OBJECTIVE: To determine the effects of lumbar extension exercise on strength, disability index, and pain scores in patients after lumbar discectomy surgery.
DESIGN: Prospective comparative study.
SUBJECTS: Forty patients experiencing a herniated disc at lumbar levels were divided into 4 subgroups for different training frequencies: twice/week (group 1), once/week (group 2), once/2 weeks (group 3), and no training (control).
METHODS: After completing the initial 12-week training, all subjects participated in a 12-week follow-up training.
RESULTS: Groups 1 and 2 showed significant increases in lumbar extension strength (26 Nm and 7 Nm, respectively), while group 3 and the control group showed significant decreases in lumbar extension strength. Groups 1 and 2 showed significant decreases in disability index (1.4 and 0.8 Oswestry Disability Index points, respectively), and group 1 showed significant decreases in back and leg pain scores (both 0.5 units on a 10-cm visual analog scale).
CONCLUSION: Lumbar extension strength and disability index improve with training frequencies of once and twice per week, while back and leg pain improve with a training frequency of twice per week. The clinical importance of these improvements is questionable, as the scores were already very low after the discectomy and the magnitude of absolute improvements were small.
Key words: training frequency; lumbar extension strength; disability; pain.
J Rehabil Med 2010; 42: 839–845
Correspondence address: Jae Kun Shim, Department of Kinesiology, Neuroscience and Cognitive Science Program, Fischell Department of Bioengineering, University of Maryland, College Park, MD 20742, USA. E-mail: jkshim@umd.edu
Submitted December 14, 2009; accepted July 8, 2010
INTRODUCTION
Previous studies on the epidemiology of back pain have indicated that approximately 80% of people experience back pain during their lifetime (1, 2). Weber showed that patients who underwent lumbar discectomy surgery experienced less pain and greater mobility sooner than those treated conservatively (3). Lumbar disc herniation is often treated with surgical procedures followed by postoperative rehabilitation. It has been reported that lumbar discectomy surgery provides excellent results, with a success rate of approximately 90%, when followed by rehabilitation in the early postoperative phase (4–6). However, if rehabilitation is not performed within 11 years following lumbar surgery, the success rate decreases to 60–90% (4, 7). Approximately 80% of operated patients return to work 12 months after surgery, whereas the remaining 20% do not (8). Other studies have documented that 10–40% of operated patients experience adverse symptoms, such as pain and motor deficit (9, 10). If patients still experience persistent unfavorable symptoms, active rehabilitation programs are suggested as postoperative treatments (4).
A lumbar extension exercise program has been considered to be beneficial for strengthening the lumbar extensors and improving postoperative outcomes in lumbar discectomy surgery patients. Several types of postoperative rehabilitation programs have been used in previous studies. It appears that intensive exercise provides better results than mild exercise for the purpose of postoperative rehabilitation. Studies on short-term intensive rehabilitation programs up to 6 weeks post-operation showed that intensive strength training programs were beneficial for the patients. The intensive exercise allowed patients to return to work after a shorter period of time (11–14). Most studies examining the training effects of postoperative rehabilitation employed training periods of less than 3 months. Thus, evidence for the efficacy of long-term training programs following lumbar discectomy surgery is lacking. It is well known that exercise frequency is critical for a training program, and previous studies have systematically investigated the effectiveness of training programs under different training frequencies in non-patient groups (15–19). However, to our knowledge, there is no study examining the effect of postoperative training frequency on rehabilitation outcomes of patients recovering from discectomy surgery over longer periods of training. Thus, the necessary training frequency to improve or maintain the lumbar strength and other rehabilitation outcomes in the long-term postoperative rehabilitation phase is unknown.
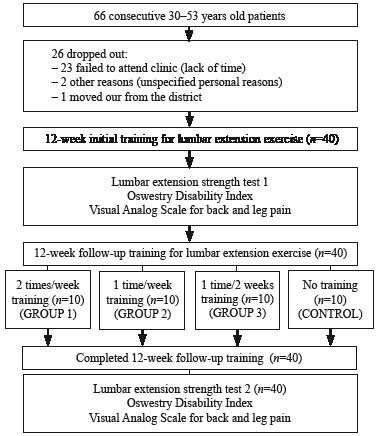
The objective of this study was to determine how performing lumbar extension exercise at different training frequencies affects lumbar extension strength, disability scores, and pain scores in patients recovering from lumbar discectomy surgery (Fig. 1). After receiving the 12-week initial training, all patients were divided into 4 groups so that the mean values of the test scores of each group were similar. Each group received different training frequencies for the next 12-week post-training: twice a week, once a week, once per 2 weeks and no training at all. The lumbar extension strength, disability, and pain were tested before and after the 12-week post-training. We hypothesized that different training frequencies would be associated with different rehabilitation outcomes of lumbar extension strength, disability scores, and pain scores.
Fig. 1. Patient assignment.
METHODS
Subjects
The inclusion criteria for subjects in this study were male patients with traumatic herniated disc injuries at different lumbar levels (L4–S1). Each subject had symptoms for at least 10 months before having discectomy surgery. Immediately following 6 weeks of rest post-operation, subjects participated in a 12-week isokinetic lumbar extension training program provided by a MedX system (Ocala, FL, USA; Fig. 2). After the initial 12-week lumbar extension training, each subject underwent lumbar extension strength testing and completed the Oswestry Disability Index (ODI), and visual analog scale (VAS) for back and leg pain intensity. Following these tests, subjects were divided into 4 subgroups so that the mean values of their test scores and physical characteristics were similar for the follow-up lumbar training protocols with different training frequencies (group 1: twice a week; group 2: once a week; group 3: once every 2 weeks and control group: no training) (Table I). For the subgroup assignment, we ran an optimization procedure in MatLab (MatLAB 7, MathWorks, Inc., MA, USA) with the cost function that minimizes differences in ODI scores, VAS scores, age, height, and body mass between groups and found the compositions of subjects for each group. Although we did not preset any criteria for exclusion, each group had 10 patients before the follow-up training. Physical characteristics, ODI, VAS and strength levels of the subjects were not statistically different across the groups. Subjects in each group were not aware of what training protocols other groups were following. The University’s Institutional Review Board (IRB) approved the procedures of this study and all subjects (n = 66) gave informed consent.
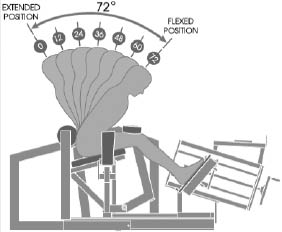
Fig. 2. Lumbar positions on the MedX training system.
| Table I. Subject characteristics (n = 40) |
| Variables | Group 1 (n = 10) | Group 2 (n = 10) | Group 3 (n = 10) | Control group (n = 10) | p-value |
| Age (years) | 39.00 ± 2.26 | 41.60 ± 1.63 | 41.70 ± 1.85 | 41.90 ± 1.55 | 0.649 |
| Height (cm) | 175.21 ± 1.92 | 172.96 ± 1.53 | 174.32 ± 2.08 | 173.37 ± 1.87 | 0.831 |
| Body mass (kg) | 76.66 ± 2.57 | 74.86 ± 2.58 | 78.25 ± 1.89 | 73.32 ± 2.32 | 0.488 |
| Duration of low back pain (month) Duration of leg pain (month) Back pain VAS before operation (cm) Leg pain VAS before operation (cm) ODI before operation (%) | 17.10 ± 1.43 9.10 ± 0.80 7.70 ± 0.42 8.50 ± 0.34 85.20 ± 2.46 | 15.00 ± 1.06 7.70 ± 0.82 7.90 ± 0.38 8.50 ± 0.27 84.10 ± 2.38 | 17.30 ± 0.76 9.60 ± 0.65 7.60 ± 0.40 8.60 ± 0.31 83.80 ± 2.27 | 18.40 ± 1.21 9.20 ± 0.70 7.70 ± 0.45 8.70 ± 0.30 84.28 ± 1.09 | 0.219 0.309 0.964 0.960 0.972 |
| Location of the prolapsed disk (right/left/central), n | 5/4/1 | 5/2/3 | 4/4/2 | 5/5/0 | |
| Level of herniated disc (L4-L5/L5-S1), n | 6/4 | 5/5 | 4/6 | 4/6 | |
| Operation type (ELD/OLM), n | 6/4 | 5/5 | 6/4 | 5/5 | |
| Values are mean ± SEs (standard errors). p-values are from analysis of variance results. VAS: visual analog scale; ODI: Oswestry disability index; ELD: endoscopic laser discectomy; OLM: open laser microdiscectomy. |
Interventions
After the discectomy operation, all patients had 6 weeks of rest. They were advised to avoid lifting, back bending, and carrying heavy objects during this period. At the end of the rest period, all subjects started an initial 12-week lumbar extension training program: twice per week with isokinetic exercise (24º/s). The isokinetic training consisted of 2 sets of 15–20 repetitions (Fig. 2). Throughout the initial training program, subjects were asked to produce maximum torque on the MedX machine for concentric and eccentric lumbar extension for each repetition. The lower body, including the hip, thighs, shanks, and feet, were all mechanically fixed to the MedX machine with Velcro straps. During the exercise, the subjects were asked to cross their arms on the chest and move the upper body as if it was a single rigid body in such a way that the head and the upper extremities would be moving with the trunk.
After completing the initial 12-week training, all subjects participated in a 12-week follow-up training, which had similar protocols to the initial training. Subjects were assigned to 1 of 4 groups: group 1, group 2, group 3, or control group. The subjects were advised to avoid any other physical activities that might influence lumbar extension strength, disability and pain over the entire training period. Although the subjects were instructed to avoid regular strength training, carrying heavy objects, or aquatic exercises (20), they were encouraged to continue their routine daily living activities, such as walking, shopping, cooking, house working, etc.
Outcome measurements
Lumbar strength, subjectively perceived functional impairment, and pain were quantified as outcome measurements. The orders of these tests were balanced across all subjects.
Lumbar extension strength. The test was performed before and after the follow-up training period. All subjects completed 2 isometric lumbar extension strength tests on 2 separate days. The testing dates were separated by at least 72 h to allow subjects enough time to recover from any residual fatigue or soreness associated with prior testing (16, 18, 21, 22). Prior to testing, the subjects completed 2–3 practice sessions to become familiar with the testing equipment and procedure. After the familiarization sessions, maximum isometric lumbar extension torque was measured to estimate the isometric lumbar extension strength. For each isometric test, subjects were seated and secured in the MedX machine. Subjects were then asked slowly to increase the lumber extension torque over 5 s. Once they reached the maximum torque, they were instructed to slowly reduce the torque. A 5-min rest period was provided between angle conditions. The results of the 2 tests were averaged and used as reference values. The isometric lumbar extension strength was measured using a MedX lumbar extension machine at 7 angular positions of the upper body, which included 72º, 60º, 48º, 36º, 24º, 12º, and 0º of the trunk angle (Fig. 2). Subjects were positioned sitting upright in the equipment according to the procedure described in previous research (22–25). Previous studies showed that this equipment was highly reliable (r = 0.94–0.98) and valid for the quantification of isometric lumbar extension strength (16, 22). The orders of angles were balanced across all subjects.
Oswestry Disability Index score and visual analog scale value. The ODI and VAS were recorded before the initial training and follow-up training. The Oswestry Low Back Pain Disability Questionnaire is used to monitor subjectively perceived functional impairment in post-operated lumbar discectomy patients. The percentage disability determined from the questionnaire was then assessed on the ODI with increasing disability levels, represented in 20% increments. The results are characterized into 5 categories – minimal disability, moderate disability, severe disability, crippled, and exaggerating symptoms (26). The VAS is used to measure a perception or sensation that cannot easily or directly be measured. In this study, the VAS assessed the amount of subjectively perceived pain across a pain continuum from none to extreme pain. Patients indicate pain levels by marking a point on the horizontal 10-cm scale. Pain levels are characterized into 6 categories, each with 2-cm increments – no pain, mild pain, moderate pain, severe pain, very severe pain, and worst possible pain (27).
Statistical analysis
All values are expressed as means and standard errors (SEs). The mean strength values calculated over all angles were quantified. The raw values of the lumbar strength, ODI scores, and VAS scores were first quantified. The raw values of each subject were normalized by the baseline mean value of the group to which the subjects belonged (28). The normalization was performed while dividing test values collected both before the follow-up training and after the follow-up training by the mean values calculated from the follow-up training for each group. This procedure was performed to ensure that the baseline mean values of each group were not different across groups. Two-way repeated measures analysis of variance (ANOVA) was performed with a cross-classified random effects model: the within-subject factor of Period (2 levels: before and after the follow-up training) and the between-subject factor of Group (4 levels: group 1, group 2, group 3 and control group). The critical value for significant difference was set at a = 0.05. Bonferroni corrections were used for multiple comparisons.
RESULTS
Lumbar extension strength
The isometric strength values at each angle (i.e. 72º, 60º, 48º, 36º, 24º, 12º and 0º) and mean values over all angles before and after the follow-up training are shown in Table II. Groups 1 and 2 showed increases in lumbar extension strength after the follow-up training at each angle, while group 3 and the control group showed decreases. These findings were supported by a 2-way repeated measures ANOVA with factors of Group and Period. There were statistically significant Period effects for each angle: 0º (F[1,36] = 35.40, p < 0.001), 12º (F [1,36] = 14.06, p < 0.01), 24º (F [1,36] = 4.53, p < 0.05), 36º (F [1,36] = 12.88, p < 0.01), 48º (F [1,36] = 11.48, p < 0.01), 60º (F [1,36] = 6.22, p < 0.05) and 72º (F [1,36] = 4.64, p < 0.05). Significant Group × Period interactions were also found at each angle: 0º (F [3,36] = 170.77, p < 0.001), 12º (F [3,36] = 97.91, p < 0.001), 24º (F [3,36] = 73.50, p < 0.001), 36º (F [3,36] = 85.94, p < 0.001), 48º (F [3,36] = 109.49, p < 0.001), 60º (F [3,36] = 93.58, p < 0.001) and 72º (F [3,36] = 85.88, p < 0.001). Group effect was not statistically significant: 0º (F [3,36] = 0.95, p = 0.426), 12º (F [3,36] = 1.48, p = 0.235), 24º (F [3,36] = 1.39, p = 0.260), 36º (F [3,36] = 1.39, p = 0.262), 48º (F [3,36] = 1.31, p = 0.287), 60º (F [3,36] = 1.50, p = 0.231) and 72º (F [3,36] = 1.48, p = 0.237).
| Table II. Isometric lumbar extension strength values (Nm) at 7 trunk angles and averaged values over all angles before and after the 12-week follow-up training |
| Group | Angle (degrees of lumbar flexion) | |
| 0º | 12º | 24º | 36º | 48º | 60º | 72º | Meanº |
| Group 1 (n = 10) | *** | *** | *** | *** | *** | *** | *** | *** |
| Pre-training strength (Nm) | 174.74 ± 10.31 | 197.10 ± 9.10 | 216.32 ± 10.05 | 235.77 ± 10.63 | 247.06 ± 10.34 | 257.61 ± 10.41 | 264.82 ± 10.13 | 227.63 ± 5.20 |
| Post-training strength (Nm) | 196.11 ± 11.19 | 223.23 ± 9.14 | 245.02 ± 11.76 | 257.45 ± 11.88 | 274.74 ± 11.84 | 287.28 ± 13.14 | 297.35 ± 12.70 | 254.45 ± 5.84 |
| Rate of increase, % | +12.40 | +13.56 | +13.21 | +9.15 | +11.19 | +11.34 | +12.28 | +11.78 |
| Group 2 (n = 10) | * | ** | * | ** | ** | *** | ** | *** |
| Pre-training strength (Nm) | 168.53 ± 13.01 | 196.35 ± 11.31 | 215.99 ± 11.04 | 226.11 ± 10.98 | 236.52 ± 11.60 | 245.99 ± 11.62 | 258.10 ± 12.23 | 221.08 ± 5.44 |
| Post-training strength (Nm) | 172.10 ± 13.93 | 203.63 ± 10.73 | 223.79 ± 11.28 | 237.04 ± 12.14 | 243.77 ± 12.23 | 252.96 ± 11.79 | 265.86 ± 11.77 | 228.45 ± 5.61 |
| Rate of increase, % | +1.84 | +4.00 | +3.73 | +4.74 | +3.02 | +2.86 | +3.01 | +3.33 |
| Group 3 (n = 10) | *** | *** | *** | *** | *** | *** | *** | *** |
| Pre-training strength (Nm) | 169.96 ± 12.82 | 199.93 ± 12.23 | 218.48 ± 12.23 | 229.97 ± 12.79 | 243.68 ± 12.97 | 252.55 ± 13.65 | 263.54 ± 13.46 | 225.44 ± 5.89 |
| Post-training strength (Nm) | 157.84 ± 12.03 | 178.66 ± 13.25 | 201.74 ± 13.40 | 208.64 ± 13.86 | 222.54 ± 12.61 | 233.75 ± 12.77 | 244.99 ± 13.44 | 206.88 ± 5.83 |
| Rate of increase, % | –7.13 | –11.20 | –8.06 | –9.72 | –8.82 | –7.46 | –7.04 | –8.24 |
| Control group (n = 10) | *** | *** | *** | *** | *** | *** | *** | *** |
| Pre-training strength (Nm) | 177.93 ± 7.12 | 196.65 ± 10.32 | 216.58 ± 10.83 | 232.38 ± 10.66 | 249.29 ± 10.39 | 257.05 ± 10.55 | 265.70 ± 11.04 | 227.94 ± 5.17 |
| Post-training strength (Nm) | 143.54 ± 7.99 | 164.31 ± 8.33 | 183.31 ± 8.93 | 201.64 ± 9.36 | 218.13 ± 9.11 | 225.08 ± 10.30 | 230.06 ± 10.40 | 195.15 ± 4.95 |
| Rate of increase, % | –19.75 | –16.36 | –15.28 | –13.18 | –12.46 | –12.57 | –13.41 | –14.38 |
| Values are mean ± standard errors. Statistically significant Period effect *p < 0.05; **p < 0.01; ***p < 0.001. |
The normalized strength values indicated that group 1 and group 2, respectively, showed 11.8% (from 228 Nm to 254 Nm) and 3.3% (from 221 Nm to 228 Nm) significant increases in isometric strength values, after the follow-up training, while group 3 and the control group, respectively, showed 8.2% (from 225 Nm to 207 Nm) and 14.4% (from 228 Nm to 195 Nm) significant decrease in strength. These findings were supported by a 2-way repeated measures ANOVA with Group and Period factors, which showed statistically significant effects of Period (F [1, 276] = 65.66, p < 0.001), Group (F [3, 276] = 5.79, p < 0.01), and Group × Period interaction (F [3, 276] = 638.15, p < 0.001). It is to be noted that the increase in absolute strength values was relatively small in Group 2, although it was statistically significant in normalized values.
Oswestry Disability Index score and visual analog scale value
The ODI scores and VAS values of back and leg pain before and after the follow-up training are presented in Table III.
| Table III. Mean ODI scores and VAS values in before and after the 12-week follow-up training |
| | Group 1 (n = 10) | Group 2 (n = 10) | Group 3 (n = 10) | Control group (n = 10) |
| ODI (0–100%) | * | * | | |
| Pre-training score (%) | 10.8 ± 0.74 | 10.4 ± 0.83 | 10.4 ± 0.71 | 9.8 ± 1.05 |
| Post-training score (%) | 9.4 ± 0.85 | 9.6 ± 0.65 | 9.8 ± 0.63 | 10.4 ± 0.72 |
| Rate of increase, % | –13.0 | –7.7 | –5.8 | +6.1 |
| Back pain VAS (0–10 cm) | * | | | |
| Pre-training score (cm) | 1.0 ± 0.21 | 0.9 ± 0.23 | 0.9 ± 0.28 | 1.0 ± 0.26 |
| Post-training score (cm) | 0.5 ± 0.22 | 0.6 ± 0.16 | 0.8 ± 0.25 | 1.3 ± 0.30 |
| Rate of increase (%) | –50.0 | –33.4 | –11.1 | +30.0 |
| Leg pain VAS (0–10 cm) | * | | | |
| Pre-training score (cm) | 0.9 ± 0.18 | 0.8 ± 0.25 | 0.8 ± 0.25 | 0.9 ± 0.23 |
| Post-training score (cm) | 0.4 ± 0.22 | 0.5 ± 0.17 | 0.7 ± 0.21 | 1.1 ± 0.23 |
| Rate of increase, % | –55.6 | –37.5 | –12.5 | +22.2 |
| Values are mean ± standard errors *Statistically significant Period effect (p < 0.05). ODI: Oswestry disability index; VAS: visual analog scale. |
Groups 1 and 2, respectively, showed 13.0% (from 10.8 to 9.4) and 7.7% (from 10.4 to 9.6) significant decreases in ODI scores, after the follow-up training. Other groups did not show significant increases or decreases. These findings were supported by the 2-way repeated measures ANOVA with Group and Period factors, which showed statistically significant effects of Period (F [1, 36] = 4.80, p < 0.05) and Group × Period interaction (F [3, 36] = 3.03, p < 0.05). Group effect was not statistically significant (F [3, 36] = 0.31, p = 0.820). It is to be noted that the improvement of absolute ODI scores in both group 1 and group 2 were relatively small in their magnitudes, although statistically significant.
Group 1 showed 50.0% (from 1.0 to 0.5) significant decrease in back pain VAS values after the follow-up training, although other groups did not show statistically significant changes. These findings were supported by the 2-way repeated measures ANOVA with Group and Period factors, which showed statistically a significant effect of Period (F [1, 36] = 4.50, p < 0.05) and Group × Period interaction (F [3, 36] = 5.20, p < 0.01). Group effect was not statistically significant (F [3, 36] = 0.50, p = 0.683). Leg pain VAS values showed similar trends. Group 1 showed 55.6% (from 0.9 to 0.4) significant decreases in leg pain VAS values after the follow-up training, although other groups did not show statistically significant changes. These findings were supported by the 2-way repeated measures ANOVA with Group and Period factors, which showed a statistically significant effect of Period (F [1, 36] = 6.41, p < 0.05) and Group × Period interaction (F [3, 36] = 4.19, p < 0.05). Group effect was not statistically significant (F [3, 36] = 0.46, p = 0.709). It is also to be noted that the improvements in absolute VAS values in group 1 are small, although statistically significant.
DISCUSSION
Training frequency is one of the main considerations of strength training for rehabilitation efficacy. A low training frequency can easily yield no increase in strength, or even a decrease. On the other hand, high-frequency training may cause an increased risk of injury (17). Thus, it is critical to find an optimal training frequency that allows for the maintenance or increase of strength for a particular group of trainees. The optimal training frequency varies between groups of trainees with different physical characteristics and medical conditions or histories. Specifically, the optimal training frequency for those who have medical conditions may be different from non-patient groups, and the optimal training frequency found in the non-patient groups may not necessarily be applied to patient groups (4, 8, 15–17, 23, 29).
Previous studies examining the effect of lumbar strength training in non-patient groups showed that training frequency had a large influence on training outcomes. Graves et al. (17) investigated 4 different training frequencies (once every 2 weeks, once every week, twice every week, and 3 times every week) in non-patient groups regarding lumbar extension strength. Surprisingly, this study showed that the 4 groups training for 12 weeks, each with different training frequencies, did not have a significant difference in lumbar extension isometric strength. However, our study clearly showed that lumbar strength training protocols with different training frequencies are associated with differential rehabilitation outcomes. Carpenter et al. (23) investigated the effectiveness of a 20-week training period with the same training frequency conditions as Graves’. This study showed that there was a slight increase in the lumbar extension strength between the 12th week and 20th week. These results indicated that lumbar extensors experienced training adaptations that were somewhat different from other muscle groups that reported to be optimally trained with a minimum training frequency of 3 times a week (30). Tucci et al. (16) used similar training protocols as those used in our study. They investigated the effects of 12-week reduced training (once every 4 weeks and once every 2 weeks) and detraining (i.e. no training) on lumbar extension strength after a 10–12-week initial training period (1–3 time(s) per week). They found that groups undertaking reduced training maintained lumbar extension strength after the detraining period.
Patients recovering from lumbar disc hernia experience a decrease in lumbar flexion, extension, and rotational strength, in muscular power and endurance, and in spinal mobility. These patients also suffer from paraspinal muscle feed-forward control impairments, from elevated levels of pain and depression, and from interferences with activities of daily living (2, 6, 31–34). Previous studies have recommended strength training, stability ball training, physical therapy, and stretching as effective rehabilitation methods to patients recovering from low back pain and discectomy surgery (4, 34–36). Alternatively, as in our study, other studies investigating the effects of strength training in patients after a discectomy have suggested that strength training is an effective method for rehabilitation. Kjellby-Wendt & Styf (12) showed that the early active training group, compared with the control group, had a significant decrease in pain 6–12 weeks after surgery. It was also found that this group’s range of motion in the lumbar spine was increased, more than the control group, 12 weeks after surgery. Manniche et al. (13) provided both high- and low-intensity exercise programs to discectomy patients and found that high-intensity exercise was more beneficial regarding disability index and work capabilities, which were tested at 26-week and 1-year follow-ups.
Choi et al. (8) recently compared the efficacy of intensive exercise (lumbar training, limb training, and aerobic exercise) and home-based lumbar conditioning exercise. The home-based exercise group showed an 18% increase in lumbar extension strength after 12 weeks, while the intensive exercise group showed a 52% increase. Hakkinen et al. (4) investigated the effects of strength training and stretching exercises in discectomy patients across 12 months. All patients were instructed to perform stabilization exercises and stretching, while a portion of the subjects were grouped and instructed to perform additional strengthening exercises. After 2 months, there was a slightly greater improvement in strength and endurance of the trunk muscles for patients who performed the additional strength exercises. At the 12-month follow-up, all subjects significantly increased trunk muscle strength and spine mobility. The improvements were the same regardless of whether subjects were instructed to perform additional strength exercises. Conversely, a recent study by Helmhout et al. (36) showed that there was little difference between the lumbar extension strength exercise and physical therapy with aerobic exercise.
Few studies have investigated the effect of strength training frequency on the rehabilitation of patients recovering from lumbar discectomy or low back pain. Rainville et al. (37) examined the effect of training volume for patients with moderate spinal pain levels. Patients received an aggressive supervised 2-hour training either 2 or 3 times a week for 6 continuous weeks followed by a 12-month follow-up. They found similar results for flexibility, strength, and pain for patients undergoing rehabilitation either 2 or 3 times per week. Despite Rainville et al.’s (37) and other studies (2, 4) showing strength training delivered 2 or more times a week to be equally effective, our study found that as little as once per week strength training can improve patients’ lumbar extension strength and disability scores, while 2 times a week was necessary to improve pain scores. Apart from physical and subjective pain measures, the results also have implications for time and medical cost minimization regarding the maintenance or improvements in rehabilitation outcomes. At a time when medical costs are high and time is a commodity, minimizing both can be an attractive option. Limke et al. (15) provided 2 different volumes of strength training (1 set vs 2 sets) to patients with chronic low back pain. After 6 weeks of strength training, different tests were performed: strength in the back, progressive isoinertial lifting evaluation, disability index score, and pain value. The results showed that there was no significant difference in these measures between 2 different training volumes.
It is recommended that lumbar disectomy patients strength train at least once every week in order to maintain or increase lumbar strength. Our study showed that increasing the training frequency from once to twice per week was more effective for lumbar extention strength and subjectively perceived disability and pain. During the initial training, the patients may have achieved imporvements of lumbar strength, perceived disability and pain. After the follow-up training, however, group 3 and the control group showed deterioration or no changes in these scores. It appears that the frequencies of no training and once per 2 weeks were not enough to maintain the continuous effects of the initial training with the frequency of twice per week. In other words, the patients probably did not undergo enough training overloads after the reduction in training frequencies. It is still unknown how the training frequency will affect the rehabilitation outcomes of lumbar discectomy patients over extended training periods.
Limitations of the study. We examined the effect of 3 different frequencies of lumbar extension training (twice a week, once a week, and once every 2 weeks). However, other factors that are also critical for training outcomes, such as training modality and intensity, were not considered in the current study. Follow-up studies are needed to investigate the influences of training modality and intensity of lumbar extension training. In addition, we examined the influence of varying training frequencies on strength and pain in lumbar discectomy patients. There are other functional measures, such as endurance, flexibility and lifting capacity, which may be considered for a more comprehensive overview of the recovery process after lumbar discectomy surgeries. Although there were statistically significant percentage improvements in the ODI and VAS scores through training, in some cases greater than 50%, the clinical importance of these improvements is questionable as the scores were already very low after the discectomy and the magnitudes of absolute improvements were relatively small. The small number of subjects may have influenced the results and claims reported in this study.
ACKNOWLEDGEMENTS
The project was supported in part by the grants from Tae-Do Academic & Cultural Foundation of Korea, Sports Promotion Fund of Seoul Olympic Sports Promotion Foundation from the Ministry of Culture, Sports and Tourism of Korea, Gangneung-Wonju National University of Korea, Kyung Hee University International Scholars Program of Korea, and Maryland Industrial Partnerships (MIPS) Award.
REFERENCES