OBJECTIVE: To determine if repetitive task training after stroke improves functional activity.
DESIGN: Systematic review and meta-analysis of trials comparing repetitive task training with attention control or usual care.
DATA SOURCES: The Cochrane Stroke Trials Register, electronic databases of published, unpublished and non-English language papers; conference proceedings, reference lists, and trial authors.
Review methods: Included studies were randomized/quasi-randomized trials in adults after stroke where an active motor sequence aiming to improve functional activity was performed repetitively within a single training session. We used Cochrane Collaboration methods, resources, and software.
RESULTS: We included 14 trials with 17 intervention-control pairs and 659 participants. Results were statistically significant for walking distance (mean difference 54.6, 95% confidence interval (95% CI) 17.5, 91.7); walking speed (standardized mean difference (SMD) 0.29, 95% CI 0.04, 0.53); sit-to-stand (standard effect estimate 0.35, 95% CI 0.13, 0.56), and activities of daily living: SMD 0.29, 95% CI 0.07, 0.51; and of borderline statistical significance for measures of walking ability (SMD 0.25, 95% CI 0.00, 0.51), and global motor function (SMD 0.32, 95% CI –0.01, 0.66). There were no statistically significant differences for hand/arm functional activity, lower limb functional activity scales, or sitting/standing balance/reach.
CONCLUSION: Repetitive task training resulted in modest improvement across a range of lower limb outcome measures, but not upper limb outcome measures. Training may be sufficient to have a small impact on activities of daily living. Interventions involving elements of repetition and task training are diverse and difficult to classify: the results presented are specific to trials where both elements are clearly present in the intervention, without major confounding by other potential mechanisms of action.
Key words: stroke; physical therapy modalities; recovery of function; task performance and analysis; motor activity; activities of daily living.
J Rehabil Med 2010; 42: 9–15
Correspondence address: Beverley French, Brook 434, University of Central Lancashire, Preston, PR1 2HE, UK. E-mail: bfrench1@uclan.ac.uk
Submitted November 25, 2008; accepted September 1, 2009
INTRODUCTION
Stroke is a major cause of long-term neurological disability in adults (1), with approximately half of all stroke survivors left with severe functional problems in the acute stage of stroke (2). Prevalence rates vary depending on the cohort studied, but up to 20% of people with initial impairment have no functional use of the arm at 6 months (3–6), and 15% are unable to walk independently indoors (7). Only 18% regain unrestricted walking ability (8).
Exercise programmes in which movement related to functional activity is directly trained (referred to as task-related training) have shown better results than impairment-focussed programmes (9). More intensive therapy has been shown to improve the rate of recovery in activities of daily living (ADL) (10), particularly if a functional approach is adopted (11, 12). One way of increasing intensity is to include task repetition. Repetitive task training (RTT) therefore combines elements of both relevance to functional activity, and intensity of practice.
In the UK, task-related training has not traditionally been a significant part of therapy after stroke, which has been dominated by the Bobath approach. This specifically minimizes repetitive active movement, and relies on therapist-guided restoration of “normal movement” patterns, rather than the purposeful, but possibly unnatural, movement that could occur as a result of a more pragmatic approach within RTT. However, RTT has the potential to be a resource efficient component of stroke rehabilitation, including delivery in a group setting, or self-initiated practice in the home environment. As part of a wider UK Health Technology Assessment review (13) we examined the efficacy of RTT compared with either attention control or usual care approaches, in a Cochrane systematic review (14). This paper is a summary of the core review.
METHODS
We used QUORUM guidelines (15), and Cochrane Collaboration methods, resources, and software (RevMan 4.2). Studies were eligible if they were randomized or quasi-randomized controlled trials in adults after stroke, with an intervention where an active motor sequence was performed repetitively within a single training session, and where the practice aimed towards a clear functional activity goal. Functional activity goals could be complex whole tasks, such as walking, or smaller movements to facilitate activity, such as grasp, grip or balance. To be included, trials of repetitive activity were required to involve complex multi-joint movement with measurement of functional activity as an outcome. Trials were included only if the amount of practice could be quantified, either in terms of duration or number of repetitions.
Trials were excluded if they were focused on impairment-related outcomes, such as motor performance or endurance, rather than functional activity; if assisted movement was predominant; or if trials combined RTT with other interventions where the influence of task repetition could not be isolated, e.g. electrical stimulation, virtual environments, forced use, robotics. We included trials using mechanical or robotic assistance if the purpose was to facilitate task-related repetition, but excluded trials using mechanical means for repeating simple single joint movement. We included mixed interventions with some element of exercise, as well as task-related training if it was judged that the task-related components were predominant, e.g. 10 min treadmill or static cycling in a 1 h lower limb circuit training programme. Trial authors were contacted for clarification of the content of interventions. Trials of constraint-induced movement therapy and treadmill training were considered to be a form of enhanced task-related training (where other mechanisms such as restraint as well as task repetition were active). These trials were included in the full review (13), but are not included here.
The primary outcomes were measures of:
• global functional activity, e.g. Motor Assessment Scale
• functional activity of the upper limb
– arm function, e.g. Action Research Arm Test
– hand function, e.g. Jebsen Test of Hand Function
– sitting balance/reach, e.g. Reaching Performance Scale
• functional activity of the lower limb
– walking distance/speed, e.g. 6-minute walk test
– walking activity, e.g. Functional Ambulation Classification
– sit-to-stand
– lower limb functional activity, e.g. Rivermead Mobility Index
–standing balance/reach, e.g. Berg Balance Scale
Secondary outcomes were ADL, health-related quality of life, impairment measures and adverse events. Primary outcome timing was at the end of the treatment period, with follow-up at up to 6 and 12 months.
The Cochrane Stroke Group Trials Register was searched by the Trials Coordinator in October 2006 using the Intervention Types: “Physiotherapy” and “Occupational Therapy”. We also searched the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 3 2006); MEDLINE (1966 to September Week 4, 2006); EMBASE (1980 to Week 40, 2006); CINAHL (1982 to October Week 1, 2006); AMED (1985 to Week 40, 2006); SPORTDiscus (1980 to October Week 1, 2006); ISI Science Citation Index (1973 to 14 October 2006); Index to Theses (1970 to September 2006); ZETOC (to 14 October 2006); PEDro (to 3 October 2006); OT Seeker (to 21 April 2006); and OT Search (to March 2006). Because the terminology related to exercise-related interventions can be unspecific, the search design and parameters were set very widely. The full search strategy was developed by the review team and checked by the Cochrane Stroke Group Trials Coordinator, and is available from the authors.
Because task-based training is popular in other countries, we sought to identify additional non-English language trials by searching Chinese, Russian and Indian databases using broad descriptors for stroke, rehabilitation and physical therapy. The China National Knowledge database was searched in both English and Chinese. Sixteen methods sections and 3 full non-English language papers that were screened as potentially relevant were commercially translated. Registers of unpublished trials were searched, as well as conference proceedings not covered by the Cochrane Stroke Group. Trial authors were contacted, 27 existing systematic reviews of physical therapy in stroke were combed for relevant references, cited referencing searching was carried out for all included trials, and messages were posted on physiotherapy bulletin boards online.
We trained reviewers, using the κ statistic to assess adequate levels of agreement prior to independent filtering, data extraction and review of the quality of the eligible trials by 2 reviewers. Filtering was undertaken by all reviewers together until an acceptable κ (0.63) was achieved. Inter-rater reliability of judgement over 8 studies of 7 criteria for quality assessment using unweighted multiple κ was median κ = 0.67 (range 0.48–0.85). Disagreements were reviewed and instructions for critical appraisal grading were revised. We attempted to contact all trial authors for clarification of intervention content, and the whole review team were involved in the final decision if there was any uncertainty about trial inclusion.
Extracted data included details of randomization method, study population, intervention methods and delivery, reason for losses to follow-up, information relating to treatment monitoring, acceptability and adherence, and post-therapy and follow-up outcome measures. Assessment of methodological quality was classified as adequate, unclear or inadequate for allocation concealment, baseline comparability of groups, equal treatment during intervention and usual care, loss to follow-up, and blinding of outcome assessors.
All statistical treatments were based on guidance in the Cochrane Handbook (16). For continuous outcomes using similar measurement scales, we used the weighted mean difference (WMD) with 95% confidence intervals (95% CI). Where similar outcomes were measured using different outcome scales, results were combined using standardized mean difference (SMD) and 95% CI. Outcomes containing both dichotomous and continuous measurement units were analysed using the generic inverse variance method, and expressed as an estimate of the standardized effect (SE). Most of the available data were post-therapy scores, but change from baseline scores were used where available across trials. The degree of heterogeneity among the trials was assessed by the I2 statistic for each outcome, and if greater than 50%, meta-analysis used both fixed and random-effects modelling. To assess clinical diversity, planned subgroup analyses were undertaken for type of participant (time from stroke), and intervention type and dosage. To assess methodological diversity, planned sensitivity analyses were undertaken for allocation concealment, with post-hoc analyses for equivalence of treatment, and type of comparison group.
RESULTS
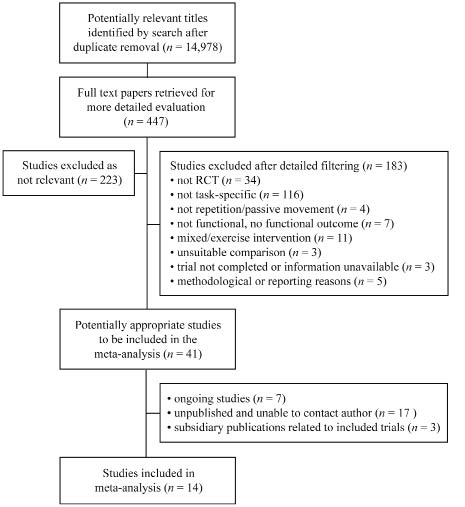
Of 14,978 items identified by the search (after removal of duplicates), 447 records considered potentially relevant were identified from screening on title and abstract, and the full papers for these items were retrieved, including 71 papers in languages other than English. Out of the 447 full papers retrieved, 223 were excluded as not relevant, and 224 were categorized as potentially relevant and progressed to more detailed filtering. Details of the 210 further exclusions are given in Fig. 1.
Fig. 1. Inclusion and exclusion of papers in the meta-analysis. RCT: randomized controlled trials.
We identified 14 trials, which were all included in the meta-analysis. Three of the trials had 2 arms that met the inclusion criteria, resulting in 17 intervention-control comparisons relevant to the review.
Trials could be split into 3 major types: whole therapy approaches, such as movement science, where the rehabilitation programme as a whole is grounded in task-specific motor relearning principles; mixed task practice approaches including circuit training, which provide sessional practice in a range of task-specific activities, often in a group and context relevant setting and sometimes combined with small elements of strength or endurance training; and single task training, dealing with a specific skill such as sit-to-stand, or balance. Table I illustrates the intervention details for one study from each category.
| Table I. Examples of intervention types |
| Category and example | Details of intervention |
| Whole therapy approaches, e.g. Movement Science (Van Vliet et al. (25)) | Rehabilitation based on movement science principle that skill in performance is a direct function of the amount of practice. Programme involved use of everyday objects for training, and practice outside of delivered sessions. Median treatment was 23 min per weekday, delivered by physiotherapists, occupational therapists and physiotherapy assistants, in hospital, and as an outpatient after discharge. Comparison group: Bobath based therapy. |
| Mixed task training e.g. circuit training (Salbach et al. (24)) | Mobility intervention: 10 walking-related tasks designed to strengthen the lower extremities and enhance walking balance, speed and distance in a progressive manner. Sessions were 1 h, 3 times a week for 6 weeks = 18 h, delivered individually by a physical or occupational therapist after discharge from physical rehabilitation in a hospital outpatient or rehabilitation setting. Comparison group: upper extremity training. |
| Single task training e.g. sit-to-stand training (Barreca et al. (17)) | Sit-to-stand training: group class practice in attaining standing from sitting from a variety of different heights and surfaces. Sessions were 45 min, 3 times a week until competence or discharge. Classes had 6 or 7 participants, supervised by 2 registered practical nurses, with extra practice delivered by nurses trained on the sit-to-stand protocol in a ward setting using videotapes, written instruction and practice. Comparison group: usual care + recreation therapy. |
Table II identifies the relevant trials for the 3 main categories of RTT intervention for upper and lower limbs. Trials that recruited within 6 months after stroke, and those that provided more than 20 h of training are labelled.
| Table II. Classification of included studies |
| Lower limbs | Upper limbs |
| Whole therapy approaches |
| Langhammer & Stanghelle (22) (0–6) Van Vliet et al. (25) (0–6) |
| Mixed task practice/exercise, and circuit training approaches |
| Salbach et al. (24) Dean et al. (20) Blennerhassett & Dite (19) (0–6) Kwakkel et al. (11) (0–6, > 20 h) McClellan & Ada (23) (> 20 h) | Higgins et al. (26) Blennerhassett & Dite (19) (0–6) Kwakkel et al. (11) (0–6, > 20 h) Turton & Fraser (27) (> 20 h) Winstein et al. (28) (0–6) Yen et al. (29) (0–6, > 20 h) |
| Single task training: Sitting/standing balance and reach |
| de Sèze et al.(21) (0–6) Barreca et al. (17) (0–6) | de Sèze et al. (21) (0–6) Dean & Shepherd (18) Howe et al. (35) (0–6) |
| 0–6: recruited within 6 months post-stroke; > 20 h: more than 20 h training provided in the intervention. |
Table III details the outcome measures used in the trials for lower limb functional activity; balance or sit-to-stand; upper limb functional activity; and quality of life or global functional activity. As the trials used a variety of outcome measures, most results are presented as standardized mean difference except walking speed, which is expressed as a weighted mean difference for metres walked in 6 minutes.
| Table III. Outcome measures used from the included studies |
| | Lower limb function | Balance/sit-to-stand | Upper limb/hand function | Quality of life, health status, ADL function, global function |
| Barreca et al (15) | | Number able to stand | | |
| Blennerhassett & Dite (19) | 6-min walk test Step test | Timed up & go test | MAS arm MAS hand | |
| Dean & Shephard (18) | 10-m walk speed | Reaching distance | | |
| Dean et al. (20) | 6-min walk test 10-m walk speed Step test | | | |
| De Sèze et al. (21) | FAC | Sitting Equilibrium Index Standing Equilibrium Index | | FIMTM |
| Howe et al. (35) | | Lateral reach-time Sit-to-stand: time | | |
| Kwakkel et al. (11) | FAC | | Action research arm test | Barthel Index |
| Langhammer & Stanghelle (22) | MAS – walking SMES: trunk, balance, gait | MAS balanced sitting MAS sit-to-stand | MAS arm MAS hand | MAS Barthel Index |
| McClellan & Ada (23) | MAS walking | Functional reach | | |
| Salbach & Mayo (24), Higgins et al. (26) | 6-min walk test 5-m walk speed | Timed up & go test Berg Balance | Box & block test 9-hole peg test | Barthel Index |
| Turton & Fraser (27) | | | Southern Motor Group Assessment – UE 10-hole peg test | |
| Van Vliet et al. (25) | RMA leg and trunk 6-min walk test MAS walking | MAS balanced sitting MAS sit-to-stand | MAS arm MAS hand | RMA gross function Barthel Index |
| Winstein et al. (28) | | | Functional test of the hemiparetic upper extremity | |
| Yen et al. (29) | | | Wolf motor function test | |
| ADL: activities of daily living; FAC: Functional Ambulation Classification; FIMTM: Functional Independence Measure; MAS: Motor Assessment Scale; RMA: Rivermead Motor Assessment; SMES: Sødring Motor Evaluation of Stroke patients; UE: upper extremity. |
Lower limb functional activity/standing balance
Ten trials (11, 17–25) with 476 participants measured lower limb functional activity or standing balance. The types of intervention are summarized in Table II, and details of the outcome measures used in the trials are given in Table III. Four of the trials recruited in the first 3 months following stroke (11, 17, 21, 22). All trials were delivered by a therapist in hospital or community settings, except for one (23), which was a home mobility programme for participants following videotaped exercise, with therapist telephone contact and follow-up. Two trials included more than 20 h total practice time (11, 23), while the rest provided less than 20 h.
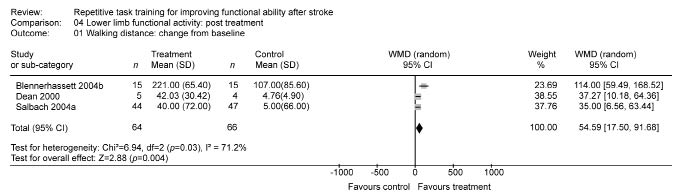
Table IV summarizes the pooled treatment effects for different measures of lower limb function. There was a statistically significant small to moderate impact of repetitive task training on some aspects, including walking distance, walking speed, and sit-to-stand. Pooled results for the Functional Ambulation Classification measure were small, and of borderline statistical significance. There was no evidence of effect on lower limb functional activity scales, or standing balance/reach.
| Table IV. Impact of repetitive task training on lower limb measures |
| | n | Post-treatment effect size (95% CI) |
| Walking distance | 130 | WMD 54.59 (17.50, 91.68) |
| Walking speed | 263 | SMD 0.29 (0.04, 0.53) |
| Sit-to-stand | 346 | SE 0.35 (0.13, 0.56) |
| Functional Ambulation Classification | 238 | SMD 0.25 (0.00, 0.51) |
| Lower limb functional activity scales | 176 | SMD 0.20 (–0.10, 0.50) |
| Standing balance/reach | 132 | SMD 0.29 (–0.06, 0.63) |
| CI: confidence interval; SE: standardized effect; SMD: standardized mean difference; WMD: weighted mean difference. |
The forest plot for walking distance is given in Fig. 2. In effect, participants in the experimental groups could walk on average 55 m further in 6 min than those in the control groups. Re-analysis using the SMD confirmed that the result remained statistically significant: SMD 0.98, 95% CI 0.23, 1.73.
Fig. 2. Forest plot for walking distance: Change from baseline. ■ = effect size for one trial; horizontal line = 95% confidence interval; ♦ = pooled effect size for all trials. CI: confidence interval; SD: standard deviation; WMD: weighted mean difference. John Wiley & Sons Ltd, on behalf of the Cochrane Collaboration, grant permission to print this figure.
Upper limb function/sitting balance
Eight trials (11, 19, 22, 25–29) with 467 participants measured upper limb functional activity. The types of interventions are summarized in Table II, and the outcome measurements in Table III. All of these interventions were delivered by a therapist in hospital or community settings, except one (18) delivered by a therapist in the home environment, and one (27) consisting of self-initiated practice in the home environment using a booklet of exercises, after instruction by a therapist. All but 2 trials (26, 29) were carried out 0–6 months post-stroke, and 3 trials (11, 27, 29) provided more than 20 h total training time. In 2 of the trials (27, 28) training time was additional to usual care.
Table V summarizes the pooled treatment effects, with no evidence of effect for RTT on arm or hand functional activity, or on sitting balance/reach.
| Table V. Impact of repetitive task training on upper limb measures |
| | n | Post-treatment effect size (95% CI) |
| Arm functional activity | 412 | SMD 0.17 (–0.03, 0.36) |
| Hand functional activity | 281 | SMD 0.16 (–0.07, 0.40) |
| Sitting balance/reach | 210 | SMD 0.23 (–0.05, 0.50) |
| CI: confidence interval; SMD: standardized mean difference. |
Global motor functional activity
For the 2 trials (22, 25) using global motor functional activity measures, there was a pooled small to moderate, borderline statistically significant effect on global motor functional activity: SMD 0.32, 95% CI –0.01, 0.66.
Secondary outcomes
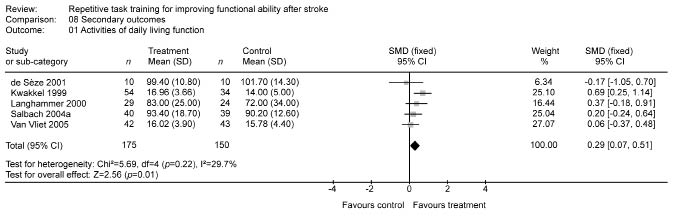
There was a small, statistically significant effect of RTT on ADL: SMD 0.29, 95% CI 0.07, 0.51 (Fig. 3).
Fig. 3. Forest plot for secondary outcome: activities of daily living. ■ = effect size for one trial; horizontal line = 95% confidence interval; ♦ = pooled effect size for all trials. CI: confidence interval; SD: standard deviation; SMD: standardized mean difference. John Wiley & Sons Ltd, on behalf of the Cochrane Collaboration, grant permission to print this figure.
There was no evidence of impact on upper limb impairment: SMD 0.14, 95% CI –0.15, 0.43, lower limb impairment: SMD 0.13, 95% CI –0.33, 0.59, or perceptions of quality of life/health status: SMD 0.08, 95% CI –0.24, 0.41. RTT was not associated with a greater number of adverse events, although the data on which this was based were limited.
Follow-up analyses
Results for later follow-up to 6 or 12 months post-therapy were not statistically significant for either upper or lower limbs (Table VI).
| Table VI. Retention effects of training at up to 6 months and 6–12 months post-therapy |
| | Treatment effect size up to 6 months post-therapy | Treatment effect size 6–12 months post-therapy |
| n | SMD (95% CI) | n | SMD (95% CI) |
| Upper limb | 51 | 0.50 (–0.06, 1.06) | 195 | –0.02 (–0.31, 0.26) |
| Lower limb | 80 | 0.11 (–0.33, 0.56) | 170 | –0.01 (–0.32, 0.29) |
| CI: confidence interval; SMD: standardized mean difference. |
Subgroup and sensitivity analyses
Upper limb treatment effects were not modified by time since stroke, dosage of task practice, or type of task training. Lower limb treatment effects were not found to be dependent on time since stroke. The effects of larger vs smaller amounts of training also did not reach statistical significance (p = 0.15). Comparing mixed task training approaches against whole therapy or single task training showed a moderate effect (p = 0.08), but the sample size (n = 63) for single task training was very small.
In the sensitivity analyses, there was no statistically significant difference between trials judged to have adequate, vs inadequate or unclear, allocation concealment (χ2 = 0.03, df = 1, p = 0.86); or between trials providing equal vs additional treatment time (χ2 = 1.47, df = 1, p = 0.23). The difference between trials using an attention control and those using a usual care comparison group was not quite statistically significant (χ2 = 2.08, df = 1, p = 0.15).
Quality of the evidence
Eight out of 14 trials had adequate allocation concealment. Five of the remaining 6 trials reported allocation concealment, but the method lacked detail. One of the trials (27) was quasi-randomized. Of the randomized controlled trials that were not pilot studies, only 4 out of 10 gave a power calculation for sample size. However, 7 of the trials had more than 50 participants. All except 2 (27, 28) of the trials stated that blinded independent assessors were used, but only 4 (11, 20, 24, 25) referred to checks for assessor unblinding. Therapy time was non-equivalent in 2 trials (27, 28). In summary, the overall quality of the trials gives a degree of confidence in the results.
DISCUSSION
This review aimed to consider whether repetitive task-related training impacted on functional activity outcomes. In practice, many rehabilitation interventions include mixed interventions, making them difficult to place into simple categories, so in practice we did include diverse interventions, and chose to use duration of practice as a surrogate for quantification of repetition. The review also excluded complex interventions with multiple mechanisms of action, such as robotics, functional electrical stimulation, and constraint-induced movement therapy. As with any review, the results must be interpreted in the light of the definitions chosen to guide inclusion. We acknowledge that classification of intervention content involves judgement, and if any trial author who we have not communicated with feels that our judgement is incorrect, we would be happy to review the decisions made.
The included trials are clinically diverse, and there are gaps in the evidence base, with only a few trials in the different categories of intervention, and at different stages after stroke. However, the pooled results for different types of lower limb outcome measure provide sufficient evidence to validate the general principle that repetitive, task-related training for lower limbs can result in functional activity gain, when compared against other forms of usual care, or attention control. While the degree of gain is modest, impact does appear to be of a clinically meaningful magnitude, but it is unclear whether these effects are sustained once training has ended. In the pooled results for those studies that provided later assessments (19–23, 25), improvements at the end of training were not evident at the later stage. It is unclear from this review whether this is related to characteristics of the participants, the intensity of training or the degree of improvement required before detectable change was noted.
As in other reviews (10) we found a differentiation of effect of training for upper and lower limbs, but in contrast to other reviews (30) we found no evidence of significant benefit from repetitive training of upper limb functional activity. Upper limb treatment effects of longer (SMD 0.40, 95% CI 0.03, 0.78) vs shorter (SMD 0.18, 95% CI –0.02, 0.39) amounts of training were of a different magnitude, but the difference did not reach statistical significance (p = 0.31). Hence, the review did not provide evidence to support a suggestion that upper limb results are moderated by the amount of practice (12). However, this is very tentative, as only 3 studies included more than 20 h training, with a recent review of robotics suggesting a dose-response relationship for upper limb therapy (31). Some caution is also needed in interpreting the lack of evidence for adverse effect, as few trials specifically monitored these as an outcome. If task-specific training is used in clinical practice, adverse effects should be monitored.
Evidence from this review does not support the suggestion that earlier provision of treatment results in greater improvement in functional activity, as treatment effects were not modified by time since stroke. Improvement in functional activity was possible even in the later stages of recovery (32). We were unable to come to any conclusions about the previously identified dose-response relationship between amount of therapy and improved outcome (10), but the results from subgroup analysis suggest this as a priority for further research for both upper and lower limb interventions.
The diversity of interventions makes it difficult to speculate about the mechanisms of action responsible for gains in lower limb functional ability. While all contained repetition and task practice, they could also include some element of endurance or strength training. The results presented here are specific to trials where both elements are clearly present in the intervention, without major confounding by other potential mechanisms of action. However, recent reviews of other therapies where repetition is a major mechanism, such as treadmill training (33) and robot-aided therapy (34), showed little or no consistent functional gain, so this would suggest that reflecting real-world task complexity in training is a significant factor.
The evidence provided by the review appears to be widely applicable, perhaps with the exception of very severely disabled people with little postural control or voluntary movement, those with very mild deficits, and those with severe communication difficulties. These groups were usually excluded from the trials. In addition, the review excluded many trials of types of movement, which aim to help people to progress into activity-related training, such as gait training or cycling, and trials with a large element of passive movement, which could effectively also exclude people with severe impairments.
In terms of generalizability to European care contexts there are only 2 trials of limb-specific RTT therapy:one quasi-randomized trial of upper limb therapy (27); and one trial of leg training (11). Two trials using whole therapy approaches (22, 25), and 3 trials of balance training (18, 21, 35) have also been completed in European contexts. While RTT is likely to be transferable in principle, its effectiveness against other forms of care usual in Europe, and its acceptability in these healthcare settings have not been widely tested. In particular, the feasibility and acceptability of circuit-style training approaches in community, rehabilitation, and residential settings would need to be evaluated. The delivery of interventions after the usual rehabilitation period would have resource consequences, but the presence of 2 trials involving self-delivery in the home environment (23, 27), and 3 trials involving group delivery of task-specific training (17, 19, 20), suggest that more resource-efficient modes of delivery are feasible.
ACKNOWLEDGEMENTS
We would like to acknowledge the help of trial authors, who kindly replied to our requests for information.
This paper is based on a Cochrane review published in The Cochrane Library 2007 Issue 4 (see www.thecochranelibrary.com for information) (14). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the Cochrane Library should be consulted for the most recent version of the review. The results of a Cochrane review can be interpreted differently, depending on people’s perspectives and circumstance. Please consider the conclusions presented carefully. They are the opinions of the review authors, and are not necessarily shared by the Cochrane Collaboration.
Funding: This review is part of a wider project funded by the NHS R&D Health Technology Assessment Programme Project Number 05/17/04 (13). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the UK Department of Health.
Conflicts of interest: The authors declare they have no competing interests.
REFERENCES