Evan H. Kwong, BSc(Pharm), MD, MSc, FRCPC1, Noorshina Virani, BScPT, MD, FRCPC1,4, Magali Robert, MD, FRCSC3,4, Kate Gerry, BScPT4, Anita Harding, MD, FRCSC3, M. Sarah Rose, PhD5, Sean P. Dukelow, MD, PhD, FRCPC1,2 and Pamela M. Barton, BSc(Hons), MD, FRCPC1,2,4
From the 1Division of Physical Medicine and Rehabilitation, Department of Clinical Neurosciences, 2Hotchkiss Brain Institute, 3Department of Obstetrics and Gynaecology, University of Calgary, 4Alberta Health Services Chronic Pain Centre and 5Alberta Health Services, Calgary, Alberta, Canada
OBJECTIVE: To determine the inter-rater reliability of the Active Straight-Leg Raise and One-Leg Standing tests.
DESIGN: Cross-sectional pilot study.
SUBJECTS: Thirty-one women who were either not pregnant or at least 9 months post-partum.
METHODS: Subjects completed a questionnaire and standardized pain and disability assessments. The Active Straight-Leg Raise and One-Leg Standing tests were assessed by 3 independent, blinded examiners. Inter-rater reliability was determined, and relationships with assessments were explored.
RESULTS: For the Active Straight-Leg Raise test, the kappa coefficient was 0.87, sensitivity 71%, and specificity 91%. Relationships with various pain and disability assessments were demonstrated, including the Functional Pelvic Pain Scale (r = 0.77) and Roland-Morris Disability Questionnaire (r = 0.70). For the One-Leg Standing test, kappa coefficients were –0.02 and 0.14 for the left and right sides, respectively, and thus no further analyses were performed.
CONCLUSION: In women with a spectrum of low-back and pelvic pain, the Active Straight-Leg Raise test had good inter-rater reliability, whereas the One-Leg Standing test did not. Further studies are required regarding the validity of the Active Straight-Leg Raise test.
Key words: low-back pain; pelvic girdle pain; pelvic pain; sacroiliac joint; reproducibility of results; reliability, Active Straight-Leg Raise test; One-Leg Standing test.
J Rehabil Med 2013; 45: 00–00
Guarantor’s address: Pamela Barton, Alberta Health Services Chronic Pain Centre, Holy Cross Centre, #160, 2210 – 2nd Street SW, Calgary, Alberta, Canada T2S 3C3. E-mail: Pamela.Barton@albertahealthservices.ca
Accepted May 20, 2013; Epub ahead of print Aug 27, 2013
INTRODUCTION
The prevalence of chronic non-cancer pain worldwide ranges from 10.5% to 55.2% depending on the criteria used and study methodology; however, a prevalence of 11% in adults is probably a reasonable estimate (1). Low-back pain is experienced by a significant portion of those with chronic non-cancer pain (2, 3).
A recently described subset of low-back pain is “pelvic girdle pain” attributed to biomechanical failure to transfer load effectively from the trunk across the lumbopelvic region to the lower limbs (4–6). The terminology used to describe the pain associated with this failed load transfer is not standardized, resulting in a variety of terms being used, including: posterior pelvic pain since pregnancy, lumbopelvic pain, and pelvic girdle pain.
Whereas low-back pain is described as pain present between the 12th rib and the inferior gluteal fold, pelvic girdle pain occurs only between the posterior iliac crest and the inferior gluteal fold, and can be experienced in the anterior pelvis (4). Pelvic girdle pain may also affect the pelvic floor (7, 8). It has been most extensively studied in pregnant and post-partum women (often described as posterior pelvic pain since pregnancy), where its prevalence in that population is estimated to be approximately 20% (4). Although pelvic girdle pain may occur in men and other women, it has not been well studied in these populations.
Pelvic girdle pain is usually associated with disorders of the sacroiliac joints and symphysis pubis. Any dysfunction of the mobile sacroiliac joints can be a contributing factor (9, 10). It has been estimated that sacroiliac joint disorders represent approximately 13% of all low-back pain (4). Other factors associated with failed load transfer include laxity of the sacroiliac joint ligaments (4, 11), alterations in motor control (12–14), changes in muscle recruitment (15, 16), or changes in breathing patterns (17).
Classical physical examination methods do not easily identify sacroiliac and lumbopelvic causes of low-back pain. Although there are a number of physical examination tests for detecting problems with the sacroiliac joints, they must be performed as a battery of at least 4–5 manoeuvres in order to achieve adequate sensitivity in detecting dysfunction (4, 18, 19). Numerous studies of the reliability of sacroiliac joint tests have been criticized for poor methodology (19). Also, the majority of these tests are pain provocation tests, e.g. Patrick’s FABER test, Gaenslen’s test (18). In contrast, the Active Straight-Leg Raise (ASLR) (4, 20) and One-Leg Standing (OLS) (5, 21) tests do not provoke pain, but instead are attempts to assess the effectiveness of load transfer across the lumbopelvic region to the lower limbs (12, 22). Some physical examination tests are difficult to perform and require considerable experience, thus there is a need for simple tests that are reliable and can be taught easily to clinicians. Any test which facilitates the detection of failed load transfer would be useful, in order to initiate appropriate and timely referrals and/or treatments such as the use of a sacroiliac belt or core stability exercise programmes (23, 24).
The ASLR test has been found to be reliable, sensitive, and specific for detecting failed load transfer across the lumbopelvic region in pregnant and post-partum women (20, 25, 26). Failed load transfer may also be common in other women in general (17). When experienced manual physical therapists examined individuals (men and women) with chronic non-specific back pain using the ASLR, they reported test-retest reliability with kappa values of 0.70 (left side) and 0.71 (right side) (17).
Patients with posterior pelvic pain since pregnancy have been shown to have positive ASLR tests (26). A high internal consistency between the ASLR and Trendelenburg tests has also been reported (15). In addition, the ASLR test outcome correlates with the Quebec Back Pain Disability Questionnaire (26), indicating a relationship of positive ASLR test scores with functional impairment. However, there have been few studies examining the relationship of the ASLR test with other physical examination tests or with other disability assessments.
Another physical examination test of load transfer across the lumbopelvic region is the OLS test. The OLS test differs from the One-Leg Stork test, originally also known as the Gillet test. The original Gillet test is performed with the patient standing on one leg by flexing the contralateral hip and knee to the chest, while the examiner assesses the movement of the posterior superior iliac spine on the non-weight-bearing side (27). In contrast, the OLS test assesses load transfer from the lumbopelvic region to the weight-bearing leg (see methods section below). The OLS has good inter-rater reliability, with kappa values of 0.67 and 0.77 on the left and right sides, respectively, in non-pregnant individuals, when performed by experienced manual physical therapists (21). An adapted OLS test uses slightly different anatomical landmarks, with an additional stress component (Squat Stress Modification) that may enhance the sensitivity of the test (Lee, D; personal communication).
The inter-rater reliability of the ASLR test, the OLS test, or the adapted OLS test has not been extensively studied, either: (i) in women who are not pregnant or more than 9 months post-partum, with and without lumbopelvic pain; or (ii) with physicians as the examiners. In addition, the correlation of these tests with many clinically used pain and disability assessments has not been extensively studied. Finally, there have been no studies comparing the results of the ASLR and OLS tests.
The overall aim of this pilot study was to lay a foundation for future studies examining the prevalence and relevance of failed load transfer across the lumbopelvic region, as measured by the ASLR and OLS tests, in a general chronic pain centre population with low-back and/or pelvic pain. In this cross-sectional pilot study, the primary objective was to determine the inter-rater reliability of the ASLR and OLS tests in women by 3 examiners (2 physicians and a manual physical therapist). The secondary objectives were: (i) to explore the relationships between each of the ASLR and OLS tests and various pain and disability assessments; and (ii) to explore the relationship between the ASLR and OLS tests.
METHODS
This cross-sectional pilot study was approved by the Conjoint Health Research Ethics Board of the Faculty of Medicine, University of Calgary (Calgary, Alberta, Canada).
Subjects
Subjects were recruited over a 1-month period from Calgary (Alberta, Canada) through advertisements at the Alberta Health Services Chronic Pain Centre (AHS CPC), the Advanced Spinal Care Centre, and the community. Recruitment enlisted subjects with and without pain in order to obtain a range of scores to better evaluate the physical examination tests. A pre-study sample size calculation indicated that, with 32 subjects, a 2-tailed test, a null value of 0.00 and power of 80%, that a kappa value of 0.50 would be detectable (28).
The inclusion criteria were: English-speaking women 18–65 years of age, with or without low-back, buttock, and/or pelvic pain. The exclusion criteria were: currently pregnant, less than 9 months post-partum, or pain as a result of pregnancy or childbirth.
After informed consent, 34 subjects were initially enrolled. After data collection, 3 subjects were excluded because it was determined that their pain began during pregnancy or childbirth. This resulted in a final total of 31 subjects.
Study protocol
Subjects completed a questionnaire consisting of demographic information, a brief pain and medication history (analgesics, anti-inflammatories, muscle relaxants, opioids, antidepressants or anticonvulsants), as well as standardized pain and disability assessments, outlined further below. Three clinicians examined each subject independently, in a randomized order, using the physical examination tests below. These examiners were blinded in terms of the questionnaire and the subjects’ pain.
Examiners
Three right-handed examiners conducted the physical examination tests: one manual physical therapist with 9 years of experience, one experienced musculoskeletal physician with a prior degree in physical therapy (BScPT) and 8 years in practice as a specialist in physical medicine and rehabilitation, and one gynaecology fellowship trainee with 9 years of experience as a family physician.
Prior to the start of the study, the gynaecology fellowship trainee was introduced to the physical examination tests and had the opportunity to practice them in a clinical setting. Thereafter, 2 separate standardization sessions for the physical examination tests were held 6 days apart, using staff members from the AHS CPC as volunteer subjects. At each of the 2 sessions, the volunteers were first examined separately by each examiner, and then the results were compared. Each volunteer was then re-examined and reviewed together by all of the examiners and the principal investigator (PB).
Physical examination tests
Active Straight-Leg Raise test (4, 20). While lying supine, the subject raised her leg by flexing at the hip with the knee extended, alternating between left and right (3–4 times per side) such that the heel was 20 cm high off the examination table each time. Reading from a standardized script, the examiner then asked the subject to score the effort required to lift each leg on a 6-point scale: 0: not difficult at all; 1: minimally difficult; 2: somewhat difficult; 3: fairly difficult; 4: very difficult; and 5: unable to do task. Subjects were reminded that they were reporting effort and not pain. The scores from each leg were added together, giving a total score out of 10. A positive test was any score greater than zero (4, 29).
One-Leg Standing test (5, 21). The subject stood with her back to the examiner. To examine the right side, the examiner placed the right thumb on the subject’s right posterior superior iliac spine (PSIS) and the remainder of the right hand on the right iliac crest and right ilium, while the left thumb was placed on the right inferior lateral angle (ILA) of the sacrum. The subject then raised her left knee to the waist (90º flexion at hip and knee) while the examiner attempted to detect any anterior or posterior rotation of the right ilium with respect to the sacrum. This was repeated to a maximum of 4 trials, if needed. Similarly, to examine the left side, the left thumb was placed on the left PSIS and the right thumb on the left ILA of the sacrum, and the subject’s right knee was raised.
In the standard OLS test, the test was considered positive if there was any detectable anterior rotation of the ilium upon the sacrum (sacral counter-nutation). If, after 4 trials, the examiner did not palpate any movement of the ilium, or if the ilium rotated posteriorly (negative test with sacral nutation), the examiner repeated the same manoeuvre, but with the Squat Stress Modification (Lee, D; personal communication), a more subtle finding, described as follows. After raising the knee as before, the subject was asked to slowly squat by flexing less than 90º at the knee of the weight-bearing leg. The test was also positive if the examiner palpated any anterior rotation of the ilium when the subject squatted. The test was negative if, with either manoeuvre, the examiner did not palpate any movement of the ilium or any anterior rotation of the ilium.
The test score was: 0: no anterior rotation of the ilium with either Standard OLS test or Squat Stress Modification; 1: anterior rotation of the ilium only on the OLS test with Squat Stress Modification; 2: inconsistent anterior rotation of the ilium on the Standard OLS test (at least 1 trial out of 4); or 3: obvious anterior rotation of the ilium on the Standard OLS test. The OLS test was positive for any score greater than zero.
Standardized pain and disability assessments
Standardized pain and disability assessments relevant to a clinical pain practice were chosen to explore their relationships with the ASLR and OLS tests. The Numeric Pain Rating Scale (NPRS) (30) was used to rate each subject’s pain on an 11-point scale from 0 to 10. The location, extent, and descriptors for pain were drawn on a Pain Location Diagram displaying the human body using the same numbering system as Margolis (31), modified with the addition of a separate diagram of the pelvic floor. For each subject, the total number of indicated pain areas on the human body diagram was recorded. The pelvic floor areas were used to help define the pain groups, but not used when totalling the number of pain areas for determining pain severity, because this pelvic floor component has not yet been validated. The Roland-Morris Disability Questionnaire (RMDQ) lists 24 different potential disabilities from back pain (32). The Neuropathic Pain Diagnostic Questionnaire (DN4) contains 7 questions concerning the characteristics and associated symptoms of pain (33). The Functional Pelvic Pain Scale (FPPS) grades each of 8 different functional domains on a scale from 0–4 (34). In all scales, higher scores indicate more severe pain or more functional impairment.
Pain group definitions
An example of a completed pain location diagram is shown in Fig. 1. A transparent pain location diagram template with specific numbered areas, as described by Margolis (31), was overlaid onto each subject’s completed pain diagram. Each area was included if any part of it was filled in by each subject. These areas were used to define 3 different pain groups: Group A: no low-back or pelvic pain; Group B: low-back pain without pelvic pain; and Group C: both low-back and pelvic pain. Low-back pain was defined as the area below the 12th ribs extending to the inferior gluteal folds (any of areas of 36–37, corresponding to the left and right flanks as well as any of areas 38–39, corresponding to the left and right buttocks). Pelvic pain included anterior pelvic pain (area 16, corresponding to the symphysis pubis) and/or pelvic floor pain (any filled-in areas of the pelvic floor diagram).
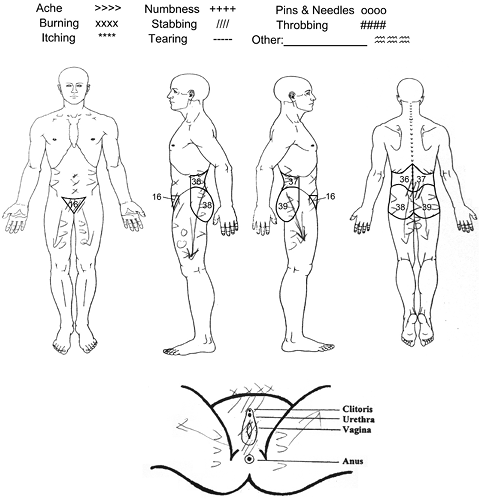
Fig. 1. Example of a subject’s completed pain location diagram. On the body pain diagram, only the numbered areas used to define the pain groups are displayed (areas 16 and 36–39).
Statistical analyses
Inter-rater reliability. Kappa statistics for inter-rater reliability for all 3 raters were calculated with 95% confidence intervals (95% CI) for both the ASLR and the OLS tests. Percentage agreement between the 3 examiners was also calculated.
Sensitivity and specificity. When all 3 raters agreed on whether the ASLR test was positive or negative, the subject was classified as positive or negative, and the percentage of positive subjects calculated. The results of the ASLR test (positive or negative) were cross-tabulated with the presence or absence of low-back or pelvic pain (yes vs no) to calculate the sensitivity and specificity of the ASLR test. Sensitivity and specificity were calculated with the data when all 3 raters agreed, as well as separately for each individual rater across all 31 subjects.
Relationship with pain and disability assessments. For the ASLR test, the scores (0–10) from the 3 raters were averaged for each of the 31 subjects. Box-plots demarcating the median and first and third quartiles were then created to illustrate the relationship between the 3 pain groups (A–C) and the mean ASLR test scores. Differences between the pain groups were tested using the Kruskal-Wallis (K-W) rank test. The relationship between each of the pain and disability assessments and the mean ASLR test scores was examined using a scatterplot and the Spearman rho correlation coefficient. To examine the relationship between the mean ASLR test scores and the number of different pain medications taken by each subject, subjects were divided into 3 groups: no pain medications, 1–2 and 3–5 different pain medications. These groups were plotted against the mean ASLR test scores using box-plots, and differences were tested statistically using the K-W rank test.
The Stata Data Analysis and Statistical Software (StataCorp, Texas, USA) was used for all statistical analyses.
RESULTS
The mean age of the 31 women in this cross-sectional pilot study was 41 years (standard deviation 11). Subjects were categorized into the 3 defined pain groups: Group A: no low-back or pelvic pain (n = 11); Group B: low-back pain without pelvic pain (n = 13); and Group C: both low-back and pelvic pain (n = 7).
Inter-rater reliability of the Active Straight-Leg Raise test
In the primary analysis of the inter-rater reliability of the ASLR test among all 3 examiners, the kappa value was calculated as 0.87 (95% CI 0.77–1.00). All 3 raters agreed on 28/31 subjects (90% percentage agreement), of which 13 were rated as positive (13/28 = 46%) and 15 were rated as negative (15/28 = 54%) (Table I).
|
Table I. Contingency table to calculate the sensitivity and specificity of the Active Straight-Leg Raise (ASLR) test for detecting low-back pain with or without pelvic pain. Positive/negative ASLR tests of subjects were included for which all 3 examiners agreed, and categorized into 3 pain groups (n = 28 after 3 were excluded due to non-agreement) |
||||
|
Low-back pain n |
Low-back and pelvic pain n |
No pain n |
Total n |
|
|
ASLR positive |
7 |
5 |
1 |
13 |
|
ASLR negative |
5 |
0 |
10 |
15 |
|
Total |
12 |
5 |
11 |
28 |
Sensitivity and specificity of the Active Straight-Leg Raise test
For detecting low-back and/or pelvic pain when all 3 raters agreed (28/31 subjects), the sensitivity and specificity of the ASLR test was calculated to be 71% (95% CI 44–90%) and 91% (95% CI 59–100%), respectively. In 3 cases the raters did not agree, so we present the sensitivity and specificity for each individual rater across all 31 subjects. With all 31 subjects, the sensitivities for each rater were as follows: Rater 1: 65% (95% CI 41–85%); Raters 2 and 3: 70% (95% CI 46–88%). The specificity of each individual rater remained the same at 91% (95% CI 59–100%).
Active Straight-Leg Raise test scores among the 3 pain groups
There was a significant difference in the mean ASLR test scores among the 3 pain groups (Fig. 2). The mean ASLR score increased progressively from mostly (10 of 11) negative scores in Group A (no low-back or pelvic pain) to positive scores in Group B (low-back pain without pelvic pain). The highest scores were in Group C (both low-back and pelvic pain).
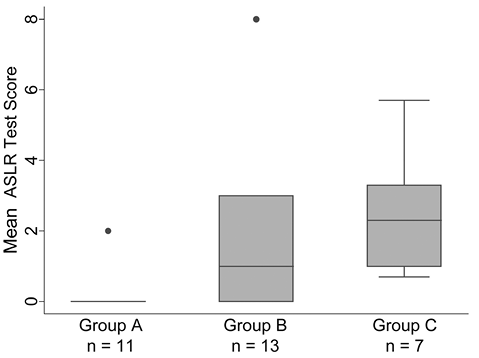
Fig. 2. Distribution of Active Straight-Leg Raise (ASLR) test scores by pain group. Group A: no low-back or pelvic pain; Group B: low-back pain without pelvic pain; and Group C: both low-back and pelvic pain. Kruskal-Wallis rank test χ2 = 12.67, 2 d.f., p = 0.002. •: outliers.
The positive relationships between the ASLR test scores and each of the pain and disability assessments: FPPS, RMDQ, number of reported pain areas of the Pain Location Diagram, NPRS and DN4 questionnaire are summarized in Table II. Data for the FPPS and RMDQ are shown in Figs 3 and 4.
Higher mean ASLR test scores were associated with more pain medications being taken (K-W test χ2 = 12.87, 2.d.f., p = 0.0016) (figure not shown).
|
Table II. Relationships between the Active Straight-Leg Raise test and pain and disability assessments |
|
|
Pain and disability assessment |
Spearman’s rho |
|
Functional Pelvic Pain Scale |
0.77* |
|
Roland-Morris Disability Questionnaire |
0.70* |
|
Pain Location Diagram (excluding pelvic floor), number of areas |
0.70* |
|
Numeric Pain Rating Scale: mean |
0.66* |
|
Neuropathic Pain Diagnostic Questionnaire |
0.55* |
|
*p < 0.005. |
|
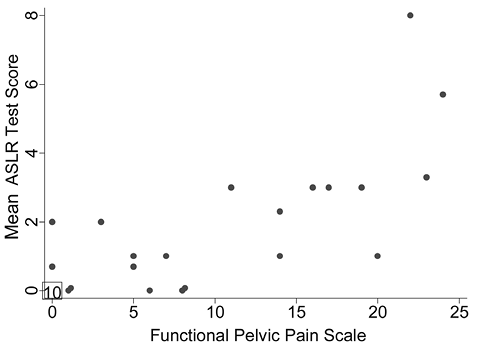
Fig. 3. Relationship between the Active Straight-Leg Raise (ASLR) test scores (mean of all 3 raters) and the Functional Pelvic Pain Scale (FPPS) scores for all 31 subjects. Note: data from 10 individuals who scored 0 on both the FPPS and ASLR test were plotted at (0, 0). Spearman rho = 0.77.
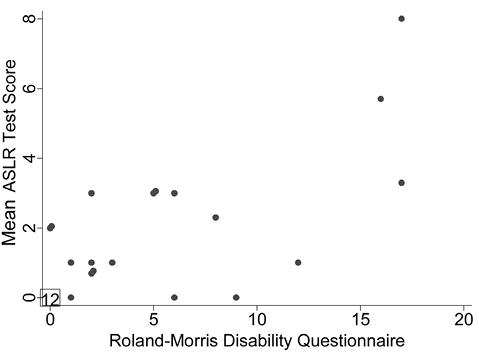
Fig. 4. Relationship between the Active Straight-Leg Raise (ASLR) test scores (mean of all 3 raters) and the Roland-Morris Disability Questionnaire (RMDQ) scores for all 31 subjects. Note: data from 12 individuals who scored 0 on both the RMDQ and ASLR test were plotted at (0, 0). Spearman rho = 0.70.
Inter-rater reliability of the One-Leg Standing test
The OLS test had poor inter-rater reliability with kappa values of –0.02 (95% CI –0.16 to 0.30) and 0.14 (95% CI –0.07 to 0.42), for the left and right sides, respectively. Due to the very low kappa values and percentage agreement for the OLS test, further analysis of its relationship with the pain and disability assessments was not explored. The relationship between the ASLR and OLS tests was also not explored.
DISCUSSION
The ASLR test is a physical examination test used to detect failed load transfer across the lumbopelvic region (4, 20). It has good inter-rater reliability in women with posterior pelvic pain since pregnancy (PPPP) (20, 25, 26), as well as in men and women with chronic non-specific back pain (17). Our cross-sectional pilot study has shown that the ASLR test has good inter-rater reliability in a less-studied population: women who are either not pregnant or at least 9 months post-partum, with a spectrum of pain (ranging from no pain, to severe low-back pain with or without pelvic pain). This reliability was demonstrated by both a musculoskeletal and non-musculoskeletal physician, as well as by an experienced manual physical therapist. In our study, the ASLR test was found to have a sensitivity of 71% and a specificity of 91% for low-back and/or pelvic pain. Furthermore, the mean ASLR test score increased as the distribution of body pain involvement increased. That is, those with both low-back and pelvic pain (Group C) tended toward higher ASLR test scores than those with low-back pain without pelvic pain (Group B). Those without low-back or pelvic pain (Group A) typically had negative ASLR tests. In addition, we found positive correlations between the mean ASLR test scores and various pain and disability assessments, including the FPPS and RMDQ. Those taking more pain medications also had higher ASLR test scores. Our secondary data suggest that, in those with low-back and/or pelvic pain, higher ASLR test scores were associated with greater functional impairment and pain.
The OLS test is another physical examination test used to evaluate failed load transfer across the lumbopelvic region (5, 21). In our study, the OLS test was shown to have poor inter-rater reliability and thus further analysis was not completed. The 4-point scale (0–3) for the modified OLS test included subtle positives (scores of 1 and 2), which may have compromised inter-rater reliability. However, post-hoc exploratory analyses assuming a standard OLS test with only a 2-point scale (scores of 0, 1, 2 being negative and only 3 being positive) also had similarly low kappa values (data not shown). Other studies have also shown poor reliability for palpation of bony landmarks of the low-back (35, 36), as well as for different sacroiliac joint provocation and mobility tests (37, 38). Although extensive training programmes for palpation tests may improve inter-rater reliability (39), physical examination tests should ideally be simple, easily taught and reliable. In our study, the ASLR test meets these criteria, whereas the OLS test does not.
This cross-sectional pilot study had a few limitations: (i) limited sample size: although this is a small study, the sample size of 31 is comparable to other studies in the literature (21, 25), and is of adequate size for determining inter-rater reliability and exploring relationships with pain and disability assessments. This pilot study forms a basis for a future larger-scale study; (ii) recall bias: subjects were examined in a randomized, but sequential, order by 3 examiners on the same day. Thus, there may have been recall bias from the subjects regarding the ASLR test, which would result in higher kappa values and better inter-rater reliability. This situation could have occurred despite each subject being distracted by the OLS test in between each successive ASLR test by the 3 examiners. While the risk of recall bias may be minimized by delaying the ASLR test by more than one day or week between examiner assessments, it is possible that subjects may have biomechanical differences on different days that would affect the consistency of the ASLR test. In addition, although the ASLR test relies on subjective reporting of effort, it has been shown to correlate with the objective component of the test (40).
Based on our study, as well as previous studies (4, 25, 26), the ASLR test is relevant for the detection of failed load transfer across the lumbopelvic region in patients presenting with low-back, buttock, and/or pelvic pain (anterior pelvic or pelvic floor pain), and could be used by many disciplines including: family practice, gynaecology, orthopaedics, neurology, neurosurgery, rheumatology, and physical medicine and rehabilitation. The ability to successfully detect failed load transfer in patients with low-back and/or pelvic pain may encourage the routine use of the ASLR test, enabling early initiation of appropriate conservative treatment strategies. In contrast, the OLS test proved challenging for our examiners to reliably execute in the present study, which raises the question of its utility by different clinicians with varying levels of expertise and experience.
Previous studies of sacroiliac joint pain provocation and mobility tests have not shown good validity, due, in most part, to poor methodology, in particular poor reliability of the tests (36, 41). Most recently, in pregnant women with lumbopelvic pain, the severity of pain, its associated disability, and the prevalence of failed load transfer as measured by the ASLR test has been reported (42). Since the ASLR test has been shown by our study and others (17, 20, 25, 26) to have good inter-rater reliability, future studies may be helpful to examine its validity in a larger population, including both male and female subjects with and without low-back and/or pelvic pain.
In conclusion, this cross-sectional pilot study has shown that the ASLR test has good inter-rater reliability in detecting failed load transfer across the lumbopelvic region in women with a spectrum of pain ranging from no pain, to severe low-back pain with or without pelvic pain. The OLS test had poor inter-rater reliability in our study. Higher positive scores for the ASLR test were associated with greater levels of pain, disability and pain medication use. Further studies are required to determine the prevalence and significance of failed load transfer across the lumbopelvic region, as measured by the ASLR test, in a larger group of subjects, including men and women with and without low-back and/or pelvic pain.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Andry Vleeming and Diane Lee for their teaching and helpful conversations while preparing the study. The authors would also like to acknowledge assistance from the AHS CPC during the course of this study.
REFERENCES
