Friedbert Kohler, MD1,2, Melissa Selb, MSc3,4, Reuben Escorpizo, DPT, MSc3,4,5, Nenad Kostanjsek, MSc,6Gerold Stucki, MD, MS3,4,5 and Marcelo Riberto, MD, PhD7 on behalf of the International Society of Physical and Rehabilitation Medicine (ISPRM) sub-committee Implementation of the ICF and the participants of the São Paulo ISPRM – World Health Organization (WHO) workshop
From the 1Braeside Hospital, Wetherill Park, NSW, Australia 2School of Public Health and Community Medicine, Faculty of Medicine, University of NSW, Sydney, Australia, 3ICF Research Branch in cooperation with the World Health Organization (WHO) Collaborating Centre for the Family of International Classifications in Germany, Nottwil, Switzerland, 4Swiss Paraplegic Research, Nottwil, Switzerland, 5Department of Health Sciences and Health Policy, University of Lucerne, Lucerne/Nottwil, Switzerland, 6WHO, Classifications, Terminologies and Standards, Geneva, Switzerland, and 7University of São Paulo, Ribeirão Preto, Brazil
BACKGROUND: To optimize patient functioning, rehabilitation professionals often rely on measurements of functioning as well as on classifications. Although the International Classification of Diseases (ICD) and the International Classification of Functioning, Disability and Health (ICF) are used, their joint use has yet to become an established practice. To encourage their joint use in daily practice, the World Health Organization (WHO) has invited all rehabilitation practitioners worldwide to support the ICD-11 revision process by identifying the ICF categories that correspond to specific rehabilitation-relevant health conditions. The first step in completing this task, generating the list of these health conditions, was taken at a February 2012 workshop in São Paulo, Brazil.
OBJECTIVES: The objectives of this paper are to present the results of the São Paulo workshop, and to invite practitioners to participate in the ICD-ICF joint use initiative.
Discussion: Alternating plenary and small working group sessions were held and 103 rehabilitation-relevant health conditions were identified. With this list available, WHO together with the International Society of Physical and Rehabilitation Medicine (ISPRM), is reaching out to clinicians of all rehabilitation disciplines to take on the challenge of identifying the ICF categories for at least one of the health conditions listed.
Key words: International Classification of Diseases; ICF, classification; functioning; ICD revision; rehabilitation.
J Rehabil Med 2012; 44: 805–810
Correspondence address: Melissa Selb, Coordinator of the ICF Research Branch, c/o Swiss Paraplegic Research, Guido-Zäch-Strasse 4, 6207 Nottwil, Switzerland. Web: www.icf-research-branch.org. E-mail: melissa.selb@paranet.ch
Submitted August 22, 2012; accepted September 7, 2012
Introduction
Rehabilitation aims to optimize functioning (1, 2). In clinical practice, rehabilitation professionals rely on classifications and measurements of functioning (3, 4). The universal classification of functioning is the International Classification of Functioning, Disability and Health (ICF) (5). In rehabilitation practice, functioning is generally assessed separately, though in a complementary manner, from the diagnosis of health conditions as classified in the International Classification of Diseases (ICD) (6). Although the ICD and the ICF are used, their joint use in real-life contexts has yet to become an established practice. The main challenge for the joint use of the ICF with the ICD is the alignment of concepts and terminology. There is an opportunity to achieve this alignment within the framework of the current revision of the ICD-10 to the ICD-11. In this revision, the ICD will be supplemented with a number of so-called properties that allow for a better and more complete characterization of health conditions than previously. For the first time the ICD will also include the concept of functioning (and disability) through so-called functioning properties. Functioning properties are a value set of ICF categories from the ICF component of activities and participation that have been pre-selected and partially re-worded by the World Health Organization (WHO) and were developed with consideration of the domains of the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0), the World Health Survey (WHS), the disease-specific ICF Core Sets and the Generic ICF Core Set. Maximizing the value for users, functioning properties are intended to allow practitioners to describe the impact of a health condition on a person’s functioning by enabling practitioners to select the most relevant ICF categories for a particular ICD health condition (7–12).
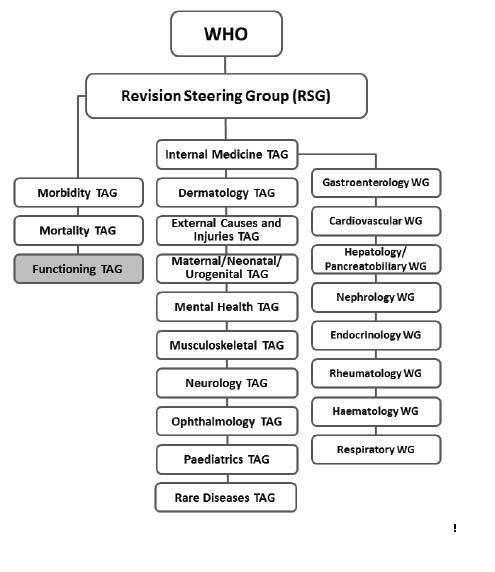
To further facilitate the integration of functioning properties in the ICD revision process, WHO has established a group of ICF experts called the functioning Topic Advisory Group or fTAG. The fTAG is a part of the ICD revision’s organizational structure that also includes other Topic Advisory Groups (TAG) made up of experts (practitioners and scientists) from specific areas of health (Fig. 1), who advise WHO on the revision of the ICD, including developing evidence-based proposals for content in their respective ICD chapter, address any revision issues that may arise, and coordinate the review of the revised chapter content.
Fig. 1. Overview of the International Classification of Diseases (ICD)-11 revision Topic Advisory Groups (TAG) and Working Groups (WG). WHO: World Health Organization.
One of the primary tasks of the fTAG is specification or population of functioning properties. To facilitate the completion of this task, fTAG has invited all rehabilitation practitioners worldwide to contribute. Since functioning properties cut across many rehabilitation disciplines, e.g. physical and rehabilitation medicine, physical therapy, occupational therapy, orthotics and prosthetics, opening this collaboration to the broad rehabilitation community is an essential part of the whole process. The first group to respond to the invitation was the International Society of Physical and Rehabilitation Medicine (ISPRM). ISPRM’s response to the call for contribution reflects ISPRM’s long-standing endeavour to facilitate the implementation of the ICF in rehabilitation practice (12–16). The sub-committee Implementation of the ICF is a sub-committee of the ISPRM-WHO-Liaison-Committee, and the work is part of the collaboration plan of ISPRM with WHO for the years 2011–2013.
There are 3 steps to completing the task of populating functioning properties:
1. Identification of health conditions that are associated with disability from a public health perspective and that are amenable to rehabilitation interventions.
2. Recruitment of experts for each of these health conditions and training them in the methods for identifying the functioning properties.
3. Development of ICF-based profiles of functioning for specific health conditions by identifying or populating the functioning properties using a standardized procedure outlined in a guidance document that was developed by the fTAG (17).
The first step was addressed at a workshop held in São Paulo, Brazil from 23–25 February 2012 during a symposium on the implementation of the World Report on Disability sponsored by ISPRM. With the results of the workshop available, the second step has now begun and an appeal is being made to rehabilitation professionals worldwide who are interested in serving as experts in populating the functioning properties for a specified health condition.
The objective of this special report is to present the results of the São Paulo workshop, and invite rehabilitation practitioners to participate in this ICD-ICF joint use initiative.
Methods
In order to identify the top health conditions that are associated with disability from a public health perspective and amenable to rehabilitation interventions, a 4-tiered strategy was employed.
The first tier utilized the list of the top 100 conditions from the global burden of disease (GBD) list from data sources at WHO, i.e. the GBD study disease and injury cause list found in the Global Burden of Disease Operations Manual (January 2009) (available from the WHO website: http://www.who.int/healthinfo/global_burden_disease/en/). This document, which lists and ranks the health conditions based on “years lived with disability (YLD)”, was initially reviewed by the workshop participants for relevance to rehabilitation. The resulting list was then examined more closely by small working groups to identify the health conditions that were most prevalent in rehabilitation practice and that were amenable to rehabilitation interventions. The small working groups were formed based on the countries or regions represented by the participants (Australia, Europe, Latin America with a separate group for Brazil and the USA). The results of the working groups were collated and the unified list was reviewed again in a plenary session, and a final consensus on the rehabilitation-relevant health conditions was reached.
The second tier required the identification of additional health conditions that were not included in the initial YLD list, but were considered rehabilitation-relevant and thus necessary to be included in the final list of health conditions. The additional health conditions were agreed upon in small working groups and in the second plenary session.
The third tier examined whether the health conditions identified are elements of reimbursements or rehabilitation service provision across a range of sample countries (by convenience) including Australia, Brazil, Turkey and Germany. The aim of this task was to ensure that there were no omissions of major rehabilitation-relevant health conditions, by considering cost coverage and country-specific service provision.
Having identified the most rehabilitation-relevant health conditions, the final tier involved identifying the corresponding ICD codes for the health conditions listed. Since some of the health conditions comprise more than one disease, disorder or syndrome, more than one ICD code may be identified for selected health conditions.
Results
The review and analysis of the initial YLD list of the most prevalent health conditions resulted in a list of 76 health conditions. Twenty-seven health conditions that were not included in the initial list from WHO were identified as relevant for rehabilitation and thus added to the list, including 5 health conditions resulting from discussions on country-specific considerations. In total, there were 103 health conditions (Table I).The list also shows the most relevant ICD codes for each health condition as well as the health conditions for which ICF Core Sets (10, 18–20) have already been developed and/or for which functioning properties have already been populated.
An ICF Core Set is an extract from the full ICF classification of ICF categories that are most essential in describing a person with a specific health condition in a comprehensive and multidisciplinary assessment (i.e. comprehensive version), as well as for reporting functioning and health in clinical practice and in research studies (i.e. brief version). ICF Core Sets are developed through a rigorous scientific process that includes conducting a systematic literature review, a multi-centre cross-sectional study, an expert survey and a qualitative study and an international consensus conference. As the minimum standard for describing functioning and disability, the Brief ICF Core Set has been used to populate the functioning properties (10, 18–20).
The third column of Table I indicates the health conditions that were on the initial YLD list that were also considered relevant for rehabilitation practice. The fourth and fifth columns indicate the health conditions that were added or deleted during the workshop as a result of discussions in the small working groups and on reimbursement and country-specific service provision. The fifth column shows the health conditions that were deemed irrelevant for rehabilitation practice and thus deleted from the list.
|
Table I. Results of the São Paulo Workshop: health conditions in bold are included in the final list of rehabilitation-relevant health conditions
|
|
Health condition
|
ICD-10 code(s)
|
On original YLD list and considered rehabilitation-relevant
|
Rehabilitation-relevant, thus added to the list
|
Irrelevant to rehabilitation, thus deleted from the list
|
ICF Core Set exists or FP already identified
|
|
Abdominal wall defect
|
Q79.5
|
|
|
×
|
|
|
Abortion
|
A04
|
|
|
×
|
|
|
Alzheimer’s and other dementias
|
F00, G30
|
×
|
|
|
|
|
Amputation (traumatic amputations involving multiple body regions)
|
T05
|
|
×
|
|
|
|
Amyotrophic diseases (amyotrophic lateral sclerosis)
|
G12.2
|
|
×
|
|
|
|
Anencephaly
|
Q00.00
|
|
|
×
|
|
|
Ankylosing spondylitis and other spondylopathies
|
M45, M48–M49
|
|
×
|
|
ICF Core Set for M45
|
|
Anorectal atresia
|
Q42.3
|
|
|
×
|
|
|
Appendicitis
|
K35
|
|
|
×
|
|
|
Ascariasis
|
B77
|
|
|
×
|
|
|
Asthma
|
J45
|
×
|
|
|
FP identified
|
|
Benign prostatic hypertrophy
|
D29.1
|
×
|
|
|
|
|
Bipolar affective disorder
|
F31
|
×
|
|
|
ICF Core Set
|
|
Birth asphyxia and birth trauma
|
P21.0
|
×
|
|
|
|
|
Bladder cancer
|
C67
|
×
|
|
|
|
|
Brain injury (traumatic brain injury or acquired brain injury)
|
S06
|
|
×
|
|
ICF Core Set
|
|
Breast cancer
|
C50
|
×
|
|
|
ICF Core Set
|
|
Cataracts
|
H25
|
|
|
×
|
|
|
Cerebral palsy
|
G80
|
|
×
|
|
|
|
Cerebrovascular disease including stroke
|
I60–I69
|
×
|
|
|
ICF Core Set for I64
|
|
Cervix uteri cancer
|
C53
|
×
|
|
|
|
|
Chagas disease
|
B57
|
×
|
|
|
|
|
Chlamydia
|
X92
|
|
|
×
|
|
|
Chronic obstructive pulmonary disease
|
J44
|
×
|
|
|
ICF Core Set
|
|
Cirrhosis of the liver
|
K70.3
|
|
|
×
|
|
|
Cleft lip
|
Q36
|
×
|
|
|
|
|
Cleft palate
|
Q35
|
×
|
|
|
|
|
Colon and rectum cancers
|
C18, C20
|
×
|
|
|
|
|
Complex regional pain syndrome
|
M89.0, G56.4
|
|
×
|
|
|
|
Congenital heart anomalies
|
Q20–Q28
|
×
|
|
|
|
|
Corpus uteri cancer
|
C54
|
×
|
|
|
|
|
Dengue
|
A90
|
|
|
×
|
|
|
Dental caries
|
K02
|
|
|
×
|
|
|
Developmental delay
|
F80–F89
|
|
|
×
|
|
|
Diabetes mellitus
|
E09–E14
|
×
|
|
|
ICF Core Set
|
|
Diarrhoeal diseases
|
A09, K52
|
|
|
×
|
|
|
Diphtheria
|
A36
|
|
|
×
|
|
|
Down’s syndrome
|
Q90
|
×
|
|
|
|
|
Drownings
|
T75.1
|
×
|
|
|
|
|
Drug use disorders
|
Z72.2
|
×
|
|
|
|
|
Edentulism
|
K05.3
|
|
|
×
|
|
|
Endocrine disorders
|
E20–35
|
×
|
|
|
|
|
Epilepsy
|
G40
|
×
|
|
|
FP identified
|
|
Falls
|
W00–19
|
×
|
|
|
|
|
Fires
|
X00–09
|
×
|
|
|
|
|
Fracture of femur
|
S72
|
|
×
|
|
|
|
Fracture of lower leg, including ankle
|
S82
|
|
×
|
|
|
|
Fracture of lumbar spine and pelvis
|
S32
|
|
×
|
|
|
|
Glaucoma
|
H40–H42
|
|
|
×
|
|
|
Gonorrhoea
|
Y71, X71
|
|
|
×
|
|
|
Gout
|
M10
|
×
|
|
|
|
|
Haemophilia
|
D66–D68
|
|
×
|
|
|
|
Hearing loss, adult onset
|
H90, H91
|
×
|
|
|
ICF Core Set
|
|
Heart failure
|
I50
|
|
×
|
|
|
|
Hepatitis B
|
B18.0
|
|
|
×
|
|
|
Table I. Contd.
|
|
Hepatitis C
|
B18.2
|
|
|
×
|
|
|
HIV/AIDS
|
B20–B24
|
×
|
|
|
|
|
Hookworm disease (ancylostomiasis and necatoriasis)
|
B76
|
|
|
×
|
|
|
Hypertensive disorders of pregnancy
|
Q15
|
|
|
×
|
|
|
Hypertensive heart disease
|
I11
|
×
|
|
|
|
|
Impingement syndrome
|
M75.4
|
|
×
|
|
|
|
Inflammatory heart disease
|
I51.9
|
|
|
×
|
|
|
Insomnia (primary)
|
G47.0
|
|
|
×
|
ICF Core Set for G47
|
|
Iodine deficiency
|
E00.0–9
|
|
|
×
|
|
|
Iron-deficiency anaemia
|
D50
|
|
|
×
|
FP identified
|
|
Ischaemic heart diseases
|
I20–I25
|
×
|
|
|
FP identified for I21, ICF Core Set for I25
|
|
Japanese encephalitis
|
A83
|
×
|
|
|
|
|
Joint arthroplasty
|
Z50.9
|
|
×
|
|
|
|
Leishmaniasis
|
B55
|
×
|
|
|
|
|
Leprosy and sequelae of leprosy
|
A30, B92
|
×
|
|
|
|
|
Leukaemia
|
C90.1 C91, C92, C93, C94–95
|
×
|
|
|
|
|
Liver cancer
|
C22
|
×
|
|
|
|
|
Low back pain (dorsalgia)
|
M54.5
|
×
|
|
|
ICF Core Set
|
|
Low birth weight
|
P07.0
|
×
|
|
|
|
|
Lower limbs fractures
|
S82, T02.5
|
|
×
|
|
|
|
Lower respiratory infections
|
J20–J22
|
×
|
|
|
|
|
Lymphatic filariasis
|
B74
|
×
|
|
|
|
|
Lymphomas and multiple myeloma
|
C81–96
|
×
|
|
|
|
|
Macular degeneration and other sense disorders
|
H00–21, 27–35, 43, H35
|
×
|
|
|
|
|
Malaria
|
B50–54
|
×
|
|
|
|
|
Maternal haemorrhage
|
P50.4
|
|
|
×
|
|
|
Maternal sepsis
|
N97
|
|
|
×
|
|
|
Measles
|
B05
|
|
|
×
|
|
|
Melanoma and other skin cancers
|
C43
|
×
|
|
|
|
|
Meningitis
|
G03.0–G03.9
|
×
|
|
|
|
|
Mental and behavioural disorders due to use of alcohol
|
F10
|
×
|
|
|
|
|
Mild mental retardation attributable to lead exposure (unspecified mental retardation)
|
F79
|
×
|
|
|
|
|
Mouth and oropharynx cancers
|
C00–C14
|
×
|
|
|
ICF Core Set
|
|
Movement disorders (e.g. ataxia, hemiplegia, dysdiadochokinesia)
|
G11, G81, R27
|
|
×
|
|
|
|
Musculoskeletal pain syndrome (fibromyalgia, entrapment/ mononeuropathies)
|
G56–58, M79.7
|
|
×
|
|
ICF Core Set for M79.7
|
|
Multiple sclerosis
|
G35
|
×
|
|
|
ICF Core Set
|
|
Muscle dystrophy
|
G71.0
|
|
×
|
|
|
|
Myopathies
|
G71.2, G72
|
|
×
|
|
|
|
Nephritis and nephrosis
|
N01–05, N10–N12
|
×
|
|
|
|
|
Neuropathies
|
G60–G64, G90
|
|
×
|
|
|
|
Obsessive-compulsive disorder
|
F42.2
|
|
|
×
|
|
|
Obstructed labour
|
O64
|
|
|
×
|
|
|
Oesophageal atresia
|
Q39.1
|
×
|
|
|
|
|
Oesophagus cancer
|
C15
|
×
|
|
|
|
|
Onchocerciasis
|
B73
|
×
|
|
|
|
|
Osteoarthritis
|
M15, M16, M17, M18, M19
|
×
|
|
|
ICF Core Set
|
|
Other intentional injuries
|
X83
|
×
|
|
|
|
|
Other joint disorder, not elsewhere classified
|
M25
|
|
×
|
|
|
|
Other neurotic conditions
|
F48
|
|
×
|
|
|
|
Other unintentional injuries
|
V01–X59.9
|
×
|
|
|
|
|
Otitis media
|
H65–H67
|
|
|
×
|
|
|
Ovary cancer
|
C56
|
×
|
|
|
|
|
Pancreas cancer
|
C25
|
×
|
|
|
|
|
Panic disorder
|
F41
|
|
|
×
|
|
|
Parkinson’s disease
|
G20
|
×
|
|
|
|
|
Peptic ulcer disease
|
K25–K27
|
|
|
×
|
|
|
Table I. Contd.
|
|
Periodontal disease
|
K05.2–5.5
|
|
|
×
|
|
|
Pertussis
|
A37.9
|
|
|
×
|
|
|
Poisonings
|
T36–T50
|
×
|
|
|
|
|
Poliomyelitis and sequelae of poliomyelitis
|
A80, B91
|
×
|
|
|
|
|
Post-traumatic stress disorder
|
F43.1
|
×
|
|
|
|
|
Prostate cancer
|
C61
|
×
|
|
|
|
|
Protein-energy malnutrition
|
E43–E46
|
×
|
|
|
|
|
Pulmonary hypertension
|
I27
|
|
×
|
|
|
|
Refractive errors
|
H52
|
|
|
×
|
|
|
Renal agenesis
|
Q60
|
|
|
×
|
|
|
Renal failure
|
N17–N19
|
|
×
|
|
|
|
Rheumatic heart disease
|
I09
|
×
|
|
|
|
|
Rheumatoid arthritis
|
M05–M06,
|
×
|
|
|
ICF Core Set
|
|
Road traffic accidents
|
V01–V99
|
×
|
|
|
|
|
Schistosomiasis
|
B65
|
|
|
×
|
|
|
Schizophrenia
|
F20
|
×
|
|
|
|
|
Spinal cord injury
|
G82
|
|
×
|
|
ICF Core Set
|
|
Scleroderma, dermatomyositis
|
L94.0–L94.1, M33–M34
|
|
×
|
|
|
|
Self-inflicted injuries
|
X60–X84
|
×
|
|
|
|
|
Skin diseases, e.g. psoriasis, decubitus ulcer and pressure area, other disorders of skin and subcutaneous tissue not elsewhere classified
|
L40, L89, L98
|
×
|
|
|
|
|
Spina bifida
|
Q05
|
×
|
|
|
|
|
Stomach cancer
|
C16
|
×
|
|
|
|
|
Syphilis
|
A50
|
×
|
|
|
|
|
Tetanus
|
A33–A35
|
×
|
|
|
|
|
Trachea, bronchus and lung cancers
|
C33–34
|
×
|
|
|
|
|
Trachoma
|
A71
|
|
|
×
|
|
|
Trichuriasis
|
B79
|
|
|
×
|
|
|
Trypanosomiasis
|
B56.9
|
|
|
×
|
|
|
Tuberculosis and sequelae of tuberculosis
|
A15–A19, B90
|
×
|
|
|
|
|
Unipolar depressive disorders
|
F32–F33
|
|
|
×
|
ICF Core Set
|
|
Upper respiratory infections
|
J00–J06
|
|
|
×
|
|
|
Upper limbs fractures
|
T02.2
|
|
×
|
|
|
|
Vertebral fractures
|
M48.4, S12–S13, S22.0
|
|
×
|
|
|
|
Violence
|
R45.6, T74.0
|
×
|
|
|
|
|
Vitamin A deficiency
|
E50
|
|
|
×
|
|
|
War
|
Y36
|
×
|
|
|
|
|
ICD: International Classification of Diseases; YLD: years lived with disability; ICF: International Classification of Functioning, Disability and Health; FP: functioning properties.
|
Discussion
The data available for the third tier of the process varied considerably from country to country, thus making any comparisons difficult. It demonstrated that there are significant differences in provision of rehabilitation services and reimbursement between countries. For example, the small working group consisting of participants from Brazil focused on the health conditions that received cost coverage for rehabilitation services and assistive devices/equipment, while the small working group with participants from Turkey provided information on the main rehabilitation medicine diagnoses, and the groups representing participants from Germany and Australia both listed health conditions that accounted for the most bed days in rehabilitation facilities. This diversity of data does, however, support a broad approach to the consideration of functioning in rehabilitation-relevant ICD-11 codes.
While the list of health conditions include specific ICD codes for each of the health conditions, there may be additional ICD codes for selected health conditions that need to be populated with functioning properties. Most of the ICD codes listed in Table I reflect the so-called parent code. This is the broad overlying code under which more detailed sub-codes are nested, e.g. under the parent code “M05 Seropositive rheumatoid arthritis” is the sub-code “M05.2 Rheumatoid vasculitis” (6). The expert who agrees to populate specific health conditions may also decide to populate sub-codes should this be deemed essential. Health conditions for which ICF Core Sets have been developed have already been populated with the Brief ICF Core Set and thus do not need to be populated again.
If an ICF Core Set for a specific health condition does not exist, populating the functioning properties follows a set of guidelines, which comprise gathering evidence by conducting a literature review to identify research that has examined the most widely used health status measurement instruments for respective health conditions, and linking the measurement instruments to the ICF using established linking rules (21). Once the list of ICF codes is finalized, it will be given to the ICF Research Branch for entering into the electronic system dedicated for the ICD-11 revision process. The ICF Research Branch is the organization coordinating the initiative on behalf of the fTAG and in close collaboration with ISPRM.
Conclusion and call for action
Rehabilitation practitioners are involved in the day-to-day management of health conditions that have been identified during the São Paulo workshop as being amenable to rehabilitation. It is therefore appropriate that rehabilitation practitioners are engaged in the ICD-11 revision process in completing the task of assigning the functioning properties to the ICD codes of rehabilitation-relevant health conditions. Nevertheless, it is crucial that other health practitioners are also involved in the population of functioning properties, particularly for the conditions that are not generally treated by rehabilitation practitioners in the traditional sense, e.g. hearing loss.
Practitioners with relevant expertise in any of the rehabilitation-relevant health conditions listed are invited to assist in this task by registering their interest with the ICF Research Branch in Nottwil, Switzerland (melissa.selb@paranet.ch).
Acknowledgements
We would like to express our thanks to the ISPRM Implementation of the ICF Sub-Committee and the participants of the São Paulo ISPRM/WHO workshop who provided valuable input to the discussions at the workshop in São Paulo: Salomon Abuchaibe, Maher Saad Al-Jadid, Livia Borgneth, Cassia Maria Buchalla, Marcos Renato de Assis, Luana Talita Diniz Ferreira, Sonia Flores, Perola Grimberg Plapler, Maria Herrera, Alvydas Juocevicius, Friedbert Kohler, Jorge Lains, Christina May Moran de Brito, Olivier Remy-Neris, Marcelo Riberto, Aydan Oral, Gerold Stucki and Myrtha Vitale.
References