OBJECTIVE: The aim of this study was to evaluate the relationship between the functional status of patients with low back pain and the perceived importance of pain-related everyday functions assessed in the Oswestry Disability Index.
DESIGN: The sample was based on 219 successive adult patients with low back pain referred to a tertiary clinic.
Patients: A total of 168 patients (76.6%) participated in the study, mean age 48.2 years (standard deviation 11.6).
METHODS: In a questionnaire the patients were asked to complete the Oswestry Disability Index and the same domains using visual analogue scales. Subjects were also asked to assess the relative importance of these domains by using a visual analogue scale.
RESULTS: Sleeping, walking and personal care were the 3 most important functions for both men and women. Patients with low back pain gave more importance to most of the functional abilities that are needed in everyday life and self-management than to the intensity of pain. However, when the patients reported their current experience in functions, greatest difficulty was experienced in lifting.
CONCLUSION: Development of outcome measure instruments for patients with low back pain could benefit from taking into account patients’ perceptions. In addition, functional measures should be weighted according to the relative importance of each function to the patients.
Key words: perception; quality; outcome; relative importance; low back pain; Oswestry Disability Index.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Carita Kemppi, Department of Physical and Rehabilitation Medicine, Turku University Hospital, PO Box 52, FI-20521 Turku, Finland. E-mail: carita.kemppi@tyks.fi
Submitted March 22, 2011; accepted September 9, 2011
Introduction
Low back pain (LBP) affects up to 85% of people in the industrialized countries at some point in their lives (1). The incidence and prevalence are roughly the same all over the world (1, 2). LBP is neither a disease nor a diagnostic entity of any sort; it is rather a constellation of symptoms and clinical presentations (3). It is considered to be one of the major causes of musculoskeletal disability (3), being a common reason for using healthcare.
Patient’s experienced intensity of pain is commonly measured by visual analogue scale (VAS) (4). A change or reduction in pain, measured on this VAS scale, is thought to be an outcome measure that also indirectly defines treatment success in a particular disease. However, a small study of 13 patients with chronic pain (including LBP) showed that functional tasks affecting everyday living were the most important outcome markers for these patients (5).
Despite its frequency of occurrence and ubiquitous nature, the symptoms of LBP and the associated disability do not always correlate with objective data, such as imaging results (6). In addition, physical examination findings, such as range of motion and muscle strength, often have only a weak association with those outcomes that patients consider relevant, such as symptom relief, daily functioning or work status (7). It is often impossible to determine the definite cause or aetiology of back pain (6, 8). Thus, measures to depict patients’ overall functional ability are needed.
Several disease-specific outcome measures have been developed to help measure disability of patients with LBP with the Oswestry Disability Index (ODI) or its adaptations among the most widely used and well validated (9–12). The ODI consists of questions about back pain intensity and 9 common daily functions (personal care, lifting, walking, sitting, standing, sleeping, sex life, social life and travelling). These items were selected for the ODI based on the views and opinions of clinicians and the outcome measures that they considered to be potentially relevant for describing and measuring the disabilities of patients with LBP (9, 12). Although the ODI is based on a patient’s subjective experience of his or her own state of disability, the selection and verbal expressions of these functional alternatives have been determined by clinicians. When a patient assesses his or her functional ability he or she needs to choose from pre-defined alternatives with fixed verbal expressions (9–11). It may be that none of the pre-determined expressions adequately describes his or her current condition.
In the ODI, all the functional disabilities measured to produce the overall index are considered to be equally important and are given equal weight in the index computation. Although the use of equal weights makes the index figure computation easier, there is no scientific evidence to support the underlying idea that all the functions or the ability to perform these functions are equally important when determining the functional disability of patients. This holds both for clinical assessment by health professionals and for patient perception.
In studying medical conditions, many efforts have been made to develop disease-specific outcome measures, in which individuals rate and weight the relative importance of everyday activities with respect to their perceived relevance (13–18). These measurement properties have been investigated, but not widely assessed in the field of LBP (19).
The aim of this study was to determine the relative importance of different pain-related everyday functions, from the perspective of patients who have LBP, in order to establish whether patients themselves consider the functional abilities assessed in the ODI to be equally important to their daily lives.
Methods
The sample was based on 219 successive adult patients with LBP referred to the Turku University Hospital, Department of Physical and Rehabilitation Medicine. The sample was systematically collected from October 2007 to May 2008. The key inclusion criterion was LBP as the primary cause for referral; patients with LBP and also concomitant symptoms of pain in other parts of back, and pain and/or disabilities in upper and/or lower extremities were also accepted. Exclusion criteria included LBP caused by infection, acute trauma or malignancy, inability to read and write Finnish and cognitive problems to co-operate.
The ethics committee of The Hospital District of Southwest Finland approved the study, and the subjects identified for potential inclusion in the study received a written description of the sampling, study purpose, the planned use and storage of the information they were to provide and a description of the subject’s rights according to the Declaration of Helsinki. Subjects willing to participate gave written informed consent and permission to collect data from hospital registers.
Two separate face and content validity studies among convenient samples of 21 and 23 healthy young adults were carried out. In addition, the time needed for answering and how easy the questions were to comprehend were tested. The findings from these pilot studies were used to develop the final questionnaire. The questionnaires were posted to participating patients, who were asked to complete and return it on their next visit to the specialist in Physical and Rehabilitation Medicine.
Functional status was assessed using the methods of the traditional ODI (v2.1), and VAS. In the ODI, pain and 9 functions each have 6 ordinal statements, from 0 (indicating no problems in abilities or no pain) to 5 (denoting the most disabling level or worst imaginable pain). The total score is converted to a percentage. The other method to measure the functional status was based on self-assessment of pain and the very same 9 functions as in the ODI, using a 10-cm double anchored horizontal VAS, with endpoints from 0 (no problem in performing) to 100 (impossible to perform). Pain intensity was scored in VAS with endpoints 0 (no pain at all) to 100 (worst possible pain). The total score was converted to a percentage. To clarify the influence of answering order, every second subject received a form where the traditional ODI (v2.1) was solicited first and VAS after. The other half received a form with VAS first, followed by the ODI (v2.1).
After assessing the disability status, the subjects were asked to assess the relative importance of pain intensity and of each of the 9 separate functions used in the ODI (v2.1). This was determined by using VAS, with endpoints from 0 (extremely unimportant) to 100 (extremely important).
Statistical analysis
Raw data was used in descriptive and univariate statistical analyses. In many cases, the distributions of the disability functions were skewed and the descriptive analyses were based on Wilcoxon signed-rank test, and the χ2 tests were applied for the proportions. However, for computing the overall ODI and VAS scores the few missing values were replaced by group means. There was a normal distribution of overall ODI and VAS scores and both parametric and non-parametric tests produced identical statistical significance levels.
Results
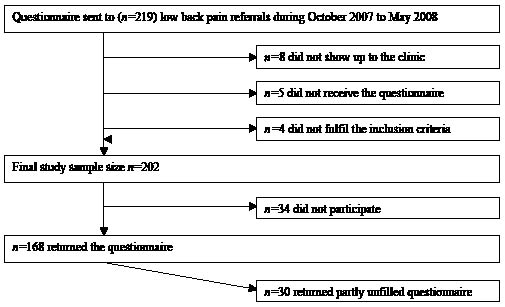
Eight patients did not attend the clinic, 5 reported that they had not received the questionnaire and 4 dropped out of the study because of their inability to co-operate. The most commonly expressed reason for not participating was improvement or recovery and not having LBP symptoms at the time of the study. The final study sample was 202 patients with LBP (Fig. 1).
Fig. 1. Sampling and participation of the study sample.
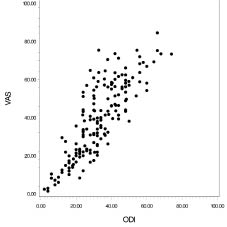
Altogether 168 patients returned the questionnaire (76.7%). The sample consisted of 71 males (42%) and 97 females (58%) with a mean age of 48.2 years (standard deviation (SD) 11.6). Some respondents (n = 30) did not answer all the questions, most commonly about sex life (n = 18). The mean overall ODI score was 32.8% and mean overall VAS score was 39.2%, differences between sexes were minor (NS). There was a high correlation (r = 0.828, p < 0.0001) between the overall scores of ODI and VAS (Fig. 2).
Fig. 2. Relationship of the overall scores of Oswestry Disability Index (ODI) and visual analogue scale (VAS) methods expressed as percentages (r = 0.861, p < 0.001).
The relative importance of pain intensity and different pain-related functions assessed varied considerably, but the order was almost the same with only a small variation between sexes. Sleeping, walking and personal care were the 3 most important functions for both men and women. The patients considered sleeping to be of more significance than most other functions or pain. This was particularly pronounced among men (Table I). Patients with LBP gave more importance to most of the functional abilities that are needed in everyday life and self-management, than to the intensity of pain. Sex life, lifting and travelling were considered the 3 least important functions both among men and women. Among men increasing age had a statistically significant correlation with lower importance of sex life (p < 0.01), standing and lifting (p < 0.05). Among women the correlations were similar, although statistically non-significant.
| Table I. Perceived relative importance of pain and 9 selected pain-related functional abilities among patients with low back pain by sex, presented in order of importance |
| Items | Men Median | Women Median | All Median |
| Sleeping | 96 | 95 | 96 |
| Personal care | 92* | 96 | 95* |
| Walking | 92* | 95 | 94** |
| Sitting | 92*** | 91*** | 91*** |
| Social life | 90*** | 92*** | 91*** |
| Standing | 90*** | 91*** | 91*** |
| Pain | 87*** | 90*** | 89*** |
| Sex life | 86*** | 88*** | 87*** |
| Lifting | 79*** | 79*** | 79*** |
| Travelling | 74*** | 78*** | 76*** |
| Statistical comparison between sleeping and all other items by Wilcoxon signed-rank test: *p < 0.05, **p < 0.01, ***p < 0.001. |
The correlations between pain intensity and all functional abilities measured with VAS (r = 0.430–0.595) were statistically significant (p < 0.001) for both among men and women. However, there were no significant correlations between the pain intensity and the relative importance of different functions or pain.
When patients reported their current experience in functions, greatest difficulty was experienced in lifting (Table II) and this was seen both with the ODI and VAS methods. Sleep was one of the functions least affected by LBP. However, when the functions were placed in the order of experienced difficulty, the order varied depending on which method was used.
| Table II. Patient experiences of pain and 9 selected pain-related functional abilities measured with visual analogue score (VAS) method among patients with low back pain by sex |
| Items | Men Median (IQR) | Women Median (IQR) | All Median (IQR) |
| Pain intensity | 54.0 (26.0–67.0) | 51.0 (30.0–68.5) | 52.5 (28.3–68.0) |
| Personal care | 27.0 (9.0–45.0) | 22.0 (4.5–39.0) | 24.5 (24.5–43.8) |
| Lifting | 49.0 (29.0–73.0) | 59.0 (33.5–71.5) | 53.5 (30.0–72.8) |
| Walking | 34.0 (12.0–63.0) | 37.0 (14.0–60.0) | 35.5 (13.3–61.8) |
| Sitting | 41.0 (19.0–65.0) | 49.0 (25.5–65.0) | 44.5 (22.0–65.0) |
| Standing | 40.0 (20.0–63.0) | 41.0 (21.0–61.0) | 41.0 (21.0–61.8) |
| Sleeping | 29.0 (12.0–50.0) | 37.0 (9.5–63.5) | 32.5 (11.0–60.8) |
| Sex life | 24.0 (7.0–47.0) | 22.0 (7.0–38.5) | 23.5 (7.0–43.8) |
| Social life | 28.0 (5.0–50.0) | 36.0 (10.0–61.0) | 32.5 (9.0–58.8) |
| Travelling | 38.0 (16.0–65.0) | 43.0 (20.5–70.0) | 41.0 (18.3–67.0) |
| IQR: interquartile range. |
The order of presenting the two methods did not affect the participation rate, the measures of functional ability or their relative importance. However, all functional assessments using the VAS method were completed by significantly more patients (92.9%) than with the ODI method (74.5%, p < 0.001). Furthermore, the number of unanswered items were more than double with the ODI (n = 26) method than with the VAS method (n = 12, p < 0.001).
Discussion
The Hospital District of Southwest Finland provides a healthcare service for approximately 460,000 people residing in the area. The systematic sampling of the districts referrals produced a representative sample. The diagnosis of each patient case referred was also confirmed by specialists in the Department of Physical and Rehabilitation Medicine. Thus, our sample represents patients with LBP seen in a tertiary clinic and our findings can be best generalized to such chronic LBP population. As the aim of this particular work was not to produce an abridged version of the ODI, the findings of the present study can be used to critically evaluate the role of different functional abilities when evaluating patient’s overall clinical status.
Occupational status is an important confounder in patients with LBP (20). Although the aggregate point prevalence for LBP among European workers was 33.0% in 2000, it ranged between 22.0% and 57.0% depending on the occupation (21). Thus, it would be important to study further how much perceived importance of functional abilities among patients with LBP depends on occupational status and working conditions.
Our study shows that different functions vary in importance for patients with LBP. Both men and women expressed almost the same order of relative importance of these functions, which indicates a good reliability of the methods used. The most disabling functions were not perceived as those that were the most important functions in LBP patients’ daily life. One could assume that patients would perceive as more important those functions where they experienced the most difficulties or pain due to their LBP, rather than those that they can perform without difficulties. Thus, in order to obtain a more reliable and comprehensive picture of the functional capacity of patients, the overall measure could benefit from including both the scores of each individual item, as well as the relative weight of its perceived importance.
Earlier studies (9–10) have shown that the mean score of each of the 9 functional disabilities tended to increase with pain intensity, which was interpreted as a sign of good internal consistency. However, a follow-up study of patients with LBP showed that pain severity did not predict functional disability (22). This can be explained by differences in methodology used in the different studies. In the ODI questionnaire pain intensity is addressed as an independent question, but it is also built in implicitly in all the other 9 sections when asking about patient’s disabilities due to pain, as each assessed disability has been considered as a functional consequence of pain.
A small study of patients with chronic pain (5) stated that, as long as patients were able to achieve different functions important to their way of lives despite pain, this achievement was regarded as treatment success. This was supported by our findings showing that pain intensity did not correlate with the relative importance of pain or different functional abilities in LBP patients’ lives. Thus, it is possible that clinically relevant improvements in pain may lead to almost unnoticeable changes in treatment success experienced by patients with LBP if it does not improve the functions they consider to be relevant.
In the ICF Core Set study (23) only 3% of patients with LBP mentioned that sleeping was the function where they experienced the most difficulties because of back pain. On the other hand, when patients with LBP were asked to mention one severe, important and frequent activity in their lives, sleeping (or lying flat) was most commonly mentioned first (24). Similarly, in the IMMPACT survey, which included more than 500 patients with LBP, sleep-related problems were considered among the most important aspects (25). These findings corroborate our finding that sleep is one of the most important functions for patients and even a small change in ability to sleep may have a strong overall influence on everyday life.
It appears that patients’ expectations of different functions vary, with higher disability level tolerated for some functions than for others. When offered pre-defined lists of functions, determined by healthcare professionals, subjects may indicate high levels of disability or pain. However, these functions may be of low importance to them, such that the score does not necessarily indicate the handicap the patient experiences.
It has been stated that patients prefer a question format in which they are asked to define their symptoms in a time-frame of “now” or “today” (10). Our questionnaire used the time-frame of “today”. In our study the subjects who omitted some assessments stated that they had not experienced such disability that particular day. Increasing the time-frame to one week or more may have increased the completion rate. Previous studies have shown that LBP and neck pain patients can accurately recall mean pain over one week (26, 27). However, the significantly longer time-frame could have caused recall bias. In retrospective questionnaire studies there is a need to balance the occurrence of experienced disabilities and the problem of recalling the extent and severity of these events.
Our questionnaire was formed by soliciting the ODI and the VAS entities separately. This was done in order to lower the probability that by answering identical questions repeatedly, the preceding answer could direct the following one. It is possible that subjects may have had difficulties in finding an alternative from the pre-defined ODI statements, which accurately define their level of pain or functional status. This could explain the higher number of unanswered questions with the ODI than the VAS method. The sex life question was most commonly left unanswered, which is consistent with earlier studies and a reason why this question is omitted in some versions of the ODI (10).
In a previous study, the perception of significant pain was characterized by loss of function and self-management, and not by physical symptoms (5). Furthermore, patients’ criteria for treatment success, improvement or recovery were perceived by achieving functional tasks that had previously been difficult, instead of the physical measures often used by clinicians (5). These are corroborated by our findings that the level of experienced pain was not significantly correlated with the relative importance of pain.
In conclusion, development of outcome measure instruments for patients with LBP could benefit from taking into account the perceptions of patients themselves. In addition, functional measures should be weighted according to the relative importance of each function to the patients. Such outcome measure instruments could better serve the clinicians in their treatment decisions as well as research purposes.
Acknowledgements
Grants from the research funds of The Hospital District of Southwest Finland and from the Yrjö Jahnsson Foundation were received in support of this work.
References