OBJECTIVE: To describe the timing and factors associated with the occurrence of sentinel events (financial strain, difficulty accessing therapy, return to work, accommodation change and independent transport use) during transition to the community for individuals with traumatic brain injury.
DESIGN: Longitudinal cohort design with data collected pre discharge and at 1, 3 and 6-month follow-ups.
SUBJECTS: Individuals with moderate to severe traumatic brain injury (n = 127), discharged home from acute care and inpatient rehabilitation.
METHODS: Data were collected using self-report questionnaires (sentinel events questionnaire, Mayo Portland Adaptability Inventory-4, Sydney Psychosocial Reintegration Scale, Depression Anxiety Stress Scale). Logistic regression was used to identify factors associated with sentinel events.
RESULTS: The most commonly reported events were independent transport use and return to work, reported on 104 and 90 occasions, respectively. A longer hospital stay and poorer community integration were related to negative events (e.g. reduced therapy). The inverse relationship was seen for positive events. Links existed between sentinel events (e.g. previous financial strain increased the likelihood of this event in transition).
CONCLUSION: This paper highlights the interplay between personal and environmental factors and life events in shaping transition experiences. Individualised service planning and monitoring of sentinel events is important to promote successful community transition.
Key words: brain injuries; life change event; community integration.
J Rehabil Med
Correspondence address: Miss Emily Nalder, Centre for Functioning and Health Research, Po Box 6053, Buranda, Queensland, Australia, 4012. E-mail: e.nalder@uq.edu.au
Submitted June 14, 2011; accepted May 22, 2012
Introduction
A key transition occurs as individuals with a traumatic brain injury (TBI) move from hospital care to living at home in the community (1). Studies focusing on this transition phase are relatively new in brain injury rehabilitation research, and the transition phase is defined for the purpose of this paper as the first 6-months following discharge. Research to date has investigated functional or health outcomes during transition (2, 3) and qualitatively explored the transition experiences of individuals with TBI and their family members (4, 5). An alternative approach is to consider the key events that are experienced during the transition phase, and their potential impact upon future aspects of the life course for individuals with TBI (6).
The life course theory is based on the premise that ageing and human development is a life-long process, shaped by past experiences and historical events (7). Life course theory offers a different conceptual approach to current research addressing community re-integration. It focuses on understanding life according to events that occur over time in differing societal and personal contexts and the influence of such events on how individuals’ lives unfold. Key principles of life course theory reflect the need to consider the timing of life events, human agency, the links between individuals’ lives, and historical time and place (or the influence of the environment and historical events), when examining the life course (8). Life course theory therefore can provide a framework to guide longitudinal research into key events influencing successful community re-integration following TBI.
Community integration has been the dominant outcome measure used to reflect the experiences of individuals with TBI following hospital discharge (9). Consistently, research indicates that individuals with TBI have lower levels of community integration than their pre-morbid status and when compared to the general population (3). Lower productivity and employment levels (10), fewer opportunities for participation in social or recreational activities, social isolation (11), increased dependency upon informal caregivers (12), and emotional distress (2, 13) have been negative experiences reported to occur following TBI. Additionally, research indicates that family caregivers are also at risk of negative outcomes in the long-term including caregiver burden and elevated symptoms of depression and stress (14).
Using the life course theory, the concept of “sentinel events” was developed to guide research during transition to the community after TBI in order to better understand the life events which may shape experiences and contribute to poor community integration (6). A sentinel event is defined as “an important event, either positive or negative, which arises in the life of an individual and requires investigation to assess its timing, precursors and impact (both positive and negative) on aspects of the life course”(6). Eight sentinel events relevant to the transition phase were drawn from a pilot study (5), and a literature review (1). These events included experiencing financial strain, relationship breakdown, moving to a more restricted living situation, having difficulty accessing therapy services, returning to work, returning to independent use of transportation, regaining independence in the home, and returning to driving (6).
Importantly, sentinel events have been shown to influence perceived transition success for individuals with TBI (15). In a longitudinal investigation of the transition from hospital to home, 5 events including financial strain, changing living situation, having difficulty accessing therapy services, returning to work and independent use of transport were observed to influence perceptions of transition success over time (15). Three events: return to work, moving to a more restricted environment and returning to independent use of transport, were positively correlated with perceived transition success while the remaining two events: financial strain and experiencing difficulty accessing therapy services, had a negative correlation. These findings suggest that further examination of these 5 sentinel events is warranted. To date most of the research investigating these events has focused on longer-term community re-integration outcomes, generally measured from 6–12 months post-injury or beyond (16). For example, research has shown that individuals with TBI can experience difficulty in resuming key occupational roles such as those of worker, spouse, or driver (3, 12, 16), and experience difficulty with independent living, particularly more complex activities such as money management (17) and use of public transport (16). On the whole however, little is known about the rate of occurrence and timing of these events and of the factors which relate to them in the transition phase. Such information would inform the delivery of rehabilitation and support services ensuring they are provided at key time-points and to individuals who will benefit most.
Factors known to influence community integration after TBI include severity of injury, age, gender, education, occupation, living arrangements, cognitive and emotional status, and functional performance (18). In general individuals with a less severe injury, who are younger, have higher educational or employment qualifications, and fewer cognitive impairments, emotional distress and participation restrictions, achieve greater levels of community re-integration (18). Similar factors have been linked to return to work and driving. Age, prior work, psychological distress, injury severity and cognitive status was associated with return to work at 2 years post-injury (19), and at 10 years post-injury return to driving was associated with a less severe injury and fewer cognitive impairments (20).
As many sentinel events occur for the first time during the first 6-months in the community (6), understanding the factors which relate to these events may help identify individuals at risk of a less successful transition. In particular, it may be useful to identify any factors at the time of discharge from hospital that predict the occurrence of events during the transition phase, thereby enabling health professionals to identify individuals who may require additional supports to transition to the community successfully. Furthermore, based on the recognition that past experiences can shape later outcomes (8), it may be important to consider links between sentinel events. For example, is there a link between return to work or relationship breakdown, and financial strain? Such information may assist professionals in promoting the occurrence of positive events and preventing clusters of negative events. This paper aims to:
1) provide descriptive information on the occurrence and timing of 5 sentinel events during transition from hospital to community for individuals with TBI, and
2) to identify the demographic and injury related factors, and other sentinel events, that are related to the occurrence of 5 sentinel events during the transition phase. Given the exploratory nature of this research no specific study hypotheses were formulated.
Methods
Design
A prospective longitudinal investigation was conducted with data collected at 4 time points during the transition from hospital to home for individuals with TBI.
Participants
Participants were recruited over a 24-month period between 2007 and 2009 from an inpatient rehabilitation unit and an acute neurosciences ward, both located in a tertiary hospital in Australia. Participants were sampled consecutively at the time of discharge from hospital. Inclusion criteria included having a diagnosis of TBI, aged between 18 and 60 years, returning to live in a community setting and adequate cognitive and communication skills to provide informed consent and participate in an interview, based on reports from treating speech and occupational therapists. Participants in hospital for less than 4 days, who had mental health conditions which would impair provision of informed consent (as documented by a treating doctor), or who were transferred to another medical facility (e.g. a nursing home), were excluded.
From a total of 240 eligible participants, 98 people declined to participate in the research or were unable to be contacted again following discharge, 1 person died in hospital and 14 participants were excluded from analyses because they withdrew consent or were missing data at 3 or more assessment points. The final sample consisted of 127 individuals with TBI, with a mean age of 35 years (standard deviation (SD) 12.38). The majority were male (78%) and employed in paid full-time work prior to the injury (64%). Level of injury severity varied: 31% had an extremely severe injury, post traumatic amnesia (PTA) duration > 4 weeks (n = 39), 28% had a very severe injury, PTA duration 1–4 weeks (n = 36), 25% had a severe injury, PTA duration 1–7 days (n = 32), 2 % had a moderate injury, PTA duration of less than or equal to one day (n = 2) and no participants had a mild injury, (i.e., minimum duration of PTA recorded was one day). Mean length of hospital stay (i.e., total hospital stay including acute and rehabilitation) was 74 days (SD 90.74, 4–776), mean Glasgow Coma Scale (GCS) within 24 h of injury was 9.92 (SD 4.39, 3–15), and mean duration of PTA was 29 days (SD 29.50, 1–173). Table I presents sample characteristics and the number of participants who completed each assessment.
Of the 127 individuals with TBI partaking in the study, 83 had a caregiver also consenting to participate. Caregivers were defined as the family member or friend most closely associated with the individual on a daily basis and were primarily a spouse or partner (61%), or a parent (31%) of the individual with TBI. In this paper carer data is only used to reflect the occurrence of a sentinel event (a proxy report) in cases where individuals with TBI were known to be poor historians.
|
Table I. Sample characteristics at each follow-up point during transition
|
|
Variable
|
Pre-discharge
(n = 122)
Mean (SD) [range]
Median (IQR)
|
1 month
(n = 121)
Mean (SD) [range]
Median (IQR)
|
3 months
(n = 118)
Mean (SD) [range]
Median (IQR)
|
6 months
(n = 107)
Mean (SD) [range]
Median (IQR)
|
|
SPRS
|
53.92 (8.56) [24–72]
56 (49–60)
|
55.65 (10.01) [26-72]
58 (48–62)
|
55.17 (12.41) [14-72]
58.5 (48–64)
|
57.54 (11.86) [22-72]
60 (51–67)
|
|
DASS
|
16.66 (19.09) [0–106]
12 (4–22)
|
19.04 (20.74) [0–90]
12 (3–30)
|
19.63 (22.43) [0–96]
10 (2–30)
|
16.50 (19.81) [0–82]
8 (2–24)
|
|
MPAI-4
|
42.27 (7.53) [18–62]
42 (38.5–47)
|
40.74 (10.31) [–4 – 62]
41 (36–48)
|
40.90 (10.15) [10–65]
41 (33–50)
|
38.39 (12.91) [–4–65]
39 (32–46)
|
|
SPRS: Sydney Psychosocial Reintegration Scale; DASS: Depression Anxiety Stress Scales; MPAI-4: Mayo Portland Adaptability Inventory-4; SD: standard deviation; IQR: interquartile range.
|
Measures
The primary outcome measure was a sentinel events questionnaire (SEQ) used to collect information on the occurrence (yes/no) and timing (recording the specific date of occurrence) of sentinel events during transition (6). The 5 sentinel events which are the focus of this paper were; 1) financial strain, “having to borrow money or goods greater than $100 in value, or accessing funds via superannuation accounts, charitable organisations, savings plans, or via sale of assets”, 2) experiencing difficulty accessing therapy services, “having sought therapy or rehabilitation services and been unable to access that service or having therapy services discontinued despite wishing that they would be ongoing”, 3) returning to work, “having resumed paid or voluntary work or study”, 4) moving to a more restricted living situation, “moving to a more restrictive living situation such as, returning home to live with parents, moving into supported accommodation or being re-hospitalised”, and 5) returning to independent use of transport, “having started to travel in the community by private or public modes of transport (for example driving a privately owned vehicle, public transport or taxi use) without the help of a family member or friend” (6). Not all participants were engaged in paid employment prior to the injury and thus for the purposes of this investigation individuals were considered as having returned to work if they resumed activities identified by the individual as giving meaning and productivity to their day including for example volunteer work or caring responsibilities.
The SEQ was developed for an ABI population and younger people with TBI trialled the measure during its development. A recent study investigated participant-proxy agreement for SEQ items and return to work demonstrated very good agreement (κ > 0.81), moving to a more restrictive living situation and returning to independent transport use had good agreement (κ 0.61–0.8), and financial strain and experiencing difficulty accessing therapy had moderate agreement (κ 0.41–0.6) (6).
Other measures were used to collect information on factors potentially associated with the occurrence of sentinel events in transition. Level of psychosocial integration was measured by the Sydney Psychosocial Reintegration Scale (SPRS) (21); global functioning was measured by the Mayo-Portland Adaptability Inventory-4 (MPAI-4) (22); and emotional wellbeing was measured by the Depression Anxiety Stress Scales (DASS-21) (23). All measures have been used with the TBI population and have established psychometric properties including reliability and validity (13, 21, 24, 25).
Procedure
The project had ethical approval from university and hospital ethics committees and all participants gave written informed consent. Measures were completed during an interview between a member of the research team and individuals with TBI (and their caregiver) at 4 time points: in the week prior to discharge (baseline), and at 1, 3 and 6 months post discharge. As it was often difficult to schedule appointments with participants we conducted follow-up assessments within bands of time around the 1, 3- and 6-month point post discharge. For example, at 1-month we collected data within two weeks of the required date for follow-up, and at 6-months we collected data within 12-weeks of the required assessment. Most participants completed the measures over the telephone, however in a small number of cases use of face to face, email or postal methods of data collection were used to achieve higher response rates (26). Additional demographic and injury related information (e.g. duration of PTA) was collected via a combination of participant report and medical chart review.
Data Analysis
Descriptive statistics and Kaplan-Meier estimates were used to summarise the timing and frequency of sentinel events as reported by individuals with TBI. Logistic regression was used to identify personal factors related to the experience of each sentinel event. An event was defined as having occurred if it was reported at least once during the first 6-months post discharge. Model building strategies as outlined by Hosmer & Lemeshow (27) were employed in this investigation. The model building strategy first involves univariate logistic regression to identify explanatory variables associated with each of the five sentinel events used as outcome variables (i.e. financial strain, reduced therapy access, return to work, moving to a more restricted living situation and return to independent use of transport). Explanatory variables were all measured at baseline and included age, gender, country of birth (born in Australia vs born outside of Australia), relationship status (in a relationship vs not in a relationship), geographic location (metropolitan vs rural dwelling), years of education, length of stay in hospital (days), initial GCS score, duration of PTA, total and subscale scores of the SPRS, DASS and MPAI-4, and experience of sentinel events during hospitalisation. The MPAI manual allows for conversion of raw data to a standardised T-score to allow for comparison of individuals results to other people with ABI. Standardised MPAI-4 scores were used as explanatory variables in analyses. Previous research using Rasch analysis has also demonstrated that the MPAI-4 has acceptable degrees of separation for items and person (25). Explanatory variables associated with the outcome variable (p < 0.25) were then included in a multiple logistic regression model developed using a backwards stepwise approach to identify the most parsimonious model (27). Explanatory variables of least significance were dropped from the model in a step-wise process until all remaining variables had a p-value of less than (or approaching) 0.01, and no collinearity was evident. In cases where collinearity was apparent we maintained subscale rather than total scores, considered the presence of missing data, and monitored the relative importance of each variable using odds ratio (OR) and p-values. Given the large number of correlations a significance level of p < 0.01 was used. Missing values for 3 variables (education, GCS and country of birth) were imputed using best subsets regression using variables not included in the final multiple regression models to minimise collinearity with variables retained in these models. All statistical analyses were completed using the software program Stata version 10 (StataCorp, Texas, USA).
Results
Timing and frequency of sentinel events
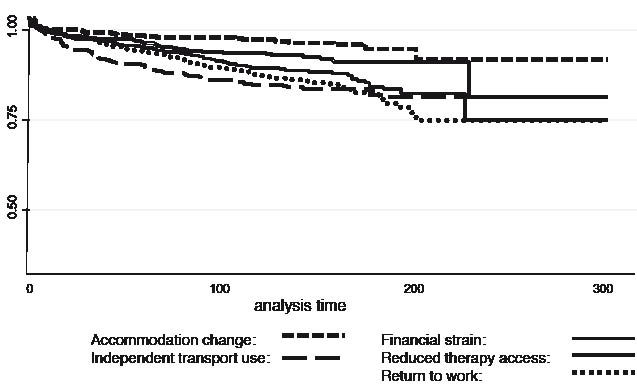
Table II summarises the frequency and timing of sentinel events reported by individuals with TBI during transition. Timing was variable for all sentinel events and this is reflected in Fig. 1, showing the Kaplan-Meier survival curves for the occurrences of each sentinel event during the 6-month period of follow-up. Moving to a more restricted living situation, experiencing difficulty accessing therapy services and returning to independent use of transport occurred on average within the first 1–2 months post discharge (Fig. 1). Returning to work and financial strain occurred on average later (2–3 months after discharge).
|
Table II. Descriptive data on the occurrence of sentinel events for participants with TBI (n = 127)
|
|
Sentinel event
|
Probability of experiencing event in transition
|
Occurrences of event
n
|
Timing of eventa
Median, (IQR)
|
|
K-M
|
95% CI
|
|
Independent transport use
|
0.20
|
0.17– 0.25
|
104
|
24.5
(7.05–58.5)
|
|
Return to work
|
0.27
|
0.21–0.34
|
90
|
53 (17–109)
|
|
Financial strain
|
0.27
|
0.15–0.44
|
76
|
44.5 (10–98)
|
|
Difficulty accessing therapy services
|
0.22
|
0.09–0.47
|
64
|
14 (1–65.5)
|
|
Moving to a restricted living situation
|
0.12
|
0.07–0.2
|
45
|
1 (1–43)
|
|
aMeasured in number of days since discharge.
The value 0.1 denotes events which occurred on the day of discharge from hospital.
IQR: interquartile range; CI: confidence interval; K-M: Kaplan-Meier failure function.
|
Fig. 1. Kaplan-Meier survival curve reflecting the occurrence and timing of sentinel events.
Factors associated with the occurrence of sentinel events – results of univariate analyses to identify variables for inclusion in subsequent multiple regression model development
The next paragraphs contain results of the univariate logistic regression analyses describing the relationships between the occurrence of sentinel events and the explanatory variables where p < 0.25 as per the model building strategy (27). Negative events are presented first followed by a discussion of factors related to the occurrence of positive sentinel events.
For the sentinel event financial strain, explanatory variables included in backwards stepwise logistic regression as (p < 0.25) included; SPRS scores (p = 0.01), MPAI-4 scores (p = 0.002), DASS scores (p = 0.01), and pre-discharge experience of financial strain (p < 0.001), relationship breakdown (p = 0.07), reduced therapy access (p = 0.21) and independent use of transportation (p = 0.17). The event of experiencing difficulty accessing therapy services in transition had the following explanatory variables included in a backwards stepwise regression; country of birth (p = 0.03), length of stay (p = 0.04), GCS scores (p = 0.02), duration of PTA (p = 0.22), SPRS scores (p = 0.13), MPAI-4 scores (p = 0.02), and pre-discharge experience of independent transport use (p = 0.20).
Return to work had the following explanatory variables included in the backwards stepwise regression; education (p = 0.01), length of hospital stay (p = 0.002), GCS scores (p = 0.02), PTA scores (p = 0.004), SPRS scores (p = 0.03), DASS scores (p = 0.15), MPAI-4 scores (p = 0.12), and pre-discharge experience of regaining independence in the home (p = 0.16), in use of transport (p = 0.21) and relationship breakdown (p = 0.14). Moving to a more restricted living situation had the following explanatory variables included in a backwards stepwise regression; relationship status (p = 0.01), age (p = 0.03), DASS scores (p = 0.11), MPAI-4 scores (p = 0.19), and pre-discharge experience of financial strain (p = 0.06) and difficulty accessing therapy services (p = 0.05). Returning to independent use of transportation had the following explanatory variables included in a backwards stepwise regression; education (p = 0.16), length of stay (p = 0.001), place of residence (p = 0.05), duration of PTA (p = 0.001), SPRS relationships scores (p = 0.21), DASS anxiety scale scores (p = 0.23), and pre-discharge experience of independent transport use (p = 0.01), regaining independence at home (p = 0.24) and financial strain (p = 0.03).
The number of explanatory variables in each multiple logistic regression model was reduced using a backwards stepwise approach. Five models were obtained identifying the most important factors related to the occurrence of each sentinel event during transition. (Table III). Missing data were evident for some explanatory variables (MPAI-4 items) leading to cases being dropped from multiple regression analyses. No cases were dropped from the model examining use of transport. Five cases were dropped from the remaining 4 models.
|
Table III. Association between explanatory variables and occurrence of sentinel events using multiple regression models
|
|
Explanatory variables
|
Financial strain
OR (95% CI), p-value
|
Reduced therapy access
OR (95% CI), p-value
|
Return to work
OR (95% CI), p-value
|
Change in living situation
OR (95% CI), p-value
|
Independent transport use
OR (95% CI), p-value
|
|
Education
|
–
|
–
|
1.24 (1.04 –1.49), 0.018
|
–
|
–
|
|
Ethnicity
|
–
|
0.31 (0.10–0.94), 0.038
|
–
|
–
|
–
|
|
GCS
|
|
0.84 (0.76–0.93), 0.001*
|
|
|
|
|
LOS
|
–
|
–
|
0.99 (0.98–1.00), 0.001*
|
–
|
0.99 (0.98–0.99), 0.001*
|
|
Relationship status
|
–
|
–
|
–
|
0.29 (0.12–0.66), 0.003*
|
–
|
|
MPAI–4
|
|
|
|
|
|
|
Ability
|
1.07 (1.03–1.12), 0.001*
|
–
|
–
|
1.03 (1.00–1.07), 0.077
|
–
|
|
Adjustment
|
–
|
1.08 (1.02–1.13), 0.004*
|
0.95(0.91–1.00), 0.031
|
–
|
–
|
|
Pre–discharge
|
|
|
|
|
|
|
Financial strain
|
6.06 (2.13–17.22), 0.001*
|
–
|
–
|
–
|
0.27 (0.09–0.78), 0.016
|
|
Independent transport use
|
–
|
–
|
–
|
–
|
0.07 (0.01–0.44), 0.004*
|
|
Reduced therapy access
|
–
|
–
|
–
|
3.84 (0.95–15.55), 0.059
|
–
|
|
Participants correctly classified by model (%)
|
73.8
|
73.8
|
73.0
|
68.9
|
85.0
|
|
*p < 0.01. OR: odds ratio; CI: confidence interval; GCS: Glasgow Coma Scale; LOS: length of hospital stay measured in number of days; MPAI-4: Mayo Portland Adaptability Inventory; SPRS: Sydney Psychosocial Reintegration Scale; DASS: Depression Anxiety Stress Scale.
|
Results of multiple logistic regression regarding factors most influential in predicting the occurrence of sentinel events
Two models were developed examining the occurrence of negative sentinel events. The first model using financial strain as the outcome variable was significant (p < 0.001), and individuals who experienced financial strain in hospital and who had more impairments as rated on the MPAI-4 Ability subscale were more likely to experience financial strain in transition. The second model which used reduced therapy access as the outcome variable was significant (p < 0.001) and the explanatory variables GCS and MPAI-4 Adjustment score were significant with country of birth approaching significance. Individuals with a more severe injury and poorer adjustment were more likely to report difficulty accessing therapy in transition.
Three models were developed examining the occurrence of positive sentinel events. The model predicting return to work was significant (p < 0.001). Length of hospital stay was a significant explanatory variable (p < 0.01) and both years of education and MPAI-4 Adjustment score approached significance. Individuals with a shorter hospital stay were more likely to return to work in transition. The model using moving to a more restricted living situation as the outcome variable, was significant (p = 0.001) and the only significant explanatory variable was relationship status. However, both the MPAI-4 Ability score and experiencing restricted therapy access in hospital approached significance. Individuals in a relationship were less likely to change living situation in transition. The final model with return to independent use of transport as the outcome variable was significant (p < 0.001) and the associations with explanatory variables (length of stay, and resuming independent transport use) were significant. Experiencing financial strain in hospital approached significance. Individuals with a shorter hospital stay and who had not resumed transport use while in hospital were more likely to resume independent transport use in transition.
Discussion
This paper examined the occurrence of 5 sentinel events during the transition from hospital to home, as they are known to influence perceptions of transition success for individuals with TBI. All events occurred relatively frequently ranging from moving to a more restricted living situation which was reported on 45 occasions, to returning to independent transport use which was reported on 104 occasions. The timing of all events was extremely varied over the first 6 months after discharge. In general positive sentinel events, such as regaining independence and returning to work, were more likely to be experienced by individuals with higher levels of global functioning and psychosocial integration. Individuals with lower levels of functioning were at greater risk of experiencing more negative sentinel events (e.g. financial strain). This investigation also identified links between sentinel events, for instance, individuals who had experienced financial strain in hospital were less likely to independently use transport.
This study looked at the occurrence of negative events like financial strain and relationship breakdown, as well as the events associated with the return of independence and participation in the community, which are traditionally the focus of rehabilitation (28). While it is encouraging that a relatively high percentage of individuals report achieving independent transport use (104 occurrences) and returning to work (90 occurrences), the proportion who experience negative events such as financial strain (76 occurrences), difficulty accessing therapy (64 occurrences) and moving to a more restricted living situation (45 occurrences), is of concern. The prevalence of events such as financial strain and experiencing difficulty accessing therapy with this population may reflect specific service delivery issues relevant to the Australian context. For example, this study considered the occurrence of these events during the early transition phase from hospital to home and at the site of recruitment there was no designated transitional rehabilitation service within the public healthcare system. These findings suggest that there is a need to discuss these issues in discharge planning and early community rehabilitation to ensure that individuals and families are prepared for life during the transition phase (29). The SEQ may also be a useful tool in documenting individual experiences and informing healthcare policy addressing the service and support needs of individuals with TBI during the transition phase.
The first study aim was to consider the timing of sentinel events and the results indicate considerable variability across individuals, and that all events can occur at any stage during transition. The variation in timing within and across sentinel events is not entirely unexpected as recovery following TBI is acknowledged to be heterogeneous (30), and the sample in this investigation was quite varied in terms of injury severity. This variability in timing of events would suggest that services and policies developed to support individuals with TBI during transition should be designed flexibly to meet individual needs, with capacity for positive lifetime planning.
While it is important to consider the timing of events to inform service delivery, it is equally important to identify factors associated with the occurrence of these events the second study aim. This investigation aimed to build on previous research by using information available at hospital discharge to identify those individuals more likely to experience sentinel events in transition.
Consistent with previous research, individuals with higher levels of education and a less severe injury were more likely to return to work. Adjustment to injury, including mood and interpersonal interactions, was also important. Godfrey and colleagues (31) described a stress appraisal and coping model to explain the process of emotional adjustment following TBI. Findings of this investigation suggest that there is a bi-directional relationship between stress and life roles (i.e. work can contribute to stress responses such as depression or anxiety and stress can influence return to work). The most significant factor was length of stay (p = 0.001) reflecting that those with more severe injuries were less likely to return to work and this reinforces a need for community based rehabilitation and therapeutic interventions to support individuals with TBI in returning to work or to engage in other meaningful activities.
Returning to independent use of transport was related to length of hospital stay and sentinel events including transport use and financial strain during hospitalisation. To date most research examining transport use has considered a stroke population and thus this research adds to the body of knowledge for individuals with TBI (33). The relationship between length of stay and transport use may reflect injury severity, as individuals with cognitive impairments including safety awareness and judgement are likely to have more difficulty using transport (33). Financial strain in hospital was also related to independent use of transport both of which are unmet needs of individuals following TBI, suggesting that financial support is important to ensure individuals with TBI are not disadvantaged in accessing the community (34). Interestingly, individuals who had returned to independent use of transport while in hospital were less likely to experience this event post discharge. This suggests that once this event is achieved it is more often than not maintained, which is encouraging for individuals and therapists who may have use of transport as a goal for therapy.
Moving to a more restricted living situation after hospital discharge was more common among people not in a relationship, thus in this study it appeared that the need to change living situation was related to the level of support that was available to the individual with TBI (35). Presumably individuals in a relationship have access to family supports and therefore would have less of a need to change living environments. Availability of supports may also influence other explanatory variables (the MPAI-4 ability subscale and pre-discharge reduced therapy access) which showed relationships that were approaching significance. For example, consideration of an individual’s sensory, motor and cognitive abilities is an integral component of discharge planning and selection of the most appropriate home environment based on predicted support needs (36).
To date, there has been limited empirical research which has investigated factors associated with financial strain for individuals with TBI. In this investigation, a history of financial difficulty during the hospital admission was the factor most important in identifying individuals likely to experience financial strain post discharge (OR = 6.06). Individuals identified as having financial difficulty in hospital may therefore benefit from education and support to organise financial assistance before discharge where possible. The MPAI-4 ability subscale was also related to financial strain suggesting that level of function should be considered when determining eligibility for financial supports.
Individuals with a more severe injury and with poorer adjustment were also more likely to perceive difficulty accessing therapy services. Previous research has highlighted the long term challenges with community integration facing individuals with more severe injuries and thus the need for long term supports (28, 37). It is therefore alarming that during the transition to community, individuals with a more severe injury perceive therapy services to be lacking. In future research, it would be important to investigate whether the perceived difficulty in accessing therapy stems from unavailability of services, or whether it is related to differing perceptions of need. For instance, the ‘assessed need’ or need as defined by professionals or service providers may differ significantly from the ‘felt or expressed need’, which is more consistent with the individual’s experience (38, 39). Individuals with a more severe injury may have had greater exposure to rehabilitation services in the hospital, and therefore find the transition to the community where services are often less intensive a greater adjustment (i.e. greater expressed need). Furthermore, individuals who returned to independent transport use in hospital were less likely to encounter difficulty with therapy access. It may be the case that individuals who regain independence perceive less of a need to access therapy in the community. The concept of ‘need’ is a key distributional principle in social policy and therefore important in determining access to resources. The perception of restricted therapy access warrants further qualitative investigation to understand the nature of experiences in accessing therapy post hospital discharge.
Identifying factors that are related to the occurrence of sentinel events may assist services with allocation of resources to promote the occurrence of positive events (for example return to work) and prevent undesirable events (e.g. problems with therapy access) in transition. The finding that individuals with a more severe injury are more likely to encounter negative events in transition supports previous literature regarding community integration following TBI (40). The MPAI-4 was shown to be a good predictor of two events, namely financial strain and reduced therapy access. MPAI-4 items were developed to reflect the range of physical, cognitive, emotional, behavioural and social problems that people may experience following acquired brain injury (22). This measure or other measures of functioning and participation may therefore be useful in discharge planning or community rehabilitation, to identify individuals more likely to experience positive and/or negative transition events, and to allocate rehabilitation resources accordingly. Future research is required however to better identify the specific physical, cognitive or behavioural impairments that relate to the occurrence (or non-occurrence) of sentinel events in transition.
A novel component of this study was investigating whether links exist between sentinel events. Significantly, pre-discharge experiences of sentinel events were significant explanatory variables in three of the multiple logistic regression models (predicting financial strain, accommodation changes and independent transport use). This highlights the importance of these events to later experiences and has implications for practice as it may enable early intervention (e.g. referral for community based rehabilitation or financial assistance). It also highlights the individual nature of the transition experience as people experienced differing sentinel events at different stages throughout transition. The findings therefore suggest a need for co-ordinated service delivery from the point of hospital discharge, with individualised planning and the capacity for input and evaluation of services based on individual need. Future research could examine links between sentinel events occurring at different time points across the transition phase, and explore whether individuals experience clusters or sequences of events. For example, difficulty accessing therapy services and changing living situation after discharge may lead to added stress on caregivers and to relationship breakdown. This in turn may limit the individual’s ability to resume work, as previous research has identified the importance of informal supports for return to work (41). Identifying patterns in the occurrence of sentinel events would be important to prevent cycles of negative transition experiences.
Study limitations
This study used a relatively small sample size and a sample of participants with TBI, recruited from one site and individuals with very mild injuries (i.e. hospital stay of less than 4 days), and high care needs requiring discharge to another healthcare facility such as a nursing home or hospital were excluded. The generalizability of findings may be limited due to factors specific to the research location. The sample was very heterogeneous particularly in terms of injury severity and while a measure of global functioning was included (MPAI-4), there was no specific examination of the relationship between cognitive or physical impairments and occurrence of sentinel events. Future research should therefore consider the occurrence of sentinel events in relation to impairment, and among samples divided by injury severity (i.e. mild vs moderate vs severe) to see whether experiences differ. Use of logistic regression to examine factors associated with the occurrence of sentinel events limits findings as it assumes explanatory and outcome variables are constant and not time varying (e.g. level of functioning may change over time once individuals with TBI leave hospital). Additionally, missing data were evident in the analyses and may have biased the results.
Future research considering these sentinel events with a larger sample and in different contexts is required. Investigation of time-varying factors associated with the occurrence of sentinel events (e.g. the relationship between events such as return to work and the development of depression post discharge), is also recommended. Future research could consider using more specific measures of impairment (e.g. measures of cognitive function) to improve the predictive power of the models and better identify individuals requiring supports during transition. Additionally, qualitative research to obtain more detail on the experience of sentinel events would further enhance the knowledge base regarding the process of community re-integration.
In conclusion, this study demonstrated that both positive (e.g. return to work P = 0.27) and negative events (e.g financial strain P = 0.27) were frequently reported by individuals with TBI during the transition from hospital to the community. Furthermore, links exist in the occurrence of sentinel events, whereby experiences in hospital were related to events arising during transition. Consideration of sentinel events in rehabilitation programs both in hospital and in the community may enable early intervention, and contribute to the perception of a successful transition from hospital to home for individuals with TBI.
Acknowledgements
Funding support has been received by way of an Australian Research Council Linkage grant (LP0776294) with partner organisations Department of Communities (Disability Services) and the Acquired Brain Injury Outreach Service. Funding agencies had no influence on data interpretation and conclusions drawn.
The authors wish to thank Professors Linda Worrall and Lesley Chenoweth, Doctors Tamara Ownsworth and Melissa Kendall, and Cassandra Shields for their input into the conceptual design of this project, and assistance with data collection.
References