OBJECTIVE: The aim of this study was to determine how employee well-being, psychosocial factors at work, leadership and perceived occupational health services predict entering rehabilitation as modelled in the Job Well-being Pyramid.
METHODS: A random population of 967 civil servants participated in a survey on psychosocial factors and health at work in 2000 in Finland. A total of 147 employees entered rehabilitation during the median follow-up time of 7 years.
RESULTS: Permanent employment, large organizations, feedback from supervisors, client violence and physically monotonous work were associated with an increased rate of entering rehabilitation, whereas physical jobs, clear aims, high appreciation, job satisfaction and job enjoyment were associated with a decreased rate of entering rehabilitation. Employee well-being in general was also associated with entering rehabilitation, and this was decreased by good work ability, good health, mental well-being and physical fitness and increased by constant musculoskeletal symptoms. On the other hand, support from supervisors, job control, work pressure, team climate at work, communication, bullying and discrimination, physical work environment, and sense of coherence appeared to have no association.
CONCLUSION: Various psychosocial factors at work and job well-being predict entering rehabilitation. The association between employee health and entering rehabilitation refers to the fact that the selection process for rehabilitation works reasonably well and those in need of rehabilitation are also granted it. In general, these findings coincide well with the Job Well-being Pyramid model. Improving job conditions and well-being at work is likely to decrease the need for rehabilitation.
Key words: rehabilitation; psychosocial factors; well-being; cohort study.
J Rehabil Med 2012: 44: 669–676
Correspondence address: Anne Lamminpää, University of Helsinki, Hjelt Institute, FI-00014 Helsinki, Finland. E-mail: anne.lamminpaa@fimnet.fi
Submitted November 6, 2011; accepted March 14, 2012
INTRODUCTION
In a successful rehabilitation process employees, employers and the social insurance organization all attain their goals. Employees want to enhance their health and work ability, whereas employers would like to see employees with improved job productivity. The main interests of the social insurance institution, on the other hand, are to decrease the number and length of periods of sick leave and to avoid having to provide disability pensions. Therefore, the employees chosen for rehabilitation should be those who are likely to benefit from it. They should be motivated and committed to rehabilitation. The employer loses the work input of an employee during rehabilitation, yet the social insurance organization pays most of the expenses of rehabilitation. Rehabilitation can be a relatively inexpensive way to prevent or postpone early retirement.
Any type of rehabilitation may have an effect at an early stage of decreased work ability, but may be ineffective later on if applied as the only mode of rehabilitation (1). When chronic disability is present, multimodal medical rehabilitation needs to be combined with vocational rehabilitation in order to reduce absenteeism and disability pension. It is also essential that the workplace is integrated into rehabilitation. Furthermore, ongoing good health and workplace support have the greatest potential to facilitate long-term return-to-work (2).
Disorders, mainly mental or musculoskeletal, have been recognized to have major consequences for employees, employers and society, particularly in terms of unnecessarily long periods of sick leave and undue early retirements. There is a consensus that, through rehabilitation, it is possible to shorten long periods of sick leave and postpone, if not prevent, early retirements. Therefore, in Finland, occupational health services are required by law to support the rehabilitation process by selecting employees for rehabilitation and following them up afterwards (3). When symptoms occur, the collaboration between employees, workplace and the occupational health services is emphasized; the occupational health services having the role of coordinator.
The concept of “functional health” reached a new level in 2001 in the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health (ICF) (4). The health and health-related domains are classified from the perspectives of body, individual and society by means of two lists: a list of body functions and structure and a list of activity and participation. Since an individual’s functioning and disability always occurs in some environment, the ICF also includes a list of environmental factors. The ICF Core Set has been further developed to serve the needs of vocational rehabilitation (5).
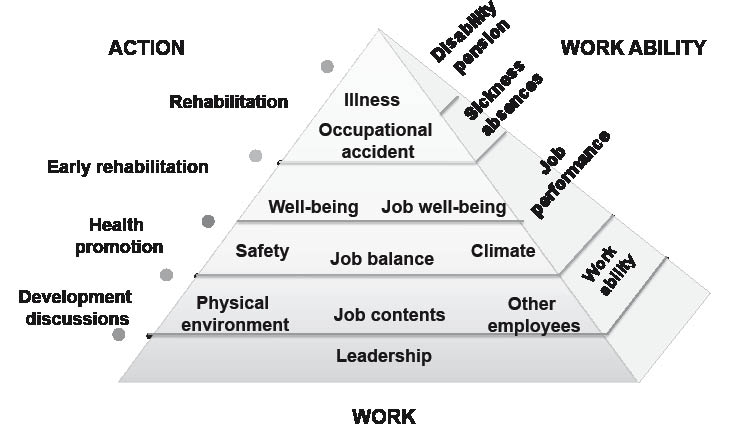
Another comprehensive concept concerning the multiple factors involved with employees’ well-being is visualized in the Job Well-being Pyramid (Fig. 1). The Job Well-being Pyramid, which was developed in Finland, is a hierarchical model on the working environment and its relationships with employee health (1, 6–8). Each side of the Pyramid is an independent entity: Work, Work Ability, and Action. In the Job Well-being Pyramid, the best results are thought to be achieved when problems are prevented at lower levels, e.g. job content, work environment and job well-being. Scientific literature supports this assumption (1, 6–8).
Fig. 1. The job well-being pyramid.
We have tested the validity of the Job Well-being Pyramid among civil servants in Finland. The governmental sector comprises approximately 120,000 employees. The administration is mainly run under 11 ministries, the largest branches of administration being education (25% of total personnel), internal affairs, defence, finance, justice, and employment and the economy. The rate of sickness absence has been quite stable, 8–9 work days/person work year, and the disability pension rate has been approximately 1%. The number of occupational accidents in the state sector has been quite low, being 4.7 per 100 person work years in 2010. We have reported previously that employee well-being, in terms of job satisfaction, health, sense of coherence and physical well-being, predicted sickness absences, occupational accidents and disability pensions (8).
The aim of this study was to examine to what extent leadership, work-related psychosocial factors, employee well-being and perceived occupational health services predict entering rehabilitation.
METHODS
Participants
The participants in this study are those civil servants who responded to the “All Well at Work?” survey in 2000. A random sample from the Finnish governmental personnel was invited to participate in the survey. The study population represents all administrative branches.
“All Well at Work?” survey
Data were collected via a postal questionnaire. Out of 2,000 invitees, 998 employees (54%) responded. Thirty-one respondents declined to allow the use of their answers in any further study; therefore, 967 participants could be included in this study. The proportion of women and the mean age were slightly higher among the respondents than among the invitees (52% vs 47% and 44.8 years vs 42.4 years, respectively).
The “All Well at Work?” survey measured factors describing psychosocial and organizational working conditions, health, work ability and personal resources. Characteristics of work and work organization were measured according to the main items of the Healthy Organization Questionnaire (9). The main parameters concerning health and work ability were musculoskeletal symptoms, mental strain by the General Health Questionnaire 12 (GHQ-12) (10, 11), and work ability by the Work Ability Index (WAI) (12). Personal resources were measured with the Sense of Coherence Scale (SOC) (13).
Follow-up
The follow-up was register-based and ended at the end of employment, at pension, at death, or at the end of study on 31 December 2007. Data on rehabilitation were provided by the Social Insurance Institution of Finland. Data on occupational vocational rehabilitation were provided by the Actuary Division of the State Treasury. The follow-up time varied from 0.03 to 7.3 years, the median time being 7.3 years. Two-thirds of the study population reached the maximum follow-up time.
Predictors
The predictors are covered briefly here; a full description is given in Appendix I.
Work-related psychosocial factors. Organizational factors were measured by questions on the type of job contract (permanent or temporary) and the size of the organization (number of employees). Leadership was measured by two questions; one on support and one on feedback from the supervisor. Job content was measured by questions on job type, clarity of aims at work and job control, whereas job balance was measured by two questions on work pressure. Social work climate was assessed by questions on team climate at work, communication, appreciation at work, bullying and discrimination. Physical work environment was measured by questions on client violence, monotonous work movements, crowdedness of workplace and other physical factors.
Employee well-being and work ability. Job well-being was measured by two questions, one on satisfaction and one on enjoyment at work. Health was measured by a single question. Mental well-being was assessed by a single question and the GHQ-12 and SOC scales. The GHQ version with 12 items, with total score ranging from 12 to 48 was used. Also, the SOC was used in its shorter 13-item version, the total score ranging from 7 to 91. Physical well-being was measured by two questions; one on physical fitness and one on musculoskeletal symptoms. Work ability was measured by the WAI, which has 7 items, the index being the sum of all items (7–49).
Work health promotion and occupational health services. Work health promotion was measured by two questions, one on recreation and exercise and one on promotion of mental well-being. Employees’ perceptions on occupational health services were assessed by a 3-part question concerning preventive healthcare, care of sickness and disease and rehabilitation.
Outcome
Rehabilitation. The purpose of the rehabilitation is to improve work ability. In Finland, the Social Insurance Institution is the main provider of rehabilitation measures for working age people. It has a statutory duty to arrange rehabilitation as vocational rehabilitation for those with diminished working capacity and as medical rehabilitation for severely handicapped people. In addition, some rehabilitation is discretionary, based on annual appropriations and consists of, for example, vocationally devoted courses for occupational groups without severe symptoms. Vocational rehabilitation, on the other hand, is granted by the pension system either for preventive purposes or as an alternative to the disability pension if the rehabilitation prospects are considered good.
In this study, the outcome included group-based rehabilitation courses, vocational training, rehabilitation examinations, work testing, and training aimed at maintaining work capacity, and medical in-patient rehabilitation that goes beyond curative treatment and is necessary to maintain or improve functional capacity and work ability.
RESULTS
Baseline characteristics
The study population consisted of 458 men (47%) and 509 women (53%). The mean age was 45.1 (standard deviation (SD) 9.7) years, and the study population included employees of all ages (Table I). The mean overall tenure was 22.7 years, and mean tenure at governmental service was 16.9 years. Approximately one-third of the study population had a university-level professional education, and approximately half were lower officials. One-quarter had a supervisory post. Most participants had a permanent employment (86%) and a regular day shift (83%). Only 5% of the participants had purely physical work.
| Table I. Baseline characteristics in the “All Well at Work?” survey among civil servants in Finland in 2000 (n = 967) |
| Characteristics | |
| Age, years, mean (SD) [range] | 45.1 (9.7) [23–65] |
| Overall tenure, years, mean (SD) [range] | 22.7 (10.5) [1–50] |
| Governmental tenure at the beginning of follow-up, years, mean (SD) [range] (n = 966) | 16.9 (10.1) [0–45] |
| Sex, n (%) | |
| | Men | 458 (47) |
| | Women | 509 (53) |
| Professional education, n (%) | |
| | Primary | 306 (32) |
| | Middle | 309 (32) |
| | University or collage, n (%) | 350 (36) |
| Professional status, n (%) | |
| | Higher office personnel | 366 (38) |
| | Lower office personnel | 496 (52) |
| | Other employees | 92 (10) |
| Supervisory status, n (%) | |
| | Yes | 252 (26) |
| | No | 708 (74) |
| Work shift, n (%) | |
| | Regular day shift | 795 (83) |
| | Varying or periodical shift | 139 (14) |
| | Part-time | 25 (3) |
| SD: standard deviation. |
Rehabilitation
Of the participants, 118 (12%) had been in rehabilitation during the previous year at the beginning of the study, and 147 (15%) were in rehabilitation during follow-up. Note that the self-reported previous rehabilitation consisted of any kind of measure with rehabilitative intention, whereas the follow-up was based only on data from registers, as mentioned above.
Permanent employment (relative risk (RR) 1.54, 95% confidence interval (CI) 0.75–3.17), large organizations (1.45, 0.85–2.47) and feedback from supervisors (1.50, 0.91–2.48) appeared to be associated with an increased rate of entering rehabilitation, whereas support from supervisors had no association (Table II). Physical job (0.62, 0.26–1.50) and clarity of aims (0.68, 0.36–1.28) appeared to predict a decreased rate of entering rehabilitation (Table III). Job control and work pressure were not associated with rate of entering rehabilitation.
| Table II. Association between work factors and leadership and rehabilitation (n = 967) |
| Factor | Rehabilitation |
| Subjects n | Cases n | RR (95% CI) |
| Organizational factors | | | |
| Job contract | 966 | 147 | |
| | Temporary | 136 | 11 | 1.00 |
| | Permanent | 830 | 136 | 1.54 (0.75–3.17) |
| Personnel | 962 | 147 | |
| | ≤ 100 | 571 | 84 | 1.00 |
| | 101–500 | 285 | 45 | 1.04 (0.71–1.52 |
| | < 500 | 106 | 18 | 1.45 (0.85–2.47) |
| Leadership | | | |
| Support from supervisors | 958 | 145 | |
| | Seldom or almost never | 239 | 34 | 1.00 |
| | Sometimes | 282 | 37 | 1.00 (0.61–1.63) |
| | Rather often or always | 437 | 74 | 1.15 (0.71–1.88) |
| Feedback from supervisors | 958 | 145 | |
| | Seldom or almost never | 445 | 61 | 1.00 |
| | Sometimes | 324 | 49 | 1.06 (0.70–1.61) |
| | Rather often or always | 189 | 35 | 1.50 (0.91–2.48) |
| RRs were adjusted for sex, age, education, change in well-being during previous year, sickness absence during previous year, previous participation in work health promotion, and previous participation in rehabilitation. RR: risk ratio; CI: confidence interval. |
| Table III. Association between job content and balance and rehabilitation (n = 967) |
| Predictor | Rehabilitation |
| Subjects n | Cases n | RR (95% CI) |
| Job content | | | |
| Job type | 965 | 147 | |
| | Mental | 728 | 111 | 1.00 |
| | Both | 190 | 30 | 0.90 (0.57–1.43) |
| | Physical | 47 | 6 | 0.62 (0.26–1.50) |
| Clarity of aims at work | 962 | 146 | |
| | Poor or rather poor (2–6) | 80 | 14 | 1.00 |
| | Rather good (7–8) | 435 | 71 | 0.87 (0.46–1.62) |
| | Very good (9–10) | 447 | 61 | 0.68 (0.36–1.28) |
| Job control | 954 | 146 | |
| | Low (4–9) | 324 | 51 | 1.00 |
| | Somewhat (10–13) | 383 | 64 | 1.24 (0.82–1.87) |
| | High (14–20) | 247 | 31 | 1.04 (0.61–1.79) |
| Job balance | | | |
| Work pressure | 962 | 146 | |
| | Seldom or now and then (2–6) | 413 | 59 | 1.00 |
| | Rather often (7–8) | 351 | 56 | 1.11 (0.75–1.65) |
| | Very often (9–10) | 198 | 31 | 1.03 (0.63–1.69) |
| RRs were adjusted for sex, age, education, change in well-being during previous year, sickness absence during previous year, previous participation in work health promotion, and previous participation in rehabilitation. RR: risk ratio; CI: confidence interval. |
High appreciation at work appeared to decrease the likelihood of entering rehabilitation (RR 0.75, 95% CI 0.42–1.33) (Table IV). Other factors measuring the social environment, i.e. team climate at work, communication, and bullying and discrimination, appeared not to have any association with rate of entering rehabilitation. Client violence (1.31, 0.76–2.26) and physically monotonous work (1.64, 0.94–2.85) were associated with an increase in rate of entering rehabilitation, whereas there was no such association concerning other factors of physical environment.
| Table IV. Association between social and physical work environment and rehabilitation (n = 967) |
| Predictor | Rehabilitation |
| Subjects n | Cases n | RR (95% CI) |
| Social work environment | | | |
| Team climate at work | 951 | 143 | |
| | Poor (5–12) | 194 | 31 | 1.00 |
| | Neutral (13–17) | 337 | 46 | 0.87 (0.55–1.37) |
| | Good (18–25) | 420 | 66 | 1.07 (0.69–1.66) |
| Communication | 942 | 135 | |
| | Poor (5–12) | 131 | 19 | 1.00 |
| | Neither good nor poor (13–17) | 371 | 52 | 0.98 (0.55–1.77) |
| | Good (18–25) | 440 | 64 | 1.12 (0.60–2.11) |
| Appreciation at work | 960 | 145 | |
| | Little or very little | 147 | 26 | 1.00 |
| | Moderate | 324 | 44 | 0.67 (0.39–1.18) |
| | Much or very much | 489 | 75 | 0.75 (0.42–1.33) |
| Bullying and discrimination | 955 | 145 | |
| | Sometimes (2–4) | 106 | 21 | 1.00 |
| | Seldom (5–7) | 397 | 56 | 0.93 (0.50–1.72) |
| | Never (8) | 452 | 68 | 0.99 (0.52–1.89) |
| Physical work environment | | | |
| Client violence | 963 | 146 | |
| | Never | 668 | 92 | 1.00 |
| | Seldom | 186 | 36 | 1.52 (1.02–2.26) |
| | Now and then or often or very often | 109 | 18 | 1.31 (0.76–2.26) |
| Physically monotonous | 963 | 146 | |
| | None or doesn’t bother | 494 | 61 | 1.00 |
| | Bothers somewhat | 375 | 65 | 1.28 (0.88–1.86) |
| | Bothers a lot | 94 | 20 | 1.64 (0.94–2.85) |
| Crowdedness and noise | 961 | 147 | |
| | None or doesn’t bother | 544 | 80 | 1.00 |
| | Bothers somewhat | 318 | 52 | 1.08 (0.73–1.58) |
| | Bothers a lot | 99 | 15 | 0.98 (0.53–1.82) |
| Other environmental factors | 961 | 147 | |
| | None or doesn’t bother | 324 | 45 | 1.00 |
| | Bothers somewhat | 412 | 63 | 0.92 (0.61–1.39) |
| | Bothers a lot | 225 | 39 | 1.06 (0.64–1.77) |
| RRs were adjusted for sex, age, education, change in well-being during previous year, sickness absence during previous year, previous participation in work health promotion, and previous participation in rehabilitation. RR: risk ratio; CI: confidence interval. |
The associations between well-being, health and work ability and entering rehabilitation were consistent (Table V). Good levels of job satisfaction (RR 0.69, 95% CI 0.42–1.15), job enjoyment (0.77, 0.48–1.25), health (0.52, 0.26–1.04), mental well-being (0.76, 0.45–1.34), psychiatric distress measured by GHQ-12 (0.73, 0.50–1.08), physical fitness (0.52, 0.29–0.94) and WAI (0.22, 0.10–0.49) predicted a decrease in entering rehabilitation. On the other hand, constant musculoskeletal symptoms predicted an increase in the rate of entering rehabilitation (2.72, 1.55–4.77). SOC was the only factor that appeared to have no association with rehabilitation.
| Table V. Association between well-being, work ability and rehabilitation (n = 967) |
| Predictor | Rehabilitation |
| Subjects n | Cases n | RR (95% CI) |
| Well-being | | | |
| Job satisfaction | 967 | | 960 |
| | Rather or very dissatisfied | 100 | 18 | 1.00 |
| | Neither satisfied nor dissatisfied | 204 | 28 | 0.57 (0.31–1.05) |
| | Rather or very satisfied | 663 | 101 | 0.69 (0.42–1.15) |
| Job enjoyment | 967 | | 960 |
| | Seldom or almost never | 140 | 25 | 1.00 |
| | Occasionally | 401 | 58 | 0.71 (0.44–1.14) |
| | Rather or very often | 426 | 64 | 0.77 (0.48–1.25) |
| Health | 962 | | 958 |
| | Rather or very poor | 53 | 15 | 1.00 |
| | Moderate | 236 | 38 | 0.52 (0.27–1.01) |
| | Rather or very good | 673 | 93 | 0.52 (0.26–1.04) |
| Mental well-being | 961 | | 957 |
| | Rather or very poor | 98 | 20 | 1.00 |
| | Moderate | 290 | 53 | 0.94 (0.55–1.59) |
| | Rather or very good | 573 | 73 | 0.78 (0.45–1.34) |
| GHQ-12 | 954 | | |
| | “Case” (4–12) | 184 | 42 | 1.00 |
| | Healthy (0–3) | 770 | 103 | 0.73 (0.50–1.08) |
| SOC | 944 | | 938 |
| | Weak (13–45) | 45 | 9 | 1.00 |
| | Moderate (46–71) | 176 | 31 | 0.94 (0.44–2.01) |
| | Strong (72–91) | 723 | 105 | 0.87 (0.43–1.75) |
| Physical fitness | 963 | | 959 |
| | Rather or very poor | 80 | 19 | 1.00 |
| | Moderate | 323 | 56 | 0.72 (0.41–1.27) |
| | Rather or very good | 560 | 72 | 0.52 (0.29–0.94) |
| Musculoskeletal symptoms | 961 | | 956 |
| | None | 222 | 17 | 1.00 |
| | Occasionally | 491 | 69 | 1.59 (0.93–2.73) |
| | Constantly | 248 | 61 | 2.72 (1.55–4.77) |
| Work ability | | | |
| WAI | 916 | | 913 |
| | Poor (7–27) | 38 | 14 | 1.00 |
| | Moderately poor (28–36) | 136 | 29 | 0.42 (0.21–0.84) |
| | Good (37–43) | 453 | 69 | 0.30 (0.15–0.62) |
| | Excellent (44–49) | 289 | 29 | 0.22 (0.10–0.49) |
| RRs were adjusted for sex, age, education, change in well-being during previous year, sickness absence during previous year, previous participation in work health promotion, and previous participation in rehabilitation. RR: risk ratio; CI: confidence interval; GHQ: General Health Questionnaire; SOC: Sense of Coherence; WAI: Work Ability Index. |
Work health promotion, such as recreation and exercise or promotion of mental well-being, was not associated with entering rehabilitation (Table VI). Neither the preventative nor healthcare measures provided by the occupational health services appeared to be associated with the rate of entering rehabilitation, although those employees who had no opinion on healthcare services entered rehabilitation less often than others (RR 0.69, 95% CI 0.39–1.22). Instead, the rehabilitation services perceived as good were associated with a decreased rate of entering rehabilitation (0.49, 0.26–0.94).
| Table VI. Association between health promotion at work, occupational healthcare and rehabilitation (n = 967) |
| Predictor | Rehabilitation |
| Subjects n | Cases n | RR (95% CI) |
| Work health promotion | | | |
| Recreation and exercise | 966 | 147 | |
| | Rather or very little | 253 | 34 | 1.00 |
| | Somewhat | 309 | 47 | 1.18 (0.74–1.88) |
| | Rather or very much | 404 | 66 | 1.18 (0.73–1.93) |
| Promotion of mental well-being | 964 | 147 | |
| | Rather or very little | 577 | 88 | 1.00 |
| | Somewhat | 255 | 37 | 0.84 (0.55–1.28) |
| | Rather or very much | 132 | 22 | 1.11 (0.65–1.89) |
| Occupational healthcare | | | |
| Prevention | 942 | 144 | |
| | Rather or very badly | 327 | 59 | 1.00 |
| | Neither well nor badly | 310 | 42 | 1.00 (0.61–1.66) |
| | Rather or very well | 305 | 43 | 1.06 (0.56–2.03) |
| Health care | 947 | 146 | |
| | Rather or very badly | 111 | 23 | 1.00 |
| | Neither well nor badly | 252 | 33 | 0.69 (0.39–1.22) |
| | Rather or very well | 584 | 90 | 1.07 (0.61–1.86) |
| Rehabilitation | 932 | 143 | |
| | Rather or very badly | 265 | 52 | 1.00 |
| | Neither well nor badly | 318 | 43 | 0.57 (0.34–0.96) |
| | Rather or very well | 349 | 48 | 0.49 (0.26–0.94) |
| RRs were adjusted for sex, age, education, change in well-being during previous year, sickness absence during previous year, previous participation in work health promotion, and previous participation in rehabilitation. RR: risk ratio; CI: confidence interval. |
DISCUSSION
Ill-health, diseases, disabilities and decreased work ability are the most common reasons for entering rehabilitation. Yet, it is not always evident that a disease is the reason for decreased work ability. The aim of this study was to identify to what extent employee well-being, work-related psychosocial factors, leadership, and perceived occupational health services predict entering rehabilitation, as modelled in the Job Well-being Pyramid. We found that the overall entity complied well with the model and that all levels of the pyramid were associated with entering rehabilitation even though some individual factors showed no association.
Permanent employment and large organizations were associated with an increased rate of entering rehabilitation. Temporary workers tend to be younger and probably healthier, as do those with permanent employment contracts, which may partly explain the result even though the analyses were adjusted for age and previous sickness absences. On the other hand, the application process for rehabilitation takes time and neither the employee nor the employer are willing to start a long application process during a short temporary or fixed-term contract. Other authors have also noted that the rehabilitation system is more likely to grant rehabilitation to those with permanent employment than to those without employment (14, 15). Employees with temporary or atypical employment are easily missed, and nowadays the development projects on work-related rehabilitation in Finland increasingly also attempt to involve workers with atypical employment and those who are self-employed (16–18). As for organization size, it may be easier to pursue rehabilitation in large organizations.
In our study the psychosocial factors at work affected the rate of entry to rehabilitation. Feedback from supervisors was associated with an increased rate of entering rehabilitation, whereas perceived support from supervisors had no association. This apparent inconsistency may be due to methodological issues, such as poorly formulated questions concerning the perceived behaviour of the supervisor. The finding concerning feedback from supervisors may also be true, in the sense that a good supervisor monitors the well-being of workers and supports rehabilitation if an employee appears to be in need of it. In other words, good workplaces both prevent the need for rehabilitation and support employees in seeking entry to rehabilitation.
Clear aims and high levels of appreciation at work were associated with a decreased rate of entering rehabilitation, whereas job control, work pressure, team climate at work, communication, bullying and discrimination appeared to have no association. The latter factors may have methodological weaknesses. The study population was reasonably homogenous concerning work pressure and bullying and discrimination, thus a small but true effect may not have been detected. Furthermore, the impact of factors such as job control, team climate and communication may be too indirect to be predictive for rehabilitation.
Client violence and physically monotonous work were associated with an increased rate of entering rehabilitation, whereas physical employment was associated with a decreased rate, and other physical work environment factors appeared to have no association with entering rehabilitation. It is likely that monotonous work increases the need for rehabilitation, but other associations or the lack of them are not as straightforward. The finding on client violence probably represents more the impact of profession than the client violence as such. Namely, those professionals such as policemen and prison officers, who mostly encounter violent clients, have demanding jobs both psychosocially and physically. Physical work, on the other hand, appears to decrease the need for rehabilitation, which may reflect the fact that a physically demanding job keeps an employee physically fit, but also that physically unfit or unhealthy workers pursue physically less demanding work. The questions on crowdedness and noise in the workplace and other physical factors, such as temperature, lighting, draughts and indoor air quality, were too ambiguous, and thus methodologically weak, and our findings of no associations concerning them cannot be considered reliable.
Our findings that job satisfaction and job enjoyment were predictive concerning entering rehabilitation were consistent with published research in which job satisfaction has been associated with both the health and mental and physical well-being of employees (8, 19). The importance of work that not only is within the individual’s physical abilities, but also fulfils the worker’s emotional and intellectual needs, has been emphasized (2). There are factors beyond the employees’ tangible environment that help them to manage and overcome the difficulties they experience. These include personal characteristics and a variety of other experiential influences associated with undertaking tasks and actions. Together with the desire to be working, job enjoyment and personal satisfaction influence all return-to-work phases, but particularly the later ones. Young’s (2) findings suggest an opportunity for proactive intervention and early rehabilitation.
It is important to define properly the risk groups that are in obvious need of rehabilitation and to find those employees who are likely to benefit from and reach the goals of rehabilitation. In our study, decreased health, mental and physical well-being and work ability was associated with entering rehabilitation, referring to the fact that the selection process worked well and those entering rehabilitation were indeed in need of it. On the other hand, the authors of another Finnish cohort study suspected that preventive measures to reduce the risk of disability pension amongst high-risk employees through rehabilitation are not targeted as intended (15). They reported that many risk factors previously found to be associated with high risks of early retirement on health grounds were not predictive for future participation in rehabilitation. Yet, their findings concerning the type of job contract and job control were similar to ours.
In our study, GHQ was associated with entering rehabilitation. The GHQ is a good predictor of sick leave and disability pension (8), and could therefore also serve as a predictor of the need for rehabilitation. From the well-being measures we used, the SOC was the only one that had no association with entering rehabilitation, which was unexpected because it has predicted sickness absences and disability pension as mentioned earlier. In theory, the SOC is conceptually more a measure of the construct and psychological resources of one’s personality (19) than of mental well-being, and the phenomenon that the SOC describes may not be influential in the selection process for rehabilitation.
For measuring work ability, the WAI has been used in occupational health services in Finland for years. It detects well those subjects whose work ability has decreased, and offers an easy way to assess the potential need for rehabilitation. However, rehabilitation is also aimed at those who are at risk of diminishing work ability. In one Finnish study concerning early rehabilitation, the participants were initially in a worse condition than the non-participants for all measures, e.g. GHQ, musculoskeletal symptoms and WAI, and the two-year follow-up showed that the criteria for selecting the correct target group were largely fulfilled and early rehabilitation covered the majority of persons in need (20). It is evident that more sensitive scales than the WAI are needed in order to target rehabilitation activities early enough. The GHQ-12 might serve as such an auxiliary scale and should be further evaluated in this respect. In addition, the SOC merits further testing before any final conclusions on its predictive value.
Work health promotion had no association with entering rehabilitation in our study, which accords with the literature (1). Nevertheless, the finding may refer both to the fact that the interventions were ineffective and that the follow-up time was too short. The perceived competence of occupational health services in prevention or healthcare also appeared to have no association with entering rehabilitation. Yet, the U-shaped association between healthcare services and entering rehabilitation may be a true one: those who are healthy and do not use occupational health services are neutral in their opinion about them. The perceived good competence of occupational health services in rehabilitation instead did predict the employee’s later participation in rehabilitation. The rehabilitative activities provided by the occupational health services are likely to decrease the need to seek rehabilitation from other sources.
The ICF is a known model for rehabilitation, yet the ICF Core Set awaits further validation. The findings of our study are mostly consistent with the ICF conceptualization, even though our study was based on the Job Well-being Pyramid model. Our findings coincided well with what was expected based on the pyramid model. Items on the Work side of the pyramid, such as leadership, work resources, perceptual level of work, well-being and health, were predictors of entering rehabilitation.
In conclusion, psychosocial factors at work predict entering rehabilitation, yet the measurement of psychosocial factors is prone to methodological weaknesses, which may hide or attenuate true associations. Factors that are perceived more personally, such as feedback from supervisors and appreciation at work, may have more direct impact than, for example, team climate and communication. In general, the findings of this study coincide well with the Job Well-being Pyramid model. Improving job conditions and well-being at work is likely to decrease the need for rehabilitation.
REFERENCES