Anthony B. Ward, BSc, FRCPEd, FRCP1, Christoph Gutenbrunner, MD, PhD2, Alessandro Giustini, MD3, Alain Delarque, MD4, Veronika Fialka-Moser, MD, PhD5, Carlotte Kiekens, MD, PhD6, Mihai Berteanu, MD, PhD7 and Nicolas Christodoulou, MD, PhD8
From the 1Past-President, UEMS Section of PRM, North Staffordshire Rehabilitation Medicine, Haywood Hospital, Stoke on Trent, United Kingdom, 2Past-President, Professional Practice Committee, UEMS Section of PRM, Department for Rehabilitation Medicine, Medizin Hochschule, Hannover, Germany, 3Past-President, European Society of PRM, Rehabilitation Hospital San Pancrazio - KosGroup Santo, Arco (Trento), Italy, 4Past-President, UEMS Section of PRM, Department de Médecine Physique et de Réadaptation, CHU Timone, Marseille, France, 5Past-President, UEMS Section of PRM, Universitäts Klinik für Physikalische Medizin und Rehabilitation, Allgemeines Krankenhaus der Stadt Wien, Vienna, Austria, 6Member, Professional Practice Committee, UEMS Section of PRM, Physical and Rehabilitation Medicine, UZ Leuven, Campus Pellenberg, Pellenberg, Belgium, 7President, Professional Practice Committee, UEMS Section of PRM, Department of Physical & Rehabilitation Medicine, University Hospital Elias, Bucharest, Romania and 8President, UEMS Section of PRM, European University Cyprus, School of Sciences, Nicosia, Cyprus
Physical & Rehabilitation Medicine (PRM) programmes in post-acute settings cover interventions for the rehabilitation of people with a variety of disabling health conditions. The setting of the intervention is more important than the timing and these programmes can be carried out in a variety of facilities. This paper describes the role of PRM services and of PRM specialists in delivering rehabilitation programmes to people, who have initially been admitted to hospital. The emphasis is on improving patients’ activities and addressing participation issues. PRM programmes in post-acute settings provide a range of treatments and have a major influence in the long-term on the pace and extent of return of function and recovery from ill-health. This paper will define the meaning of post-acute settings and will describe the patient’s journey through the post-acute setting. In particular, it addresses the standards of care across Europe that patients should expect.
This paper also examines the general principles of funding such programmes within the context of different health care systems across Europe. Coordinated care improves outcomes and economic profiles for both payers and providers of services.
This paper describes the value of PRM interventions and PRM specialist-led teams in promoting better outcomes for people with disabilities with complex needs.
Key words: rehabilitation; post acute settings; physical & rehabilitation medicine programmes; clinical pathways.
J Rehabil Med 2012; 44: 289–298
Correspondence address: Professor Anthony B Ward, North Staffordshire Rehabilitation Centre, Haywood Hospital, High Lane, Burslem, Stoke on Trent, ST6 7AG, United Kingdom. E-mail: anthony@bward2.freeserve.co.uk
Submitted November 7, 2011; accepted February 21, 2012
Introduction
This paper describes a person’s rehabilitation experience in Physical & Rehabilitation Medicine (PRM) programmes following illness or injury. Dealing with patients during the early phase following admission to hospital has already been described (1) and this document covers a range of PRM programmes in post-acute settings. This is in the context of great changes in health care both at European and at national levels. It is thus important to describe what PRM is, what it can offer, how it can best provide its services and expertise and what standards of service delivery and specialist training should be demanded from the public. The scope of services have been taken from several national documents, such as the Royal College of Physicians of London Working Party Report, “Rehabilitation Medicine, 2011 and Beyond” (2). This will be updated in data obtained from the Italian National Plan for Rehabilitation, 2011 (3). It should also be stated that there is a good body of evidence in the literature to show the effectiveness and cost-efficiency of coordinated multidisciplinary rehabilitation, in which PRM specialists work. These are described in the Royal College of Physicians report (2) and the raw evidence has not been duplicated for this paper.
PRM programmes in post-acute settings provide more than just a follow on from those in acute settings. They also set up systems for picking up the needs of people living in the community and have a variety of aims, which will be discussed below. This paper will describe the concepts of PRM interventions for a variety of health conditions within the context of the different national and regional health settings. It will also address the needs of a person with a disability resulting from an acquired health condition, so that he or she may respond to a PRM programme in post acute settings to assist in his or her rehabilitation. The context of the paper relates more the setting of the PRM programme and what goes into it rather than its input at a certain phase of a health condition. It also shows that PRM is a vibrant specialty, through which doctors can positively contribute to a person’s rehabilitation, but can also ensure higher quality care through specialist multi-professional interventions (3). The UEMS Section of PRM highlights that, within the challenges that face health services, people with disabilities have, through good standards of PRM care, a better chance, not only of survival, but also of an active participation in society. Its publications can be accessed through its website (www.euro-prm.org) (4–16). The purpose of this paper is to highlight the change in PRM services that are relevant for patients who are leaving acute hospitals earlier and are, as a result, more sick than before.
Definitions
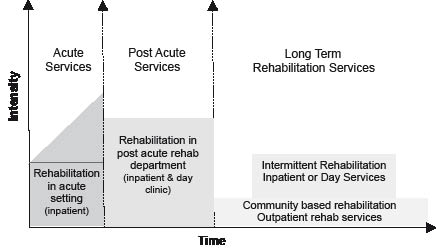
Using a systematic approach to PRM service delivery (4) (Fig. 1), one may see the relationship between disease (through ICD), function (through ICF), interventions (through services and health interventions) and the classification of health accounts in the post acute setting.
Fig. 1. Services of PRM within the framework of the WHO services matrix (6) (from Ref 6). Published from ref 6 with permission.
Post-acute PRM programmes are perhaps best classified according to the referral pattern of the patient. A common route of entry is through a patient’s transfer from an acute setting, such as a hospital. Rehabilitation in post-acute settings is not necessarily an inpatient activity, but most programmes start when patients are still in hospital. Patients are most commonly treated in stand-alone rehabilitation facilities or in ambulatory facilities in PRM departments. Both cover the same issues as many aspects of PRM in acute settings, but are different in both time and in situation, in which the whole range rehabilitation activities is covered from addressing impairments, promoting patients’ activities and facilitating their participation in society with the context of the personal and environmental factors (15).
Rehabilitation in post-acute settings is governed by both the setting and activity. The timing and intensity of treatment and the focus on the achievement of short-term goals are important, but should be included as part of the continuum of the rehabilitation process. It is not really governed by the location of physical setting, which can be various, but in the context of this paper, it is in a setting under the clinical governance of a PRM team. The definition of PRM programmes in post acute settings concerns activities that start when the patient is medically stable and no longer requires to be in an acute hospital. This is usually within the first month after a patient’s acute admission for illness or injury, but may be longer in very severely injured patients following acquired brain injury (2). The patient’s journey after a variable time would then lead on a longer term PRM programme, if required, which essentially cover activities taking place in the community. The patients’ needs and the availability of treatment facilities and professional activity should control the intensity of the PRM programmes (16–19). The establishment of a specialised rehabilitation plan is thus crucial.
Patients enter a programme of goal-oriented multi-professional rehabilitation under the responsibility of a PRM specialist, which can result in greater gains through the interaction of the professionals’ involved than that of the sum of the individual components (10, 20). A core team exists (see below), with whom the PRM specialist works in close proximity and its composition of professionals will depend upon the activities of the service (2). There is also a more extended team of professionals, whose input is invited for specific aspects of the rehabilitation plan. These may include among others, clinical engineers, wheelchair technicians, dietitians, etc.
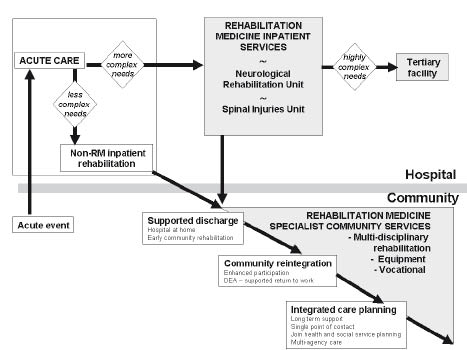
Point of entry in to post-acute Physical & Rehabilitation Medicine programmes
The point of entry into an appropriate post-acute PRM programme depends not only on the location of the PRM service and its relationship to acute facilities, but also on its clinical activities (see below). A number of models and options were described in the paper on PRM in acute settings (1) and these are relevant to referrals from hospital inpatients. The majority of patients will have a period of inpatient treatment as part of their post acute PRM provision, but others, who are safe and able to return home, may be able to participate in this in ambulatory or community settings (21).
Why are specialist Physical & Rehabilitation Medicine programmes required?
It is recognised that people with more complex needs need specialist services (22). Specialist rehabilitation services should be planned and delivered through co-ordinated networks to work both in hospital and the community to support local rehabilitation and care support teams. For example, the British Society of Rehabilitation Medicine (BSRM) standards (23,24) recommend that there should be a local specialist rehabilitation service led by a minimum of 6.0 whole time equivalents (WTE) trained specialists in PRM per million population, including 3.6 WTE for district specialist inpatient rehabilitation services and their associated out-reach activities and 2.4 WTE for specialist community rehabilitation services.
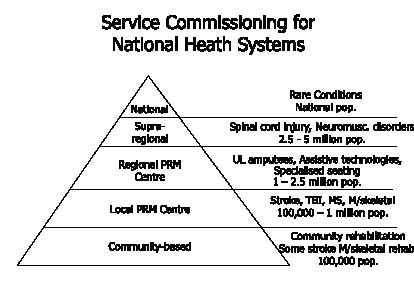
A small number of people have very complex needs, and require a higher level of highly specialised PRM care (e.g. post-acute spinal cord injury patients or those with neuropsychiatric problems following brain injury). A larger number of people also require specialist rehabilitation in similar settings, but in less specialised units for conditions, such as some musculoskeletal trauma and problems. Very highly trained rehabilitation professionals are actually in short supply and it is not feasible or economical to duplicate these high cost/low volume services in every locality (2). Therefore, a ‘hub and spoke’ arrangement can exist, whereby patients are placed in the appropriate service for their needs over a defined geographical area. This requires the cooperation of health payers because the eventual pathway into longer term rehabilitation will require comprehensive arrangements to ensure that people with disabilities do not lose the gains they have made in rehabilitation, once they move out of the post-acute setting. In addition, the best way to define costs is by providing costing data on a day-by-day per person basis using the agreed measures of complexity and outcome (25, 26). Fig. 2 highlights the complexity of conditions and the relevant recommended provision for PRM services. The cost of PRM programmes invites a consideration of healthcare tariffs and these are being developed for specialist neurological rehabilitation services (26). The rationale and development of a case-mix model is based on the fact that patients with complex needs incur higher treatment costs and that fair payment should be weighted in proportion to costs of providing that treatment. Case complexity can be measured by the Rehabilitation Complexity Scale and five bands have been described (26, 27).
Fig. 2. Service Commissioning for PRM services (2, 26).
Tertiary ‘specialised’ rehabilitation services are high cost/low volume services, which provide for people with highly complex rehabilitation needs that are beyond the scope of their local and district specialist services. These are normally provided in co-ordinated service networks through collaborative (specialised) commissioning arrangements. Local specialist PRM services are led or supported by PRM specialist, working both in hospital and the community setting. The specialist multi-professional rehabilitation team provides advice and support for local general rehabilitation teams. In addition, some local services specialise in certain conditions, e.g. motor neurone disease and provide highly complex specialist expertise and management. These anomalies demonstrate a diverse pattern of rehabilitation service development with many interesting and expert community services developing. Providing the formula for funding to support these developments requires a dialogue between the PRM specialists and the payers/commissioners, but many cases are high cost and inevitably require longer lengths of stay. It is thus necessary to make the argument in terms of cost efficiency. In the UK, the argument has been highly persuasive in achieving funding of these services, as investing in rehabilitation is offset many times by long-term savings in the cost of care (28, 29).
Example of PRM practice:
Following a bomb blast a 19-year-old soldier receives a right above-knee amputation. PRM assessment identifies impairments such as limb loss, pain, a previously unsuspected moderate brain injury, unilateral deafness and post-traumatic stress; limitations in activities such as walking, sleeping, concentrating; and restrictions in participation including fulfilment of military and family roles. Outcome is enhanced by alterations in the environment beginning with the provision of a prosthesis, specialist treatment for the brain injury and stress-related symptoms, and should eventually include adjustments made for the process of re-employment with access to vocational rehabilitation services. Continued attention to his social environment, including his family life and relationships with others in his unit), and to the bereavement aspects of his situation is also a crucial aspect of his rehabilitation.
Eligibility, Admission and Discharge Criteria (24–26, 30)
Admission
PRM specialists admit patients to these specialised programmes when they require the activity of a trained specialist multi-professional team. Comprehensive ICF core sets for patients entering PRM programmes in post-acute settings have been described and validated (31–34). The entry criteria are governed by (i) the facilities of the centre, (ii) the competences, skills and interests of the professionals within the team and by (iii) the local health care needs. They thus vary from centre to centre, but essentially are as follows:
Patients who:
• ideally are medically stable and are fit to participate in a PRM programme;
• will benefit from the activities of a multidisciplinary PRM team and require, for inpatient programmes, the input of more than two professionals within the team;
• have defined goals for their rehabilitation; and
• understand and are motivated to participate in a goal-oriented rehabilitation programme or have the potential to do so.
It is difficult to describe exclusion criteria in this paper, as each centre needs to define their own depending on their assets and on the availability of alternative services. They become clear, if there are robust criteria for accepting patients to a PRM programme and a centre needs to inform referring clinicians of what other services are available and where. It is possible that some people are not yet ready to enter a programme in a post-acute setting and it is necessary for the PRM team to develop a system of reviewing these patients to identify their eligibility at a later date, e.g. a person in coma following a very severe brain injury, who may respond at a later date. Certain programmes are dedicated to particular pathologies, e.g. stroke, limb loss, etc., but they are also part of a global PRM approach to managing people with complex needs (2, 35).
Discharge
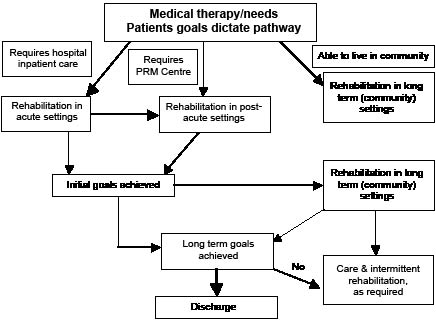
Moving out of PRM programmes in post-acute settings to those in longer term settings should be seen as a continuum. Where this involves a change from an inpatient setting to one in the community, discharge plans will create the further needs of the patient and a discharge process should be in place. As PRM programmes (no matter what the setting) involve goal setting, achieving the relevant goals for that part of the rehabilitation process will dictate where that is best carried out. Goals are negotiated with patient and their relatives and thus their agreement is an important part of finding the right setting to meet their needs. Fig. 3 highlights the clinical pathway for a patient going through the range of PRM settings.
Fig. 3. Rehabilitation pathway (5, 30).
Key roles and skills of the Physical and Rehabilitation Medicine Specialist
The core roles of PRM specialists include the diagnosis and medical management of conditions causing complex disability (2, 36, 37). These are given in Appendix I, but one of the PRM physician’s key contributions to the work of the multi-professional rehabilitation team is to provide a holistic description of the patient’s situation from both a medical and a non-medical point of view, thus helping individuals and families to identify abilities, resources and possibilities as well as illness, disability and problems.
Disabilities can almost always be made more severe by omissions or ill-considered actions, and prevention is a fundamental principle of PRM. In many situations, a PRM specialist can make a vital contribution through anticipation and prevention of physical, psychological and social complications, based on knowledge of a condition’s natural history and prognosis. The range and value of 9 aspects of a PRM specialist in the team is highlighted in Appendix I. Examples of the tasks and skills entailed are also given (2, 36, 37). The addition of a PRM specialist may be seen as expensive, but his or her training and contribution to the treatment programme do confer to teams a range of skills that is unique to them among other PRM service team members. In addition to medical investigation and treatment, some of the important contributions that the PRM specialist can bring to the team are (2):
a) Confirmation or refutation of diagnosis (the longer time scale of rehabilitation afford greater opportunity for observation over time and new diagnoses often become apparent over that period).
b) Prognostication – the PRM specialist’s knowledge of pathology through his/her training is invariably greater than that found among nursing and other health professional staff. The PRM specialist has thus a greater understanding of the expected course of a condition – especially in the context of progressive disease, cancers etc. This is critical for forward planning of the rehabilitation programme.
c) The PRM specialist is comprehensively trained in communication, whether this concerns policy planning at service level, leading a multi-professional team or giving information to patients and relatives, such as breaking bad news etc.
d) Leading on service development and the negotiation of funding for established and new treatment strategies.
e) Team leadership and the responsibility for the conduct of service activities.
The Scope of Physical and Rehabilitation Medicine Practice
Physical and Rehabilitation Medicine specialists apply their medical rehabilitation interventions as appropriate throughout all phases of the rehabilitation process. The medical conditions treated come into 4 groups; sudden onset conditions, intermittent conditions, progressive conditions and stable conditions (Table I) (22, 31). These present to specialists in PRM in post-acute settings, as they are determined by need rather than by diagnosis. People with longer term conditions experience changing needs and PRM makes a contribution when changing needs call for medical reassessment and co-ordinated rehabilitative responses.
| Table I. Range of conditions |
| Sudden onset conditions | E.g. brain or spinal cord injury, where a catastrophic onset is followed by a variable degree of recovery. |
| Intermittent conditions | E.g. relapsing remitting multiple sclerosis, where the condition itself may fluctuate, although the problem of unpredictability is ever-present. |
| Progressive conditions | Impairments and disability gradually increase over a timescale, which may vary from a few months (in the case of rapidly progressive conditions) to many years (e.g. in secondary progressive multiple sclerosis or Parkinson’s disease). |
| Stable conditions | E.g. cerebral palsy or post-polio, where the condition itself is often static, but the additional effects of degenerative and other changes may be superimposed over time, producing new disability and new rehabilitation needs. |
Relations/liaison with other services
One aspect of a PRM programme in a post-acute setting is the relationship with the services referring patients in and those who will continue the healthcare or rehabilitation process thereafter. It is thus important that specialists in PRM build up a network of cooperation with other medical disciplines, with whom they work, as well as therapists and nurses. This allows better working during the rehabilitation process, but developing close relationships with primary care teams of general practitioners and community therapists and nurses ensures that treatments can continue following discharge from the PRM centre and that patients and families can maintain their skill levels and activities. Table II highlights the interactions between members of the PRM team and other medical disciplines and services (2, 5, 21, 36–40).
| Table II. Admission and discharge liaison (21, 23) |
| Liaison | Medical specialists/ Professionals involved | Systems required |
| Referrals in | PRM specialist in acute setting Acute care physicians, (e.g. neurologist and others) Acute care surgeons (e.g. neuro and orthopaedic surgeons) Psychiatrists | Direct from PRM service in acute setting Establishment of referral team, e.g. rehabilitation coordinator, specialist nurse, PRM specialist (see similar system for rehabilitation specialist in acute settings) |
| Liaison out | Primary care team (general practitioner) care services, institutional care (nursing homes, etc.) Vocational and employment services Other health services | PRM services including Resettlement officer/service Occupational therapy, rehabilitation engineering, etc. PRM services including vocational and occupational therapists Depending on individual service facilities |
Clinical conditions served by Physical and Rehabilitation Medicine
The range of this widely based medical specialty is shown in Appendix II. Its practice depends on the facilities available and the expertise/background of the professionals involved in service delivery. Each UEMS member state also has different requirements and the specialty’s field of competence has been described (17). Appendix III give a brief overview of the areas of practice in PRM and some examples of conditions seen by PRM consultants.
Outcomes and measurement of the impact of Physical & Rehabilitation Medicine services
It is difficult to recommend the outcome criteria for PRM services or ideal measurements, as they will obviously be specific to the health care environment, to the activity of the provider unit and to the patients’ individual goals. Rehabilitation research is well advanced in the systematic recording of functional outcomes. Standard outcomes in post-acute settings are aligned to functional determinants, as described in the WHO’s International Classification of Functioning, Disability and Health (41). In trying to justify the higher cost specialist services, there is now a hierarchical dataset of 3 inter-related standardized global disability measures ranging from the Barthel Index of Activities of Daily Living (42) for the lower cost high volume services to the Functional Independence Measure (FIM) (43) and then on to FIM and FAM (Functional Assessment Measure) (44) for the higher cost inpatient specialist services associated with brain injury rehabilitation. Currently, there is work going on in several countries in using the Barthel Index as a common tool for all services, but adopting the other two to reflect the nature of greater intervention complexity. A basket of commonly approved measures has been created, from which individual services could chose the appropriate item for their particular service model or user group. It is not within the remit of this paper to go into outcome measures in great detail, but to mention the importance for defining individual rehabilitation goals for each patient. Goal attainment should be recorded for each patient and there are several ways of building this into an evaluation of outcome within the framework of collecting standardized measures as well. This has already been applied in the several countries for PRM programmes among people with neurological conditions, but can equally apply to other health conditions, given their specialist nature (45–49).
Costs of Physical & Rehabilitation Medicine services in post-acute settings
Costs differ according to the facilities provided, but the cost of the PRM team is the important feature in PRM programmes in post-acute settings. They are also difficult to equate over the different healthcare systems throughout Europe, but a recent UK cost analysis of specialist inpatient services for neurologically compromised patients showed that any expected variations in cost are largely due to differences in staff costs (50). Staff pay made up 66% of total costs and, therefore, a projection of 150% for total staff costs over those of standard inpatient services provides a reasonable estimate of the total costs of a unit. Children’s services were almost twice that (51). Why should payers/commissioners of health care pay for PRM programmes as opposed to non-specialist rehabilitation? There are several reasons, but the most important is that a PRM team treating people with complex needs due to a disabling health condition is the most efficient way of bringing together all the required services to allow better outcomes in terms of functional activity and participation in society (2). The costs of care for these people is great with overall mean first-year charges for spinal cord injured patients of US$523,089 and mean annual charges over the remainder of life were US$79,759 (2009 data) (52). Similar costs were reported in Belgium (53), but there is good evidence that coordinated PRM programmes can substantially reduce these and justify their activities (2, 53).
Standards of practice
Standards of rehabilitation practice and PRM practice have been published in many countries, but are written in their local languages (46–49). An example of one, published by the British Society of Rehabilitation Medicine is shown in Appendix IV (54). Mapping of services to ensure that practice standards are maintained is important and the current work of the specialty is focused on this (54, 55). Finally, research must be embedded into service designs to allow the development of PRM to respond to changing patient and societal needs. The UEMS Section has described the standards, to which specialists in PRM work and the extent of their competencies and work (4). In addition, there is a need to address treatment pathways for people not considered eligible for admission to a PRM programme in post acute settings. Care pathways for them have been described in several countries, but reference is given to some of those in France, Italy and the UK (2, 46, 56–58).
AcknowledgEments
Other Members of UEMS Section of PRM Professional Practice Committee
T. Bender (HU), K. Borg (SE), H. Damjan (SI), R. Frischnecht (CH), E. Ilieva (BG), A. Kriscunias (LT), L. Krohn (DK), E. Kyllonen (FI), A. Luckmann (EE), J. McElligott (IR), V. Neumann (UK), A. Oral (TK), F. Parada Pereira (PL), K. Sekely-Kauzlaric (CR), J. Stanghelle (NO), K. Stibrant Sunnerhagen (SE), G. Stucki (CH), P. Takac (SK), P. Tederko (PL), V.R. Tuulik-Leisi (EE), M. Tzara (GR), E. Varela Donoso (ES), A. Vetras (LV), J. Votava (CZ), D. Wever (NL). M. Zampolini (IT).
References