumed to cause re-injury (5, 7). Kinesiophobia is described as excessive, irrational and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or re-injury (8).
Fear of movement has been identified in relation to the fear-avoidance belief model as an important factor showing that some patients develop impairment, disability and depression in relation to chronic pain (5, 7). Fear-avoidance belief (FAB) means that the individual avoids activity or movement due to a perception that it can cause injury (9). This definition is used in the current article, but the concept itself has not been fully defined (6, 10). The concept of FAB was first developed in relation to patients with chronic musculoskeletal pain, but may also include disorders with other aetiologies (9, 11). Research on FAB, or closely related constructs, in patients with cardiac disease has so far been limited. Van Ittersum et al. (12) analysed FAB and kinesiophobia in patients with an implantable cardioverter defibrillator and the results indicate a negative association between fear of exercise and health-related quality of life. Bäck et al. (13) showed that 20% of patients with coronary artery disease (CAD) had occurrence of kinesiophobia 6 months after the cardiac event. Patients with higher levels of kinesiophobia participated to a lesser extent in cardiac rehabilitation, had lower levels of physical activity, poorer muscle function and health-related quality of life and a higher degree of anxiety and depression, compared with the group with low levels of kinesiophobia.
Physical activity and exercise are closely related concepts (14), but they are often incorrectly used synonymously. In this study, we are careful to distinguish these concepts, because of the differences in secondary preventive effects (15–17). It is known that exercise capacity, as determined by direct measurement of peak oxygen intake (VO2peak), is a powerful predictor of cardiac death and therefore exerts a major long-term influence on prognosis after CAD (18). A sufficient level of physical activity is considered adequate as primary prevention to reduce the incidence of several major public health diseases, including CAD (19). Furthermore, there is evidence that individualized and organized exercise in cardiac rehabilitation reduces mortality from cardiovascular disease (15–17). In addition, exercise has positive effects on risk markers, such as a reduction in total cholesterol and triglycerides, systolic blood pressure and improvements in quality of life (15–17). However, the effects of physical activity in secondary prevention in patients with CAD are more limited. The influence of exercise after percutaneous coronary intervention (PCI) has been described in a review article (20). The results suggest that moderate exercise increased VO2peak, improved quality of life and helped to reduce cardiac events and hospital admissions. Most of the reviewed studies revealed a significantly lower rate of re-stenosis, compared with non-exercise controls (20).
Fear of movement has been reported to be strongly associated with limitations in physical activities (5), and previous studies have suggested that FAB and kinesiophobia are likely to occur in patients with heart-related problems (12, 13). However, to our knowledge, FAB has not been analysed in relation to exercise-based cardiac rehabilitation led by a registered physiotherapist (RPT), after an acute MI. Therefore, the aim of this study was to examine the presence of FAB in patients after first-time MI and to determine how FAB changes over time. An additional aim was to analyse FAB and physical activity levels in patients attending exercise-based cardiac rehabilitation compared with a control group.
Material and Methods
Patients
Sixty-nine patients following first-time MI and PCI, in a county hospital for emergency care in western Sweden, were consecutively invited to participate in the study. A total of 64 patients agreed to participate. Exclusion criteria were: patients who did not understand written or spoken Swedish, or those with severe mental or physical disability. Patients aged 75 years and older were also excluded, because older patients often had their first check-up by phone, due to difficulties in getting to the hospital.
The patients attended a standard check-up visit 1–2 weeks post-infarction, where they were offered RPT-led exercise-based cardiac rehabilitation in accordance with the regular care programme. At this visit they were also invited to participate in the study. The patients were informed about the study in accordance with guidelines from the Swedish Ethical Review Board and the principles of the Declaration of Helsinki. All patients gave their informed consent to participate. Before the start of the study, written permission was also obtained from the medical unit manager and the personal data representative in the hospital organization.
Intervention
All patients in the cardiac rehabilitation group and control group who agreed to participate in the study, were sent 2 self-assessment questionnaires on FAB and physical activity and 1 questionnaire with background information by post; at baseline (1 month post-infarction) and at follow-up (4 months post-infarction). The intervention was part of standard treatment, in which all patients at the check-up visit 1–2 weeks post-infarction were given brief information by a RPT including advice on exercise and an invitation to participate in exercise-based cardiac rehabilitation. In the present study, the cardiac rehabilitation group consisted of patients who agreed to attend exercised-based cardiac rehabilitation under the guidance of the RPT. These patients were offered an individual visit, including a subjective assessment, a sub-maximal exercise test on a stationary bicycle and received individual exercise advice. After this, the patients attended RPT-led group training, including aerobic exercise and muscular endurance exercise according to the international guidelines for cardiac rehabilitation (17). The control group consisted of patients who declined cardiac rehabilitation and thus chose to manage the rehabilitation on their own. In the present study, these patients were regarded as controls.
Measurements and evaluations
The Fear Avoidance Belief Questionnaire (FABQ) consists of 16 items relating to patients’ beliefs about the relationship between perceived discomfort and movement, which can lead to fear of movement and avoidance of physical activity/exercise. The statements are divided into 2 subscales: physical activity (5 items) and work (11 items), which are considered to be valid and reliable for patients with chronic pain when used separately (21).
The modified version (m-FABQ) is the original subscale of physical activity modified to 4 items, which, in a pilot study, was found to have good correlation with the original scale for physical activity (n = 36, r = 0.97) (11). The questionnaire has been translated and validated for use in a Swedish pain population (11). Like the original version of the FABQ, the m-FABQ is a self-report questionnaire in which the patient estimates each item on a Likert scale between 0 and 6, from strongly disagree to strongly agree. The patient’s response is added up to give a total (0–24), where a higher score indicates a higher degree of FAB. In the study by Linton et al. (22) a score above the median (≥ 9) was regarded as having significantly increased risk of developing pain and increased physical activity problems. Thus, we considered a FAB score ≥ 9 as clinically relevant.
The scale was originally designed to measure FAB in patients with low back pain. For this study, the questionnaire was modified for patients with MI. In the original statement, the words “pain” and “back” often recur. In this study, we used the words “complaints” and “heart”, respectively.
The Exercise and Physical Activity Questionnaire consists of 8 items. Three items measure intensity and frequency associated with exercise. The patient estimates his/her exercise volume on each of 3 intensity levels; low, moderate and high, from never, to 3 times/week or more. Four of the items investigate everyday physical activity in relation to the 4 seasons and the last item relates to the intensity of activities of daily work, ranking from not intense to very intense. When added together, the items result in a physical activity index (PAI) in the range 0–32. A high PAI score has been shown to indicate both a high total activity volume and exercise at high intensity. The questionnaire was considered to be valid and reliable in a normal population (24).
Statistical analyses
The data were computerized and analysed using the Statistical Package for the Social Sciences (IBM SPSS 20.0, Chicago, IL, USA). Descriptive data are presented as means and medians (range), where applicable. For comparisons between groups, the χ2 test was used for dichotomous variables and the Mann-Whitney U test for ordinal data. Wilcoxon signed-rank test was used for comparisons of the paired observations within the study groups. A p-value ≤ 0.05 was considered statistically significant.
A sample size was calculated on a p-value of 0.05, power of 0.80, a standard deviation of 5, and a difference of 3.5 between the groups, which gave 33 patients in each group. The calculations were made with intention-to-treat analyses.
Results
The 3 questionnaires were posted to all 64 patients included at baseline, of whom 62 (97%) responded. At the 4-month follow-up questionnaires were again posted to all 64 patients and 57 (89%) responded. One patient did not take part in the follow-up due to bypass surgery and one questionnaire was returned by the post office with an unknown address. The remainder (n = 5) were recorded as missing (Fig. 1). Descriptive data are reported in Table I. There were no significant differences in baseline characteristics between groups. In the total study population, among those who reported other illnesses, diabetes was most common (11.3%), followed by hypertension (9.7%) and asthma (6.5%).
FAB changed over time in the total study population (Table II). There was a significant decrease, in terms of both total FAB (p = 0.04) and the percentage of patients with FAB of clinical relevance (≥ 9) (p = 0.01). Comparing the groups, the cardiac rehabilitation group had a significantly higher FAB at baseline (p = 0.02) and there was a significant decrease in FAB within the group between baseline and the 4-month follow-up (p = 0.01). There were no significant inter-group differences at follow-up (Table III).
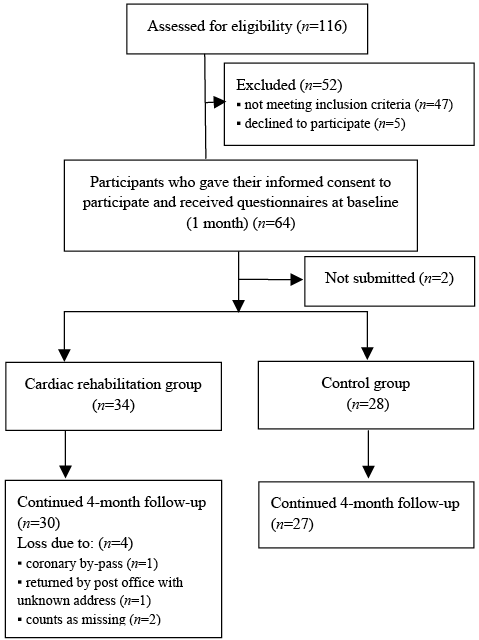
Fig. 1. Study population.
|
Table I. Baseline characteristics of the study population (n = 62) |
|||
|
Cardiac rehabilitation group (n = 34) |
Control group (n = 28) |
p-value |
|
|
Male/female (%) |
24/10 (70) |
22/6 (79) |
n.s. |
|
Age, years, mean (SD) |
61 (9.1) |
61 (8.0) |
n.s. |
|
Cohabiting, n (%) |
29 (85) |
25 (89) |
n.s. |
|
Employed, n (%) Internal missing |
19 (56) |
15 (56) 1 |
n.s. |
|
Sick leave, n (% of employed) |
17 (89) |
10 (67) |
n.s. |
|
Pension, n (%) |
14 (41) |
10 (37) |
n.s. |
|
Other illness, n (%) |
16 (47) |
8 (29) |
n.s. |
|
Group training outside cardiac rehabilitation, n (%) |
5 (15) |
5 (18) |
n.s. |
|
Regular exercise at moderate intensity, n (%) |
20 (59) |
11 (39) |
n.s. |
|
Regular exercise at high intensity, n (%) |
9 (26) |
8 (29) |
n.s. |
|
Nominal data are presented as n (%). Interval data are presented as mean ± 1 standard deviations (SD). p ≤ 0.05 was considered significant. The χ2 test was used for the dichotomous variables and the Mann-Whitney U test was used for the ordinal variables. n.s.: not significant. |
|||
A larger proportion of patients exercised regularly at a higher intensity level at the 4-month follow-up compared with baseline (p = 0.02) (Table II). Comparing groups, there was a significant increase in higher intensity activities within the cardiac rehabilitation group (p = 0.05), which was not the case in the control group (Table III). At follow-up there was a significant increase in the total amount of physical activity and exercise, both within the cardiac rehabilitation group (p = 0.03) and compared with the control group (p = 0.02).
|
Table II. Changes in fear-avoidance beliefs and physical activity over time in the total study population (n = 62) |
|||
|
Baseline (n = 62) |
Follow-up (n = 62) |
p-value |
|
|
m-FABQ Mean (SD) Median (range) Internal missing, n |
7.6 (5.2) 8 (0–16) 1 |
6.0 (5.1) 6 (0–18) 5 |
0.04* |
|
m-FABQ ≥ 9 (%) |
29 (48) |
13 (21) |
0.01* |
|
PAI Mean (SD) Median (range) Internal missing, n |
14.1 (6.0) 12.3 (0–26) 2 |
15.5 (5.6) 15.3 (4.5–28) 6 |
0.06 |
|
Regular exercise at moderate intensity, n (%) |
31 (50.0) |
37 (59.7) |
0.70 |
|
Regular exercise at high intensity, n (%) Internal missing, n |
17 (27.4) |
23 (37.1) 5 |
0.02* |
|
Nominal data are presented as n (%). Interval data are presented as mean ± 1 SD and median (range). *p ≤ 0.05, Wilcoxon signed-rank test. m-FABQ: modified Fear-Avoidance Beliefs Questionnaire; PAI: Physical Activity Index; SD: standard deviation. |
|||
|
Table III. Comparison between groups in fear-avoidance beliefs and physical activity at baseline and after 4-month follow-up (n = 62) |
||||||
|
Cardiac rehabilitation group |
Control group |
p-value between groups |
||||
|
Baseline n = 34 |
Follow-up n = 3 4 |
Baseline n = 28 |
Follow-up n = 28 |
Baseline |
Follow-up |
|
|
m-FABQ Mean (SD) Median (range) Internal missing, n Sign difference between baseline and follow-up |
8.9 (4.9) 10 (0–16) |
5.9 (5.1) 6.0 (0–18) 4 0.01* |
5.9 (5.0) 6 (0–16) 1 |
6.1 (5.1) 6.0 (0–16) 1 0.91 |
0.02* |
0.91 |
|
m-FABQ ≥ 9, n (%) Internal missing, n Sign difference between baseline and follow-up |
21 (62) |
7 (20.7) 4 0.01* |
8 (29) |
6 (21.4) 1 0.22 |
0.02* |
0.50 |
|
PAI Mean (SD) Median (range) Sign difference between baseline and follow-up |
14.6 (5.8) 13.5 (4–25.5) |
17.2 (5.7) 16.5 (6.5–26) 0.03* |
13.4 (6.3) 11.5 (0–26) |
13.7 (5.1) 14.0 (4.5–28) 0.70 |
0.34 |
0.02* |
|
Regular exercise at moderate intensity, n (%) Sign difference between baseline and follow-up |
20 (59) |
21 (61.8) 0.89 |
11 (39) |
16 (57.1) 0.23 |
0.13 |
0.42 |
|
Regular exercise at high intensity, n (%) Internal missing, n Sign difference between baseline and follow-up |
9 (26) |
15 (44.1) 4 0.05* |
8 (29) |
8 (28.6) 1 0.93 |
0.85 |
0.15 |
|
Nominal data are presented as n (%). Interval data are presented as mean ± 1 stamdard deviation (SD) and median (range). p-value calculations between groups the Mann-Whitney U test and within groups the Wilcoxon signed-rank test. *p ≤ 0.05. m-FABQ: modified Fear-Avoidance Beliefs Questionnaire; PAI: Physical Activity Index. |
||||||


Discussion
The prevalence of clinically relevant FAB (≥ 9) in the present study was 48% at baseline, 1 month post-infarction, and this had decreased to 21% by follow-up, 3 months later. Comparing the groups, there was a significantly higher level of FAB in the cardiac rehabilitation group at baseline, but at follow-up, this difference was no longer seen 3 months later. In this group, there were also significant increases over time, both in total activity (PAI) and in exercising at higher intensity.
A study by Bäck et al. (13) showed that 20% of patients with CAD had kinesiophobia 6 months after a cardiac event. The fact that, after an acute MI, patients obtained high FAB scores might be regarded as normal (4). It is, however, important that the patient decreases the level of FAB over time to reduce the risk of negative health impacts and to maximize successful secondary prevention (5). Furthermore, it is interesting to note that the patients with higher FAB scores at baseline tended to choose supervised cardiac rehabilitation to a greater extent than those with low levels of FAB. At follow-up 3 months later, this difference in FAB had equalized. Access to physical fitness tests and professional exercise advice on an individual basis before starting exercise may be factors that reduce FAB.
According to the fear-avoidance model (7), the best way to overcome FAB of clinical relevance is to confront one’s fears. Previous studies of patients with chronic pain revealed a reduction in levels of FAB/-fear of movement and improved function after cognitive exposure-based rehabilitation programmes (24, 25). Since FAB decreased over time in the cardiac rehabilitation group, it is possible that RPT-led cardiac rehabilitation can give the patient time and opportunity to confront his/her fear of exercise during supervised exercise. On the other hand, there were no differences in FAB between the groups at follow-up. This finding indicates that future research is needed in order to identify more specifically which patients post-MI require extra attention with regard to FAB.
Moreover, the amount of regular exercise at the higher intensity level tended to increase over time in the cardiac rehabilitation group. This is interesting, as recent research primarily suggests that regular exercise, intensity level 13–15 on Borg’s scales of exertion (26), is needed to achieve positive secondary preventive effects in patients with CAD (15–17).
In a recent effort to increase physical activity levels in patients with sedentary lifestyles, patients have been referred by their primary carer to exercise providers, such as fitness instructors in the community (termed exercise referral schemes). However, evidence suggests that the benefits of exercise referral schemes are temporary and may not be applicable to patients with specific diagnoses, such as CAD (27).
There are many factors that are likely to influence patients’ adherence with secondary prevention advice. It is important to note that it is common for patients to have misconceptions in their perception of whether they can influence their disease themselves by their behavior and lifestyle (28). The RPT is attributed a very important role in cardiac rehabilitation and is considered to be an expert on prescribing individualized exercise (29). Furthermore, the RPT is thought to play an important role in motivating and encouraging patients to make lifestyle changes in the field of physical exercise (30). Further research is needed into the impact of FAB and kinesiophobia on attendance at exercise-based cardiac rehabilitation.
In considering the limitations of the study in a randomized controlled trial the groups may have been more comparable at baseline. However, the aim of the study was to analyse FAB as part of standard treatment, which may also be regarded as a strength, as it reflects routine clinical practice. Furthermore, the instrument FABQ is criticised for lack of sensitivity, i.e. it is unable to connect fear with specific activities or movements (10). The fear-avoidance models are also criticised and are thought to require a conceptual extension, to better reflect reality and provide adequate clinical benefit (10). However, the FABQ is considered to be a useful screening tool for FAB in patients with pain, facilitating the implementation of early treatment measures (11). An additional limitation of the present study is that neither the FABQ nor the m-FABQ has been tested for reliability or validity in patients with MI, and the fact that the words “pain” and “back” were replaced to better fit this context should also be taken into consideration. The Tampa Scale for Kinesiophobia Heart (TSK-SV-Heart) has subsequently been modified and validated in Swedish (31). Future research could employ this tool due to its more comprehensive screening of patients for kinesiophobia.
In future studies, it would be of interest to analyse the impact of FAB, fear of movement and kinesiophobia on clinical variables in cardiac rehabilitation outcomes for patients with MI. This research could lead to the development of treatment strategies specifically for excessive fear of movement in patients with MI, before implementation in clinical practice.
In conclusion, compared with controls, patients attending RPT-led exercise-based cardiac rehabilitation demonstrated a higher FAB at baseline, which decreased over time. Attendees increased their levels of physical activity and exercise over time. Therefore, attendance at cardiac rehabilitation is strongly recommended for patients with MI and especially for those with increased fear of movement.
Acknowledgements
The authors would like to thank Helena Norén, Jessica Bengtsson and Hilda Hagman for help with including the patients, and the Department of Research and Development, NU-Hospital Group.
The authors declare no conflicts of interest.
References
