OBJECTIVE: The aim of this study was to explore what characterizes patients receiving clinical interventions vs combined clinical and work-related interventions in a cohort of sick-listed subjects with musculoskeletal or mental disorders. Factors associated with return-to-work were also analysed.
DESIGN: A prospective cohort study.
METHODS: A total of 699 newly sick-listed patients responded to a questionnaire on sociodemographics, measures of health, functioning, work ability, self-efficacy, social support, work conditions, and expectations. The 3-month follow-up questionnaire included patients’ self-reported measures of return-to-work, work ability and type of interventions. The most frequent International Classification of Diseases-10 diagnoses for patients’ musculoskeletal disorders were dorsopathies (M50–54) and soft tissue disorders (M70–79), and for patients with mental disorders, depression (F32–39) and stress reactions (F43).
RESULTS: Patients with mental disorders who received combined interventions returned to work to a higher degree than those who received only clinical intervention. The prevalence of work-related interventions was higher for those who were younger and more highly educated. For patients with musculoskeletal disorders better health, work ability and positive expectations of return-to-work were associated with return-to-work. However, combined interventions did not affect return-to-work in this group.
CONCLUSION: Receiving combined interventions increased the probability of return-to-work for patients with mental disorders, but not for patients with musculoskeletal disorders. Better health, positive expectations of return-to-work and better work ability were associated with return-to-work for patients with musculoskeletal disorders.
Key words: musculoskeletal disorders; mental disorders; sick leave; ICD-10; return-to-work; intervention; work ability.
J Rehabil Med 2012; 44: 355–362
Correspondence address: Charlotte Wåhlin, Division of Physiotherapy, Department of Medical and Health Sciences, Linköping University, SE-581 83 Linköping, Sweden. E-mail: charlotte.wahlin@liu.se
Submitted May 25, 2011; accepted November 23, 2011
Introduction
There is ongoing debate concerning sick leave, entitlement to sickness benefits and vocational rehabilitation in Sweden. Studying early return-to-work (RTW) is of special interest since the Swedish government introduced reforms in the national sickness insurance system in 2008 focusing on early assessments of work ability, entitlement to benefits and the use of evidence-based methods for RTW. The primary goal within the first 90 days is to return to ordinary work if possible. There is also growing evidence that early rehabilitation and work-related interventions may be more effective than later interventions for enhancing RTW (1–3). A recent review (4) shows that access to vocational rehabilitation is poor and varies among patient groups. Medical treatment and clinical rehabilitation intervention are primarily provided by primary healthcare (PHC) or by private healthcare practitioners in Sweden. The occupational health service (OHS) is often responsible for assessment of work ability and work-related interventions. The different responsibilities place high demands on collaboration and coordination in the RTW process. In a study of sick-listed individuals, Heijbel et al. (5) found that access to vocational rehabilitation and contact with stakeholders involved in the RTW process increased if a rehabilitation investigation was made by the employer. Furthermore, Kärrholm et al. (6) concluded that systematic cooperation between employer, OHS and the social insurance office reduced the number of days on sick leave for employees on long-term sick leave. In clinical practice, patients on sick leave are mainly prescribed medical and clinical interventions.
Different intervention strategies can be used to increase the possibilities for workers to return-to-work. Clinical intervention with a combined behavioural-oriented physiotherapy and cognitive behavioural therapy intervention reduced the number of days on sick leave for women with spinal pain (7). The results of a review (8) showed that patients with non-acute low back pain can benefit from exercise interventions to reduce the number of days on sick leave. Multidisciplinary interventions have an effect on RTW for people on sick leave due to back pain (9, 10) and for patients on long-term sick leave with mainly musculoskeletal disorders (MSD) and mental disorders (MD) (11). However, evidence on the effect of multidisciplinary interventions for patients with neck pain is lacking (10), and the evidence base is also scarce for patients with MD. Several studies including MSD patients on long-term sick leave indicate that RTW is more successful if workplace interventions are implemented in addition to clinical rehabilitation interventions and multimodal rehabilitation (1–3, 11, 12).
A systematic review (13) of randomized controlled trials (RCTs) evaluating the effectiveness of workplace interventions compared with clinical interventions showed that workplace interventions for MSDs have an effect on reducing sickness absence, but not on health outcome. Shiri et al. (14) found that ergonomic intervention at the workplace reduced sickness absence for sick-listed employees with upper-extremity MSDs, but had no effect on pain outcome. Lambeek et al. (12) found that clinical rehabilitation interventions performed by a team in combination with workplace interventions including participatory ergonomics and graded activity programmes based on cognitive behavioural principles was effective for reducing back pain, increasing functioning and RTW. Research also indicates that work modification seems to be cost-effective for returning persons with MSD to work (1). Due to a lack of studies evaluating the effect of workplace interventions for MD, no conclusions can be drawn (13). However, there is evidence that workplace-oriented interventions for persons on long-term sick leave with burn-out increase RTW (15). Findings from a Dutch study also indicate that a cognitive behavioural approach combined with workplace advice promotes RTW for workers with psychological conditions (16).
However, there are conflicting results concerning the effectiveness of different interventions for sick-listed patients with MSD and MD. Identification of psychosocial and workplace variables are important in early patient screening to ensure the appropriate choice of tailored rehabilitation intervention (17–19). A number of studies have explored the factors associated with duration of sickness absence (18, 20–23) and prognostic factors for RTW (24–26). It is suggested that the individual’s work and life situations should be included in early patient screening and considered in returning individuals to work. In practice, rehabilitation interventions may be chosen not only by evidence, but also by other factors. Few studies have focused on praxis behaviour in relation to patient characteristics. Most clinical studies include selected patient populations and aim to analyse the effects of interventions in specific subgroups. This can limit the external validity of the results. In clinical reasoning, symptoms and health status, external factors, such as work demands, and the patient’s own attitudes and expectations may be important for choice of treatment (17, 19, 23). By changing the perspective and looking instead at clinical behaviour, and analysing which patients receive which type of interventions, the results may become more valid.
The aim of this study was to explore what characterizes patients receiving clinical interventions vs combined clinical and work-related interventions in a cohort of sick-listed patients with musculoskeletal or mental disorders. A further aim was to analyse the factors associated with RTW.
Methods
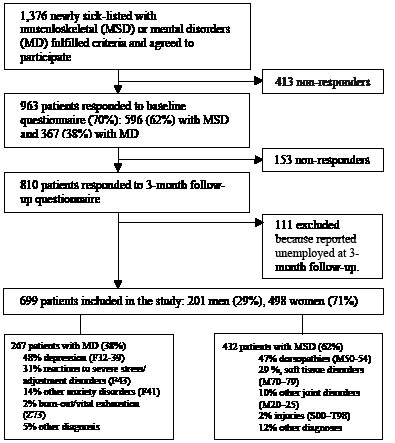
The Return to Work East Sweden Study (ReWESS) is a prospective cohort study comprising individuals who sought PHC or OHS for MSD or MD and were sick-listed. A total of 1,376 subjects were recruited between June 2008 and December 2009; a total of 413 subjects were excluded because they did not return the questionnaire or did not want to continue participating in the study. Thus, the final study sample consisted of 963 subjects on sick leave who answered the baseline questionnaire. All the subjects were followed up after 3 months, and a total of 810 subjects returned the questionnaire. A total of 111 patients were excluded because they were unemployed at the 3-month follow-up. Of these patients, 63 were also unemployed at baseline. This study is based on 699 subjects who answered both questionnaires and who were in employment at the 3-month follow-up.
Inclusion criteria were: being on sick leave for MSD or MD; age 18–65 years; and having a good knowledge of Swedish. Inclusions were based on an International Classification of Diseases (ICD)-10 diagnosis on the sickness certificate issued by physicians. As indicated in the flow-chart (Fig. 1), the ICD-10 diagnoses for MSD patients were: 47% with dorsopathies (M50–54), 29% with soft tissue disorders (M70–79), 10% with other joint disorders (M20–25), 2% with injuries (S00–T98), and 12% with other disorders of the musculoskeletal system. For MD patients, the diagnoses were: 48% with depression (F32–39), 31% with reactions to severe stress and adjustment disorders (F43), 14% with other anxiety disorders (F41), 2% with burn-out/vital exhaustion (Z73), and 5% with other diagnosis due to mental disorders. Exclusion criteria were sick leave for the same diagnosis in the previous month or sick leave due to a psychiatric diagnosis, such as schizophrenia or psychotic disorders, neurological disorders, rheumatic disease, fracture, or pregnancy. Every second week, the research team monitored all patients who became sick-listed at 1 of the 39 PHC centres of the region and 5 OHS centres. Only patients who fulfilled the inclusion criteria were asked to participate. Recruitment was carried out by telephone. All subjects received written and verbal information about the study before giving their consent to participation. The baseline questionnaire was sent to the patients immediately after they were included. The patients were followed up after 3 months using a postal questionnaire. If necessary, they were reminded by telephone a maximum of twice before being classified as non-responders. Ethical approval was granted by the local ethics committee (Dnr M78–05).
Fig. 1. Flowchart of participants.
Self-reported measures at baseline
The baseline questionnaire included sociodemographic variables (age, sex, marital status, and educational level), degree of sick leave, private economic issues, expectations and self-efficacy, social support, health, functioning and work ability, and work conditions. The patient’s educational level was categorized into two groups, lower education and higher education (university degree). The degree of sick leave was categorized as full-time or part-time and worries about private economic status as “yes” or “no”.
Expectations and self-efficacy. Expectations of RTW were measured by asking the question “In your estimation, what are the chances that you will be working in 6 months?” This question was rated on a 5-point scale, where 1 was “very good chance” and 5 was “very little chance”. Self-efficacy was measured by using the Self-Efficacy Scale (SES); patients were asked to rate their ability to perform 20 daily activities, despite their pain (27). The patients rated their ability on an 11-grade scale, with 0 for not confident at all to perform the activity and 10 for very confident. Higher scores indicate higher perceived self-efficacy, and the total range is 0–200 points.
Social support. Social support was measured using the Orth-Gomér instrument, Availability of Social Integration Index (AVSI), dealing with social support from family and close friends (28). Each dimension in AVSI consists of 6 items, ranging from 6 to 36, and higher scores indicate better social support.
Health, functioning and work ability. Health-related quality of life was measured using EuroQol-5D (EQ-5D), consisting of the 5 dimensions mobility, self-care, usual activities, pain and discomfort, and anxiety and depression (29). Each dimension is divided into 3 levels (no, some, severe problems), yielding a total of 243 possible states. A tariff for transforming states into scores ranging from –0.59 (worse than death as 0 = death) to 1 (perfect health) related to a UK population study (30). The second part includes the EQ visual analogue scale (EQ-VAS), with end points of zero for the worst imaginable health state and 100 for the best imaginable health state.
The Shirom Melamed Burnout Questionnaire (SMBQ) was used to measure different aspects of mental functioning (physical fatigue, tension, emotional exhaustion, listlessness and cognitive difficulties) (31). The SMBQ includes 22 items graded from 1 to 7, where high scores indicate more symptoms. The overall burn-out index (SMBQ-Global) is the average of the 22 items. A high level of burn-out on the SMBQ has been defined as a mean value greater than or equal to 4. The Functional Rating Index (FRI) was used to measure physical functioning and pain in the musculoskeletal system. Using a 5-point scale, the instrument consists of 10 questions pertaining to pain, sleep, daily activities, ability to work and body movements (32). The total FRI score is calculated, as recommended by Feise & Menke (32), by adding up all responses. The range of scores is 0–100%. A higher score indicates higher perceived dysfunction and pain.
To measure work ability we used the question “current work ability compared with the lifetime best” from the Work Ability Index (WAI) (33). The score is graded from 0 to 10, where 0 stands for completely unable to work and 10 stands for work ability at its best. A study by Ahlstrom et al. (34) shows that this single-item question on work ability may be a good alternative to the WAI, and Alavinia et al. (35) have shown that this item has predictive power for future disability.
Work conditions. Work conditions were measured with the Effort–Reward Imbalance scale (ERI) (36). Effort was measured using 6 items that deal with aspects of the work environment that are perceived as demanding. The higher the perceived distress because of high effort at work, the higher the resulting effort score. Reward was measured using 11 items concerning esteem, salary/promotion, and job security. The lower the reward score, the less perceived reward at work. Effort and reward questions contained a 4-point Likert scale ranging from 1 (is not correct at all) to 4 (is correct). The ratio of effort to reward expresses the amount of perceived effort–reward imbalance at work. Calculation of this imbalance was made using the formula described by Siegrist et al. (36). The ratio for effort–reward is high when the ERI ratio is higher than 1. Perceived physical strenuousness of work was measured using the Borg Scale, ranging from 6 to 20, asking the question: “How physically strenuous do you consider your work is, on average?”
Self-reported measures at 3-month follow-up
Self-reported work ability was followed up using the single-item question concerning the WAI item “current work ability compared with the lifetime best” (33–35). The 3-month questionnaire also included questions on healthcare utilization of PHC, OHS, private healthcare practitioners, and type of intervention received.
Primary outcome. The primary outcome, RTW within 3 months, was obtained through the question “Have you returned to work?” together with an indication of possible part-time RTW. In Sweden, sickness benefit can be paid at 25%, 50%, 75% or 100%, depending on assessment of the degree of work ability.
Classification of interventions
The patients in the clinical intervention group received clinical interventions from at least one health professional, viz., physician, physiotherapist, occupational therapist, behavioural therapist, psychologist and nurse. Information on work-related interventions were derived through the open question “What interventions/changes have been made at the workplace in order to facilitate your RTW?” This information was used to place the patient in one of the two subgroups: those who were given clinical intervention only, and those who were given a combination of clinical and work-related interventions.
Statistical methods
The analyses were performed in the two diagnostic groups of MSD and MD separately. Descriptive analysis for the intervention groups was carried out using proportions or means with standard deviations or confidence intervals (CI) for the variables assessed. Independent sample t-test or Pearson’s χ2 test were used in the comparison of the intervention groups concerning age, sex, educational level, economic situation, sick leave rate, RTW expectations and RTW. For adjusted analyses of group differences, analysis of covariance (ANCOVA) was used with age and gender as covariates. In that way, self-rated health, mental functioning, physical functioning, self-efficacy, work ability, physical strenuousness, and work conditions, were analysed.
Multiple logistic regression analysis was used to test the association between different explanatory variables and the outcome RTW within 3 months. The association between RTW and each possible explanatory variable was evaluated in a logistic regression, controlling for demographic variables including sex, age, educational level, and economic worries. Model I contains only demographic variables. Variables with a significance level of p < 0.10 were included in the following two models with adjustment for demographic variables. The results are presented in odds ratios (OR) with 95% CI. All tests were two-sided with significant level of p < 0.05. Statistical data were analysed using the Statistical software Package for the Social Sciences (SPSS) program (version 18.0).
Results
The 3-month follow-up cohort comprised 699 patients (498 women and 201 men). The mean age was 48 years (standard deviation (SD) 10.7). MSD was the most common diagnosis (62%). The 153 non-responders of the baseline cohort were significantly younger (p = 0.04), although no differences were found in distributions of sex (p = 0.24) and diagnosis (p = 0.8).
Mental disorders
For those patients who had MD and received combined interventions the mean age was lower (p = 0.03), their educational level was higher (p < 0.001), and their RTW expectations were higher at baseline (p = 0.04) compared with those who received clinical intervention. There was no significant difference between the groups concerning sex, marital status, worries about private economy or sick leave rate (Table I).
The group of patients who received combined intervention had, at baseline, significantly better social support (p = 0.02), better physical functioning according to FRI (p < 0.05), and better self-efficacy according to SES (p = 0.04), compared with those who received clinical intervention (Table II). There were no significant differences between the intervention groups concerning measures of health (EQ-5D, EQ-VAS), mental functioning (SMBQ), effort–reward at work (ERI) or physical strenuousness of work. Self-reported work ability did not differ significantly for any of the intervention groups at baseline or at the 3-month follow-up. After 3 months, both intervention groups had significantly improved their work ability. The group with MD who received combined interventions had a higher prevalence of RTW (87%) at the 3-month follow-up compared with the group who received clinical intervention (77%) (p = 0.036) (Table II). Most MD patients (74%) returned to work full-time, 8% returned to a degree of 75%, and approximately one-fifth (18%) returned to work partially to a degree of 25% or 50%.
Association with RTW. The demographic variables age, sex, education level and worries about private economy were not associated with RTW within 3 months (Table III). In model II, adjustments were made for RTW expectations, health measures, health resources and work ability; no association with RTW was found. In model III, further adjustment was made for type of intervention. Combined clinical and work-related intervention was associated with RTW within 3 months (OR 2.7, 95% CI 1.2–5.9).
Musculoskeletal disorders
For patients who had MSD and received a combined intervention, the educational level was higher (p = 0.005), they were significantly younger (p = 0.008), and they were on part-time sick leave to a higher degree (p = 0.004) than those who received clinical intervention. There was no significant difference between the groups concerning sex, marital status or worries about private economy or RTW expectations (Table I).
| Table I. Baseline characteristics of the total study population (n = 699) presented in subgroups of musculoskeletal disorders (MSD) and mental disorders (MD) divided into clinical vs combined intervention |
| Variables | MSD (n = 432) | | MD (n = 267) | |
| Clinical (n = 314) | Combined (n = 118) | p-value | Clinical (n = 146) | Combined (n = 121) | p-value |
| Sex, % (n) | | | | | | |
| Female | 63 (199) | 66 (78) | 0.6 | 82 (119) | 84 (102) | 0.07 |
| Male | 37 (115) | 34 (40) | | 18 (27) | 16 (19) | |
| Age, years, mean (SD) | 48.9 (10.5) | 45.9 (10.3) | 0.008 | 45.5 (10.7) | 42.6 (9.9) | 0.026 |
| Marital status, % (n) | | | | | | |
| Married/living together | 79 (243) | 77 (90) | 0.7 | 72 (103) | 81 (98) | 0.09 |
| Living alone/other | 21 (66) | 23 (27) | | 28 (40) | 19 (23) | |
| Educational level, % (n) | | | | | | |
| Lower education | 84 (260) | 72 (83) | 0.005 | 67 (96) | 44 (53) | 0.000 |
| Higher education (university) | 16 (49) | 28 (32) | | 33 (48) | 56 (67) | |
| Worried about economic situation, % (n) | | | | | | |
| Yes | 30 (92) | 23 (26) | 0.13 | 35 (51) | 28 (33) | 0.2 |
| No | 70 (213) | 77 (89) | | 65 (95) | 72 (86) | |
| Sick leave, % (n) | | | | | | |
| Full-time sick leave | 77 (222) | 63 (71) | 0.004 | 61 (83) | 60 (68) | 0.8 |
| Part-time sick leave | 23 (66) | 37 (42) | | 39 (53) | 40 (46) | |
| RTW expectations, % (n) | | | | | | |
| High | 80 (247) | 80 (94) | 0.97 | 76 (109) | 86 (104) | 0.04 |
| Low | 20 (61) | 20 (23) | | 24 (35) | 14 (17) | |
| The internal drop out varied to a small degree between variables, but do not influence the results when comparing groups. Significant results are shown in bold. RTW: return-to-work; SD: standard deviation. |
Patients with MSD who received a combined intervention perceived their work at baseline as less physically strenuous (p < 0.05) compared with those who received clinical intervention (Table II). There were no significant differences between the groups in measures of health (EQ-5D, EQ-VAS), mental functioning (SMBQ), physical functioning (FRI), social support (AVSI), self-efficacy (SES) or effort–reward imbalance at work (ERI). Self-reported work ability did not significantly differ between the groups at baseline or at the 3-month follow-up (Table II). After 3 months, both groups had significantly improved their work ability. The groups with and without combined intervention did not differ in prevalence of RTW within 3 months (Table II). Most MSD patients (81%) returned to work full-time, 3% returned to a degree of 75%, and 15% of MSD patients returned to work partially, to a degree of 25% or 50%.
| Table II. Self-reported health and work measures presented in subgroups of musculoskeletal disorders (MSD) and mental disorders (MD) divided into clinical vs combined intervention in mean and 95% confidence interval (CI), and in percentage (%), frequencies (n) for return-to-work (RTW). |
| Variables | MSD (n = 432) | p-value | MD (n = 267) | p-value |
| Clinical (n = 314) Mean (95% CI) | Combined (n = 118) Mean (95% CI) | Clinical (n = 146) Mean (95% CI) | Combined (n = 121) Mean (95% CI) |
| Health EuroQol | | | | | | |
| EQ-5D (–0.59 to 1.0) | 0.45 (0.42–0.5) | 0.42 (0.36–0.48) | 0.3 | 0.49 (0.44–0.53) | 0.51 (0.46–0.56) | 0.5 |
| EQ-VAS (0–100) | 56.4 (54.0–54.8) | 55.4 (51.6–59.3) | 0.4 | 46.7 (43.3–50.0) | 48.2 (44.6–51.9) | 0.5 |
| Mental functioning | | | | | | |
| SMBQ (1–7, burn-out ≥ 4) | 3.5 (3.3–3.6) | 3.5 (3.3–3.7) | 0.9 | 5.2 (5.0–5.4) | 5.2 (5.0–5.4) | 0.9 |
| Social support | | | | | | |
| AVSI (6–36) | 20.2 (19.6–20.9) | 21.3 (20.3–22.3) | 0.1 | 18.3 (17.4–19.2) | 19.9 (18.9–20.9) | 0.02 |
| Physical functioning | | | | | | |
| FRI (0–100) | 53.7 (51–56) | 56.2 (53–60) | 0.2 | 32.7 (30–35.4) | 28.6 (25.6–31.6) | 0.046 |
| Self-efficacy | | | | | | |
| SES (0–200) | 129 (124–134) | 122 (114–130) | 0.2 | 139 (131–146) | 151 (143–159) | 0.037 |
| Work conditions | | | | | | |
| ERI (high ≥ 1) | 0.93 (0.89–0.97) | 0.91 (0.84–0.97) | 0.5 | 1.1 (1.04–1.18) | 1.04 (0.96–1.1) | 0.2 |
| Physical strenuousness of work (6–20) | 14.7 (14.4–15) | 14.2 (13.7–14.6) | 0.042 | 12.8 (12.2–13.3) | 12 (11.4–12.6) | 0.066 |
| Work ability (0–10) | | | | | | |
| At baseline | 3.6 (3.3–3.9) | 3.7 (3.1–4.2) | 0.9 | 3.7 (3.3–4.2) | 3.2 (2.7–3.7) | 0.1 |
| At 3 months | 5.9 (5.6–6.3) | 5.9 (5.3–6.4) | 0.8 | 6.0 (5.5–6.4) | 6.4 (5.9–6.9) | 0.2 |
| Primary outcome RTW within 3 months, % (n) |
| Yes | 73 (229) | 79 (93) | 0.2 | 77 (112) | 87 (105) | 0.036 |
| No | 27 (85) | 21 (25) | | 23 (34) | 13 (16) | |
| Significant results are shown in bold. Scores and p-values adjusted for age and gender using analysis of covariance except for main outcome RTW. AVSI: Availability of Social Integration Index; ERI: Effort–Reward Imbalance Questionnaire; FRI: Functional Rating Index; SMBQ: Shirom Melamed Burnout Questionnaire; SES: Self-Efficacy Scale; Work ability: current work ability relative to lifetime best. |
Association with RTW. The demographic variables age, sex, education level and worries about private economy were not associated with RTW within 3 months (Table III). In model II, adjustments were made for RTW expectations, health measures, health resources and work ability. High RTW expectations (OR 2.4, 95% CI 1.2–4.8), better work ability (OR 1.2, 95% CI 1.1–1.4), and better self-rated health (EQ-5D) (OR 3.89, 95% CI 1.24–12.2) were significantly associated with RTW within 3 months. In model III, further adjustment was made for type of intervention, which did not change the results of model II.
| Table III. Regression model for mental disorders (MD) and musculoskeletal disorders (MSD): multivariate adjusted odds ratios (OR) for return-to-work (RTW) at 3 months and 95% confidence intervals (CI) in relation to demographic variables (model I), health and personal resources (model II), and to combined intervention (model III) |
| Variables | MD | MSD |
| Model I | Model II | Model III | Model I | Model II | Model III |
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Age | 1.00 | 0.97–1.04 | 1.02 | 0.98–1.05 | 1.02 | 0.98–1.06 | 0.99 | 0.98–1.02 | 0.99 | 0.96–1.02 | 0.99 | 0.96–1.02 |
| Sex (female) | 0.66 | 0.24–1.83 | 0.62 | 0.21–1.80 | 0.54 | 0.18–1.65 | 0.68 | 0.40–1.17 | 0.75 | 0.41–1.37 | 0.75 | 0.41–1.38 |
| University education | 0.93 | 0.47–1.84 | 0.83 | 0.39–1.76 | 0.76 | 0.35–1.64 | 1.69 | 0.86–3.34 | 1.72 | 0.81–3.66 | 1.68 | 0.79–3.59 |
| No worries about economy | 0.58 | 0.29–1.17 | 0.82 | 0.38–1.80 | 0.87 | 0.39–1.95 | 0.70 | 0.40–1.20 | 1.28 | 0.67–2.44 | 1.30 | 0.68–2.50 |
| Sick leave rate full-time | | | 0.44 | 0.17–1.11 | 0.47 | 0.18–1.21 | | | 2.41 | 1.22–4.76 | 2.41 | 1.22–4.78 |
| High RTW expectation | | | 1.84 | 0.73–4.62 | 1.70 | 0.67–4.40 | | | 1.22 | 1.07–1.38 | 1.21 | 1.07–1.38 |
| Work ability | | | 1.07 | 0.89–1.28 | 1.12 | 0.93–1.36 | | | 3.84 | 1.23–11.96 | 3.89 | 1.24–12.17 |
| EQ-5D | | | 0.50 | 0.10–2.48 | 0.43 | 0.08–2.24 | | | 0.80 | 0.62–1.02 | 0.80 | 0.62–1.02 |
| SMBQ | | | 0.65 | 0.39–1.08 | 0.64 | 0.39–1.07 | | | 1.00 | 0.98–1.03 | 1.00 | 0.98–1.03 |
| FRI | | | 0.99 | 0.97–1.02 | 0.99 | 0.97–1.02 | | | 0.99 | 0.98–1.00 | 0.99 | 0.98–1.00 |
| SES | | | 1.00 | 0.99–1.01 | 1.00 | 0.99–1.01 | | | 0.92 | 0.82–1.05 | 0.93 | 0.82–1.05 |
| Combined intervention | | | | | 2.73 | 1.25–5.96 | | | | | 1.22 | 0.66–2.26 |
| FRI: Functional Rating Index; SES: Self-Efficacy Scale; SMBQ: Shirom Melamed Burnout Questionnaire; EQ-5D: EuroQol-5D. |
Discussion
In this cohort study on newly sick-listed subjects with MSD or MD, the analyses focused on the first 3-month period of RTW. The main finding was that receiving combined clinical and work-related interventions was associated with increased prevalence of RTW within 3 months for patients with MD but not for patients with MSD. Better health, positive RTW expectations and better work ability, were associated with RTW for patients with MSD.
Among patients with MD, those who were younger, more highly educated, had stronger health resources and higher expectations of RTW, more often received work-related intervention. A study by van Oostrom et al. (37) concluded that workplace intervention is effective only for those employees on sick leave due to distress who are motivated to RTW. Present health status and RTW expectations are shown to influence the prognosis of returning to work (18, 24, 26). We found that the combined intervention group returned to work to a significantly higher degree at the 3-month follow-up compared with the clinical intervention group. Karlson et al. (15) also found positive effects of work-related interventions for patients with MD.
Factors associated with RTW at the 3-month follow-up differed for the two patient groups with MSD and MD. For patients with MD, the effect of receiving combined clinical and work-related intervention was greater than other prognostic factors for RTW. Studies have identified other important prognostic factors associated with RTW (20, 24, 26). For example, long duration of the problem, prior mental problems, older age, somatization and high disability were negative predictors for RTW.
It might be expected that the characteristics of individual health- and work-related factors would influence the choice of intervention, but for patients with MSD the intervention groups were quite similar in these factors. Patients with MSD who received combined interventions were to a greater degree younger, had a higher level of education and were more often on part-time sick leave. All these factors can be expected to influence a more successful RTW, which, in part, has been shown in previous studies of prognostic factors for duration of sick leave and RTW (18, 21, 22, 25). Choice of work-related interventions seems to be more influenced by these factors than by work-related factors. Irrespective of the type of intervention, the effect on RTW was equal. Part-time sick leave seems to increase access to work-related intervention, and as suggested by Sieurin et al. (38), it provides opportunities for employees with lower work ability to stay in work.
For patients with MSD, other factors were found to be associated with RTW compared with patients with MD, such as better health, positive RTW expectations and better work ability. Some of these personal resources have been found to reduce sickness absence in previous studies (18, 21, 22, 25). Lindell et al. (25) found that low total previous sick listing, young age and positive expectations of RTW were predictive for RTW and are important considerations in clinical practice. The results are ambiguous; Anema et al. (39) found that patients’ health characteristics contribute only somewhat to the explanation of RTW; instead job characteristics, receiving work interventions and compensation policies were more strongly related to sustainable RTW. Questions on beliefs and expectations were not included in their study. Others have shown that pain intensity and heavy physical work are the main significant factors for long-term sickness absence in MSD (21). Furthermore, a study by Alavinia et al. (35) demonstrated that poor work ability is predictive for receiving disability pension among construction workers, further supporting the importance of work ability in relation to RTW in MSD.
MSD and MD often lead to reduced work ability, and poor work ability is found to be associated with being on sick leave (40) and can also delay RTW (11). We found that RTW occurs for most patients even though high scores for work ability were not achieved. This merely shows that the likelihood of RTW is influenced by many factors, as reported in previous research (18–21). Work-related interventions were found to be scarce; only approximately one-quarter of patients with MSD and approximately half of patients with MD received a combined intervention. Similar results in a Swedish context have been presented by Heijbel et al. (5), who observed that less than half of the employees on long-term sick leave had been in contact with rehabilitation providers and stakeholders at the workplace. In an international comparison, it was found that work interventions were used sparingly in Sweden compared with other countries (9–20% for workers with low back pain) (39). The incentives for employers to provide workplace adjustments have been reduced further since that study, which may be a reason for the low prevalence of workplace interventions in our study. Employers seem to be more willing to invest in work-related interventions for those employees who are younger, more highly educated, or have other stronger individual health resources. This indicates that access to work-related intervention may not be equitable in practice. A Swedish review by Burstrom et al. (4) found differences concerning access, e.g. men, younger employees, being on long-term sick leave and those who were employed rather than unemployed were more likely to receive vocational rehabilitation. Women comprised the majority of our study population, as in many other studies including sick-listed persons (5, 14, 15, 26). This might reflect that women have a higher risk of being sick-listed compared with men. Previous research has found that being a women is associated with increased risk for long-term sickness due to MSD (21, 22). We found that the gender distribution was similar with regard to the type of intervention given. Gender was considered in the analysis of factors associated with RTW, and was not found to be associated with RTW. Similar results were found by Brouwers et al. (24) for employees sick-listed due to MD.
In RTW research, self-reported work disability and duration of sick leave are frequently-used outcomes (2, 11, 12). In this study, we used self-reported measurement of at least part-time RTW as the primary outcome vs not returning to work. Further analysis is needed to understand whether these patients were stable in their RTW. Returning to at least part-time work has positive consequences for the patients (38), although in most countries part-time sick leave is rare. When comparing the RTW process in western countries, there are several differences with regard to employment and working conditions, disability policies, healthcare and social insurance systems (2, 21, 38, 39). The economic incentive for employers to take a greater responsibility for vocational rehabilitation varies between countries depending on laws and insurance systems. However, the need to develop governmental and workplace policies for RTW seems to be a universal demand.
Self-reported measurement might be criticized, but earlier studies have found good agreement on self-reported data from employer and register information on sickness absence (41), and between self-reported data on sickness absence days and employers’ registers for the same period (42). Based on previous research we used the single item “current work ability compared with lifetime best” for measurement of work ability (34, 35). Alavina et al. (35) found that all of the separate scales in the WAI had predictive power for future disability, with the highest influence of current work ability in relation to job demand. Improvement in work ability is commonly used as an outcome measure for evaluating RTW interventions (3, 11). The severity of patients’ health problems are looked at from a patient perspective by using self-reported measures of health, mental and physical functioning and work ability, providing a more nuanced understanding of the patient’s condition. A limitation of the study may be the lack of measures of depression and anxiety, which are common symptoms in patients with long-standing pain. As this study focused on newly sick-listed subjects, these symptoms may be less prevalent. SMBQ was used as measure of the mental health condition. The Hospital Anxiety and Depression Scale or the Patient Health Questionnaire could be used to further understand mental functioning in MSD and MD patients (7, 10, 23). In this study, a follow-up questionnaire specifically tailored to the research questions and focusing on which patients received what type of intervention was used.
A strength of the study is the longitudinal prospective design, which enables us to analyse what actually happens in clinical practice. Another strength of the study is the recruitment strategy. Inclusion of sick-listed individuals was based on physician assessment of the diagnosis according to ICD-10, instead of only being based on self-reported disabilities. Few studies include both patients with MSD or MD, mainly because they may have different causes of sick leave and interventions need to be tailored according to the patients’ symptoms, prerequisites and needs. However, these two groups represent the most common causes of sick leave; they are frequent visitors in healthcare and factors associated with longer duration of sickness absence overlap between the two group (18, 23). From a patient perspective, the sick leave process has similarities no matter what the diagnosis, and is challenging for healthcare providers and employers to handle together with the sick-listed person (23, 43). A clinical implication of this study is that the rehabilitation process needs to adopt a broader perspective for sick-listed patients to include patient’s individual health-related needs and aspects of employment and work conditions. Furthermore, a clinical implication for both diagnostic groups of patients is that healthcare providers, employers and other stakeholders need to strive for access to work-related interventions.
In this study we controlled for several sociodemographic variables when analysing the factors associated with RTW. Although our results may be influenced by differences in patients’ personal resources, those with better prerequisites might also return earlier to work. However, the pattern differed for the two diagnostic groups. The RTW process was found to be better for patients with MD compared with patients with MSD. We suggest further evaluation of the type, amount and duration of interventions given in the RTW process. Future studies should strive to explore behaviour in practice, preferences in interventions enhancing RTW, and to assess who needs work-related interventions.
In conclusion, when comparing the intervention groups, for MD patients, those who had stronger individual resources and higher expectations of RTW received work-related interventions to a higher degree. For patients with MD and MSD, the prevalence of work-related interventions was higher for those who were younger and more highly educated. Receiving combined interventions increased the probability of patients with MD returning to work but not of patients with MSD. Better health, positive RTW expectations and better work ability were associated with RTW for patients with MSD.
Acknowledgements
The authors would like to thank all the participants in the ReWESS study, the healthcare providers involved in the study, and Henrik Magnusson for statistical support. This study was funded by funded by FAS (Swedish Council for Working Life and Social Research).
References