Sofia Brorsson, PhD1, Anna Nilsdotter, PhD2, Eja Pedersen, PhD1, Ann Bremander, PhD1,3 and Carina Thorstensson, PhD3
From the 1School of Business and Engineering, Department of Exercise Physiology, Biomechanics and Health, Halmstad University, 2Department of Research and Education, Halmstad County Hospital, Halmstad and 3Research and Development Centre, Spenshult Hospital for Rheumatic Diseases, Oskarstrom, Sweden
OBJECTIVE: Balance between flexor and extensor muscle activity is essential for optimal function. The purpose of this pilot study was to compare the relationship between maximum finger flexion force and maximum finger extension force in women with rheumatoid arthritis and healthy women.
METHODS: Twenty healthy women (median age 61 years) and 20 women with rheumatoid arthritis (median age 59.5 years, median disease duration 16.5 years) were included in the study. Finger extension force was measured with an electronic device, EX-it, and finger flexion force using Grippit. The Grip Ability Test and the score from the patient-reported outcome Disability Arm Shoulder and Hand were used to evaluate activity limitations.
RESULTS: Patients with rheumatoid arthritis showed significantly decreased hand function compared with healthy controls. A correlation was found between extension force and flexion force in the healthy group (r = 0.65, p = 0.002), but not in the rheumatoid arthritis group (r = 0.25, p = 0.289).
CONCLUSION: Impaired hand function appears to influence the relationship between maximum finger flexion and extension force. This study showed a difference in the relationship between maximum finger flexion and extension force in healthy controls and those with rheumatoid arthritis.
Key words: hand function; hand strength; rheumatoid arthritis; muscle ratio; flexion force; extension force.
J Rehabil Med 2012; 44: 605–608
Correspondence address: Sofia Brorsson, Halmstad University, School of Business and Engineering, PO Box 823, SE-301 18 Halmstad, Sweden. E-mail: sofia.brorsson@hh.se
Submitted September 28, 2011; accepted February 13, 2012
INTRODUCTION
Hand grip strength has been shown to be a good indicator of general muscle strength (1). Moreover, hand grip strength can be used to predict multiple outcomes, such as changes in activities of daily living (ADL), disability, mortality and general upper extremity strength (2–4). Hand and finger extensor muscles are important stabilizers during flexion force production and controlled grip strength (5). A balance between flexor and extensor muscle activity is essential for optimal function, as has been shown previously for lower extremity, trunk and shoulder function (6–11). Information on the relationship between finger extensor and finger flexor muscle force is lacking, both for patients with impaired hand function and for healthy subjects.
Patients with rheumatoid arthritis (RA) are frequently affected by pain, weakness and restricted mobility. It has been estimated that 80–90% of patients have reduced hand function (12). Impaired grip ability in RA can be due to deformities such as ulnar deviation with dislocation or subluxation, reduced strength in the flexor muscles, or dysfunctional extensor muscles, leading to an inability to open the hand, thus affecting the ability to perform ADL (13–15).
The purpose of this study was to compare the relationship between maximum finger flexor and finger extensor force in healthy women and women with impaired hand function.
SUBJECTS AND METHODS
Subjects
The RA group comprised 20 female patients (diagnosis using the 1987 American College of Rheumatology (ACR) criteria (16)) visiting the specialist outpatient clinic at Spenshult Rheumatic Hospital during January 2005. The inclusion criteria for the patients with RA were: disease duration of at least 1 year and full active finger flexion and extension ability. Patients who fulfilled the inclusion criteria were invited to participate in the study. The median age of the RA group was 59.5 years (range 33–70 years) and the median disease duration 16.5 years (range 3–38 years). The median age of the healthy group was 61.0 years (range 36–73 years). The healthy control group, chosen to match the RA group regarding sex and age, were recruited via posters at Halmstad University and in Halland region, Sweden. The exclusion criteria for the healthy subjects were: inflammatory or muscle disease or previous hand or arm injuries (17). The study was approved by the ethics committee of Lund University. All procedures complied with the Declaration of Helsinki.
Measurements of body function and activity performance
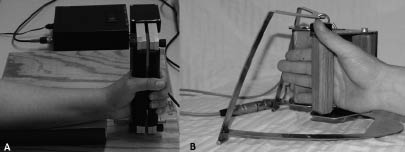
The measurements of body function were finger flexion and finger extension forces. Finger flexion and finger extension forces in Newton (N) were measured by the newly developed device called EX-it (17) and the Grippit instrument, respectively (Detektor AB, Göteborg, Sweden) (18). Both devices have shown good validity and reliability (18, 19). The procedure for the measurements was standardized in terms of sitting position, instructions and encouragement (Fig. 1) (20, 21), and measurements were carried out by one assessor only (SB).
Fig. 1. (A) Grip force was measured with the Grippit device. (B) Finger extension force was measured using the EX-it. All participants were seated in an upright position, the forearm resting on an arm support and the hand was placed in the Grippit/EX-it.
Hand activity performance was evaluated using the Grip Ability Test (GAT), and the patient-reported outcome measure, Disabilities of Arm, Shoulder and Hand (DASH) (15). GAT measures the degree of limitation of ADL and is designed for patients with RA. GAT is performed according to a standardized protocol, and is based on 3 items chosen to represent different hand grips: (i) put a flexigrip stocking on the non-dominant hand, (ii) put a paper clip on an envelope; and (iii) pour water from a jug. The longer the time required by the patient to carry out the tasks, the higher the GAT value, scoring from 4 to 276, a higher score corresponds to lower hand function (22). The DASH measure has two components: the disability/symptom section (30 items) and the optional high-performance sport/music or work section (4 items) (http://www.dash.iwh.on.ca/score.htm). In this study, the Swedish version of the disability/symptom section was used (15). The items in DASH are rated from 1 (no difficulty) to 5 (unable to perform). A score is calculated from 0 to 100, where a higher score indicates greater disability (15).
Statistics
SPSS version 18.0 was used in the statistical analysis. As data were not normally distributed, non-parametric methods were used for the statistical analyses. Associations between two variables were analysed with Spearman’s rank correlation test (r) and linear regression analysis was conducted on the statistically significant factors. A p-value of less than 0.05 (two-tailed test) was considered to indicate statistical significance.
RESULTS
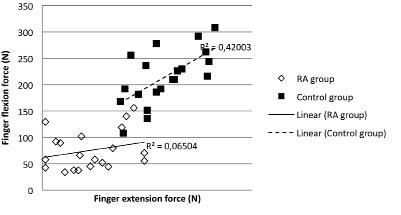
The results of the hand function measures are presented in Table I. A statistically significant correlation was found between finger extension and flexion force in the healthy group (r = 0.648, p = 0.002). No such correlation was found in the RA group (r = 0.250, p = 0.289) (Fig. 2), neither was any correlation found when assuming non-linear correlations (data not shown).
Fig. 2. Correlation between finger extension and flexion force in patients with rheumatoid arthritis compared with a healthy control group.
The RA group showed lower hand strength than the healthy group in both the extension force and the flexion force, as well as decreased DASH and GAT (Table I).
| Table I. Hand function and activity performance |
| Outcome measure | RA group (n = 20)Median (95% CI) | Healthy group (n = 20)Median (95% CI) |
| Extension force (N) | 14.5 (10.7–21.0) | 38.7 (36.0–45.6) |
| Flexion force (N) | 62.0 (58.2–92.7) | 213 (189.9–238.4) |
| DASH score (0–100) | 38.8 (29.5–44.3) | 3.3 (2.6–9.6) |
| GAT value (4–276) | 20.4 (19.2–27.4) | 13.4 (12.4–14.5) |
| DASH: Disability Arm Shoulder and Hand (a higher score indicates greater disability); GAT: Grip Ability Test (a higher score corresponds to lower hand function); CI: confidence interval. |
DISCUSSION
It has previously been reported that women and men with RA have decreased muscle strength compared with healthy subjects (18, 23, 24). Impaired hand function has been associated with an imbalance between maximum finger flexion and extension force, which could lead to reduced hand function in ADL. Snijders et al. (11) demonstrated that the wrist extensor muscles must be activated to counteract the wrist flexion force. Using a biomechanical model, they also showed that grasping and pinching cause a flexing moment in the wrist joint. To be able to avoid flexion of the joint there must be equilibrium of moments, which is attained by activating the extensor muscles.
We found a pronounced decrease in finger extension force in the RA group compared with the healthy group. Goossens et al. (25) reported that patients with RA have identified the index finger, middle finger and the metacarpophalangeal joints as the most important contributors to functional ADL. Earlier studies have also reported that patients with RA have weaker grip, pinch and tripod force than healthy controls (18, 23, 26–28). It has been suggested that force assessment could be used as an accurate indicator of upper limb ability, and that grip force (i.e. flexion and pinch force) should be included in the evaluation and follow-up of patients with RA in hand rehabilitation (27–30). It has also been suggested that the decrease in force could be the direct effect of the disease on muscle function, disuse or impaired neuromuscular transmission, medication, pain or deformities such as ulnar deviation (28).
Force measurement provides a quick and easy means of determining hand impairment and function, and is useful when evaluating hand status. Earlier studies have focused on finger flexion force. Devices for assessing finger extension force have not previously been available. EX-it is a valid and reliable tool that can be used to asses finger extension (19, 23), and can be used in combination with patient-reported outcome measures and tests of functional performance to provide more information on hand function. Measurements of finger extension force in patients with RA may elucidate the role of extensor muscle weakness in the development of flexion deformities in the hand. This study has contributed to current knowledge by showing a difference in the relationship between maximum finger flexion and extension force.
The use of medication and other concomitant treatment was not included in this study. Neither was detailed information obtained about hand deformities in the patients with RA, but all patients in the study were able to fully flex and extend their fingers. The range of disease duration in the RA group was wide (2–40 years). The results of this pilot study should be confirmed in larger studies, and in other groups of patients with hand dysfunction. In addition, the relationship between flexion and extension force needs to be explored in men with and without hand dysfunction or RA.
Hand training may have the potential to normalize the relationship between finger flexor and finger extensor forces in patients with RA. Continuous exercise is recommended to prevent loss of muscle strength and to improve the performance of ADL (31–33). Therefore, further studies are required on the involvement of the finger flexor and extensor muscles in ADL. In the longer term, this might lead to better rehabilitation of hand function in patients with RA.
ACKNOWLEDGEMENTS
The authors would like to thank the patients at Spenshult Rheumatic Hospital and the healthy subjects who participated in the study. Funding for this study was provided by The Crafoord Foundation and Halmstad University.
REFERENCES