OBJECTIVE: Low admission Norton scale scores (ANSS) are usually associated with high risk of pressure ulcer. The aim of this study was to determine whether low ANSS are also associated with long-term mortality following rehabilitation in older adults.
DESIGN: A cross-sectional retrospective study.
SUBJECTS: Consecutive older adults admitted during 2009 for rehabilitation following stroke (n = 110), hip arthroplasty (n = 201), and hospital-associated deconditioning (n = 96).
METHODS: Patients were followed until January, 2011. Long-term mortality rates, i.e. within one year or more, were compared between patients with low (≤ 14) ANSS and patients with high (≥ 15) ANSS.
RESULTS: The final cohort included 407 patients (67.8% females; mean age 82.2 years). Overall, 193 (47.4%) patients had low ANSS. Patients were followed for a mean period of 524 days. Overall, 66 (16.2%) patients died during this time. Patients who died had significantly lower mean ANSS compared with those who survived (13.9 vs 14.9; p = 0.001). Cumulative survival rates were significantly lower among patients with low ANSS compared with patients with high ANSS (p = 0.004). Regression analysis showed that ANSS were independently associated with mortality (p = 0.02), regardless of rehabilitation cause, age, gender, and chronic co-morbidities.
CONCLUSION: ANSS may be used not only for evaluating pressure ulcer risk, but also for predicting long-term mortality, i.e. within one year or more, following rehabilitation in older adults.
Key words: death rates; pressure sore; rehabilitation.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Dan Justo, Department of Geriatric Rehabilitation, Tel-Aviv Sourasky Medical Center, 6 Weitzman Street, Tel-Aviv 64239, Israel. E-mail: danj@tasmc.health.gov.il
Submitted May 6, 2011; accepted October 31, 2011
INTRODUCTION
Stroke and hip fracture in older adults are associated with increased long-term mortality. According to Kaste et al. (1), the one-year mortality rate in older adults with stroke is 21%. According to Magaziner et al. (2), 17.4% of older adults with hip fractures die within one year. Rehabilitation in older adults with stroke or hip fractures is associated with decrease in these long-term mortality rates, although they remain high (3–5). Older adults with hospital-associated deconditioning (HAD) due to other surgical and medical conditions are even at higher risk for death long after rehabilitation (5). In face of these high long-term mortality rates, it is of great clinical significance to predict mortality following rehabilitation in older adults with stroke, hip arthroplasty and HAD.
The Norton scoring system is usually used for evaluating pressure ulcer risk (6). It includes 5 domains that concern fundamental aspects of well-being: physical condition, mental condition, activity, mobility, and incontinence (7). These are also features of the comprehensive geriatric assessment (CGA) made by geriatricians, which predicts morbidity in hospitalized older adults (8). Hence, the Norton scoring system may be used for predicting different aspects of prognosis in older adults other than predicting pressure ulcer risk. Indeed, we have previously shown that low admission Norton scale scores (low ANSS) are associated with prolonged rehabilitation and poor rehabilitation outcome in older adults following stroke, hip arthroplasty, and HAD (9–11). The aim of the present study was to investigate if low ANSS are also associated with all-cause long-term mortality, i.e. within one year or more, following rehabilitation in older adults with stroke, hip arthroplasty and HAD.
Material and methods
Study design
This was a cross-sectional study conducted at the department of Geriatric Rehabilitation of Tel-Aviv Sourasky Medical Center, a tertiary medical centre. The study was approved by the local ethics committee according to the principles of the Declaration of Helsinki. The electronic medical charts of consecutive older adult (≥ 65 years) patients admitted during 2009 for rehabilitation following stroke, hip arthroplasty and HAD, were reviewed.
Subjects
Included were older adults admitted for rehabilitation following stroke (n = 110), hip arthroplasty (n = 201), and HAD (n = 96). Clinical features of older adults going through rehabilitation in our institute following stroke, hip arthroplasty, and HAD, have been described previously (9–11). Excluded were patients in whom ANSS were not measured and/or were not documented in the electronic charts (n = 26).
Rehabilitation
Rehabilitation was sub-acute (1.5 h per day, 5 days a week) and included strengthening, increasing range of motion, transfer training, ambulation training, and training in activities of daily living. Rehabilitation was completed once the patient had ambulated independently, or had gained previous ambulation abilities, or had gained no improvement in ambulation despite the efforts of physical therapists.
Measurements
Measurements included: ANSS, demographic data, co-morbidities, and mortality until January 2011. Data concerning mortality was extracted from the Israeli General Register Office database. Pressure ulcers in all stages were documented (12). Definitions of co-morbidities were consistent with those of the International Classification of Diseases-9 (ICD-9) scoring system (13). ANSS were measured routinely by qualified nurses for all patients. Measuring ANSS is included in the standard training of Israeli nurses.
Norton Scoring System
Each of the 5 domains of the Norton scoring system was assessed on a scale between 1 and 4 points, and the final score ranged between 5 and 20 points (see Appendix I). ANSS ≤ 14 was considered low and represented high risk for pressure ulcers. ANSS ≥ 15 was considered high and represented low risk for pressure ulcers. The sensitivity and specificity of the Norton scoring system was 63% and 70%, respectively (6, 7). The inter-rater reliably of different domains of the Norton scoring system ranged between 0.558 and 0.761 (14).
Statistical analysis
Continuous variables were expressed as mean (standard deviation (SD)), median and inter-quartile range (IQR). The one-way Kolmogorov- Smirnov test was used in order to assess the distribution of continuous variables. The Student’s t-test was used to compare between the mean values of continuous variables with parametric distributions. The Mann-Whitney test was used to compare between the mean values of continuous variables with non-parametric distributions. The Fisher’s exact test was used to make comparisons between the prevalence of categorical variables. Cumulative survival rates were compared between patients with low and high ANSS by using the Kaplan–Meier analysis. Binary regression analysis was used in order to study which variables were independently associated with long-term mortality. Two-tailed p < 0.05 was considered statistically significant. Version 17.0 of the SPSS (SSPS Inc., Chicago, IL, USA) statistical software was used for all statistical analysis.
Results
The final cohort included 407 patients: 276 (67.8%) females and 131 (32.3%) males. Mean age for the entire cohort was 82.2 years (SD 6.7) (median: 83 years; IQR: 78–83 years). The 4 most common chronic co-morbidities were hypertension (n = 336; 82.6%), diabetes mellitus (n = 116; 28.6%), ischaemic heart disease (n = 114; 28.0%), and Parkinson’s disease (n = 31; 7.6%). Overall, 34 (8.4%) patients had pressure ulcers during rehabilitation.
Mean ANSS were 14.6 (SD 2.2) (median: 15; IQR: 13–16), and 193 (47.4%) patients had low (≤ 14) ANSS. Age was higher among patients with low ANSS relative to patients with high ANSS, as were the prevalence of hypertension and ischaemic heart disease. On the other hand, the percentage of pressure ulcers during rehabilitation was similar among patients with low ANSS and patients with high ANSS (Table I).
| Table I. Clinical characteristics of patients with low and high admission Norton scale scores (ANSS) |
| Variables | High Norton (n = 214) | Low Norton (n = 193) | Odds ratio (95% CI) | p-value |
| Age, years, mean (SD) | 80.7 (6.9) | 83.9 (6.1) | Not applicable | < 0.0001 |
| Female gender, n (%) | 144 (67.3) | 132 (68.4) | 1.05 (0.69–1.59) | 0.832 |
| Hypertension, n (%) | 169 (79.0) | 167 (86.5) | 1.71 (1.00–2.90) | 0.050 |
| Diabetes mellitus type 2, n (%) | 58 (27.1) | 58 (30.1) | 1.15 (0.75–1.77) | 0.512 |
| Ischemic heart disease, n (%) | 49 (22.9) | 65 (33.7) | 1.71 (1.10–2.64) | 0.020 |
| Parkinson’s disease, n (%) | 11 (5.1) | 20 (10.4) | 2.13 (0.99–4.57) | 0.061 |
| Pressure ulcers, n (%) | 13 (6.1) | 21 (10.9) | 1.88 (0.91–3.88) | 0.106 |
| CI: confidence interval; SD: standard deviation. |
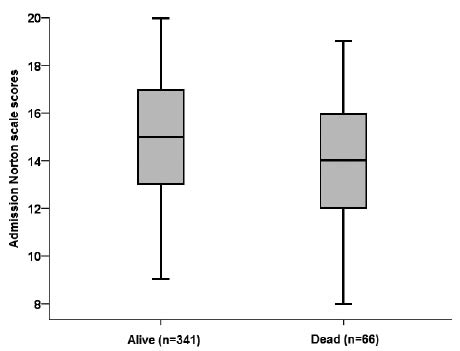
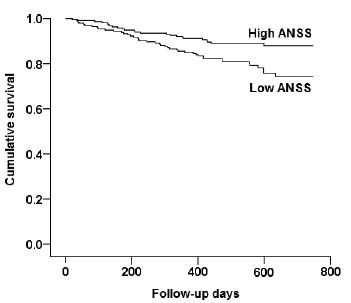
Patients were followed for a mean period of 524 days (SD 164) (median: 548 days; IQR: 428–659 days). Overall, a mean of 66 (16.2%) patients died within 270 days (SD 167) (median: 236 days; IQR: 131–396 days): 20 (18.2%) stroke patients, 27 (13.4%) hip arthroplasty patients, and 19 (19.8%) HAD patients. Patients who died had significantly lower mean ANSS compared with those who survived (13.9 (SD 2.3) vs 14.9 (SD 2.2); Fig. 1). Cumulative survival rates were significantly lower among patients with low ANSS relative to patients with high ANSS (Fig. 2). Binary regression analysis showed that ANSS were associated with mortality independent of rehabilitation cause, age, gender, and chronic co-morbidities. Age, female gender, and ischaemic heart disease were also independently associated with mortality in the study (Table II).
Fig. 1. Mean admission Norton scale scores of patients who died and those who survived, p = 0.001.
Fig. 2. Kaplan–Meier curves representing cumulative survival of patients with high and low admission Norton scale scores (ANSS), p = 0.004.
| Table II. Binary regression analysis showing which variables were independently associated with long-term mortality |
| | B | SE | Wald | p-value | HR | 95% CI for HR |
| Lower | Upper |
| Rehabilitation cause | –0.164 | 0.178 | 0.850 | 0.357 | 0.849 | 0.599 | 1.203 |
| Female gender | 0.731 | 0.316 | 5.358 | 0.021 | 2.076 | 1.118 | 3.854 |
| Age | 0.084 | 0.025 | 11.678 | 0.001 | 1.088 | 1.036 | 1.141 |
| ANSS | –0.155 | 0.067 | 5.306 | 0.021 | 0.857 | 0.751 | 0.977 |
| Hypertension | 0.298 | 0.404 | 0.544 | 0.461 | 1.347 | 0.610 | 2.973 |
| Diabetes mellitus type 2 | 0.479 | 0.362 | 1.757 | 0.185 | 1.615 | 0.795 | 3.280 |
| Ischaemic heart disease | –0.654 | 0.322 | 4.124 | 0.042 | 0.520 | 0.277 | 0.977 |
| Parkinson’s disease | –0.128 | 0.486 | 0.070 | 0.792 | 0.879 | 0.339 | 2.280 |
| HR: hazardous ratio; SE: standard error; ANSS: admission Norton scale scores; CI: confidence interval. |
Discussion
Pressure ulcers are a major problem associated with morbidity and mortality in older adults. Risk assessment scales, such as the Norton scoring system, have been available for nearly 50 years for assessing the risk of pressure ulcers, but their usefulness in preventing pressure ulcers remains uncertain, and some believe they are useless (15, 16). In our opinion, and accordance with previous studies concerning the ANSS (9–11), it is too early to abandon the Norton scoring system, especially now, after we have shown again that it can be used for purposes other than predicting pressure ulcer risk. To the best of our knowledge, this is the first study in which the Norton scoring system has been used for evaluating post-rehabilitation long-term mortality risk. According to the current findings, ANSS have been independently associated with long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD, regardless of rehabilitation cause, age, gender, and chronic co-morbidities.
According to Johnson et al. (5), 18%, 14% and 30% of patients with stroke, hip arthroplasty, and HAD, respectively, die within one year of rehabilitation. These findings are consistent with the current findings. Long-term mortality in older adults with stroke may be associated with male gender, urinary incontinence (17), depressive symptoms (18), and very old age (19). Long-term mortality in older adults with hip fractures may be associated with post-operative complications, baseline dependency in activities of daily living (ADL), very old age (4), and baseline poor mental status (20). Predictors of mortality among older adults with HAD have seldom been studied thus far (21), although increasing chronic co-morbidity and incontinence may be associated with long-term mortality in this population (5). Incontinence, dependency in ADL, and mental condition, are features of the Norton scoring system (6, 7). Thus, it is not surprising that ANSS have been associated with long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD. Age, gender, and chronic co-morbidities have also been taken into account in the regression analysis, but ANSS have remained independently associated with long-term mortality following rehabilitation in the study population regardless of these confounders. Other variables, such as low albumin serum levels and dementia, are also associated long-term mortality following rehabilitation in older adults (22, 23), but measuring ANSS does not require blood sampling, and the Norton scoring system is easier to use compared with cognitive screening tools.
We believe that ANSS should be added to the list of prognostic tools used for predicting long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD. Contrary to the CGA made by geriatricians, the Norton scoring system is simple and not time-consuming, and accordingly, can be used as a screening geriatric assessment tool by nurses. Finally, and most importantly, the Norton scoring system has already being used successfully all over the world for many years for predicting pressure ulcer risk. Hence, we believe it can also be used for other purposes immediately.
One might claim that it should be no surprise that ANSS is associated with long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD, since patients who develop pressure ulcers are more likely to have a prolonged hospital stay and complications (24). However, according to the binary regression analysis, ANSS have been associated with long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD, independent of the appearance of pressure ulcers.
The sensitivity and specificity of the Norton scoring system are 63% and 70%, respectively (7). The inter-rater reliably of different domains of the Norton scoring system ranges between 0.558 and 0.761 (14). Hence, we acknowledge the fact that long-term mortality prediction cannot be based upon a specific ANSS cut-off. In face of this limitation, ANSS have been considered a continuous variable in the regression analysis rather than a dichotomous variable. However, ANSS have been associated with long-term mortality.
Another limitation is the fact that the exact cause of death in the cohort has not been studied. It is possible that some of the patients died of causes not related to the rehabilitation and not associated with stroke, hip arthroplasty, or HAD. This limitation is known in studies concerning all-cause mortality. Future studies should address the issue of exact cause of death, as well as the association between ANSS and recurrent falls, injuries, fractures, and hospitalizations, following rehabilitation for stroke, hip arthroplasty, and HAD.
In conclusion, ANSS is independently associated with long-term mortality following rehabilitation in older adults with stroke, hip arthroplasty, and HAD, regardless of rehabilitation cause, age, gender, and chronic co-morbidities. Accordingly, we believe ANSS should be added to the tools used for predicting long-term mortality following rehabilitation in older adults. However, prospective study of these findings is needed.
References