OBJECTIVE: To develop and validate a Chinese version of the Reintegration to Normal Living Index.
DESIGN: Descriptive case-series.
SUBJECTS: Seventy-five individuals with chronic stroke and 55 age-matched healthy subjects.
METHODS: The English version of the Reintegration to Normal Living Index was translated into Chinese using standardized procedures, and then administered to both the stroke and control groups. The same instrument was administered again to the stroke subjects 1–2 weeks later.
RESULTS: The Chinese version of the Reintegration to Normal Living Index had good internal consistency (Cronbach’s α = 0.92) and test-retest reliability (intraclass coefficient = 0.87). The minimal detectable difference of the Index score was 14.8 (out of 100). Convergent validity of the Index was demonstrated by its significant association with Frenchay Activities Index (r = 0.439, p < 0.001) and Personal Wellbeing Index (r = 0.250, p = 0.033) scores among stroke subjects. The Reintegration to Normal Living Index score was significantly lower in the stroke group than in controls (p < 0.001), thus demonstrating discriminant validity. Factor analysis confirmed the two-factor structure of the Index, namely, daily functioning and perception of self.
CONCLUSION: The Reintegration to Normal Living Index is a reliable and valid tool for assessing satisfaction with community reintegration among Chinese people with chronic stroke.
Key words: cerebrovascular accident; community integration; participation; quality of life; well-being.
J Rehabil Med 2011; 43: 243–250
Correspondence address: Marco Y. C. Pang, Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Hung Hom, Hong Kong. E-mail: Marco.Pang@inet.polyu.edu.hk
Submitted June 11, 2010; accepted October 29, 2010
INTRODUCTION
Community integration involves engagement in activities in a home-like setting, the enjoyment of a social network, and involvement in productive activities (1). Individuals with stroke often experience limitations in daily functional tasks and restrictions in community activities (2). It is thus not surprising that many of these individuals express a low level of satisfaction with community reintegration after their discharge from the hospital and return to community living (3–6). For example, in a study of 45 patients with stroke carried out in the USA, Bethoux et al. (5) showed that those who had been out of the hospital for more than 6 months reported a lower degree of satisfaction with community reintegration than those who had been discharged more recently, which indicates a possible progressive decline in community reintegration over time. A study conducted in Canada found only 11% of individuals with chronic stroke to be fully satisfied with their level of community reintegration (6). According to the International Classification of Functioning, Disability and Health (ICF) model endorsed by the World Health Organization (7), activity (i.e. the execution of a task or action by an individual) and participation (i.e. involvement in a life situation) are important components of health and functioning. Considering the unsatisfactory levels of self-perceived participation in community activities reported by many stroke survivors, it is clear that community reintegration should be a key treatment outcome in this patient population (8, 9).
Stroke is the most common cause of neurological disability in Hong Kong (10). In 2008 alone, it caused more than 20,000 inpatient hospital discharges (10). A major concern is how well stroke survivors can be reintegrated into the community upon discharge from the hospital. It is also important for clinicians and administrators to know whether the interventions they provide result in any real change in perceived community reintegration. The current lack of a validated tool for measuring satisfaction with community reintegration among Chinese stroke patients makes a proper assessment of these issues difficult.
Available community integration measures in English include the 15-item Community Integration Questionnaire (1) and the 27-item Craig Handicap Assessment and Reporting Tool (11). However, the concept of community integration in these questionnaires was based on the notion of “disability” and “handicap”, rather than “activity” and “participation” as endorsed by the ICF model.
An alternative is the Assessment of Life Habits (LIFE-H), which was developed based on the concept of “participation”. However, a considerable amount of time is required to complete the questionnaire, and this may not be feasible in many clinical settings, because even the shortened version LIFE-H 3.0 contained 69 items, each of which was based on a 10-point ordinal scale (12). The ease of administration is especially relevant in community rehabilitation settings, where community reintegration is often the key indicator of treatment success/failure, but limited time is available for the clinicians to gather such important information from a large group of clients.
Other options for measuring community integration are the Community Integration Measure (13), and the Subjective Index of Physical and Social Outcome (14). Both of these scales are easy to administer and have been shown to have acceptable psychometric properties when used in patients with acquired brain injuries. However, they are not used as widely as the Reintegration to Normal Living Index (RNLI) (15). Originally developed by Wood-Dauphinee et al. (15), RNLI is an 11-item scale that evaluates satisfaction with 6 life domains following illness or trauma: mobility, self-care, activities, role within the family, comfort with relationships, and ability to handle life events. RNLI has been used in various conditions, such as stroke (3–6, 16, 17), traumatic brain injury (18), spinal cord injury (19), aneurysm (20), motor vehicle accident (21), limb amputation (22), and organ transplant (23), and in a mixed population of community-dwelling individuals with a variety of chronic conditions (24). A postal version of the RNLI is also available (25).
The RNLI has demonstrated good internal consistency and test-retest reliability (15, 25). Its construct validity is also reflected in its strong correlation with such related scales as the Spitzer Quality of Life Index (15), Frenchay Activities Index (FAI) (25), Barthel Index (25), and Short Form-36 Health Survey (25). One particular advantage of RNLI is that it involves only 11 items and takes less than 10 min to administer. It is thus considered a useful outcome measure for stroke patients in both clinical and research settings. The objectives of the study reported herein were to develop a cross-cultural adaptation of the original RNLI for use in the Chinese stroke population, and to conduct reliability and validity testing of the Chinese version of the RNLI (RNLI-C).
METHODS
Subjects
A convenience sample of individuals with stroke was recruited from local stroke self-help groups in Hong Kong and from an existing database of individuals with stroke. The inclusion criteria were: (i) a diagnosis of stroke; (ii) stroke onset of one year or longer (i.e. chronic stroke); (iii) aged 18 years or above; (iv) an Abbreviated Mental Test score of 6 or above (26); (v) community-dwelling (i.e. non-institutionalized); (vi) discharged from the hospital at least 6 months previously; and (vii) living in Hong Kong for at least one year at the time of data collection. The exclusion criteria were: (i) institutionalized; (ii) other neurological condition in addition to stroke; and (iii) another serious illness that precluded participation.
In addition, a convenience sample of age-matched healthy controls was recruited from the community through advertisements in local elderly community centres and an existing database. The eligibility criteria were the same as those for the stroke group, except for the history of stroke. The final study sample included 75 community-dwelling individuals with chronic stroke and 55 healthy controls. Ethical approval was granted by the ethics review committee of the Hong Kong Polytechnic University. Informed, written consent was obtained from each participant before the study began. All procedures were conducted in accordance with the Declaration of Helsinki.
Cultural adaptation of the Reintegration to Normal Living Index
Various methods have been used to score the RNLI. The 4-point ordinal scale (6, 13, 15, 19), 3-point ordinal scale (5, 15), and 10-cm visual analogue scale (VAS) (15) were developed by the original authors of RNLI and have been used by other researchers. A 10-point Likert Scale, and a dichotomous response scale (yes/no) were developed later by Stark et al. (24) and Daneski et al. (25), respectively. The 4-point ordinal scale (1 = does not describe my situation, 2 = describes my situation a little, 3 = describes my situation a lot, 4 = fully describes my situation) was adopted for the cross-cultural adaptation developed in this study. The 4-point scale was chosen over the 10-cm VAS or the 10-point Likert scale (15, 24) because the simplicity of the response format in the former should enable a good proportion of stroke patients to use the scale properly. While being the most simple, the dichotomous response format was not selected because it did not provide enough room for discrimination of different levels of agreement to each item and may be less responsive to change (25).
Permission was obtained from the original authors of RNLI before the initiation of the translation process. Different guidelines have been established for cultural adaptation of questionnaires (27–29). However, as recommended by the original authors, the translation process of RNLI was based mainly on the methods described by Beaton et al. (27), which were developed based on extensive review of cross-cultural adaptation in the psychological, medical, and sociological literature.
The first stage involved the forward translation of the English version of the RNLI into Chinese by two bilingual translators whose mother language is Chinese but who have different profiles. One was a physiotherapist, and the other a professionally trained translator with no background in medicine or rehabilitation. They independently produced two Chinese versions of the original RNLI.
The second stage involved a review of the two Chinese versions and the original RNLI by the two translators. The results of the translations were then collated to produce a single Chinese version of the RNLI. In the third stage, two different individuals with physiotherapy and psychology backgrounds translated the questionnaire back into the original language independently (i.e. backward translation). Both were completely blinded to the original RNLI. The purpose of this procedure was to ensure that the item content of the translation was consistent with that of the original. The forward and backward translation processes were documented carefully.
In the fourth stage, a validation committee comprising two physiotherapists with knowledge in developing measurement tools, a social worker and a clinical researcher examined the preliminary version of the questionnaire in terms of 4 areas of equivalence, namely, semantic, idiomatic, experiential, and conceptual (27). All of the committee members are bilingual individuals, with Chinese as their mother tongue, but one of them had received secondary and post-secondary education in an English-speaking country. A revised version was then pilot-tested on 5 individuals with stroke who had no prior knowledge of the original RNLI. Feedback was gathered from these individuals, on the basis of which minor modifications were made to the questionnaire to further enhance its fluency, clarity, and comprehensibility. The end result was the final version of the RNLI-C.
Validation of the Chinese version of the Reintegration to Normal Living Index
Demographics. Potential participants were first screened in telephone interviews to ensure that they fulfilled the eligibility criteria. Those eligible were then invited to a face-to-face interview during which demographic information was collected (e.g. medical history, stroke history, social history).
Chinese version of the Reintegration to Normal Living Index. Each individual was asked to rate each of the 11 items on a 4-point scale. Like the original RNLI (15), the RLNI-C has 2 subscales, with the first 8 items representing “daily functioning” and the remaining 3 “perception of self”. The scores for the items in each subscale are summed and normalized to 100 to yield the subscale score (11). Those for all items in the RNLI-C are also summed and normalized to 100 to yield the total score (15). For example, a person who obtained a score of 44/44 would be converted to a score of 100. A table for the conversion of scores was made available for the evaluator. RNLI scores lower than 60 are indicative of severe restrictions in self-perceived community reintegration, scores between 60 and 99 indicate mild to moderate restrictions, and a score of 100 indicates that the individual is fully satisfied with his or her community reintegration (3).
In the first session, a trained interviewer administered the RNLI-C to all participants in both the stroke and control groups. Approximately 1–2 weeks later, this interviewer re-administered it to the stroke group alone. This “waiting period” was intended to minimize the likelihood of participants recalling and reproducing the answers given in the first session. A time interval of 1–2 weeks is also regarded as optimal for avoiding the likelihood of significant events or life changes that may affect quality of life (30).
Frenchay Activities Index. The 15-item FAI was also administered to the stroke group in the second session to assess these individuals’ present functional status (31). The FAI was originally developed to measure the frequency with which different lifestyle activities that reflect a higher level of independence and social survival (e.g. preparing meals, performing light housework, participating in social outings) are performed (31). This index has been shown to be a reliable and valid instrument for recording pre-morbid levels of functioning and changes in the level of functioning due to stroke (31). The validated Chinese version was adopted for this study (32). Each item was rated on a 4-point scale (0: no participation, 1: less than once per week, 2: once or twice per week, 3: 3 times or more per week). Item scores were summed to provide a total FAI score for subsequent analysis.
Personal Wellbeing Index. The validated Chinese version of the Personal Wellbeing Index (PWI) was also administered to the stroke group (33) in the second session. The 7-item PWI is a generic measure of subjective well-being (33) that evaluates individuals’ level of satisfaction in 7 domains that are pertinent to a sense of personal well-being: standard of living, personal health, achievement in life, personal relationships, personal safety, community-connectedness, and future security. Each item was rated on an 11-point scale (ranging from 0 to 10), with a higher score indicating a higher level of satisfaction. The scores for each item were multiplied by a factor of 10, and then summed and averaged to yield a mean PWI score for further analysis (33).
Statistical analysis
To further explore the relationship between the characteristics of the stroke patients and community reintegration, Pearson’s correlation coefficient or Spearman’s rho were used to examine the degree of association between the RNLI-C total scores and other demographic variables (e.g. age, post-stroke duration), depending on whether the assumptions for parametric statistics were fulfilled.
Using the data obtained from the stroke group, the internal consistency of the RNLI-C was assessed by Cronbach’s alpha. The test-retest reliability of each individual item and the RNLI-C total score were tested by the Kappa statistic (κ) and intraclass correlation coefficients (ICC) (3,1) , respectively. A κ of 0.8 indicates almost perfect agreement, 0.61–0.8 substantial, 0.41–0.6 moderate, 0.21–0.4 fair, 0–0.2 slight, and < 0 poor agreement (25). An ICC > 0.75 is indicative of good reliability and 0.5–0.75 of moderate reliability (30).
The standard error of the mean (SEM) values of the RNLI-C subscale and total scores were computed using the following formula (30):
SEM = Sx √(1–rxx),
where Sx is the standard deviation (SD) of the RNLI-C total score, and rxx is the reliability coefficient.
The minimal detectable difference (MDD) values of the RNLI-C subscale and total scores were estimated using the following formula (30):
MDD = 1.96 × SEM × √2.
Confirmatory factor analysis (CFA) was performed to evaluate construct validity. CFA is a structural equation modelling technique that determines the goodness-of-fit between a hypothesized model and sample data (34). In this study, CFA was performed using Analysis of Moment Structures (AMOS), Version 17.0 (SPSS, Inc., Chicago, IL, USA) software to investigate whether the two-factor structure of the original 11-item RNLI scale (15) provided a proper model fit for our data or whether any modifications were necessary. The modification index created by AMOS provides recommendations for additions to the theoretical model, thus enhancing its goodness-of-fit statistics (35). Several goodness-of-fit indexes were examined in this study using χ2 statistics: the comparative fit index (CFI), the Tucker Lewis Index (TLI), and root mean square error of approximation (RMSEA). The criteria for an excellent model fit were: a small χ2 value with a non-significant p-value greater than 0.05, a CFI value greater than 0.95 (36), a TLI value greater than 0.95 (37), and an RMSEA value smaller than 0.05 (38).
To further assess construct validity, Pearson’s correlation coefficient was used to determine the degree of association between the RNLI-C total scores and the FAI and PWI scores (i.e. convergence). Mann–Whitney U tests were used to compare the individual RNLI-C item scores of the stroke and control groups, and an independent t-test was conducted to assess the between-group difference in the RNLI-C total score (i.e. discrimination). In addition, a receiver operating characteristic (ROC) curve was constructed to determine the tool’s ability to discriminate between the stroke and control groups. The optimal cut-off score was the highest Youden Index value (i.e. sensitivity + specificity – 1), and the corresponding sensitivity, specificity, and area under curve (AUC) were calculated. Except for CFA, all of the statistical analyses were performed using SPSS 17.0 software (SPSS, Inc., Chicago, Illinois, USA).
RESULTS
Participant characteristics
The characteristics of the participants in the stroke group are described in Table I. The majority of participants were able to walk unaided (68%) or with the use of a cane (13%) in an indoor environment, which indicates fairly good mobility. The mean RNLI-C score was 75.2 (SD = 15.0). Among the various characteristics of the participants in the stroke group, lower RNLI-score was significantly correlated with increasing age (r = –0.501, p < 0.001), number of co-morbid conditions (r = –0.342, p = 0.003), and living alone (p = –0.266, p = 0.026). Those who were widowed or had poorer functional mobility (i.e. requiring a quad cane or walker for ambulation) also had significantly lower RNLI-C score than their counterparts (p < 0.05). Only 73 and 71 of those in the stroke group completed the FAI and PWI, respectively. The mean FAI and PWI scores obtained were 25.8 (SD = 7.9) and 65.0 (SD = 13.9), respectively.
| Table I. Characteristics of the stroke group |
| Variable | |
| Basic demographics | |
| Age, years, mean (SD) | 64.4 (12.3) |
| Sex, male/female, n | 48/27 |
| Education level, none/elementary/secondary/post-secondary, n | 7/20/41/7 |
| Marital status, single/married/divorced/widowed, n | 7/51/6/11 |
| Living situation, living alone/living with someone, but usually alone/living with someone and rarely alone throughout the day, n | 10/23/42 |
| Number of co-morbid conditions, mean (SD) | 2.2 (1.5) |
| Number of medications, mean (SD) | 3.1 (2.3) |
| Stroke characteristics | |
| Number of subjects with recurrent stroke | 16 |
| Duration since the first stroke, years, mean (SD) | 5.6 (3.7) |
| Type of stroke, haemorrhagic/ischaemic/other, n | 21/51/3 |
| Side of paresis, left/right/bilateral, n | 30/41/4 |
| Mobility status | |
| Use of walking aid indoors, none/cane/quad cane/wheelchair/other, n | 51/10/7/2/5 |
| Use of walking aid outdoors, unaided/cane/quad cane/wheelchair/other, n | 25/31/8/7/4 |
| SD: standard deviation. |
Reliability analysis
The internal consistency of the RNLI-C was good, as indicated by the Cronbach’s α value (0.92). The ICCs among the items were moderate, ranging from 0.30–0.75. The deletion of any item from the questionnaire resulted in a minimal change in the Cronbach’s α value (0.91–0.92). Comparison of the scores obtained in the first and second recording sessions revealed test-retest reliability coefficients (ICC (3,1) of 0.88, 0.65, and 0.87 for the “daily functioning” subscale, “perception of self” subscale, and total scores, respectively (p < 0.001). The test-retest reliability of the individual items was further assessed by the Kappa statistic (Table II). The results indicate a moderate degree of reliability for all of the items (κ = 0.41–0.60), except for items 7 and 11, which exhibited fair reliability (κ = 0.21–0.40). The level of agreement for all 11 items between the two testing sessions was above that expected by chance (p < 0.005) The SEM values for the “daily functioning” subscale, “perception of self” subscale, and the total scores were 5.7, 9.9, and 5.4 (out of 100), respectively. The corresponding MDD values were 15.8, 27.4, and 14.8 (out of 100).
| Table II. Test-retest reliability of the Chinese version of the Reintegration to Normal Living Index scores in the stroke group |
| | Kappa statistic | p-value |
| Item (out of 4) | | |
| 1. I move around my living quarters as I feel is necessary. | 0.55 | < 0.001* |
| 2. I move around my community as I feel is necessary. | 0.60 | < 0.001* |
| 3. I am able to take trips out of town as I feel are necessary. | 0.55 | < 0.001* |
| 4. I am comfortable with how my self-care needs are met. | 0.53 | < 0.001* |
| 5. I spend most of my days occupied in a work activity that is necessary or important to me. | 0.42 | < 0.001* |
| 6. I am able to participate in recreational activities as I want to. | 0.52 | < 0.001* |
| 7. I participate in social activities with my family, friends, and/or business acquaintances as is necessary or desirable to me. | 0.30 | < 0.001* |
| 8. I assume a role in my family that meets my needs and those of other family members. | 0.43 | < 0.001* |
| 9. In general, I am comfortable with my personal relationships. | 0.45 | < 0.001* |
| 10. In general, I am comfortable with myself when I am in the company of others. | 0.45 | < 0.001* |
| 11. I feel that I can deal with life’s events as they happen. | 0.27 | 0.001* |
| | ICC (3,1) | p-value |
| Subscale (out of 100) | | |
| Daily functioning | 0.88 | < 0.001* |
| Perception of self | 0.65 | < 0.001* |
| Total score (out of 100) | 0.87 | < 0.001* |
| *p < 0.05. ICC: intraclass correlation coefficient. |
Validity analysis
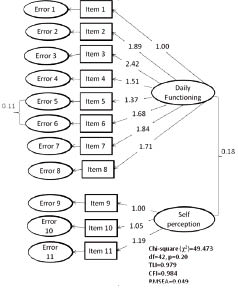
The theoretical two-factor solution (“daily functioning” and “perception of self”) (6, 14) was cross-validated on the 75 stroke participants by CFA. Fig. 1 shows the results of the final CFA model for the sample. The initial theoretical model achieved an excellent fit according to all of the goodness-of-fit statistics except the RMSEA: χ2 (degrees of freedom (df) = 43) = 56.548 (p-value = 0.081), TLI = 0.971, CFI = 0.962, and RMSEA = 0.065. The modification index suggested that a path of covariance be added between error items for items 5 (i.e. “I spend most of my days occupied in a work activity that is necessary or important to me”) and 6 (i.e. “I am able to participate in recreational activities”). The final CFA model achieved an excellent fit according to all of the goodness-of-fit statistics: χ2(df = 42) = 49.473 (p-value = 0.20), TLI = 0.979, CFI = 0.984, and RMSEA = 0.049.
Fig. 1. Final confirmatory analysis model of the Chinese version of the Reintegration to Normal Living Index (RNLI-C) scale. The model confirms the 2-factor structure of the RNLI-C, namely, daily functioning and perception of self. df: degrees of freedom; TLI: Tucker Lewis Index; CFI: comparative fit Iíndex; RMSEA: root mean square error of approximation.
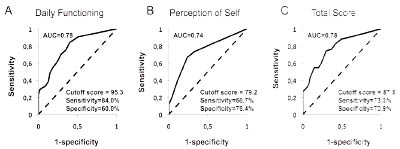
The RNLI-C scores were correlated with the FAI and PWI scores to test convergent validity, with significant moderate correlations found among the variables (Table III). The RNLI-C scores obtained from the stroke group were then compared with those from the control group (n = 55, mean age = 64.5 years, SD = 11.6) to test discriminant validity. All of the individual item, subscale, and total scores were significantly lower in the former than the latter (p < 0.001) (Table IV). ROC curves were constructed for the “daily functioning” subscale score (Fig. 2A), “perception of self” subscale score (Fig. 2B), and total score (Fig. 2C) to determine the test’s sensitivity and specificity in discriminating between the stroke patients and the controls. The respective optimal cut-off points were 95.3, 87.5, and 79.2. The AUC value ranged from 0.74 to 0.78, and the sensitivity and specificity values ranged from 66.7% to 84.0% and 60.0% to 76.4%, respectively.
| Table III. Association of Chinese version of the Reintegration to Normal Living Index (RNLI-C) scores with Frenchay Activities Index (FAI) and Personal Wellbeing Index (PWI) scores in individuals with stroke |
| RNLI-C | FAI | PWI |
| r | p | r | p |
| Daily functioning subscale | 0.471 | < 0.001* | 0.188 | 0.111 |
| Perception of self subscale | 0.280 | 0.018* | 0.363 | 0.002* |
| Total score | 0.439 | < 0.001* | 0.250 | 0.033* |
| *Indicates statistical significance (p < 0.05). |
| Table IV. Chinese version of the Reintegration to Normal Living Index (RNLI-C) scores for the stroke and control groups |
| | Stroke (n = 75) Mean (SD) | Control (n = 55) Mean (SD) | p-value |
| Item (out of 4) | | | |
| 1 | 3.5 (0.7) | 3.9 (3.1) | < 0.001* |
| 2 | 3.2 (0.8) | 3.8 (0.4) | < 0.001* |
| 3 | 2.6 (1.2) | 3.4 (0.9) | < 0.001* |
| 4 | 3.3 (0.7) | 3.8 (0.4) | < 0.001* |
| 5 | 3.0 (0.8) | 3.8 (0.6) | < 0.001* |
| 6 | 3.1 (0.8) | 3.6 (0.7) | < 0.001* |
| 7 | 2.6 (1.0) | 3.5 (0.8) | < 0.001* |
| 8 | 3.2 (0.8) | 3.6 (0.8) | < 0.001* |
| 9 | 3.2 (0.8) | 3.6 (0.5) | < 0.001* |
| 10 | 3.1 (0.8) | 3.8 (0.5) | < 0.001* |
| 11 | 2.8 (0.8) | 3.4 (0.8) | < 0.001* |
| Subscale (out of 100) | | | |
| Daily functioning | 75.3 (16.1) | 91.9 (11.1) | < 0.001* |
| Perception of self | 75.1 (16.2) | 90.0 (12.8) | < 0.001* |
| Total (out of 100) | 75.2 (15.0) | 91.4 (10.6) | < 0.001* |
| *significant between-group difference (p < 0.05). SD: standard deviation. |
Fig. 2. Receiver operating characteristic (ROC) curves of the Chinese version of the Reintegration to Normal Living Index (RNLI-C). (A) ROC curves for the “daily functioning” subscale; (B) “perception of self” subscale; and (C) total score of the RNLI-C. Their respective sensitivity, specificity, and area under curve (AUC) values are also displayed.
DISCUSSION
In this study, a Chinese version of the RNLI (RNLI-C) has been developed to measure satisfaction with community reintegration among individuals with stroke. It has also been shown to demonstrate good psychometric properties when used in the Chinese stroke population in Hong Kong.
Development of Chinese version of the Reintegration to Normal Living Index
A poor translation process may lead to a questionnaire that is not equivalent to the original and hence, erroneous comparisons of results cross different translated versions (27). Therefore, we used the established guidelines described by Beaton et al. (27) in the translation process. In both our forward and backward translation processes, more than one person was involved, which reduced the possibility of introducing bias into the preliminary version (29). Additionally, for the forward translation, the first translator was aware of the concepts being examined in RNLI. She may thus provide a more clinical perspective and may offer a translation that has more reliable equivalence from a measurement point of view (27). The other translator, in contrast, was not aware of the concepts being examined in the RNLI and had no clinical background. She may have provided a translation that better reflects the language used by that population and may be more likely to detect ambiguous meanings in the original questionnaire (29). Moreover, both backward translators were blinded to the original questionnaire, thereby avoiding information bias in the backward translation process (27). In addition to the forward and backward translators, an expert committee was also involved to examine the source and translated questionnaires. This was to ensure that the test version of the questionnaire achieved cross-cultural equivalence (27).
Level of satisfaction with community reintegration
Only 4 individuals (5%) with stroke indicated complete satisfaction with their community reintegration, with 14 individuals reporting severe restrictions in such reintegration. Our results are thus consistent with those of other studies on chronic stroke populations, which have reported a comparable RNLI score (5, 6). Difficulty with community reintegration remains a major concern for individuals with chronic stroke. A multitude of factors may underlie the suboptimal RNLI-score. As shown by our results, advancing age, widowed and living alone, co-morbidity, and poor functional mobility may contribute to limitations in reintegrating to community living. Although publicly funded hospital-based rehabilitative service for stroke patients are available, the mean length of stay in inpatient rehabilitation facilities is only 3 weeks (39). Those who are severely impaired would typically be placed in private nursing homes. While some patients may be referred by the physicians to undergo community rehabilitation after discharge, the duration of treatment is also limited (2–3 months) (39). Therefore, the patients often have not attained an optimal level of functioning when they return to community living. Moreover, the environment in Hong Kong also poses additional challenge to the stroke survivors. Hong Kong is a densely populated, fast-paced metropolitan city, with crowded, narrow streets and heavy traffic. A good proportion of buildings and facilities are still wheelchair inaccessible. These factors may discourage people with disabilities from venturing out and participating in community activities.
Reliability of the Chinese version of the Reintegration to Normal Living Index
The Cronbach’s α value obtained in this study (0.92) is very similar to that obtained in the original RNLI (15), which indicates that participants’ responses were consistent across the items and that all items were measuring the same attribute. Furthermore, there was a negligible change in the α coefficient value when any one of the items was deleted, which indicates strong item consistency and suggests that none of the items decreased scale stability.
The RNLI-C also demonstrated good test-retest reliability, as reflected by the high ICC value (0.87). Although two items (item 7: “I participate in social activities with my family, friends and/or business acquaintances as is necessary or desirable to me”; item 11: “I feel that I can deal with life events as they happen”) displayed only fair agreement, it is important to focus on the reliability of the scale as a whole (40). In addition to measurement error, there are several potential explanations for the modest reliability observed for these two items. First, the discrepancy between the scores for the first and second testing sessions may reflect changes in the participants’ perceived level of community reintegration. It cannot be ruled out that some significant event occurred in the two-week interval between testing sessions that affected the ratings. Secondly, the discrepancy may be related to the content of the items themselves. For example, item 11 involves a more abstract concept than the other items in the scale, such as item 1 (“I move around my living quarters as I feel is necessary”), which is more concrete. This explanation may also be applicable to the greater reliability exhibited by the “daily functioning” subscale (ICC = 0.88) relative to the “perception of self” subscale (ICC = 0.65).
SEM and MDD values were also established for the RNLI-C. The MDD represents the smallest difference that would reflect a real change in the RNLI-C score (30). The values established here will be useful in helping future intervention studies to determine whether the experimental treatment has induced any real change in satisfaction with community reintegration among individuals with chronic stroke.
Validity of the RNLI-C
CFA was used to examine the factor structure of the RNLI-C. The findings of this analysis revealed two primary domains of the RNLI-C (i.e. “daily functioning” and “perception of self”), which is consistent with previous research on the original RNLI (15). CFA yielded this two-factor structure, and suggested that each factor may be considered independently when scoring the RNLI-C, as the correlation between the two is weak (0.18). A recent study carried out by Stark et al. (24), however, showed the RNLI to have two factors that can be designated as “social” (items 6–11) and “physical” (items 1–5). There are several explanations for this discrepancy in factor structure. First, the sample characteristics were different in the two studies. The present study included only individuals with chronic stroke, whereas Stark et al. (24) included individuals with mixed conditions (cerebral palsy, multiple sclerosis, stroke). Secondly, we administered the RNLI-C by interviewing each subject, whereas they used different methods of questionnaire administration (postal survey, personal interviews). Thirdly, we used a 4-point scale, whereas they used a 10-point Likert-type scale. Finally, the two studies adopted different methods of factor analysis, CFA in this study and principal component analysis in theirs (24).
Convergent validity is reflected in the significant associations between the RNLI-C and the FAI and PWI. A previous study also reported a significant correlation between the RNLI and FAI (r = 0.69) (25). It is not surprising that the RNLI-C and FAI are correlated because certain items in the two scales measure similar concepts. For example, items 1–3 of the RNLI-C (Appendix I) and items 8 (“walking outside for > 15 minutes”) and 11 (“travel outing/car ride”) of the FAI are linked to the concept of “walking and moving and moving around using transportation” in the ICF model (category d450–d469) (7). Furthermore, both item 6 of the RNLI-C and item 9 (“actively pursuing a hobby”) of the FAI measure the underlying concept of “recreation and leisure” (category d920 in the ICF) (7). The FAI exhibited stronger correlation with the “daily functioning” subscale of the RNLI-C than with the “perception of self” subscale, whereas the PWI was more strongly correlated with the latter. Its greater association with the “perception of self” subscale is probably because this subscale contains items that measure individuals’ degree of satisfaction with personal relationships and their ability to handle future events, which is in accord with two of the domains evaluated in the PWI: personal relationships and future security.
Our results also demonstrate the good discriminant validity of the RNLI-C. First, the subscale and total scores in the stroke group were significantly lower than those in the control group. Secondly, ROC analysis demonstrated the RNLI-C’s ability to distinguish differences in satisfaction with community reintegration between the two groups. In light of the CFA results and convergent and discriminant validity analysis, it is reasonable to conclude that the RNLI-C displays good construct validity in measuring satisfaction with community reintegration among individuals with chronic stroke.
Limitations and future research directions
This study has several limitations. First, few of the participating stroke survivors had severely impaired mobility. The results are thus generalizable only to individuals who are moderately or mildly affected by stroke. In Hong Kong, however, stroke survivors with very severe mobility impairment (i.e. wheelchair-dependent) tend to be institutionalized. Our sample is thus quite representative of community-dwelling individuals with chronic stroke in Hong Kong.
Secondly, the RNLI-C was administered twice within 1–2 weeks, which is quite a short time-period. We could not rule out the possibility of memory bias, which may affect the results of the reliability analysis.
Thirdly, those who had substantial cognitive deficits were excluded from this study. Therefore, the RNLI-C was administered only to the patients themselves, but not to their significant others. However, for those stroke survivors who had more severe cognitive and communication disorders, administering the RNLI-C to the patients’ significant others, who are knowledgeable about the patients’ health status, may be a viable alternative (15–16). The original authors of RNLI reported adequate inter-rater reliability of scores between the patients and significant others (15). In contrast, an Australian study has shown the degree of reliability between the RNLI scores of stroke patients and their significant others to be poor (16). The reliability of scores between stroke patients and significant others on the RNLI-C in the Hong Kong context requires further study.
Conclusion
In conclusion, the RNLI-C is a reliable and valid tool for evaluating satisfaction with community reintegration in individuals with chronic stroke.
REFERENCES