Ulla Christensen, PhD, Lone Schmidt, DMSci, Charlotte Ørsted Hougaard, MSc, Karsten Thielen, MD, Else Nygaard, PhD and Rikke Lund, PhD
From the Department of Public Health, Section of Social Medicine, University of Copenhagen, Copenhagen, Denmark
OBJECTIVE: Musculoskeletal pain and avoidant coping predicts sickness absence, but how these 2 predictors relate to each other is unknown. We examined the main and combined effects of musculoskeletal pain and avoidant, behavioural coping on incidence of sickness absence.
Design and subjects: Prospective cohort study of a sample of middle-aged Danes, economically active in 2006, reporting functional limitations due to musculoskeletal pain, n = 3115.
METHODS: Data included surveys from 2000 and 2006 and register data from 2007. Outcome was sickness absence exceeding 2 consecutive weeks in 2007. The main effect of self-reported pain frequency and avoidant coping on sickness absence was analysed by multivariate logistic regression. The combined effect was calculated as departure from multiplicativity and by the inclusion of a product term.
RESULTS: Daily pain and use of avoidant coping were both associated with sickness absence in multiple adjusted analyses, odds ratio (OR)daily pain = 1.83 (95% confidence interval (CI) 1.51–2.21) and ORavoidant coping = 1.52 (95% CI 1.24–1.88) (main effects). A modest combined effect of musculoskeletal pain and avoidant coping on sickness absence was suggested (p = 0.286).
CONCLUSION: Avoidant coping and daily pain are both associated with sickness absence, but showed no strong signs of interactive effects. Clinicians should be aware of both factors.
Key words: pain; avoidant coping; sickness absence; main effect, combined effect.
J Rehabil Med 2013; 45: 00–00
Correspondence address: Ulla Christensen, Department of Public Health, University of Copenhagen. Øster Farimagsgade 5, PO Box 2099, DK-1014 Copenhagen K, Denmark. E-mail: Ulla.Christensen@sund.ku.dk
Accepted May 3, 2013; Epub ahead of print Sep 3, 2013
Introduction
Musculoskeletal pain is a common cause of disability and sickness absence in industrialized and developing countries, and causes considerable social and economic burdens on society and on the affected individual (1–3). Several studies have indicated that permanent withdrawal from the labour market is a frequent consequence of long-term sickness absence, i.e. the longer the sick leave, the more difficult it seems to be for sick-listed individuals to return to work (4, 5). Two factors have been associated with long-term sickness absence among individuals with musculoskeletal disorder; pain intensity and coping. In a Dutch prospective cohort study among 253 workers on sick leave, Lötters & Burdorf (6) found high pain intensity to be a major prognostic factor for duration of sickness absence. Holtermann et al. (7) showed how pain intensity predicted long-term absence in a longitudinal study among 1524 Danish employees with neck-shoulder and low-back pain.
According to the transactional coping model of Lazarus & Folkman (8), coping is considered to be a process that starts with an event that is primarily appraised by the individual as either threatening, harmful or challenging. As such, the individual is confronted with a condition that exceeds its resources and endangers its well-being. Pain-coping strategies have been classified according to 2 frequently used dimensions; cognitive and behavioural. Katz et al. (9) have described cognitive strategies to include pain management by using techniques such as counting, distraction, imagery, and behavioural strategies to include actions attempting to manage pain, by taking pain medication, seeking social support or resting in bed. Furthermore, 2 other categorizations regarding pain coping have been suggested; an attentional strategy and an avoidant strategy. Using attentional techniques (such as stretching or exercising the area of pain) would characterize an individual who tries to manage pain by directing focus on the source of pain. Avoidant strategies involve the opposite, i.e. resting, restriction of activities, or taking medication (9). Coping strategies are associated with sickness absence (10, 11), and in a review of studies on low back pain and determinants for sickness absence, Werner & Côte (12) reported how avoidant coping (e.g. fear avoidance behaviour and reduced activity levels) has been associated with both length and onset of sickness absence. The results from the few studies that have explored how pain and coping interact are complex. In a longitudinal study of patients with newly developed musculoskeletal pain, the use of passive coping (e.g. praying, hoping and wishful thinking) was related to higher pain intensity after 26 weeks (13), and Klapow et al. (14) found that patients with high levels of pain reported more reliance on avoidant coping strategies (e.g. avoidance, self-blame and wishful thinking) in contrast to patients with low levels of pain. On the other hand, a qualitative study among patients with chronic musculoskeletal pain in the UK, showed that pain by itself was the underlying barrier from which most other barriers to work stem (15). Insight into how pain and coping strategy may interact and affect decisions on sickness absence could be valuable for clinicians who advise patients with pain conditions.
The aim of the present study was to investigate the main effects and combined effect of musculoskeletal pain frequency and avoidant, behavioural coping on incidence of sickness absence in a Danish cohort of middle-aged men and women. In this study, coping has been measured specifically according to the stressor, pain. The analyses were adjusted for relevant socio-demographic factors. We hypothesized that the combined effect of pain frequency and an avoidant, behavioural coping strategy would increase the risk of long-term sickness absence to a higher degree than each factor alone.
Methods
Study design and population
This study is based on a prospective design and 2 linked databases. Thus, data about sickness absence in 2007 were based on information from the Danish National Register on Social Transfer Payments, while data about coping strategies and other personal characteristics were obtained from survey data collected in Autumn 2006. The study population was derived from the Danish Longitudinal Study on Work, Unemployment and Health, which was designed to investigate the associations between psychosocial factors, unemployment and health with a baseline in 2000 and follow-up in 2006. The population for the baseline survey data in 2000 included 2 population samples drawn from the “AKF longitudinal Register” maintained by the Danish Institute of Governmental Research: (i) a random sample of individuals 40- and 50-years-old (cohort 1 and 2); and (ii) a high-risk population drawn as a random sample of 36–54-year-olds (cohort 3) who had been unemployed at least 70% of the time during the last 3 years before October 1999 (total study population, n = 15,227). Of the total study population, 9,875 returned a completed questionnaire (response rate 65%). In 2006, a follow-up questionnaire was sent to the surviving respondents, now aged 42–60 years (n = 8,916) and a completed questionnaire was returned by 6151 respondents (response rate 69%). The participation rate in this follow-up survey was significantly higher among women than men, among native-born Danes than immigrants, among employed than unemployed, and among persons with > 10 years of education (χ2 test, all p-values < 0.001). There was no significant difference in contact frequency with the general practitioner (GP) between non-participants and participants in cohort 1, while more respondents in cohorts 2 and 3 had been in contact with the GP (p = 0.001 and p = 0.003, respectively) (Fig. 1).
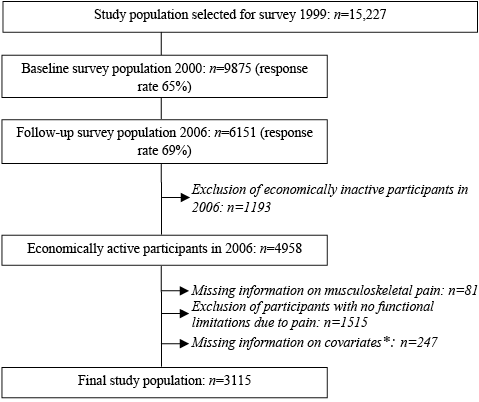
Fig. 1. Study population. *Occupational social class; cohabitation status; stressors due to physical exposures in the work environment; psychosocial stressors at work; depression.
For this study we included only those respondents who were economically active (employed or self-employed) in 2006. Moreover, all respondents agreeing on some degree of functional limitations were included in the study and would go through the coping questionnaire. The information on functional limitations due to musculoskeletal pain was based on the following question: “Have you ever experienced so much pain in your back or other joints or muscles that it has been difficult for you to perform your usual daily activities (e.g. work, household activities, sports, physical exercise)?” Response options were: “no”; “yes, somewhat”; “yes very much”.
The final study population encompassed 1,377 men and 1,738 women. According to the Danish Act on Research Ethics, projects based on register or survey data do not need approval from the National Committee on Health Research Ethics. In compliance with the Danish Act on Processing of Personal Data, the project was approved by the Danish Data Protection Agency, j.nr. 2001-54-0180.
Measures and procedures
Outcome. Information on sickness absence was derived from the National Register on Social Transfer Payments, which contains information on all sickness absence compensations in Denmark. After 2 weeks, employers are entitled to reimbursement from the municipality corresponding to the sickness benefit. Respondents with one or more episodes of sickness absence periods exceeding 2 consecutive weeks in 2007 were categorized as having the outcome. Seventeen percent of the study population had an episode of sickness absence exceeding 2 weeks in 2007.
Determinants
Pain frequency was measured in 2006 by self-reported incidence of musculoskeletal pain. Three questions were included: Do you experience pain in the upper part of your back and neck?, Do you experience pain in your lower back?, Do you experience pain in other joints (e.g. fingers, shoulder, hip, knee or ankle?), and the response options were: (1) daily; (2) a couple of times during the week; (3) a couple of times during the month; (4) only once a month; (5) seldom; (6) never. Musculoskeletal conditions and symptoms are very frequent in the Danish population (16) and consequently for the present study we dichotomized into “daily pain” in 1 or more of the 3 locations (33% of the study population) and “no daily pain”, which included response options 2–6.
Coping. Folkman & Lazarus (17) recommend that questionnaires on coping should measure coping strategies in relation to a specific stressor. Consequently, and based on the transactional coping model by Lazarus & Folkman, we developed a stressor-specific coping questionnaire in 2000. This instrument was initially developed from a Danish intervention study among patients with back pain (study population n = 537, including a control group). This study consisted of a survey, which included open-ended questions on the respondents’ behavioural coping with back-pain, and 11 semi-structured qualitative interviews with intervention participants (18).
Responses about behavioural coping from both survey and interview transcripts were categorized according to the 8 dimensions in the 66-item Ways of Coping Questionnaire (WOCQ) (8, 17). Only 6 dimensions were identified in the empirical data (confronting coping, self-controlling, seeking social support, accepting responsibility, escape-avoidance, planful problem-solving). Based on the categorization we developed 10 items. The items were validated for content and face validity by 2 focus group interviews with outpatients in a rehabilitation unit, in which we also encouraged the interviewees to discuss positive reappraisal of their pain experiences. None of the group members referred to elements of this dimension, and consequently it was not included in the questionnaire.
A test-retest of the 10 items was conducted among 112 adult individuals attending different kinds of rehabilitation and exercise programmes designed for individuals with back pain. The time interval was 8 days. The weighted Kappa coefficients ranged from κ = 0.76 to κ = 0.54 for the items on planful problem-solving (3 items), escape-avoidance (1 item), seeking social support (2 items) and self-controlling (1 item), while the coefficients for items on confronting coping (2 items) and accepting responsibility (1 item) were 0.27 and 0.25, respectively. To clarify, 1 item on confronting coping was split into 2 separate items and the wording on accepting responsibility was changed. Finally, the remaining items were pilot-tested in a study population drawn from the same sampling frame as the main survey (n = 993). The pilot-test showed good distribution of scores across all response categories apart from the item on accepting responsibility, which consequently was reformulated.
We defined the items into 2 scales that covered 2 conceptually, but not mutually exclusive coping strategies, 6 items on attentional, behavioural coping, and 4 items on avoidant, behavioural coping (Table I). This is in accordance with the categorization of behavioural pain coping strategies into attentional and avoidant suggested by Katz et al. (9). The item on getting in contact with GP was included in both scales because it encompasses aspects of both attentional, behavioural coping and avoidant coping: attentional, behavioural coping, because in the Danish healthcare system you need referral from a GP for medical examination and treatment from hospitals, specialists, physiotherapists, and chiropractors. Seeing the GP could also reflect a more avoidant way of coping, as it is the only way to get prescription drugs.
|
Table I. Items on avoidant, behavioural coping with musculoskeletal pain |
|
Avoidant, behavioural coping |
|
I was less physically active than usual |
|
I used stronger medicine than usual |
|
I stayed in bed most of the time and rested because of pain |
|
I was in contact with a medical doctor |
The Cronbach’s coefficient alpha was 0.71 for the avoidant, behavioural scale and 0.64 for the attentional, behavioural coping scale, which indicated a fair degree of internal reliability for the 2 scales. Cronbach’s coefficient is, however, sensitive to departure from normality and the coping scales did not fit a normal distribution. Therefore, we used confirmatory factor analysis to study how well the pattern of intercorrelations between items fitted the conceptually developed 2 coping scales. The Goodness-of-Fit-Index (GFI) was 0.96, which confirmed the 2-factor structure of the included coping items. Response options in the questionnaire were: all of the time (0), some of the time (1), a little of the time (2), and not at all (3). We summed the scores for the 2 scales separately, ranging from of 0 to 12 for the avoidant subscale and from 0 to 18 for the attentional, behavioural subscale. We investigated whether the coping scales could be used as dichotomized outcome measures. Initial analyses showed no associations between attentional, behavioural coping and sickness absence. As a consequence, the present study presents only the analyses regarding the avoidant, behavioural coping scale. Based on sensitivity analysis in this study population the avoidant scale was dichotomized into high use of avoidant coping (scoring < 7) and low use of avoidant coping (scoring ≥ 7).
Covariates
Apart from basic demographic variables (occupational social class, gender, age and cohabitation status (living with or without a partner)) we also included relevant physical and psychosocial work environmental factors. Physical exposures at the work place have been associated with both musculoskeletal disorders and sickness absence (7, 19–20). We included stressors due to physical exposures in the work environment based on 5 items developed and used in surveys in the National Research Centre for the Working Environment in Copenhagen (19). The items were: work in a stooping posture; work involving repeatedly twisting the back; pulling or pushing heavy burdens; lifting or moving heavy burdens; vibrations. Response options were: always (3), often (2), sometimes (1) and never (0). Items were summed to obtain a scale score with the range 0–15. The distribution curves were studied in order to choose appropriate cut-off points and 3 categories were used, low exposure (scoring 0), medium exposure (scoring 1–4) and high exposure (scoring ≥ 5). Measures on psychosocial stressors at work were derived from The Copenhagen Psychosocial Questionnaire, which has been empirically tested in a survey of a representative sample of 1,858 working Danes between 20 and 60 years of age (20). Neither of these measures was associated with sickness absence in the analytical model. The same applied for cohabitation and age (data not shown). Gender and stressors due to physical exposures remained significant in both the preliminary and the final models, as did occupational social class, measured by occupation and coded into occupational social class I–V in accordance with the standards of the Danish National Centre for Social Research and similar to the British Registrar General’s Classification I–V. Due to the association between pain and depression (21, 22) and between avoidant coping and depression (23, 14) we included data on depression using The Major Depression Inventory (MDI). This measurement is based on 12 items of depressive symptoms and a score in the range 0–50. The scale has been shown to hold good validity, and it reflects the criteria for diagnosis listed in the International Satistical Classification of Diseases and Related Health Problems – Tenth Revision (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders – Forth Edition (DSM-IV) (24). Major depressive disorder is constructed according to the DSM-IV algorithm and corresponds to a score > 25 point (24).
Statistical analyses
The analyses of the association between pain and sickness absence included bivariate contingency analyses with χ2 tests, as did the analyses of the covariates, pain frequency and sickness absence. By multivariate logistic regression the association between pain frequency, sickness absence and avoidant coping was analysed, adjusted by physical exposures in work environment, gender and occupational social class. Initial regression models included each covariate separately, and subsequently both forwards and stepwise backwards elimination was conducted to reduce the full models to a stage where only significant (p < 0.05) predictor variables remained. According to the Strobe statement a combined effect analysis is recommended when calculating interaction (25), and so the combined effect of pain and avoidant coping was calculated as departure from multiplicativity and tested by including product terms into the logistic regression model. All analyses were performed with SAS, version 9.1.3.
Results
Table II shows that the incidence of sickness absence > 2 weeks was higher among individuals with daily high pain frequency, among those with high use of avoidant coping, and among women (all p-values < 0.001). There was a graded incidence of sickness absence along the occupational social classes, i.e. lower occupational social classes had a higher incidence of sickness absence. Furthermore, higher stressors due to physical exposures in the work environment were associated with higher incidence of sickness absence (type 3 for both occupational social class and physical exposures, p < 0.001). Finally, individuals with a major depression had a significantly higher incidence of sickness absence.
|
Table II. Incidence of sickness absence > 2 weeks in 2007 by musculoskeletal pain, avoidant, behavioural coping, gender, occupational social class, stressors due to physical exposures and major depression. Danish men and women 44–62 years old (n = 3,115) |
||
|
All n |
Cases n (%) |
|
|
Daily musculoskeletal pain |
1,089 |
291 (26.7) |
|
No daily musculoskeletal pain |
2,026 |
278 (13.7) |
|
Low use of avoidant, behavioural coping |
2,029 |
391 (16.1) |
|
High use of avoidant, behavioural coping |
517 |
178 (25.6) |
|
Male gender |
1,377 |
197 (14.3) |
|
Female gender |
1,738 |
372 (21.4) |
|
Occupational social class I (highest) |
185 |
9 (4.6) |
|
Occupational social class II |
454 |
60 (11.6) |
|
Occupational social class III |
657 |
108 (14.1) |
|
Occupational social class IV |
712 |
217 (23.3) |
|
Occupational social class V (lowest) |
538 |
175 (24.5) |
|
Stressors due to high physical exposures |
758 |
254 (25.0) |
|
Stressors due to medium physical exposures |
885 |
186 (17.3) |
|
Stressors due to low physical exposures |
903 |
129 (12.5) |
|
Major depression |
83 |
55 (39.8) |
|
No major depression |
2,463 |
514 (17.2) |
Multivariate logistic regression showed mutually adjusted odds ratios for sickness absence of 2.07 (95% confidence interval (CI) 1.71–2.52) by daily pain and of 1.49 (95% CI 1.19–2.52) by high use of avoidant, behavioural coping (Table III, model 1). Neither occupational social class, physical work environment, gender nor depression confounded this association, thus OR for sickness absence by daily pain in the fully adjusted model was = 1.78 (95% CI 1.47–2.16) and OR for sickness absence by high use of avoidant coping = 1.45 (95% CI 1.18–1.80), (model 5) (Table III).
|
Table III. Adjusted odds ratios (OR) for sickness absence > 2 weeks by daily musculoskeletal pain and avoidant, behavioural coping, 44–62-year-old Danish men and women, multivariate logistic regression analysis (n = 3,115) |
|||||
|
Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95 % CI) |
Model 4 OR (95 % CI) |
Model 5 OR (95% CI) |
|
|
Musculoskeletal pain Weekly/monthly/seldom and never Daily |
1 2.07 (1.71–2.52) |
1 2.11 (1.75–2.54) |
1 1.94 (1.60–2.34) |
1 1.86 (1.54–2.26) |
1 1.78 (1.47–2.16) |
|
Avoidant coping Low use High use |
1 1.49 (1.19–1.86) |
1 1.61 (1.31–1.98) |
1 1.54 (1.25–1.90) |
1 1.52 (1.23–1.87) |
1 1.45 (1.18–1.80) |
|
Gender Men Women |
1 1.51 (1.24–1.83) |
1 1.46 (1.20–1.78) |
1 1.55 (1.27–1.89) |
1 1.54 (1.26–1.88) |
|
|
Occupational social class I II III IV V |
1 2.43 (1.17–5.01) 2.87 (1.42–5.80) 4.90 (2.45–9.78) 5.36 (2.68–10.8) |
1 2.37 (1.14–4.89) 2.60 (1.28–5.27) 4.14 (2.06–8.32) 4.24 (2.09–8.62) |
1 2.36 (1.14–4.88) 2.55 (1.26–5.18) 4.08 (2.03–8.21) 4.22 (2.07–8.58) |
||
|
Stressors due to physical work environment Low Medium High |
1 1.14 (0.88–1.47) 1.57 (1.20–2.04) |
1 1.11 (0.86–1.44) 1.51 (1.16–1.97) |
|||
|
Major depression No major depression Major depression |
1 2.02 (1.39–2.93) |
||||
|
Model 1: musculoskeletal pain and avoidant, behavioural coping, mutually adjusted; Model 2: model 1 and gender; Model 3: model 2 and occupational social class; Model 4: model 3 and stressors due to physical work environment; Model 5: model 4 and major depression. CI: confidence interval. |
|||||
Table IV shows the main and combined effects of musculoskeletal pain and avoidant coping on sickness absence. In these analyses we constructed combined variables of daily pain and avoidant coping and adjusted for covariates (gender, occupational status, stressors due to physical exposures in work environment and depression). We found separate effects of daily pain and high use of avoidant coping on sickness absence, OR = 1.83 (95% CI 1.51–2.21) and OR = 1.52 (95% CI 1.24–1.88), respectively. Being exposed both to daily pain and use of avoidant behavioural coping was associated with an almost 3-fold increase in sickness absence (OR = 2.71, 95% CI 2.04–3.62) compared with the unexposed subjects, which is slightly stronger than the expected multiplicative effect of 2.15 (1.67 × 1.29). This indicates a modest combined effect of musculoskeletal pain and avoidant coping on sickness absence. Including a product term in the analysis, showed a non-significant effect (p = 0.286).
|
Table IV. Main and joint effects of musculoskeletal pain and avoidant coping on sickness absence > 2 weeks, in a sample of 44–62-year-old Danish men and women (n = 3,115) |
||
|
n |
Multiple-adjusted ORa |
|
|
Musculoskeletal pain |
||
|
Pain weekly/monthly/seldom and never |
2,026 |
1 |
|
Pain daily |
1,089 |
1.83 (1.51–2.21) |
|
Avoidant coping |
||
|
Low use of avoidant coping |
2,420 |
1 |
|
High use of avoidant coping |
695 |
1.52 (1.24–1.88) |
|
Joint effect |
||
|
Pain weekly/monthly/seldom and never and low use of avoidant coping |
1,647 |
1 |
|
Pain weekly/monthly/seldom and never and high use of avoidant coping |
379 |
1.29 (0.95–1.75) |
|
Daily pain and low use of avoidant coping |
773 |
1.67 (1.33–2.09) |
|
Daily pain and high use of avoidant coping |
316 |
2.71 (2.04–3.62) |
|
Interaction |
||
|
p-value for interaction |
0.2862 |
|
|
aAdjusted for: gender, occupational social class, stressors due to physical work environment, major depression. OR: odds ratio. |
||
Discussion
The present analyses confirmed a strong association between musculoskeletal pain frequency, avoidant coping and long-term sickness absence exceeding 2 consecutive weeks after adjustment for the selected confounders. The combined effect analyses suggested only modest interactive effects between pain and avoidant, behavioural coping on sickness absence.
The robust association between pain frequency and sickness absence, and between high use of avoidant coping and sickness absence is in agreement with previous studies. Avoidant coping neither confounded the association between daily pain and sickness absence, nor was the association attenuated to a degree that might have indicated avoidant coping to be a potential mediator. As such, our study supports the findings of Boonen and co-authors (26) who, in a study of avoidant coping and disease status among patients with ankylosing spondylitis, showed that coping conceptually differs from pain and seems to be independent of pain. Our study adds further to this notion, as it was not conducted in a sample of pain patients with a specific diagnosis, but in a sample from a population study contributing to the knowledge about the interaction between pain and coping.
The modest combined effect of pain and avoidant coping on sickness absence raises the question of whether avoidant behavioural coping should be considered to be an adaptive or maladaptive strategy. Different pain-related cognitive and behavioural coping responses to pain have been associated with chronicity and disability in patients with musculoskeletal pain. This includes both fear-avoidance beliefs and pain-related fear and task persistence, including an enduring behaviour that may interrupt ongoing recovery with the risk of developing chronic pain and disability (27). Furthermore, Hasenbring et al. (27) have suggested that the enduring behaviour may not only be associated with subsequent disability, but, if focused on cognitive distraction and positive mood, it may have a less deleterious effect. Lazarus & Folkman (8) defined coping as “the constantly changing cognitive and behavioural efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person”. These cognitive efforts include the individual’s belief about capabilities to control the situation, e.g. the pain and the degree of disability they are experiencing because of pain. Although avoidant coping is associated with maladaption to pain (9) avoidant coping may also be considered useful by the individual, as it offers a psychological breather and an opportunity to control and escape from the pressure of the stressful situation, in this case pain (28). Use of avoidant coping reduces physical activities that are expected to increase pain and involves behaviours that do not predict or cause pain. Likewise, sickness absence has been considered a coping strategy by itself. Based on a study of 4,407 Danish slaughterhouse workers Kristensen (29) argued that employees who used sickness absence as a coping strategy may experience less work-related strain and an opportunity to undergo recuperation. This assumption has been questioned by van Rhenen et al. (30), who found that sickness absence history, taken as a proxy of the coping strategy with sickness absence, only had a minor impact on sickness absence given a general coping style. In the present study, sickness absence was associated with stressors due to high physical exposures in work environment, i.e. exposures that may cause increased pain. This may suggest that sickness absence is part of a coping process, with the overall purpose to conduct a behaviour that controls, avoids and prevents pain. Regarding avoidant coping strategy as either adaptive or maladaptive may be too simplistic. Thus, for some individuals it may be helpful to be on sick leave for a period, while for others it would lead to permanent withdrawal from the labour market. In addition, it is possible that sickness absence for a period exceeding, for example, 4 or more weeks, may be part of another coping strategy with a more deleterious effect on workability. This distinction in periods of absence ought to be investigated in future studies
Depression was strongly associated with sickness absence > 2 weeks. This is not surprising, as depressive disorder and other common mental health problems are now the leading cause of work disability in Denmark and many other European countries (31). However, depression did not confound the main effect of either pain frequency or avoidant coping in the logistic regression analyses. The analyses were also repeated, including the MDI scale as a continuous variable, but this did not change the estimates (data not shown).
The analyses revealed a graded risk for sickness absence along occupational social classes I–V. Several studies have shown an increasing prevalence of musculoskeletal morbidity by decreasing socioeconomic position, and it appears that people with a disadvantaged social situation are more vulnerable to the consequences of musculoskeletal disorders (32, 33). Moreover, a correlation between socioeconomic circumstances and coping strategy has been found in other studies (34, 35), and socioeconomic factors have been included as confounders in the analyses of different coping strategies with musculoskeletal pain (36, 37). A decrease in the use of problem-solving coping by decreasing social class among women, and an increase in the use of avoidant coping with decreasing social class among men has been found in a cross-sectional study of coping strategies with musculoskeletal pain and socioeconomic position (38). Thus, our study is embedded in the contextual approach to stress and coping, described as a complex dynamic process that involves the person, the environment, and the relationship between them (39).
Limitations
This study was based on a prospective design with a random sample of middle-aged Danish men and women as the baseline population in 2000. Detailed information on self-reported musculoskeletal pain and coping strategies were included, and sickness absence was categorized according to register-based episodes of absence. These did not include diagnostic information, but according to Danish legislation all sickness absence exceeding 2 weeks required a medical certificate. However, we cannot rule out that those individuals who reported pain and avoidant coping in 2006 and who were sickness absent in 2007 were those with a history of disease (not only musculoskeletal disorders), and who could have had previous spells of sickness absence before 2006. Consequently, we repeated all the analyses in a restricted population with the exclusion of participants with sickness absence exceeding 2 weeks in 2005 (n = 469). This restriction did not affect the results (data not shown).
The behavioural, pain-specific coping items used in this study have been thoroughly developed, tested and validated in different Danish study populations. However, it is a limitation that the specific item sets and response formats have not yet been compared with other pain-specific, behavioural coping measures.
The population for this study only included individuals aged 42–60 years, which prevents the generalization of the results to younger and older adults. However, the study sample is an appropriate age group for the study of coping with musculoskeletal pain, as the incidence of several musculoskeletal conditions increases after the age of 50 years (40).
Conclusion
No strong signs of an interactive effect on sickness absence were found between high pain frequency and avoidant, behavioural coping. However, this study confirms that pain and avoidant coping are important and independent predictors of sickness absence, which is in accordance with other studies. Consequently, clinicians should be aware of both factors when advising patients with musculoskeletal pain.
Acknowledgement
This study was supported by the Danish Research Councils (j.nr.9801268); the Danish Working Environment Research Fund: number 9-2007-03, number 20050072525/9 and number 2-2006-04, as well as the Ministry of the Interior and Health, Public Health Fund (grant number 2005-14033-8).
The authors declare no conflicts of interest.
References
