OBJECTIVE: Laryngeal hemiplegia, also known as vocal fold paralysis, causes severe communicative disability. Although voice therapy is commonly considered to be beneficial for improving the voice quality in several voice disorders, there are only a few papers that present scientific evidence of the effectiveness of voice therapy in treating the disabilities of laryngeal hemiplegia. The aim of this study was to evaluate the outcomes of voice therapy in patients with laryngeal hemiplegia and to evaluate the role of the time gap between onset of laryngeal hemiplegia and initiation of therapy.
DESIGN: A prospective study comparing subjects treated either within or more than 3 months after the onset of laryngeal hemiplegia.
SUBJECTS: The study involved 30 laryngeal patients with hemiplegia (16 males, 14 females, age range 15–80 years).
METHODS: All patients underwent videolaryngostroboscopy, maximum phonation time measurement, GIRBAS perceptual evaluation, Voice Handicap Index self-assessment and Multi-Dimensional Voice Program voice analysis before and after therapy.
RESULTS: In all tests, there were significant improvements in voice quality, both in the group treated within 3 months after the onset of laryngeal hemiplegia and in the group treated after this time.
CONCLUSION: Voice therapy is effective in treating laryngeal hemiplegia even if treatment is delayed by more than 3 months from onset of laryngeal hemiplegia.
Key words: laryngeal hemiplegia; voice therapy; multidimensional evaluation.
J Rehabil Med 2010; 42: 442–446
Correspondence address: Giovanna Cantarella, Otolaryngology Unit, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico Pad. Monteggia, Via F. Sforza 35-20122 Milano, Italy. E-mail: giovanna.cantarella@policlinico.mi.it
Submitted August 4, 2009; accepted January 15, 2010
INTRODUCTION
Laryngeal hemiplegia (LH), also known as vocal fold (VF) paralysis, is one of the most frequent pathologies encountered in voice rehabilitation practice. It is the consequence of a lesion of the vagus nerve, or more frequently, of its peripheral branch, the recurrent laryngeal nerve (RLN). The nerve lesion is often caused by iatrogenic factors (mainly cervical and thoracic surgery, or less commonly, neurosurgery), or by compression and/or infiltration by malignant neoplasia in the neck or mediastinum or by accidental trauma (cervical and thoracic injuries).
LH causes severe communicative disability. This condition can negatively influence the patient’s social, relational and professional life (1, 2). Furthermore, LH provokes a clinically debilitating condition due mainly to the chronic respiratory effort necessitated by the increased level of air flow through the incompetent glottis. The chronic effort also involves the phonatory muscles (both intrinsic and extrinsic laryngeal muscles), which contract excessively while attempting to reduce the glottal gap. LH is the cause of a typical dysphonia characterized by a breathy vocal emission and reduced intensity secondary to the insufficient glottal closure. Hypophonia and vocal fatigue are the main clinical symptoms. Another common symptom is “speech dyspnoea”, which is a typical condition of “air hunger” arising from the frequent inspirations during speech caused by increased airflow during phonation. Some patients may feel dizzy while phonating due to respiratory alkalosis, with a general feeling of exhaustion due to the efforts of the respiratory muscles.
Voice therapy (VT) is commonly considered as the first-step treatment to re-establish glottal competence, but some patients are referred to the speech therapist even several months or years after the onset of LH. This might be due to the limited awareness of the potential benefits obtainable through rehabilitative treatment. To date, only a few papers have highlighted the effectiveness of VT for LH (2, 3). Therefore, it is important to conduct studies to further demonstrate the possibility of achieving voice improvement through rehabilitation in LH. It is well known that several surgical techniques may obtain excellent and rapid voice improvement through the mediatization of the paralysed vocal fold (4–6). Nevertheless, many patients are reluctant to undergo a surgical procedure, especially if they are affected by an iatrogenic lesion of the RLN, as they may be fearful of possible complications of surgery (1).
The aim of this study was to evaluate the outcomes of VT in patients with unilateral LH and to compare the outcomes in subjects treated either within or after 3 months from the LH onset.
METHODS
Patients
This prospective study involved 30 patients affected by LH, referred to the phoniatrics and voice/speech therapy service of the Otolaryngology Unit of Ospedale Policlinico in Milan. The study group comprised 16 males and 14 females, age range 15–80 years, with a mean age of 59.20 (standard deviation (SD) 16.73) years.
The time elapsed from the onset of LH to the beginning of VT ranged from 1 month to 21 years and the mean time was 16.73 (SD 49.39) months. The sample was divided in 2 groups according to the time elapsed from the onset: within (early group) and after (late group) 3 months. The early group included 14 patients (9 males and 5 females), and late group included 16 patients (7 males and 9 females). The mean time elapsed from LH onset in the early group was 1.79 (SD 0.80) months, and in the late group 29.81 (SD 65.76) months. The mean age in the early group was 66.86 (SD 12.82) years, and in the late group 52.5 (SD 17.20) years. The difference in age was significant (U = 63.5; p = 0.043).
The paralyses were iatrogenic in 30 cases, due to the following causes: total or partial thyroidectomy (3 in early group and 4 in late group); surgical removal of cervical neoplasia (5 in early group and 2 in late group), particularly schwannoma, paraganglioma or adenopathies; pulmonary lobectomy (1 in early group and 3 in late group); thrombendarterectomy of the carotid artery (1 in early group and 2 in late group); oesophagectomy (1 in late group); carotid-subclavian bypass (1 in late group); thoracic aorta surgery (1 in early group); ischaemic bulbar stroke (1 in late group); compression by a cervical lymphoma (1 in late group); para-infective polyradiculoneuritis (1 in early group); and idiopathic paralysis (2 in early group and 1 in late group).
The paralysis was on the left side in 21 cases (13 in early group and 8 in late group) and on the right in the remaining 9 (1 in early group and 8 in late group).
Voice therapy
All patients underwent a total of 10–40 sessions of VT, 1–2 times per week, depending on the severity of dysphonia. The mean number of sessions undergone by the early group was 18.5 (SD 9.40) and by late group 18.81 (SD 8.62); there was no significant difference between groups (U = 104.5, p = ns). The subjects were instructed to repeat all the training exercises performed with the speech therapist 2–3 times a day for 10–15 min depending on the severity of the voice impairment, and to keep notes in a daily diary about the performed exercises.
The main goals of VT were to improve the loudness and steadiness of the voice and to reduce vocal effort (7, 8). Treatment modalities were tailored to the characteristics of each individual’s functional impairment, but in all cases aimed to improve vocal fold closure by strengthening adductor muscles and by achieving hyperadduction of the normal moving vocal fold.
The main rehabilitative steps included:
• relaxation exercises that aimed to release musculoskeletal tension of the shoulder, chest, neck and jaw;
• abdominal breathing training (at the beginning in the supine posture and later on in the standing position) aimed to increase breath support and to obtain a steady subglottic pressure;
• emission of a sustained /s/ on exhalation, while feeling by one hand movements and contraction of the abdominal wall;
• resonance voice exercises, such as humming, to enhance the feeling of oral vibratory sensations (9);
• digital manipulation of the thyroid cartilage;
• neck musculature massage;
• search for voice sonority by coughing and laughing;
• search for voice sonority on turning head to one side or the other;
• in case of persisting severe glottal incompetence, phonation with hard glottal attacks during pushing movements of the upper limbs (10) to achieve voice sonority during effort closure of the larynx (pushing exercises were performed in selected cases, due to risk of mucosal injury and development of hyperfunctional compensation).
Once voice sonority was obtained, the exercises included: sustained vowel emissions while enhancing diaphragmatic and abdominal breath support, controlled reading and, finally, conversation. Special attention was paid to achieving and maintaining optimal respiratory-phonatory coordination during spontaneous speech. Care was taken to correct and/or avoid the development of falsetto voice or hyperfunctional compensatory behaviours such as supraglottic constriction or tongue backing during phonation.
Methods of laryngeal and voice evaluation
Patients underwent the following evaluations before and at the end of VT:
• Videolaryngostroboscopy with a flexible FNL-10RP3 (Pentax Canada Inc., Mississauga, Ontario, USA) fiberscope or a SN 2320 (Kay Elemetrics, NJ, USA) 70 degrees rigid fibreoptic endoscope to document site and severity of the glottic gap, vocal fold vibration abnormalities and to obtain the objective assessment of post-treatment changes.
• Maximum phonation time (MPT) measurement obtained during the emission of a sustained /a/ at comfortable pitch and loudness; 3 consecutive trials were performed and the best one was considered.
• Perceptual voice evaluation by means of the GIRBAS scale (11, 12), which includes the 6 parameters of the grade of dysphonia (G), instability (I), roughness (R), breathiness (B), asthenia (A) and strain (S). The voice samples were computer-recorded using a dynamic microphone (model C 1000 S, AKG Acoustics GmbH, Vienna, Austria) at a constant distance of 5 cm from the patient’s mouth during the production of a sustained /a/, the repetition of single words and sentences, and conversation. All of the voice samples were subsequently evaluated by a jury of 4 experienced listeners (2 voice therapists and 2 phoniatricians), and scored in the usual manner (0 = normal; 1 = slight disturbance; 2 = moderate disturbance; 3 = severe disturbance). Voice samples were listened to several times until agreement was reached; nevertheless the intra-judges variability was quite low, as reported previously (13).
• Patient self-assessment by means of the Voice Handicap Index (VHI) (14). This is a 30-item test divided into 3 subscales that measure the functional, physical and emotional aspects of the disability caused by voice impairment. The subscale scores range from 0 to 50, and the total from 0 to 150; a higher score indicates a greater degree of disability.
• Multi Dimensional Voice Program (MDVP, Kay Elemetrics) analysis (15) (obtained in 12 cases): the sustained vowel /a/ was analysed. In our study, 7 parameters were considered: fundamental frequency (F0), jitter (Jitt%), shimmer (Shim%), noise to harmonic ratio (NHR), Variation’s coefficient of fundamental frequency (vF0), Variation’s coefficient of amplitude (vAm), and degree of unsounded voice (DUV).
Statistical analysis
Intra-group measures were analysed using the Wilcoxon signed-rank or Friedman tests. Intergroup pre-therapy comparison was performed with the Mann-Whitney test; and the intergroup post-therapy comparison with univariate general linear models (GLMs) correcting for age, initial grade of dysphonia and initial functional evaluation by VHI; moreover the statistical analyses of the post-therapy electroacoustic results were corrected also for initial vFo, NHR and DUV.
Group differences were also examined with multivariate GLMs. The observed power was 80%. Two-sided exact tests were used, and p-values of less than 0.05 were considered significant. All statistics were calculated using the Statistical Package for the Social Sciences 17.0 for Windows software package (SPSS Inc, Chicago, IL, USA).
RESULTS
Endoscopic evaluation confirmed the diagnosis of LH in all cases. After VT, the persistence of paralysis with improvement in glottal competence was found in all patients.
The 2 groups were similar for all variables, except for the grade of dysphonia and the functional score by VHI at basal evaluation (Tables I and II): in particular, the early group scores were worse than late group ones.
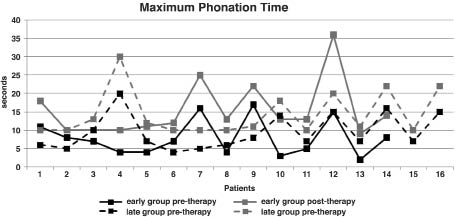
Pre-treatment MPT measurements varied from 2 to 20 s, while post-treatment values ranged from 9 to 36 s. Improvement in MPT was obtained in all the patients (Fig. 1). Before therapy, MPT was ≥ 10 s only in 9 patients, while at the post-therapy measurement MPT was ≥ 10 s in 29 cases. The 2 groups were similar for MPT before (U = 90.0) and after (F = 0.512) therapy. In the early group, the pre-treatment mean MPT value was 7.98 (SD 4.984) s, and in the late group, it was 9.50 (SD 4.872); in the early group, the post-treatment mean value was 15.43(SD 7.572) s, and in the late group, it was 14.31 (SD 6.16). The improvement was statistically significant in both groups (p < 0.0001).
Fig. 1. Pre- and post-therapy maximal phonation time values for each patient by group.
Table I shows the scores and results of univariate analyses of voice perceptive evaluation before and after VT by groups. All the patients showed a reduction in at least one parameter of the GIRBAS scale. The grade of dysphonia and the breathiness score were the most compromised parameters at basal evaluation. All the parameters had a statistically significant improvement after VT, except for strain in the early group. Table II shows the results of self-evaluation of VHI. The pre-treatment total score varied from 8 to 107, while at the end of VT the score was 0 to 87. Results were statistically significant in both groups for the global score and the 3 subscales.
| Table I. Scores for tests of voice perceptive evaluation before and after voice therapy (VT) by groups: mean (standard deviation) and univariate statistics. Z and p columns show the results of Wilcoxon tests. The pre-therapy column shows the results of Mann-Whitney tests (U, p) and the post-therapy column shows the results of univariate general linear models (GLMs) corrected for age, initial grade of dysphonia and initial functional evaluation by Voice Handicap Index (F,P) |
| | Group | Pre-therapy Mean (SD) | Post-therapy Mean (SD) | Z | p |
| Grade of dysphonia | Early | 2.64 (0.497) | 0.86 (0.770) | –3.354 | < 0.0001 |
| Late | 2.00 (0.730) | 0.63 (0.719) | –3.236 | < 0.0001 |
| | U = 58.0 p = 0.017 | F = 0.041 p = ns | | |
| Roughness | Early | 1.14 (1.099) | 0.43 (0.646) | –2.640 | 0.004 |
| Late | 1.00 (1.095) | 0.19 (0.403) | –2.511 | 0.007 |
| | U = 103.0 p = ns | F = 0.255 p = ns | | |
| Breathiness | Early | 2.29 (0.611) | 0.64 (0.842) | –3.236 | < 0.0001 |
| Late | 1.81 (0.981) | 0.56 (0.727) | –2.848 | 0.001 |
| | U = 82.5 p = ns | F = 2.258 p = ns | | |
| Asthenia | Early | 2.07 (0.829) | 0.71 (0.726) | –3.000 | 0.0001 |
| Late | 1.31 (1.195) | 0.38 (0.719) | –2.228 | 0.013 |
| | U = 72.0 p = ns | F =v0.879 p = ns | | |
| Strain | Early | 0.643 (1.151) | 0.14 (0.535) | –1.841 | ns |
| Late | 0.875 (1.025) | 0.19 (0.403) | –2.636 | 0.004 |
| | U = 93.5 p = ns | F = 2.543 p = ns | | |
| Instability | Early | 1.79 (0.975) | 0.21 (0.579) | –3.244 | < 0.0001 |
| Late | 1.25 (1.125) | 0.38 (0.619) | –2.889 | 0.001 |
| | U = 82.0 p = ns | F = 0.305 p = ns | | |
| Table II. Results of self-evaluation of Voice Handicap Index (VHI) by groups: mean (standard deviation) and univariate statistics. Z and p columns show the results of Wilcoxon tests. The pre-therapy column shows the results of Mann-Whitney tests (U, p), and the post-therapy column shows the results of univariate general linear models (GLMs) corrected for age, initial grade of dysphonia and initial functional evaluation by VHI (F,P) |
| | Group | Pre-therapy Mean (SD) | Post-therapy Mean (SD) | Z | p |
| Functional | Early | 24.86 (9.647) | 6.571 (9.428) | –3.301 | < 0.0001 |
| Late | 16.38 (9.351) | 6.06 (5.639) | –3.520 | < 0.0001 |
| | U = 60.0 p = 0.03 | F = 1.989 p = ns | | |
| Physical | Early | 24.79 (4.526) | 7.86 (10.339) | –3.062 | < 0.0001 |
| Late | 20.19 (8.697) | 9.31 (6.651) | –3.241 | <0.0001 |
| | U = 72.5 p = ns | F = 1.582 p = ns | | |
| Emotional | Early | 18.143 (10.932) | 6.57 (9.788) | –3.300 | < 0.0001 |
| Late | 12.56 (8.350) | 4.06 (5.053) | –2.933 | 0.001 |
| | U = 79.5 p = ns | F = 0.023 p = ns | | |
| Total | Early | 66.36 (20.742) | 21.00 (27.428) | –3.300 | < 0.0001 |
| Late | 49.13 (23.729) | 19.13 (15.878) | –3.517 | < 0.0001 |
| | U = 67.5 p = ns | F = 1.152 p = ns | | |
Multivariate analysis, in which all variables were analysed together, revealed that all patients improved in general (F = 4.681, p = 0.011). In particular, GLMs significant findings: MPT (F = 14.185, p = 0.001), functional score (F = 10.899, p = 0.004), physical score (F = 9.436, p = 0.006), emotional score (F = 6.418, p = 0.020), grade of dysphonia (F = 16.965, p = 0.001), breathiness (F = 17.293, p < 0.001), asthenia (F = 5.762, p = 0.026), and instability (F = 15.293, p = 0.001). No significant results were found for roughness and strain. No statistically significant differences were observed between the 2 groups in multivariate analysis, except for breathiness (F = 5.631, p = 0.028) and strain (F = 5.586, p = 0.028) after stratifying for gender. In particular, breathiness and strain in females improved less in the late group than in the early group; while in males, the improvements were the same in both groups.
Results of electroacoustic analysis by MDVP are shown in Table III for 12 participants. Statistically significant improvements were found in both groups for the parameters of frequency instability (jitter %, vF0) and for the NHR. The shimmer % and the DUV were significantly modified only in the early group, but in the late group, 4 patients had a pre-treatment DUV value greater than 0. The DUV values were null after VT in all cases.
| Table III. Results of electroacoustic analysis by Multi Dimensional Voice Program in 12 patients (5 in the early group, 7 in the late group). Z and p columns show the results of Wilcoxon tests. The pre-therapy column shows the results of Mann-Whitney tests (U, p), and in the post-therapy column shows the results of univariate GLMs corrected for age, initial grade of dysphonia, initial functional evaluation, vFo, NHR and DUV by Voice Handicap Index (F,P) |
| | Group | Pre-therapy Mean (SD) | Post-therapy Mean (SD) | Z | p |
| Jitter (%) | Early | 8.49 (5.637) | 1.46 (0.777) | –2.023 | 0.031 |
| Late | 5.22 (6.259) | 1.48 (0.804) | –2.028 | 0.023 |
| | U = 9.0 p = ns | F = 1.255 p = ns | | |
| vF0 (%) | Early | 15.24 (12.513) | 1.95 (1.079) | –2.023 | 0.031 |
| Late | 5.10 (5.815) | 1.56 (0.672) | –2.197 | 0.016 |
| | U = 4.0 p = 0.030 | F = 0.627 p = ns | | |
| Shimmer (%) | Early | 16.88 (8.954) | 4.16 (2.137) | –2.023 | 0.031 |
| Late | 7.55 (5.139) | 4.21 (1.542) | –1.690 | ns |
| | U = 6.0 p = ns | F = 0.052 p = ns | | |
| vAm | Early | 19.66 (5.730) | 9.91 (6.653) | –1.753 | ns |
| Late | 16.38 (12.974) | 11.12 (10.320) | –1.183 | ns |
| | U = 10.0 p = ns | F = 0.155 p = ns | | |
| NHR | Early | 0.44 (0.121) | 0.15 (0.020) | –2.023 | 0.031 |
| Late | 0.22 (0.204) | 0.11 (0.022) | –1.859 | 0.039 |
| | U = 5.0 p = 0.048 | F = 3.695 p = ns | | |
| DUV (%) | Early | 64.00 (30.947) | 0.00 (0.000) | –2.023 | 0.031 |
| Late | 17.76 (31.361) | 0.00 (0.000) | –1.604 | ns |
| | U = 5.0 p = 0.038 | | | |
| vF0: Variation’s coefficient of fundamental frequency; vAm: Variation’s coefficient of amplitude; NHR: noise to harmonic ratio; DUV: degree of unsounded voice. |
DISCUSSION
Although voice rehabilitative treatment is commonly considered to be effective for improving voice quality in several voice disorders, there have been only a few studies showing scientific evidence of its effectiveness in treating the disabilities of LH (16, 17). Furthermore, it is commonly thought that prompt treatment is desirable to achieve optimal results, but, to date, no studies have addressed the relationship between the delay in VT initiation and the voice improvement achieved. Our study provides further objective evidence that a conservative rehabilitative method can significantly improve voice and quality of life in patients affected by vocal fold paralysis. Patients treated 3 months after LH onset obtained results that were comparable with those achieved in patients starting VT promptly.
Before VT, the disability related to LH was comparable in the 2 groups for all parameters, except the functional scale of VHI questionnaire and the grade of dysphonia evaluated perceptually by GIRBAS scale. These 2 variables were lower in the late group. This is an expected result, as some spontaneous recovery of voice quality usually occurs with time after a lesion of vagus nerve or the RLN (2).
MPT measurements were similar before the treatment in both groups, indicating comparable glottic incompetence; in fact, it is known that the MPT value is related to the gap in the glottic closure (16).
At the end of VT, the voice quality and quality of life were comparable in the 2 groups, as demonstrated by perceptual voice evaluation, which showed an improvement for all 6 parameters of the GIRBAS scale and by the VHI self-assessment.
After VT, every patient achieved a longer MPT (Fig. 1), demonstrating a more efficient glottic closure, and the improvement was comparable in the 2 groups.
Voice acoustic analysis was obtained in only 12 patients, as there was high aperiodicity of voice signals in most of the remaining patients. The limited number of patients might explain the non-significant results for some of the variables despite the overall improvement in all the variables.
Although the late group started with better initial conditions than the early group because of spontaneous recovery, the patients in the late group obtained further improvements. This demonstrates that VT is necessary for all patients, regardless of the time since onset of LH.
The reported results demonstrate that VT is a valuable means to treat dysphonia due to LH, not only for patients in whom VT is initiated promptly, but also for patients with delayed VT initiation from the onset of LH. Several surgical approaches are available to treat LH (4, 18), but a rehabilitative treatment may also offer a significant improvement for cases with long-standing LH, such that the option of surgery can be reserved for cases with inadequate improvement based on the patient’s needs.
In conclusion, the multidimensional evaluation of voice changes highlighted that voice rehabilitative treatment is significantly effective for treating paralytic dysphonia, even when several months or years have elapsed from the onset of laryngeal paralysis.
Acknowledgements
The authors are grateful to the speech therapists Annamaria Zambarbieri, Annaclara Ciabatta and Cristiana Assi for their precious rehabilitative work and for their devotion to patients’ well being.
REFERENCES