OBJECTIVE: To evaluate the long-term effects of two different rehabilitation programmes for patients on long-term sick leave for burnout.
DESIGN: Three-year follow-up of a randomized controlled trial with two 1-year group programmes: (A) cognitively oriented behavioural rehabilitation in combination with Qigong; and (B) Qigong alone.
Patients: A total of 107 patients with burnout (78 women and 29 men), who all completed the 1-year rehabilitation programme per-protocol, were asked to participate in the follow-up.
METHODS: At the 3-year follow-up, data on psychological measures, sick leave and use of medication were compared between the programmes.
RESULTS: Patients in programme A reported being significantly more recovered from their burnout (p = 0.02), reported lower levels of burnout (p = 0.035), used more cognitive tools learned from the programme (p < 0.001), and had reduced their use of medication for depression (p = 0.002). No significant differences were found between the groups in terms of sick leave rates; both groups had improved.
CONCLUSION: A multimodal rehabilitation including cognitively oriented behavioural rehabilitation and Qigong showed positive effects 3 years after the end of intervention. The results indicate that, for many burnout patients on sick-leave, it takes time to implement cognitive tools and to establish new behaviours.
Key words: randomized controlled trial; follow-up studies; burnout; cognitive therapy; sick leave.
J Rehabil Med 2012; 44: 684–690
Correspondence address: Therese Stenlund, Department of Community, Medicine and Rehabilitation, Division of Physiotherapy, Umeå University, Umeå, Sweden. E-mail: therese.stenlund@physiother.umu.se
Submitted September 7, 2011; accepted February 28, 2012
INTRODUCTION
Burnout was first described in 1974 by Freudenberger (1), who stated that the condition was accompanied by feelings of exhaustion and fatigue in combination with physical symptoms. Maslach et al. (2) subsequently defined burnout as a work-related syndrome among individuals who worked with people. However, the definition of burnout was later broadened to include non-working situations (3). The Swedish National Board of Health and Welfare substituted burnout for “exhaustion disorder” (ICD-10, F43.8A) (4, 5) in 2003. Exhaustion disorder is characterized by physical and mental exhaustion as a result of identifiable stressors (both at and outside work) for at least 6 months. One of the diagnostic criteria is that “symptoms cause clinically significant distress or impairment in social, occupational or other important areas of functioning” (6). In 2009, long-term sick leave in Sweden (60 days or longer) consisted of 26.8% mental disorders, whereof stress-related disorders (mainly F41, F43) and depression (mainly F32, F33) were the most common diagnoses (7).
Despite the fact that long-term sick leave due to stress-related conditions and exhaustion disorders has increased, there is still a lack of evidence about which methods are most effective to rehabilitate patients with these diagnoses. Most of the previously conducted randomized controlled trials have evaluated interventions directed at the individual, often including cognitive behaviour therapy (CBT) principles, but with marginal effects on psychological variables (8–14), return to work, and sick leave (9, 11–14) in comparison with control groups. Randomized workplace interventions are scarce. However, Blonk et al. (10) compared two different interventions, extensive CBT and brief CBT combined with workplace intervention, with a control condition, and showed that all groups improved and reported reduced psychological complaints. The combined workplace intervention also gave a favourable effect on return to work. van Oostrom et al. (15) compared usual care with a workplace intervention involving sick-listed employees and their supervisors, in order to reach consensus about an action plan for return to work. Again, both groups improved in stress-related symptoms and return to work, but the employees in the workplace intervention group who had reported intention to return to work despite remaining symptoms, also returned to work earlier (after 55 days compared with 120 days).
Studies including participants who report a short period of sick leave prior to interventions have often shown reduced sick leave or earlier return to work (8, 10, 15) compared with studies including participants reporting a long-term sick leave period (11, 13, 14). Group rehabilitation for patients with burnout has been shown to have advantages, since the group can provide affirmation and support, which are basic factors in behavioural change (16).
In Sweden, rehabilitation of patients with stress-related disorders is recommended to start early in the disease process (preferably within two months of sick leave) and to consist of a multimodal rehabilitation, which includes measures to establish a balance between activity and recovery, stress reduction, conversational therapy with focus on work and other stressors (preferably in group), and work rehabilitation support (17).
Despite these recommendations and evidence from studies evaluating rehabilitation programmes for these patients, there is a lack of knowledge of the long-term effects of these programmes. In a quasi-experimental study (18), 40% had returned to work 5 years after a stress management intervention of 24 women who were on long-term sick leave due to work-related, psychological complaints. To our knowledge, however, the longest periods of follow-up in randomized controlled studies are those reported by Heiden et al. (11) and Stenlund et al. (13). These studies have reported results from 12-month follow-ups after the end of the rehabilitation. Clinically, the rehabilitation goal of back to work is still troublesome for many patients with severe burnout. Therefore, more knowledge of sick leave reduction is needed, as is knowledge of the experience of recovery in the longer term.
The aim of this study was to evaluate the long-term effects (3-year follow-up after the end of intervention) of two different rehabilitation programmes for patients on long-term sick leave due to burnout, with respect to psychological measures, sick leave and use of medication.
METHODS
Study design and study population
A randomized controlled trial, rehabilitation for stress-related disease and burnout (REST) was performed at the Stress Clinic, University Hospital of Umeå, from December 2002 until May 2006. A total of 136 patients with a mean sick leave of 335 (standard deviation 170) days until randomization participated in the study. Inclusion criteria for the patients in the REST study were: age 25–55 years; sick leave for burnout ≥ 25% of working hours during the previous 3–24 months; and a mean score ≥ 4.6 on the Shirom-Melamed Burnout Questionnaire (SMBQ) (19–21). The inclusion criteria were initially checked by the physician taking the patient’s history. The REST study is described more in detail elsewhere (13), as are sex differences in baseline data (22). The REST study, and the supplementary, 3-year follow up study assembled 3 years after the end of the 1-year rehabilitation, were approved by the Regional Ethical Review Board in Umeå (Fek dnr 02-311; dnr 2009-1373; dnr 2011-121-32M).
Rehabilitation programmes
Rehabilitation programme A consisted of cognitively oriented behavioural rehabilitation (CBR) in group in combination with Qigong. The CBR groups comprised 6–9 patients who met in 30 3-h long sessions, which included discussions of session-specific themes. There were 5 key components of the CBR programme: (i) education, i.e. stress responses, sleep and recovery, affect awareness, and medication; (ii) awareness of reactions and “self-talk”; (iii) development of behavioural/cognitive/emotional skills; (iv) spiritual issues and life values; and (v) return to work. The programme was developed by psychologists, and carried out by two physiotherapists who were specially trained in the method and served as group leaders (23). There were also short follow-up meetings, 3, 6 and 12 months after the end of the 1-year rehabilitation. Spouses and/or relatives were invited to 3 separate group meetings during the first year. In parallel with CBR, the patients performed Qigong in a group, once a week, in 1-h sessions. The Qigong programme comprised 3 parts: (i) warming up with gentle movements; (ii) movements to affect body awareness, balance and coordination, breathing and muscular tension; and (iii) relaxation and mindfulness. Work rehabilitation support was offered to the patients at the end of the 1-year rehabilitation, and consisted of a rehabilitation meeting with the patient, the responsible physician, the employer, and a clerk from the Social Insurance Agency.
Rehabilitation programme B comprised Qigong and work rehabilitation support in analogue with rehabilitation programme A.
Data collection and outcome measures
To evaluate psychological long-term effects at the 3-year follow-up, questionnaires were sent to the 107 patients who per-protocol completed the 1-year rehabilitation (58 patients in programme A and 49 patients in programme B). Sick leave data were obtained from registers at the Swedish Social Insurance Agency. Information on medication was received from questionnaires and complemented by telephone interviews when needed. Patients who did not answer the questionnaire at the 3-year follow-up (9 patients in rehabilitation programme A and 28 patients in rehabilitation programme B) were first contacted by post to give their permission to be contacted by telephone later and interviewed about their medication usage. Six patients (1 from group A, 5 from group B) declined to be contacted, and 4 patients (1 from group A, 3 from group B) could not be reached. In total, 27 patients were contacted by telephone. Sex, age, education, marital status, children at home, physical activity and exercise were registered at the 3-year follow-up for both groups by questionnaires.
Psychological measures
Variables of burnout and self-rated stress behaviour were assessed 6 times; at baseline, after 6 months, at the end of the 1-year rehabilitation, and at follow-ups performed at 6-months, 12-months and 3-years after the 1-year rehabilitation. Burnout was measured using the SMBQ (19–21). The SMBQ contains 22 items and each item was rated on a 7-point scale graded 1–7. An overall index was computed as the mean of all items, where a higher score indicated a higher level of burnout. A mean score of 4.0 or more on the SMBQ has been used previously (24) to classify possible burnout cases. Stress behaviours and reactions in everyday life were measured by the self-rated questionnaire Everyday Life Stress Scale (ELSS) (25). The ELSS contains 20 statements and each statement is rated on a 4-point scale. A total summary score (0–60 points) was calculated, where a higher score indicates more self-rated stress behaviours. At the 3-year follow-up the patients estimated occurrence of anxiety and depression with the Hospital Anxiety and Depression Scale (HAD). The subscales each consist of 7 items, and the composite total score (0–21 points) was calculated where scores lower than 7 are classified as “non-cases”, scores 8–10 as “possible cases”, and scores higher than 11 as “cases” (26).
At the 3-year follow-up, a question was included on subjective experience of recovery after the patients’ burnout, estimated on a 7-point scale, where one corresponded to being not recovered, and 7 to being fully recovered. Moreover, there were questions on rest and recovery from work to be answered by patients who were no longer on full-time sick leave. Rest and recovery from work were assessed with 8 items describing perceptions of recovery from work (e.g. rested in the morning, after a weekend, after a medium-term absence, and after a holiday) and fatigue at work (e.g. energy and tiredness during work, and mental and physical fatigue after work). The patients estimated their level of recovery and fatigue on a 5-point scale, with “never” and “very often” as end-points. Each item was dichotomized into recovered (response alternatives very often–quite often) and non-recovered (response alternatives sometimes–never) (27, 28). The patients also reported if they used any tools learned from the rehabilitation programme.
Sick leave
The patients’ sick leave levels were assessed 4 times; at baseline, at the end of the 1-year rehabilitation, and at 12-month and 3-year follow-ups after the 1-year rehabilitation. Sick leave included sickness benefit, activity and sickness compensation, as well as rehabilitation compensation. The information was collected from registers at the Swedish Social Insurance Agency. In total, 107 patients completed the 1-year rehabilitation. Out of these, consent to collect information was provided by 106 patients.
Medication
Medication use for depression and sleep disturbances were self-assessed in the questionnaires at baseline, at the end of the 1-year rehabilitation, as well as at 12-month and the 3-year follow-ups. The patients specified what kind of medication they used.
Statistical analysis
Statistical analyses were performed in SPSS version 18.0 (SPSS Inc. Chicago, IL, USA) and alpha level was set to < 0.05. All analyses were based on a per-protocol analysis, which included all patients who completed the 1-year rehabilitation. Analyses of dropouts and variables at the 3-year follow-up were made by using t-tests for continuous data and Pearson’s χ2 tests for categorical variables. Repeated measures analyses of variance with time as a within-subject variable and group as between-subject variable were used to assess changes over time in burnout and stress behaviour. If the sphericity assumption was not met, the Huynh-Feldt correction was used. To assess changes over time in the use of medication a logistic regression model was used. The method of generalized estimating equation was used to adjust for correlations within subjects over time. An imputation procedure was used to adjust for missing responses in single items in variables of burnout, stress behaviour, anxiety and depression. Missing responses were replaced with the median response for the group; this occurred in 0.2–0.6% of the items.
RESULTS
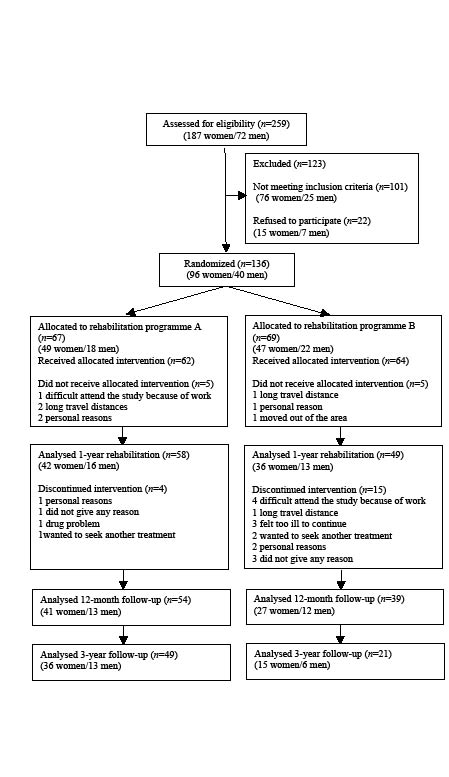
In this 3-year per-protocol follow-up of the REST-study, a total of 70 patients answered the questionnaires (response rate 65%); 49 patients in programme A (response rate 84%) and 21 patients in programme B (response rate 43%). Sick-leave data were obtained for 106 patients, and data on medication for 97 patients. A flow diagram of the patients who completed all questionnaires throughout the REST-study is presented in Fig. 1. There were no significant differences between the groups in socio-demographic measures (Table I). Neither were there any significant differences in sex, age and sick leave between the dropouts (in total 37 patients) who completed the 1-year rehabilitation and the patients who participated in the 3-year follow-up. However, in group’s specific analyses, there was a significant difference in sick leave in respondents from programme A compared with dropouts at the 3-year follow-up, since 18% (n = 9) of the respondents in programme A were on full-time sick leave, compared with 62% (n = 5) of the dropouts (p = 0.017). No significant difference was found in sick leave between respondents (19%) and dropouts (29%) in programme B (p = 0.517).
Fig. 1. Flowchart of patients who completed questionnaires in the rehabilitation for stress-related disease and burnout study.
Psychological measures
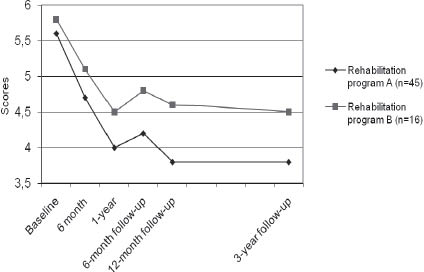
Both groups A and B improved significantly over time and reported lower levels of burnout [F(3.8, 223.6) = 24.6, p < 0.001] and stress behaviour [F(3.8, 182.5) = 17.8, p < 0.001], but there was no significant time by group interactions or group effects. Development of levels of burnout in both groups throughout the rehabilitation programme and follow-ups, including the long-term 3-year follow-up is shown in Fig. 2. At the 3-year follow-up there was a significant difference in mean SMBQ score between the groups. Fifty-one percent of the patients in programme A and 24% of the patients in programme B, reported a mean SMBQ score less than 4.0 (p = 0.035). No significant differences were found between the groups for levels of anxiety and depression (Table I).
Fig. 2. Mean values of burnout assessed with Shirom-Melamed Burnout Questionnaire at each follow-up point during the intervention period in patients who answered questionnaires at all assessments.
A significant difference was found between the groups at the 3-year follow-up for subjective experience of recovery from burnout, where patients in programme A reported being more recovered (p = 0.02). Patients in programme A also reported using significantly more tools learned from the rehabilitation programme (92%) compared with patients in programme B (33%) (p < 0.001). There were no significant differences between the groups with regard to recovery from work and fatigue at work in patients who were no longer on full-time sick leave (n = 52). Taking the groups together, 63% reported mental fatigue after work and 61% physical fatigue after work (Table I).
| Table I. Description of questionnaire data at 3-year follow-up for patients in rehabilitation programmes A and B |
| Variable | Rehabilitation programme A (n = 49) | Rehabilitation programme B (n = 21) | p-value |
| Sex, female/male, n | 36/13 | 15/6 | n.s. |
| Age, years, mean (SD) | 46 (7.0) | 45 (7.8) | n.s. |
| Education, n (%) Primary/secondary school University | 21 (43) 28 (57) | 13 (62) 8 (38) | n.s. |
| Marital status, n (%) Married/co-habited | 37 (76) | 17 (81) | n.s. |
| Children, n (%) Children at home | 30 (61) | 13 (62) | n.s. |
| Physical activity, n (%) < 30 min/day ≥ 30 min/day | 24 (49) 25 (51) | 11 (52) 10 (48) | n.s. |
| Physical exercise, n (%) ≤ 2 h/week > 2 h/week | 44 (92) 4 (8) | 18 (90) 2 (10) | n.s. |
| Shirom-Melamed Burnout Questionnaire, (max 7) mean (SD) | 3.8 (1.2) | 4.5 (1.2) | 0.050 |
| Stress Behaviour, (max 60) means (SD) | 19.3 (7.7) | 23.4 (13.2) | n.s. |
| HAD anxiety, (max 21) mean (SD) | 7.0 (4.0) | 8.5 (5.7) | n.s. |
| HAD depression, (max 21) mean (SD) | 5.3 (3.5) | 5.9 (4.5) | n.s. |
| Recovery from burnout, (max 7) mean (SD) | 4.7 (1.6) | 3.8 (1.8) | 0.020 |
| Use of functional tools, mean (SD) | 44 (92%) | 7 (33%) | < 0.001 |
| Non-recovered from work, n (%)a In the morning After a weekend After medium-term absence After vacation | 24 (65) 15 (40) 11 (30) 9 (25) | 9 (60) 8 (53) 7 (47) 4 (27) | n.s. |
| Fatigued at work, n (%)a Lack of energy during work Tired during work Mental fatigue after work Physical fatigue after work | 24 (65) 27 (73) 32 (86) 29 (78) | 9 (60) 13 (87) 12 (80) 14 (93) | n.s. |
| aData on non-recovered and fatigue at work are only from patients who were no longer on full-time sick leave (rehabilitation programme A, n = 37, and rehabilitation programme B, n = 15). SD: standard deviation; max.: maximum; HAD: Hospital Anxiety and Depression scale: score ≤ 7 = ”non-cases”; score 8–10 = ”possible cases”; score ≥ 11 = ”cases”. |
Sick leave
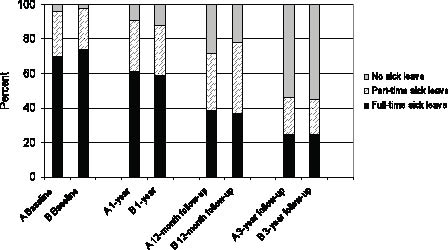
No significant differences in sick leave levels were found between the patients in programme A and B over the follow-up period of 4 years. Both groups improved over time with decreased sick leave levels, whereas 75% in both groups had part-time or no sick leave at the 3-year follow-up, compared with approximately 30% at baseline (p < 0.001; Fig. 3).
Fig. 3. Full-time, part-time or no sick leave for patients in rehabilitation programmes A (n = 57) and B (n = 49) at baseline, 1-year rehabilitation, 12-month and 3-year follow-up. Data collected from registers at the Swedish Social Insurance Agency.
Medication
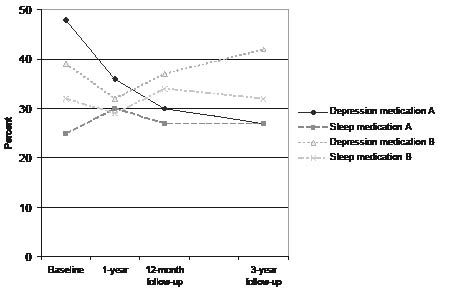
There was a significant difference in use of medication for depression between rehabilitation programmes A and B over time (χ2(3) = 15.0, p-value = 0.002; Fig. 4). At the 3-year follow-up, 27% of patients in programme A used medication for depression, compared with 42% of patients in programme B. No significant difference was found between the groups over time in the use of medication for sleep disturbances.
Fig. 4. Medication for depression and sleep problems for patients in rehabilitation programmes A (n = 56) and B (n = 41) during the intervention period and follow-ups.
DISCUSSION
In this 3-year follow-up of a randomized controlled study, the aim was to evaluate the long-term effects of two rehabilitation programmes for patients on long-term sick leave due to burnout. The aim was to study only per-protocol data, i.e. to include only patients who fulfilled the 1-year rehabilitation. Intention-to-treat analyses were performed in a previous publication of the REST-study (13). However, results from an intention-to treat analysis would be very uncertain and difficult to interpret in a long-term follow-up, such as the present one, which was the reason it was excluded.
Three years after the intervention, patients in programme A reported being significantly more recovered from their burnout, and a majority reported a burnout level below the cut-off for burnout cases. The results also showed a significant reduction in use of medication over time for depression in programme A compared with programme B. Moreover, patients in programme A reported using significantly more tools learned from CBR and Qigong in their daily lives compared with patients in programme B. For both groups, sick leave rates had decreased. However, levels of burnout and stress behaviour were at approximately the same levels at the 3-year follow-up as at the 12-month follow-up. Prognoses are troublesome for many patients with severe long-term burnout, regardless of the type of intervention. We also found that a large proportion of the patients who were no longer on full-time sick leave, and in a majority of cases were back in work, reported a high degree of fatigue at work and also regularly felt non-recovered from work.
An interesting finding in this study was the significant reduction in use of medication for depression for patients in programme A and their perception of being more recovered from their burnout. One cause could be that patients in programme A used significantly more tools learned from the rehabilitation programme consisting of both CBR and Qigong. Eighteen patients from the REST-study were earlier interviewed about their experiences of the rehabilitation programme (16). That study showed that patients in programme A used cognitive tools to gain insight, to change and to break old behavioural patterns. Patients in programme B instead used physical and psychological experiences from body movements as tools for recovery (16). However, the tools learned in group B may not have been as successful or used to the same extent as the tools learned by group A, which may be indicated by the fact that patients in group B used more anti-depressants. It is important to note that it may take time for patients to implement tools learned from CBR, to find new coping behaviours and to show the effects of a cognitively oriented programme. Therefore, effects from a rehabilitation programme may be evident a few years after completion. A reduction in medication is beneficial for both the patients and society, since side-effects and costs are reduced.
Reduction in sick leave levels in this study could be regarded as return to work for the majority of participants (in a few cases a reduction in sick leave could mean a loss of sickness benefit, unemployment, studying or taking parental leave. All patients at baseline had been unable to be gainfully employed or engaged in other full-time activities due to sickness for at least 3 months prior to inclusion). In the present study we found that 75% of patients at the 3-year follow-up had returned to work to some extent; approximately 45% were on part-time or full-time sick leave, whereas approximately 55% had no sick leave. There are few studies with such long follow-up period as this. Therefore, it is difficult to compare the long-term results of this rehabilitation programme with that of others. However, Grossi et al. (18) showed, in a study on stress management intervention with a follow-up period of 5 years, that 40% of the women under study returned to work to some extent and approximately 60% remained on sick leave or sickness benefits. Compared with that study, a larger proportion of the patients returned to work in the present study. One reason could be that patients in our study had a shorter period of sick leave before the intervention (approximately 1 year compared with 1.8 years). Previous research has shown that treatment of patients with shorter periods of sick leave gives more favourable results (8, 10, 15). Thus it seems important to find these patients with stress-related disease early on in the disease process.
In a prospective, controlled study (29) an intervention with a convergence dialogue meeting (CMD) between the patient and the supervisor was evaluated. This study aimed at finding solutions to facilitate return to work for burnout patients on sick leave. The study showed favourable results in return to work for the CMD group. One and a half years after the start of intervention, 89% of the patients in the CMD group had returned to work to some extent compared with 73% in the control group. In that study, only patients with a short period of sick leave (2–6 months) were included and patients with sick leave related to their private lives were excluded. The design was not randomized and controls were recruited from patients who declined to participate in the intervention, which implies that there may have been differences between the groups in motivation for return to work or in needs of interventions at the workplace. Compared with the study by Karlson et al (29), our study shows that, despite longer sick leave and stressors both from private life and work, it is possible for most burnout patients to return to work after a long period of sick leave. A subset of the REST study group (117 patients) was investigated earlier (30) on the impact of psychosocial working conditions and coping strategies at work on change in sick leave. Patients who perceived low control at work and who used covert coping towards supervisors and work colleagues had a higher risk of not reducing their sick leave 12-months after completed rehabilitation (30). To increase the likelihood of return to work for patients with burnout, interventions should probably focus on support in vocational rehabilitation and on establishing a more flexible and communicative work environment.
Another important factor for return to work is motivation. van Oostrom et al. (15) found that employees with distress who intended to return to work despite symptoms returned to work earlier. van Oostrom et al. (15) also discussed that employees without this intention need a different treatment approach aiming to change motivation regarding return to work with sustained symptoms. A multidisciplinary rehabilitation programme for patients on long-term sick leave showed that return to work was predicted by improved work motivation (31). In the present study, the patients’ motivation to return to work was not assessed. However, this would seem important in clinical rehabilitation of burnout patients.
We found that the patients who had reduced their sick leave and returned to work at the 3-year follow-up often had difficulty regarding fatigue and not being recovered from work. To enable comparison of the patients in the REST study with a Swedish working population we dichotomized the question of mental fatigue after work according to the procedures of Eek et al. (28). In total, 27% of the working population reported mental fatigue after work (28) compared with 63% of the rehabilitated burnout patients in this study. Despite improvements in psychological variables and reduced sick leave, a high proportion of the patients still reported fatigue and being non-recovered from work. A continued impaired cognitive function could be one reason for these findings (32, 33). Previously, rehabilitation for patients with burnout has not focused much on effects of cognitive problems at work. This should be addressed in the future.
In studies with long-term follow-ups there is a considerable problem with increasing numbers of dropouts. This is also a limitation of the present study, and especially in the evaluation of psychological data based on questionnaires. A reduction in the number of evaluated patients decreases the power to detect effects. Another problem is that dropouts may differ from respondents in important respects. Dropouts are often claimed to have a worse prognosis than the respondents, but it is also possible that they recover well and therefore are not interested in long-term follow-ups. Since it is considered ethically inappropriate to enquire about the exact reasons for dropout, this has not been done in the present study. However, it is important to consider that, in this follow-up study, a larger proportion of dropouts in programme A were on full-time sick leave at the 3-year follow-up compared with respondents, which may have affected our results.
The rehabilitation programme evaluated in our study consisted of CBR, and not strict CBT. It was developed by psychologists to suit patients with burnout, and was implemented by specially trained physiotherapists. These circumstances; the method chosen (CBR and not CBT) and the competence of the group leaders may have affected the results. There are, to our knowledge, few randomized controlled studies evaluating the effects of CBT in patients on sick leave because of burnout (10, 12), and the effects on psychological parameters have mostly been insignificant so far. In work-related burnout, in particular, the most efficient methods to improve psychological health and increase work resumption probably are work-oriented measures (10, 29). Interventions should also aim at improving individual strategies and coping at work (30).
In conclusion, in this study a multimodal rehabilitation group programme including CBR and Qigong (programme A) showed favourable long-term effects in comparison with Qigong alone (programme B). At the 3-year follow-up after the end of intervention, patients in programme A reported being significantly more recovered from burnout, had lower levels of burnout, had reduced their use of medication for depression and reported using more tools learned from the CBR. It is difficult to determine which components in the rehabilitation programme are the most effective and important. Qigong training, which was evaluated in a previous study, showed no additional effect beyond basic care (24). The CBR programme could be shortened in order to streamline and make the rehabilitation more effective. On the other hand, clinical experience shows that new coping behaviours to reduce stress and increase well-being usually take a long time to develop and integrate in ordinary life. In a qualitative part of the REST-study it was found that the support given by the group in programme A was considered very important and beneficial for recovery (16). In order to further facilitate return to work for patients with burnout, improvements in vocational rehabilitation are to be recommended. Thus, multimodal rehabilitation should start early in the disease process and should focus even more on work support, work motivation and cognitive improvements, preferably in groups.
REFERENCES